Abstract
Background
Posterior component separation with transversus abdominis release technique is increasingly being used for abdominal wall reconstruction in complex abdominal wall repair. The main purpose of this study is to present a modification of the surgical technique originally described that facilitates the surgical procedure and offers additional advantages.
Methods
Based on the knowledge of the anatomy of the retromuscular space and the preperitoneal aerolar tissue distribution, we start the incision on the posterior rectus sheath from the arcuate line in a down to up direction. The posterior rectus sheath is incised 0,5–1 cm medial to the linea semilunaris and cut longitudinally as far as the fibers of transversus abdominis muscle that are divided in the superior part of the abdomen. It is also possible to avoid cutting the fibers of this muscle if we incise the posterior rectus sheath in an oblique direction to the midline from the umbilical area. Since 2012 to 2016, 69 consecutive patients with down to up TAR have been prospectively followed. Main outcome measures included demographics, perioperative details, wound complications, and recurrences.
Results
Between 2012 and 2016, we have operated 69 patients with down to up TAR technique. Mean operative time was 251 (range 65–566) minutes. Mean hospital stay was 9,8 (2–98) days. 10 patients presented surgical site events (14,5%): 6 patients had superficial site infection, 3 deep and 1 organ space. During follow-up, 3 patients (4,3%) presented incisional hernia recurrence.
Conclusions
This novel modification allows a simpler dissection of the preperitoneal retromuscular space and makes the TAR technique easier to perform. It also enables to incise only the insertion of the transversalis fascia cranially.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of complex abdominal wall hernias is a surgical challenge and multiple techniques have been described so far. From an historical point of view, treatment of incisional abdominal hernias has evolved. Different techniques have been described and the use of synthetic non-absorbable meshes has become widespread. Onlay placement of meshes with anterior component separation technique might be used in cases of important loss of domain or if the patient has undergone previous incisional hernia repairs [1, 2]. However, this approach yields two important inconveniences: a large subcutaneous tissue dissection that may be the cause of postoperative seromas and cutaneous necrosis, and the anatomical edges of the abdominal wall like the insertion of the abdominal wall in bone structures, as the iliac crest and the costal margins, that can difficult the proper extension of the mesh and may prevent from obtaining enough overlap over the defect [3, 4]. Recent expert consensus also describes increased wound complications in standard anterior component separation in comparison with other techniques [5, 6]. Nonetheless a recent review did not show any significant differences in surgical site occurrences compared to posterior component separation [2]. Endoscopic and perforator-sparing anterior components separation have been reported as a modification to the standard anterior components separation with little consensus on the reduction of postoperative complications [7].
Complex incisional hernia repair in a retro-rectus and preperitoneal space as the modified Rives-Stoppa-Wantz procedure provides several advantages as diminishing subcutaneous tissue dissection, avoiding contact of the polypropylene mesh to the abdominal viscera and lowering the incidence of hernia recurrence [8,9,10]. However, this technique does not allow for dissection beyond the lateral border of the posterior rectus sheath, making it insufficient to overlap the defect and to provide tension-free repair of large abdominal wall defects as in the case of massive loss of domain [11]. Furthermore, it does not solve the problem of the anatomical limits for lateral hernias. The first posterior component separation (PCS) was described by Carbonell [12], creating a space between the internal oblique muscle and the transversus abdominis muscle to open the lateral attachments of the abdominal wall and facilitate the closure of large abdominal hernia defects and the placement of the mesh. However, no further contributions with this technique have been published since this initial report. The technique of PCS described by Novitsky in 2012 consists of the release of the transverse abdominis muscle (TAR) from its medial insertions to the posterior rectus sheath [13]. After this approach, a large retro-muscular and preperitoneal dissection can be reached in order to extend the mesh far enough to prevent hernia recurrence.
In order to make the dissection of TAR easier to perform and to obtain the correct plane between the peritoneum and the transversalis fascia we have suggested a modification of the technique. The aim of this study is to describe this surgical modification and our initial results.
Patients and methods
How TAR is usually performed
The original description starts the dissection as far cranially as possible in the upper abdominal wall, by incising the posterior lamina of the internal oblique aponeurosis [13]. Then, approximately 0,5 cm medial to the linea semilunaris, the transversus abdominis muscle fibers are cut from their attachments to the posterior rectus sheath and the linea alba. Cutting the muscle fibers opens the space between the peritoneum and the transverse abdominis muscle. Two layers may be then exposed to extend the preperitoneal dissection: the layer between the transversalis fascia and the muscle and the layer between the peritoneum and the transversalis fascia. The layer between the peritoneum and the fascia is especially difficult to obtain because there is no preperitoneal fat at this level. At that point, the dissection continues laterally and downwards. The preperitoneal and retroperitoneal space are developed as lateral as possible to extend the mesh [4].
