Abstract
Purpose
Major hepatic resections are performed for primary hepatobiliary malignancies, metastatic disease, and benign lesions. Patients with chronic liver disease, including cirrhosis and steatosis, are at an elevated risk of malnutrition and impaired strength and exercise capacity, deficits which cause increased risk of postoperative complications and mortality. The aims of this report are to discuss the pathophysiology of changes in nutrition, exercise capacity, and muscle strength in patient populations likely to require major hepatectomy, and review recommendations for preoperative evaluation and optimization.
Methods
Nutritional and functional impairment in preoperative hepatectomy patients, especially those with underlying liver disease, have a complex and multifactorial physiologic basis that is not completely understood.
Results
Recognition of malnutrition and compromised strength and exercise tolerance preoperatively can be difficult, but is critical in providing the opportunity to intervene prior to major hepatic resection and potentially improve postoperative outcomes. There is promising data on a variety of nutritional strategies to ensure adequate intake of calories, proteins, vitamins, and minerals in patients with cirrhosis and reduce liver size and degree of fatty infiltration in patients with hepatic steatosis. Emerging evidence supports structured exercise programs to improve exercise tolerance and counteract muscle wasting.
Conclusions
The importance of nutrition and functional status in patients indicated for major liver resection is apparent, and emerging evidence supports structured preoperative preparation programs involving nutritional intervention and exercise training. Further research is needed in this field to develop optimal protocols to evaluate and treat this heterogeneous cohort of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Importance of nutrition in major abdominal surgery
The importance of nutrition in all major surgery is now apparent, and it is accepted that assessment of nutritional status and intervention if indicated is essential in the pre- and postoperative periods [1]. More than 40% of surgical patients suffer from malnutrition [2] and there is a clear correlation between malnutrition and an increase in postoperative complications including morbidity, mortality, overall and surgical site infections, and increased length of [2,3,4,5,6,7]. The most recent set of European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines state that nutrition is critically important to recovery from major surgery, and patients at a high risk due to impaired nutritional status should ideally receive oral supplementation prior to major surgery, even if this results in the delay of resection of a malignancy [1]. Early consultation of a dietician may be indicated, and attempts should be made to provide preoperative nutritional therapy before hospital admission when feasible [1]. Oral nutrition intake is greatly preferable, and a study of patients with gastroesophageal, pancreatic, and colorectal cancers demonstrated a significant decrease in postoperative infections and length of hospital stay in patients who received 5 days of oral supplemental nutrition before surgery [8].
The primary goals of preoperative nutritional therapy should be to prevent the loss of lean body mass and provide adequate support for postoperative wound healing. There is also emerging data regarding the importance of immunomodulation in surgery particularly for malignancies to optimize long-term outcomes [4, 9, 10]. Many, but not all, recent studies support the use of immune-modulating nutritional supplementation including arginine and ω3 fatty acids in the perioperative period [4, 11].
It is important to acknowledge the increasing prevalence of obesity worldwide because of the unique nutritional risks. Obesity is a disease of macronutrient excess but is commonly associated with micronutrient deficiencies including thiamine and vitamin D [11,12,13] and decreased lean muscle mass [14]. In a recent study of 4652 people over the age of 60 in the USA, the prevalence of sarcopenic obesity was 18% in women and 43% in men [15]. There is a clear association of sarcopenic obesity with perioperative morbidity, and cancer patients with sarcopenic obesity have an elevated risk of chemotherapy toxicity and overall mortality [16]. These patients should be counseled regarding their increased perioperative risk, and ideally undergo modifications of diet and activity level before major surgery.
In conjunction with the recognition of the importance of longer term preoperative nutrition, the traditional practice of fasting after midnight prior to surgery has been challenged. A recent review of 38 randomized, controlled comparisons within 22 trials found no evidence to support the standard “nil by mouth from midnight” (NPO) preoperative fasting policy, and in fact suggested that consumption of water preoperatively resulted in decreased gastric volumes [17]. Particularly in the case of patients with underlying liver disease and its associated metabolic alterations, NPO time should be limited (except in cases of variceal bleeding or severe hepatic encephalopathy). This recommendation is in line with the ESPEN guidelines to allow intake of solid food until 6 h preoperatively and clear fluids until 2 h before anesthesia (Table 1) [1].