How we perform down-to-up TAR:
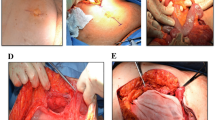
We describe a slight modification of TAR technique starting the dissection from the arcuate line in a down to up direction. We take the advantage of the preperitoneal fatty tissue distribution in the abdominal wall to prevent openings or tears in the peritoneum (Fig. 1). In this area, the preperitoneal fat can easily be detached from the posterior rectus sheath with blunt dissection, using the index finger placed under the arcuate line, extending the preperitoneal space dissection laterally and superiorly from the space of Bogros (the preperitoneal space lateral to the internal inguinal ring) (Fig. 2). Consequently, prior starting the incision on the posterior rectus sheath, medial to the semicircular line, the space between the preperitoneal fat and the transversalis fascia has already been made (Fig. 3) (videos 1-2). The posterior rectus sheath is then incised starting from the arcuate line 0.5–1 cm medial to the semicircular line to prevent injuries to the neuro-vascular bundles that come to innervate the rectus abdominis muscle. As soon as the posterior rectus sheath has been cut 4–5 cm, blunt preperitoneal dissection is continued laterally and cranially. Therefore, lateral and cranial blunt dissection is always made before the incision on the posterior rectus sheath. In this way, the risk of opening the peritoneum is minimized. The incision on the posterior rectus sheath is advanced cranially, reaching the area where the posterior lamina of the internal oblique aponeurosis becomes patent. At this level, the muscle fibers of the transversus abdominis muscle run under this lamina to the midline and need to be cut. We also maintain the same strategy from lateral to medial: the dissection is first performed lateral to cranial and, once completed, we begin the incision of the muscle fibers. We usually prefer to keep the dissection in the layer between the transversalis fascia and the muscle and between the diaphragmatic fascia and the diaphragm, as there is also a lack of preperitoneal fatty tissue at this level (area 2 in Fig. 1). Finally, a single plane behind the muscles will join a wide space over the fatty triangle, posterior rectus sheaths, the lateral preperitoneal fatty tissue and the space of Retzius. The extension of the blunt dissection may be performed to reach the central tendon of the diaphragm cranially, to the peripheral muscular part of the diaphragm more laterally, the quadratus lumborum and psoas muscle in the back and to the Retzius space caudally.
When the dissection comes superiorly from down to up, above the umbilicus, and reaches the posterior lamina of the internal oblique muscle, we can continue the incision obliquely, from lateral to medial, to get to the medial border of the posterior rectus sheath that has previously been released during the Rives procedure (Fig. 4) (video 3). As we do not keep parallel to the semicircular line, we change the direction of the incision of the posterior rectus sheath to avoid cutting muscular fibers of the transversus abdominis (line D, Fig. 3) (Fig. 5); only the insertion of the transversalis fascia on the posterior rectus sheath is incised. We have called this modification posterior rectus sheath (PRS) release. Therefore, we obtain the same retro-muscular preperitoneal dissection of TAR without cutting the muscle. Furthermore, once the posterior layer has been closed and the mesh extended in this wide preperitoneal plane, the border of the transversalis fascia and the transversus abdominis muscle can be easily sutured medially to the mesh obtaining a complete reconstruction of the abdominal wall (Fig. 6).
The next steps of the operation follow a conventional TAR technique. Briefly, once the retromuscular preperitoneal plane has been completed, the posterior rectus sheath is closed with running long-term absorbable sutures. If the restoration of the posterior layers is not possible, portions of the hernia sac or an absorbable mesh (BioA®, Gore, Arizona, USA) are used to protect the viscera from the synthetic mesh. Then, a large pore 50 × 50 cm polypropylene mesh (Bulevb®, Dipro Medical Devices SRL, Torinesse, Italy) is placed over the peritoneum and the posterior rectus sheaths fixed to both Cooper ligaments caudally, and to the upper insertion of the posterior rectus sheaths cranially. The anterior layer is then closed with interrupted or running long-term absorbable sutures. Low-suction drains are set between the mesh and the muscle layer. The excessive skin and redundant subcutaneous tissue are removed to complete the operation.
Patient selection
From a prospectively maintained database we have identified all patients who underwent TAR with down to up modification at our institution between 2012 and 2016. All patients presented complex incisional hernia according to Slater’s criteria [14].