Unique nutritional considerations in hepatic resections
Introduction to nutrition and hepatic resection
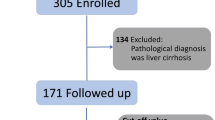
The increased understanding of the importance of nutritional status in all abdominal surgery is particularly relevant in the subset of patients who are indicated for liver surgery. Hepatic resection is indicated for a variety of benign and malignant diseases including hepatocellular carcinoma (HCC), cholangiocarcinoma, gallbladder carcinoma, rare primary hepatobiliary malignancies, metastases from colorectal cancer and other primary malignancies, and benign pathology [18]. Much of the literature on preoperative optimization for hepatic surgery focuses on patients with cirrhosis awaiting liver transplant, but these principles can be extrapolated to partial hepatic resections as well as other patient populations and surgical indications. Liver resection for living-liver donation for transplantation is another indication for major hepatectomy; however, this procedure is limited to exceptionally healthy individuals who tend to have normal preoperative nutritional and functional statuses [19].
The clinical success of a major hepatic resection depends on the ability of the remnant liver to regenerate via hyperplasia. The mortality of posthepatectomy liver failure is over 60% despite a decrease in posthepatectomy mortality rate to less than 5% in patients without underlying liver [20, 21]. Underlying liver pathology and systemic conditions including malnutrition affect the rate of regeneration following hepatectomy; therefore, nutritional evaluation is essential in determining the regeneration potential of the remaining liver and thus the safety of the resection [19]. A recent review noted malnutrition as a risk factor for postoperative liver failure following hepatic resection for all indications, likely due to a combination of immune impairment, decreased hepatic protein synthesis, and diminished ability of the liver to regenerate [5, 22, 23]. There is unique underlying pathophysiology and perioperative risk in patients with HCC in the setting of underlying cirrhosis compared to patients with malignancy associated with hepatic steatosis and these populations warrant separate discussion.
Resection of hepatocellular carcinoma in patients with cirrhosis
Prevalence of nutritional impairment
HCC is the second largest cause of cancer mortality worldwide and projected to rise from seventh to third great cause of cancer mortality in the USA over the next 15 years [24,25,26,27]. Mortality from HCC is increasing in the USA and Canada due to the high prevalence of hepatitis C and spread of nonalcoholic fatty liver disease [28]. Current guidelines [29, 30] recommend resection for BCLC stage A (single or up to three nodules ≤ 3 cm with Child-Pugh A-B and Performance Status 0). Recent reports from Asia have described a survival advantage associated with resection even in selected patients with advanced-stage tumors [31,32,33].
The most significant risk factor for HCC is cirrhosis [29] and malnutrition is found in 50–90% of patients with obstructive jaundice or moderate to severe cirrhosis [34,35,36,37]. It is one of the most important prognostic factors in end-stage liver disease overall [38] and associated with increased morbidity and mortality in the absence of major surgery [36, 39, 40]. Even in patients with CTP class A or B, the prevalence of malnutrition is as high as 25–46 and 84%, respectively [41, 42]. Protein depletion is more common in male patients for unclear reasons and in patients with alcoholic liver disease [43]. Malnutrition is even more relevant in patients with cirrhosis who require major hepatectomy due to the interplay between nutritional status, hepatic regeneration, and wound healing. Nutritional therapy for patients with liver disease undergoing hepatic and other abdominal surgeries has been proven to improve postoperative outcomes [22, 44].
Pathophysiology of nutritional deficiency
The etiology of malnutrition in patients with underlying liver disease is multifactorial. A hypermetabolic state (defined as a 120% increase in resting energy expenditure) is present in 4–34% of cirrhotic patients without association with gender, etiology, or severity of liver disease, hepatic malignancy, or presence of ascites [38, 43, 45, 46]. Cirrhosis causes hyperdynamic circulation via increased sympathetic nervous system activity, leading to systemic vasodilatation, expanded intravascular blood volume, and greater energy requirement. Complications of cirrhosis including spontaneous bacterial peritonitis, sepsis, and fever of unknown origin can also drive increases in metabolic demand and protein catabolism [34, 47].
Despite these elevated protein and calorie requirements, cirrhosis is often associated with an unintentional decrease in nutrient intake and impaired nutrition absorption and utilization. Loss of appetite can be related to alcohol-related anorexia [34], elevated cytokines tumor necrosis factor α and leptin [48], changes in ghrelin levels [34], and mechanically impaired gastric expansion due to ascites [49]. Patients with cirrhosis, particularly those with ascites, frequently report nausea, bloating, and abdominal discomfort contributing to decreased tolerance of oral intake [36, 50]. Sodium restriction required for control of peripheral edema and ascites may make the recommended diet unappealing [37]. Additionally, during hospitalizations, patients are frequently fasted in anticipation of procedures and, otherwise, do not have access to foods they find appealing [49]. Patients with cirrhosis are often placed on a low-protein diet to minimize the risk of hepatic encephalopathy, which further impairs nutritional status and wound healing potential following major surgery [49]. Protein loss in cirrhosis can result from other iatrogenic causes as well including repeat paracenteses for symptomatic relief of ascites, or due to blood loss from esophageal or gastric varices or intestinal ulcerations which may be occult [38, 47].
Portal hypertension and subsequent portosystemic shunting result in nutrients bypassing metabolic processing in the liver, impairing digestion and absorption [34, 49]. Related conditions including pancreatic insufficiency, mucosal congestion, and atrophy of small intestine villi can exacerbate the inadequate absorption and utilization of vitamin nutrients. Lactulose, a commonly prescribed disaccharide cathartic, is not absorbed in the small intestine but potentially alters the bacterial flora, and may affect absorptive capacity [47].
Perpetuating the consequences of nutrient malabsorption, cirrhosis causes intrinsic alterations in the liver’s capacity for glucose metabolism, protein synthesis, and glycogen storage. Hepatocytes are unable to store, synthesize, and metabolize glycogen, leading to a premature switch gluconeogenesis from fats and proteins after as little time as an overnight fast [47, 51, 52]. In patients with cirrhosis, serum insulin levels are higher in both fasted and post-prandial states which decreases peripheral glucose metabolism [36, 53]. Polyunsaturated fatty acid (PUFA) deficiency is seen in cirrhosis due to decreased hepatic synthesis from essential fatty acid precursors, although potential benefits of supplementation are unclear [37].
Branched-chain amino acids (BCAAs) leucine, isoleucine, and valine cannot be synthesized, must be obtained from the diet, and are predominantly metabolized by muscle. Patients with cirrhosis and decreased lean muscle mass have a deficiency of BCAAs, leading to amino acid imbalance and subsequent alteration of brain ammonia levels [54, 55]. Deficiencies of magnesium, sodium, phosphorus, and zinc also occur with liver disease, and due to iatrogenic causes like the use of diuretics [34, 38, 45]. Zinc deficiency perpetuates the damage by causing impaired appetite and taste, and altered protein metabolism [56]. Hundreds of metalloenzymes require zinc, including RNA and DNA polymerases, and zinc is sequestered in wounds, exacerbating any existing deficiency at the time of operation [5].
Cholestatic liver disease, seen in cirrhosis as well as extrahepatic cholangiocarcinomas, can cause impaired absorption of fat-soluble vitamins A, D, E, and K via abnormally low intraluminal bile salt concentrations [56]. Deficiencies of vitamins A and D are the most common, with 92% of cirrhotic patients having some degree of vitamin D deficiency and 29% having severe deficiency (< 17.5 nmol/L) [57]. Alcoholic cirrhosis is associated with water-soluble vitamin (B complex and C) and thiamine deficiency, but these deficiencies may be seen in other forms of chronic liver disease as well [37]. Vitamin C deficiency is particularly dangerous because it is essential to the function of proline and lysine hydroxylases in wound healing [5].
Although patients at the severe end of the spectrum of cirrhosis may not be operative candidates for resection of hepatic malignancies, it is clear from these data that even patients with less severe liver disease clinically are at a high risk of compromised nutrition and deficiencies in protein and other key contributors to postoperative wound healing.
Evaluation of nutritional status
While CTP score and MELD scores are helpful for quantifying the severity of liver disease, the assessment of nutritional status in patients before major hepatectomy can be challenging. The Subjective Global Assessment (SGA) uses data from clinical history and physical examination including recent weight loss, changes in oral intake, presence of gastrointestinal symptoms, functional capacity, signs of muscle wasting, presence of peripheral edema, and metabolic demands to categorize patients as well nourished, moderately malnourished, or severely malnourished [2, 58] and has been validated in chronic liver disease [59, 60].
The ESPEN guidelines [61] recommend combining SGA with anthropometric parameters including mid-arm muscle circumference (MAMC) or mid-arm circumference (MAC) and triceps skin fold thickness (TST) in all patients with liver cirrhosis or alcoholic steatosis. Malnutrition is diagnosed if MAMC/MAC or TST is below the 5th percentile in patients 18–74 years old or 10th percentile in patients over 74 years old [39]. Both SGA and the anthropometric parameters have the advantage of not being altered by the presence of ascites or peripheral edema [47]. For pretransplant or abdominal surgical patients, the ESPEN guidelines recommend the use of phase angle or body cell mass measured by bioelectric impedance to quantify malnutrition, although these measurements are less reliable in patients with ascites [45, 61, 62].