Registered preoperative clinical data included age, sex, body mass index (BMI), American Society of Anesthesiologists grade, comorbidities (hypertension, diabetes, chronic obstructive pulmonary disease and cardiopathy), previous history of cancer and smoking. Hernia characteristics included location, EHS classification [15], Ventral Hernia Working group [16] classification, length in width of defect, Slater’s classification, and operation time. Postoperative variables comprised surgical site occurrences, overall systemic complications and length of hospitalization. Hernia recurrence, chronic pain and bulging were registered as the main outcomes during long-term follow-up.
The description of variables and the statistical analysis were performed using the Statistical Package for the Social Sciences (SPSS) program (version 19.0 for Windows). Quantitative variables were expressed as mean and standard deviation or median and range, and categorical variables as absolute numbers and percentages.
Results
We have operated 69 patients with down to up modification of TAR technique. 8 out of 69 underwent a PRS release. All patients were preoperatively studied with abdominal computed tomography, underwent preoperative antibiotic prophylaxis and were admitted on the ICU during the first 24 h postoperatively. In Table 1 we present a summary of perioperative data.
According to Slater’s classification, none of our patients were class 1, 27 patients were class 2 and 42 were class 3. Other classifications used are shown in Table 2. EHS classification was: M1-M3 midline, 4 patients; M1-M5 midline, 36; M3-M5 midline, 3; L1 lateral subcostal, 15; L3 lateral iliac, 7; and L4 lateral lumbar, 4. Ventral Hernia Working group classification was: 15 patients, stage I; 38, stage II; 13, stage III; and 3, stage IV. Table 3 presents postoperative data and long-term outcomes. Median follow-up was 19,7 (8–60) months.
Discussion
Different approaches have been used for abdominal incisional hernias. Anterior components separation provides a tension-free advancement of the lateral borders of the hernia defect and mobilizes the entire abdominal wall as a block [13]. In an attempt to solve the disadvantages associated to the technique, endoscopic or robotic component separation with laparoscopic fascial release have been described [17,18,19]. The Rives-Stoppa procedure is thought to be the gold-standard treatment for midline incisional hernias, however this technique is limited by the lateral borders of the posterior rectus sheath and may be inadequate for huge midline hernias and lateral hernias. The TAR technique, as an extension of the Rives-Stoppa procedure may be considered the necessary step to treat complex abdominal incisional hernias. This new tool offers the surgeon better possibilities to perform tension-free abdominal wall reconstruction for complex abdominal hernias [4, 11, 20,21,22]. Different reasons may be suggested as advantages over other hernioplasties in complex abdominal hernias and the most important would be minimizing wound complications, the access to the retroperitoneal space to overlap the defect as much as possible and the location of the mesh in a retromuscular preperitoneal position [4]. We have summarized the different posterior component separation techniques in Table 4.
The idea of releasing the transversus abdominis muscle is to access a wide space that goes from the preperitoneal fatty tissue in the midline to the psoas muscle and the retroperitoneal space laterally in order to extend the mesh as much as possible. The retrosternal space and the Conze’s fatty triangle area are reached proximally as well as the Retzius and the Bogros spaces caudally. In the down to up TAR, we achieve the same retromuscular preperitoneal space described in the original technique [4], but the access to the lateral retromuscular space is performed by dissecting the space between the peritoneum and posterior rectus sheath below the arcuate line. The anatomical reason to perform this down to up TAR is the preperitoneal fatty tissue distribution in the abdomen (Fig. 1). The distribution of this fatty tissue reminds the shape of a trident and prevents from openings or tears in the peritoneum. There is more preperitoneal areolar tissue just in the midline, under the linea alba, below the arcuate line and lateral to the semicircular line as far as the retroperitoneum. In the midline, we have the preperitoneal fat reinforced, superiorly, by the round ligament, and, inferiorly, by the fat that surrounds the urachus, the remaining of the umbilical arteries and the Retzius space. However, the preperitoneal fat is scarce just behind the posterior rectus sheaths, where the peritoneum is thin and attached to the transversalis fascia and this is why peritoneotomies can be so frequent (area 1 of Fig. 1). In cases of hernias in stoma sites or parastomal hernias, down to up access may also facilitate entering the preperitoneal space from caudally and then surround the ostomy cranially as in the classic TAR technique.