In terms of clinical scoring systems, the Prognostic Nutritional Index (PNI) stratifies patients based on the presence or absence of an inflammatory response as indicated by serum albumin level and lymphocyte count. A low PNI has been found to be an independent predictor of poor overall survival in patients with HCC, in general [63], and HCC patients who undergo surgical resection [64, 65]. Recognizing the importance of immune-nutritional status for survival in HCC, another study [66] proposed the use of the controlling nutritional status (CONUT) score, previously validated in patients undergoing resection of colorectal cancer [67], as a prognostic factor in HCC patients undergoing hepatectomy. The score is an assessment of degree of undernutrition based on albumin, total lymphocytes, and total cholesterol [68]. The high CONUT score group was found to have a lower 5-year recurrence-free survival and overall survival rate compared to the low CONUT score group, which remained significant in multivariate analysis. CONUT score was also found to correlate with prothrombin time, Child-Pugh score of A or B vs C, and stage of hepatic fibrosis [66]. The validation of this score in other populations of patients with malignancies makes it generalizable to all patients indicated for major hepatectomy [67].
BMI can be a reliable predictor of malnutrition if the cutoff values are adjusted for severity of ascites [39], and Lee 2016 [33] demonstrated that the combination of low BMI (< 25) and low total cholesterol (< 200 mg/dl) were predictive of significantly lower recurrence-free survival and overall survival in HCC patients following surgical resection. These data suggest that BMI, albumin level, lymphocyte count, and serum cholesterol level may have prognostic value in the preoperative assessment of major hepatectomy patients. Prior research demonstrated that a larger number of comorbid factors, advanced age, and presence of symptomatic liver cirrhosis significantly predicted 30-day postoperative mortality in multivariate analysis of a European population [69].
Recommendations for preoperative nutritional intervention
In HCC patients undergoing major hepatic resection with curative intent, nutritional optimization is crucial for surgical recovery and long-term survival [70]. In general, patients with cirrhosis should take in 35–40 kcal/kg per day including 1.2–1.6 g/kg of protein [38, 61], and low-grade hepatic encephalopathy (grades I and II) should not be an indication for protein restriction [61]. Because patients with cirrhosis go into a fasting state overnight (compared to the 3 days it takes healthy individuals to have the same metabolic responses), they should receive a late evening snack to avoid the onset of gluconeogenesis [51, 52, 71]. One randomized controlled trial demonstrated significant increase in total body protein at 3, 6, and 12 months with nighttime supplementary nutrition compared to equivalent daytime supplementation [72].
Despite the 40–50% frequency of comorbid diabetes mellitus in patients with end-stage liver disease, carbohydrate intake should not be restricted, and carbohydrates should be included in 4–7 daily meals [47, 73]. On the contrary, increased fat intake in the setting of abnormally low release of hepatic VLDL can increase fat storage and exacerbate hepatic inflammation and fibrogenesis [47]. Vitamin supplementation is not routinely recommended, but is clearly indicated in the setting of a symptomatic deficiency, and if there is any suspicion for subclinical vitamin C or D deficiency [5, 47]. Patients with alcoholic cirrhosis are at an increased risk of pancreatic insufficiency, and supplemental pancreatic enzymes should be provided [37].
Patients who cannot meet their caloric and protein goals may benefit from preoperative supplementary enteral feeding, often with an increased protein or concentrated high energy formula [47, 61]. Hemorrhage from esophageal or gastric varices due to nasogastric tube placement is a concern, but overall, the nutritional benefits outweigh the risks [37]. In rare circumstances, patients with recurrent aspiration events, uncontrolled emesis, or diarrhea may be considered for parenteral nutrition but this should not be given routinely due to the associated risks of fluid overload and sepsis, and loss of the intestinal mucosal benefits of enteral feeding [47].
Supplementation with the oral branched-chain amino acids (BCAAs) leucine, isoleucine, and valine has been recommended in for patients with hepatic encephalopathy and intolerance of enteral feeding despite treatment [37, 61], although a recent review failed to demonstrate a change in mortality, quality of life, or nutritional parameters [74]. Excitingly, new data shows oral supplementation with BCAAs before treatment improves liver function after radiofrequency ablation [75, 76] and transcatheter arterial chemoembolization [77]. In a randomized prospective study, BCAA supplementation reduced early recurrence after hepatectomy for HCC although there was no difference in overall survival in this study [78].
One recent clinical trial on immunonutrition hepatic surgery divided 26 patients into two groups: one was given IMPACT, containing ω3 fatty acids, arginine, and nucleic acids, and half-portion hospital meals and compared to a group of patients who received normal hospital meals. The immunonutrition patients had significantly lower inflammation markers including white blood cells and interleukin-6, and slightly lower aspartate aminotransferase and alanine aminotransferase level, without a difference in complications or length of stay [79]. This was the first study on immunonutrition specifically in patients undergoing surgery for hepatic malignancies and proves that immunonutrition in this population warrants further investigation.
Another emerging topic in surgical nutrition is the use of synbiotics, and initial results in liver transplant patients showed promising results with synbiotics reducing the rate of postoperative complications compared to patients who underwent selective bowel decontamination [80] or fiber only [81]. These results were replicated in 61 patients with cirrhosis undergoing liver resection who received symbiotic supplementation for 14 days preoperatively and 11 days postoperatively and demonstrated a reduced rate of infectious complications and a negative correlation with levels of serum interleukin-6 and C-reactive protein [82]. The formula used in this study was a combination previously shown to reduce postoperative infections in biliary cancer surgery patients [83, 84]: probiotics Bifidobacterium breve strain Yakult and Lactobacillus casei strain Shirota with prebiotic galactooligosaccharides. Synbiotics are an exciting area of emerging research in surgical nutrition and are recommended in the perioperative period for patients with nutritional impairment undergoing major cancer surgery [1].
Enteral nutritional support in the postoperative period
Despite the most meticulous attention to preoperative nutritional status and attempts at supplementation, the reality is that the vast majority of patients with cirrhosis who undergo liver resections experience some degree of postoperative hepatic decompensation, usually associated with hyperbilirubinemia and ascites. While an extensive discussion of postoperative nutrition is beyond the scope of this review, the importance of enteral nutrition in these patients must be emphasized. Total parenteral nutrition (TPN) is well known to be associated with metabolic and infectious complications in a population already at elevated risk of these issues. A recent systematic review identified five randomized prospective trials on enteral versus parenteral nutrition following hepatectomy and found that enteral nutrition associated fewer wound infections and catheter-related complications than parenteral nutrition [85]. For these reasons, Dobhoff feeding tube placement should be performed at the time of surgery, and tube feeding initiated within 24 h of surgery per the ESPEN guidelines in patients who are anticipated to have inadequate oral intake for at least 7 days following surgery or are unable to consume or unsafe for oral nutrition [1]. Surgical feeding access, including gastrostomy and jejunostomy tubes, can be fraught with ascitic leaks and should be avoided in this population unless absolutely necessary. As stated previously, perioperative symbiotic supplementation decreased infectious complications in this patient population and should be considered in the postoperative period [82].
Resection of metastatic disease
In North American and European populations, metastatic disease, most commonly colorectal cancer, is the most common indication for hepatectomy [18]. Colorectal cancer is the second most common cause of cancer-related death in these regions [86], and approximately half of colorectal cancer patients develop liver metastases for which hepatectomy is the optimum treatment. As expected, the threat of postoperative liver failure in this population is low (approximately 10%); however, when it occurs, it contributes dramatically to postoperative mortality rate [87].
There may be no clinical evidence of liver dysfunction in patients with metastatic disease, but preoperative assessment of nutritional and functional status remains important in the setting of advances in knowledge about nutritional status in hepatectomy [23, 69] and abdominal surgical outcomes in general. In patients with cirrhosis, functional reserve of the liver has been a useful predictor of postoperative outcomes; however, in patients with metastatic disease in an otherwise healthy liver, hepatic reserve does not predict postoperative morbidity or mortality [69]. One study found that 38% of patients with advanced colorectal cancer have severe nutritional compromise, as identified by a patient-generated global assessment score (PGSGA) of ≥ 9 [88]. The SGA is useful for patients who require hepatectomy for metastatic or benign disease as well.
Steatosis due to obesity and chemotherapy
Patients at risk for hepatic steatosis due to obesity or preoperative chemotherapy warrant particular attention due to the associated increase in rate of postoperative complications. Hepatic steatosis is an accumulation of lipids within the liver due to obesity, alcohol use, diabetes mellitus, and other toxins, and is pathologic when the hepatic fat content is greater than 5% of the liver wet weight [21]. The most severe form is steatohepatitis in which the liver demonstrates fat infiltration, lobular inflammation, and ballooning hepatocytes progressing to fibrosis, likely via increased oxidative stress and peroxidation of lipids [21, 89]. Approximately 20–40% of the people in western countries are affected by hepatic steatosis with even greater prevalence (30–50%) in patients undergoing hepatic resection for metastatic disease [90, 91]. Both steatosis and steatohepatitis are proportional to BMI [90, 92] in surgical populations; however, 10–20% of lean patients suffer from steatosis [21].