In an interesting radiological review in patients after TAR [23], there was a compensatory hypertrophy of oblique muscles that may compensate the observed atrophy of transversus abdominis muscles. In order to avoid the atrophy observed in the transversus abdominis after TAR, we advocate to make the posterior rectus sheath release. The PRS release modification allows accessing the retromuscular preperitoneal space without cutting the muscle fibers of the transversus abdominis muscle. We believe that this technique preserves the branches from the intercostal nerves that come to innervate the transversus abdominis that otherwise are cut during the conventional TAR (video 1). This way we can also reinsert the transversus abdominis to the new posterior rectus sheath/fascia transversalis made up of the mesh that has just placed in the retromuscular preperitoneal position (Fig. 6). Our experience is short to draw any relevant conclusion, but we believe that the PRS release may be especially important in young patients, patients with daily activity or patients who practice sports that may benefit from preserving the integrity of this muscle.
We have obtained similar results compared to previous TAR reports [22, 24]. Compared to the largest series published, we had more SSI, but in our series we have included more cases with grade III and IV VHWG classification. However, we think that the proposed approach is not going to influence postoperative outcomes as it only aims to facilitate the surgical technique to the surgeon.
Conclusion
Due to the paucity of preperitoneal fatty tissue in the upper part of the abdominal wall in contrast with the area below the arcuate line, the modification that we present may help the surgeon to perform the original TAR technique. Finally, this technique may also facilitate to perform a posterior component separation without cutting the muscle fibers of the transversus abdominis muscle and perform a complete reconstruction of the abdominal wall by reinserting this muscle to the mesh.
References
Heller L, McNichols CH, Ramirez OM (2012) Component separations. Semin Plast Surg 26(1):25–28. https://doi.org/10.1055/s-0032-1302462
Cornette B, De Bacquer D, Berrevoet F (2017) Component separation technique for giant incisional hernia: a systematic review. Am J Surg 10 [Epub ahead of print]. https://doi.org/10.1016/j.amjsurg.2017.07.032.
de Vries Reilingh TS, van Goor H, Rosman C, Bemelmans MH, de Jong D, van Nieuwenhoven EJ, van Engeland MI, Bleichrodt RP (2003) “Components separation technique” for the repair of large abdominal wall hernias. J Am Coll Surg 196(1):32–37. https://doi.org/10.1016/S1072-7515(02)01478-3
Gibreel W, MG Sarr MR, Novitsky Y (2016) Technical considerations in performing posterior component separation with transverse abdominis muscle release. Hernia 20(3):449–459. https://doi.org/10.1007/s10029-016-1473-y
Liang MK, Holihan JL, Itani K, Alawadi ZM, Flores Gonzalez JR, Askenasy EP, Ballecer C, Sen Chong H, Goldblatt MI, Greenberg JA, Harvin JA, Keith JN, Martindale RG, Orenstein S, Richmond B, Roth JS, Szotek P, Towfigh S, Tsuda S, Vaziri K, Berge DH (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265(1):80–89. https://doi.org/10.1097/SLA.0000000000001701
Holihan JL, Askenasy EP, Greenberg JA, Keith JN, Martindale RG, Roth JS, Mo J, Ko TC, Kao LS, Liang MK, the Ventral Hernia Outcome Collaboration Writing Group (2016) Component separation vs. bridged repair for large ventral hernias: a multi-institutional risk-adjusted comparison, systematic review, and meta-analysis. Surg Infect 17(1):17–26. https://doi.org/10.1089/sur.2015.124
Fox M, Cannon RM, Egger M, Spate K, Kehdy FJ (2013) Laparoscopic component separation reduces postoperative wound complications but does not alter recurrence rates in complex hernia repairs. Am J Surg 206(6):869–874. https://doi.org/10.1016/j.amjsurg.2013.08.005
Rives J, Pire JC, Flament JB, Polot JP (1987) Major incisional hernias. In: Chevrel JP (ed) Surgery of the abdominal wall. Springer-Verlag, New York, pp 116–144
Stoppa RE. The treatment of complicated groin and incisional hernias (1989) World JSurg 13(5):545–554.
CW Iqbal, TH Pham, A Joseph, J Mai, GB Thompson, MG Sarr (2007) Long-term outcome of 254 complex incisional hernia repairs using the modified rives-Stoppa technique World J Surg 31(12):2398–2404. doi: https://doi.org/10.1007/s00268-007-9260-7 .
EM Pauli , MJ Rosen. Open ventral hernia repair with component separation (2013) Surg Clin North Am 93(5):1111–1133. https://doi.org/10.1016/j.suc.2013.06.010 .