Steatosis and particularly steatohepatitis have the potential to increase the risk of complications and mortality in major hepatectomy via multiple mechanisms [21, 93,94,95,96]. Ischemia/reperfusion injury is the major cause of damage to the remaining hepatic parenchyma during liver resection. Data from animal studies suggests that steatosis decreased total and microcirculatory blood blow, decreasing total reperfusion and leading to ongoing chronic hypoxia. This contributes to imbalances of energy homeostasis and Kupffer cell dysfunction causing an intensified inflammatory response and increased damage to hepatocytes. Additionally, steatosis impairs hepatic regeneration, likely via disturbances of cell cycle progression, and is associated with insulin resistance, which may be associated with an increased risk of postoperative wound infections [21].
Histopathologic analysis of multiple liver biopsies is the gold standard for diagnosing steatosis. There is data that computed tomography and ultrasound imaging can be used for diagnosis and monitoring of steatosis-induced hepatomegaly [97, 98]; however, there is clearly a need for more sensitive noninvasive diagnostic techniques to evaluate patients preoperatively.
Particularly relevant to patients with metastatic liver disease is the inconsistent evidence that chemotherapy may cause steatosis and steatohepatitis and adversely affect postoperative outcomes of hepatic resection. In the literature regarding colorectal cancer metastatic to the liver, there are conflicting results with regard to the type and duration of chemotherapy and associated liver injury and postoperative outcomes. One report found an association of steatohepatitis with BMI, but not with chemotherapy, although hepatic vascular injury patterns were significantly associated with oxaliplatin regimens without a change in morbidity [99]. On the contrary, another study demonstrated that ≥ 6 cycles of oxaliplatin-based chemotherapy increased the rate of hepatic sinusoidal injury, leading to decrease in functional hepatic reserve and elevated complication rate [100]. This was supported by a report demonstrating an association of oxaliplatin with sinusoidal dilation and irinotecan with steatohepatitis compared with no chemotherapy. In this group, patients with steatohepatitis were at an elevated risk of 90-day mortality [101]. Another report found a significantly elevated risk of steatosis (> 30%) with irinotecan chemotherapy compared to no chemotherapy, 5-fluorouracil, or oxaliplatin without a difference in short-term mortality [102]. A more recent study corroborated these results, noting that irinotecan chemotherapy, elevated BMI, and diabetes mellitus were associated with steatosis and steatohepatitis but chemotherapy did not increase the risk of liver-related complications [103].
Additional research has demonstrated a difference in elevated rate of steatosis in patients who received preoperative chemotherapy of any type compared to patients who did not receive chemotherapy, but this did not result in a difference in short-term clinical outcomes [104], or no differences in outcomes or presence of steatosis in patients who were treated with preoperative chemotherapy [105]. Additional investigations found a higher incidence of morbidity [106, 107] including postoperative liver failure [87] in patients who received preoperative chemotherapy in correlation with the number of cycles but not the type of chemotherapy [106]. Until there is a more definitive consensus in the literature, decisions regarding neoadjuvant therapy in this patient population should be made based on multidisciplinary consultation and attention to individual patient risks of steatosis, balanced with the fact that liver resection is usually the only option for definitive cure in these patients [108].
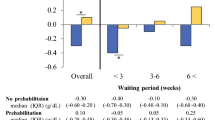
Recommendations for the treatment of obesity-related steatosis
Given the modern prevalence of obesity and recent advances in understanding the relationship between obesity, steatosis, and underlying metabolic derangements [12], obese patients in particular warrant nutritional evaluation and optimization. An early study from Japan on obesity-related hepatic steatosis demonstrated a significant reduction in mean liver volume after 3 months on a low-calorie diet [97], supporting the reversible nature of this disease [109]. Another study using ultrasound for assessment of liver size demonstrated a significant decrease in hepatomegaly following 2 weeks on a very low-calorie diet in 50 morbidly obese patients indicated for bariatric surgery, although degree of steatosis was not assessed directly [98]. In a more recent report of 111 patients undergoing major hepatic resection, just 1 week of dietary calorie and fat restriction was associated with decreased hepatic steatosis, a reduction in steatohepatitis, and decreased postoperative blood loss [90]. These exciting results indicate that even short-term preoperative dietary modifications can have a clinically significant impact on outcomes. Further investigation in dietary intervention to reduce steatosis in at-risk populations is warranted and has the potential to decrease postoperative complications and improve outcomes for these patients.
Physical condition
Compromised exercise capacity in patients with cirrhosis
Introduction and pathophysiology of impairment
The interplay between nutritional and functional status is complex, particularly in patients with malignancies or other underlying chronic diseases. Cirrhosis is clearly associated with increased fatigue and muscle wasting [110], and physical fitness has been shown to affect outcomes of liver transplant and survival in patients with cirrhosis. The term “physical fitness” includes the physiologic parameters of body composition, muscle strength, flexibility, and exercise capacity, which is the ability to consume and utilize oxygen during aerobic exercise [110]. The standard measurement of exercise capacity is maximal oxygen consumption (VO2max) which is obtained by quantifying oxygen content of expired air during an exercise test to exhaustion [110]. Muscle strength, essential for independent functioning and recovery from major surgery, naturally declines with age. It can be measured by knee flexion and extension and grip strength, although the values obtained can vary with gender, age, height, and weight [111].
A recent review evaluated 11 studies on the exercise capacity of patients with cirrhosis without other significant comorbidities, and all reports found decreased exercise capacity compared to healthy controls or predicted values [110]. Severity of liver disease as quantified by CTP score was found to have a negative correlation with VO2peak in some reports [112,113,114,115] but not others [116, 117]. Exercise capacity has been shown to correlate with mortality in patient with cirrhosis both without liver transplant and postoperatively following transplant [118, 119].
Four reports have examined muscle strength in patients with cirrhosis without additional medical problems, and two found diminished strength compared to healthy [115, 117, 120, 121]. Interestingly, in the two studies that stratified patient by CTP scores, no difference was found [117, 120], suggesting that sarcopenia may depend more on overall nutritional status than hepatic function in isolation. Muscle wasting is associated with mortality in pretransplant cirrhotic patients, independent of hepatic function [122].
The complications of cirrhosis, including hepatopulmonary syndrome, portopulmonary hypertension, ascites, and peripheral edema, affect exercise tolerance and pulmonary function as well as digestion and metabolism [110]. Cirrhotic cardiomyopathy occurs via impaired beta-adrenergic receptor signaling and alterations in cardiomyocyte membrane lipid composition and ion channels [123] and impairs the ability of the heart to increase cardiac output in response to exercise or other physiologic stress despite a baseline hyperdynamic circulatory system. In the setting of these circulatory changes, patients have an even more difficult time compensating for the anemia that can occur in cirrhosis in relation to malnutrition, alcohol abuse, and variceal hemorrhage. The prescription of beta-blockers for either prevention of variceal bleeding or comorbid cardiovascular indications can further blunt the cardiac response to anemia. Perturbations of pulmonary gas exchange can also decrease exercise capacity in cirrhosis through a variety of mechanisms. Cirrhosis can be associated with comorbid cardiopulmonary disease, basilar atelectasis, and pleural effusions, or hypoxemia can occur due to intrapulmonary shunts in hepatopulmonary syndrome, ventilation-perfusion mismatch, and diffusion-perfusion deficiency [113].
Ability to generate energy from nutrients is essential for exercise tolerance, and the alternations in carbohydrate metabolism described in cirrhosis contribute to impaired exercise capacity [113]. In another metabolic correlate, sarcopenia is common as the hepatic metabolism of glucose and protein changes with ongoing liver damage. Diminished muscle mass as well as a decrease in the ability of skeletal muscles to extract and consume oxygen is seen in cirrhosis [116], and muscle cramps are one of the most bothersome symptoms in patients with cirrhosis [50].
Evaluation of exercise capacity
The majority of research on exercise capacity and strength in liver surgery patients comes from the liver transplant population. These patients are often at the most severe end of the spectrum of liver disease and functional impairment, but consideration should be given to evaluating these parameters in all patients undergoing major hepatectomies. Measurement of VO2 is ideal and has an independent association with survival in liver transplant [118, 119]; however, the inexpensive and simple 6-min walk distance test has been shown to be predictive of mortality in patients on the liver transplant waiting list as well [113, 124]. In one study, exercise capacity also demonstrated a significant relationship with duration of posttransplant hospital stay, a finding that should be explored in major hepatectomy patients [118].
There is limited data that handgrip strength correlates with exercise capacity [118] but more research is needed to confirm this association. In one study, handgrip strength was shown to be an independent predictor of complications in patients with cirrhosis [35]. A recent prospective study advocates for the use of a combination of body mass index and thigh muscle thickness measured by ultrasound to diagnose sarcopenia while avoiding costly cross-sectional imaging [125], a technique that would be easy to use preoperatively.