Carbonell AM, Cobb WS, Chen SM (2008) Posterior components separation during retromuscular hernia repair. Hernia 12(4):359–362. https://doi.org/10.1007/s10029-008-0356-2
YW Novitsky, HL Elliott, SB Orenstein, MJ Rosen (2012) Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204(5):709–716. doi: https://doi.org/10.1016/j.amjsurg.2012.02.008.
NJ Slater AM, Berrevoet F, AM Carbonell AC, Franklin M, Kercher W, BJ Lammers EP-D, Rolls S, Towfigh S, van Greffen E, Conze J, van Goor H (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18(1):7–17. https://doi.org/10.1007/s10029-013-1168-6
FE Muysoms, M Miserez, F Berrevoet, G Campanelli, GG Champault, E Chelala, UA Dietz, HH Eker, I El Nakadi, P Hauters, M Hidalgo Pascual, A Hoeferlin, U Klinge, A Montgomery, RK Simmermacher, MP Simons, M Smietański, C Sommeling, T Tollens, T Vierendeels, A Kingsnorth (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x .
Ventral Hernia Working Group, K Breuing, CE Butler, S Ferzoco, M Franz, CS Hultman, JF Kilbridge, M Rosen, RP Silverman, D Vargo (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148(3):544–558. https://doi.org/10.1016/j.surg.2010.01.008
SC Azoury, AP Dhanasopon, X Hui, SH Tuffaha, C De La Cruz, C Liao, M Lovins, HT Nguyen (2014) Endoscopic component separation for laparoscopic and open ventral hernia repair: a single institutional comparison of outcomes and review of the technique. Hernia18(5):637–645. https://doi.org/10.1007/s10029-014-1274-0 .
AM Carbonell, JA Warren, AS Prabhu, CD Ballecer, RJ Janczyk, J Herrera, LC Huang, S Phillips, MJ Rosen, BK Poulose (2017) Reducing length of stay using a robotic-assisted approach for retromuscular ventral hernia repair: a comparative analysis from the Americas hernia society quality collaborative. Ann Surg 27 [Epub ahead of print] https://doi.org/10.1097/SLA.0000000000002244.
P Patel, A Carbonell (2017) Laparoscopic and robotic incisional hernia repair. In: MA Garcia Ureña, J López Monclús, directors. Handbook of complex abdominal wall. Madrid (Spain): Grupo CTO Editorial. 49–57.
JH Ko, EC Wang, DM Salvay, Paul BC, Dumanian GA (2009) Abdominal Wall reconstruction lessons learned from 200 “components separation” procedures. Arch Surg 144(11):1047–1055. https://doi.org/10.1001/archsurg.2009.192.
DM Krpata , JA Blatnik, YW Novitsky, MJ Rosen (2012) Posterior and open anterior components separations: a comparative analysis. Am J Surg 203(3):318–322. https://doi.org/10.1016/j.amjsurg.2011.10.009 .
YW Novitsky , M Fayezizadeh, A Majumder, R Neupane, HL Elliott, SB Orenstein (2016) Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264(2):226–232. https://doi.org/10.1097/SLA.0000000000001673 .
De Silva GS, Krpata DM, Hicks CW, Criss CN, Gao Y, Rosen MJ, Novitsky YW (2014) Comparative radiographic analysis of changes in the abdominal wall musculature morphology after open posterior component separation or bridging laparoscopic ventral hernia repair. J Am Coll Surg 218(3):353–357. https://doi.org/10.1016/j.jamcollsurg.2013.11.014
Winder JS, Behar BJ, Juza RM, Potochny J, Pauli EM (2016) Transversus abdominis release for Abdominal Wall reconstruction: early experience with a novel technique. J Am Coll Surg 223(2):271–278. https://doi.org/10.1016/j.jamcollsurg.2016.04.012
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
- Alvaro Robin-Lersundi: received honorarium for Gore for organizing workshops on abdominal wall surgery.
- Miguel-Angel García-Ureña: received honorarium for Gore for organizing workshops on abdominal wall surgery and has been an invited speaker in symposium organized by B. Braun.
- Luis Blaquez Hernando: received honorarium for Gore for organizing workshops on abdominal wall surgery.
- Javier López-Monclús: received honorarium for Gore for organizing workshops on abdominal wall surgery.
- Arturo Cruz Cidoncha: declares no conflict of interest.
- Carlos San Miguel: declares no conflict of interest.
- Elena Jimenez Cubedo: declares no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
All procedures performed in this study with human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Robin-Lersundi, A., Blazquez Hernando, L., López-Monclús, J. et al. How we do it: down to up posterior components separation. Langenbecks Arch Surg 403, 539–546 (2018). https://doi.org/10.1007/s00423-018-1655-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1655-4