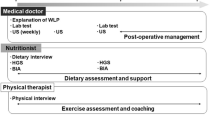
Recommendations for preoperative physical rehabilitation
There are possibilities for preoperative fitness interventions to improve hepatectomy outcomes, and two pilot studies in patients awaiting liver transplantation have demonstrated promising results for exercise training programs. Zenith et al. [126] found that weight weeks of supervised aerobic exercise training in a population of patients with CTP class A and B cirrhosis decreased fatigue while increasing peak VO2 and muscle mass without adverse effects. Debette-Gratien et al. [127] showed that a personalized 12-week adapted physical activity program in pretransplant patients improved peak VO2, knee extensor strength, and 6-min walk distance performance while also improving quality of life without complications. Caution must be used in study design and implementation of exercise programs because aerobic exercise has been found to increase hepatic venous pressure gradient, with a 16% pressure increase at 30% of peak workload and 31% pressure increase at 50% of peak workload [128]. This increase can be avoided by premedication with non-selective beta-blockers [129]. In patients with benign hepatic disease and metastatic lesions but otherwise normal liver, this would obviously be less of a concern.
Importance of physical condition in patients with metastatic disease
Physical prehabilitation programs have been studied in cardiac surgery [130], lung resection [131], and bariatric surgery [132] with promising results, but there is limited data on outcomes in patients undergoing surgery for primary or metastatic malignancies. One review of nine studies including five on colorectal cancer, two on bladder cancer, one involving liver resections, and one including abdominal oncological procedures in general found a lack of standardization of programs and outcome measures without significant differences overall in the prehabilitation groups compared to controls [133]. The report on hepatic resection involved a 4-week program of high-intensity cycling sessions, and found improved oxygen uptake and quality of life in the exercise group compared to a control group although compliance with the program, functional capacity, and postoperative complications were not addressed [134].
In a study of colorectal surgery patients who underwent mean 5.4 weeks of prehabilitation with either bike and strengthening exercises or walking and breathing exercises, one third of patients were able to improve their physical function as measured by the 6-min walk distance, and the patients who improved reported improved mental heal and self-perceived health as well [135]. Recognizing the potential impact of these interventions, a large prospective cohort study on cardiopulmonary exercise testing before non-cardiac surgery is currently underway at multiple international locations [136]. While more research is needed, there is potential for a pre-hepatectomy exercise program to improve aerobic capacity and thus mortality, as well as mental health parameters.
Conclusion
Clinical research in nutrition and preoperative preparation has been limited; however, a variety of clinical studies indicate that both patients with primary and metastatic liver disease are vulnerable to nutritional and physical compromise. On the basis of the best available evidence, patients indicated for elective hepatectomy should undergo preoperative nutritional optimization with the use of a short-term high-protein supplement diet. There is also evidence to suggest benefit from an immune supporting blend of amino acids. Selected cirrhotic patients undergoing resection will benefit from intensive postoperative nutritional support, often requiring feeding tube. For patients with steatosis, the optimal preoperative dietary regimen has not been defined; however, it is clear that steatosis is to some degree reversible. These findings lead these authors to routinely utilize 2 to 3 weeks of a calorie-restricted, low-carbohydrate, high-protein diet before surgery. In addition to preventing wound healing and infectious complications and improving patients’ quality of life, nutritional and physical optimization during the perioperative period may be associated with improved oncologic outcomes [9, 10]. Even in the modern era, major hepatectomy carries risk of morbidity and mortality, and all patients who are indicated for liver resection should have a thorough evaluation of nutritional and functional status to provide the opportunity to intervene if indicated.
References
Weinmann A, Braga M, Carli F, Higashiguchi T et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nut 36(3):623–650. https://doi.org/10.1016/j.clnu.2017.02.013
Sungurtekin H, Sungurtekin U, Balci C, Zencir M, Erdem E (2004) The influence of nutritional status on complications after major intraaabdominal surgery. J Am Coll Nutr 23(3):227–232. https://doi.org/10.1080/07315724.2004.10719365
Dempsey DT, Mullen J, Buzby GP (1988) The link between nutritional status and clinical outcome: can nutritional intervention modify it? Am J Clin Nutr 47(2 Suppl):352–356
Evans DC, Martindale R, Kiraly LN, Jones CM (2013) Nutrition optimization prior to surgery. Nutr Clin Pract 29(1):10–21. https://doi.org/10.1177/0884533613517006
Bozzetti F (2002) Rationale and indications for preoperative feeding of malnourished surgical cancer patients. Nutrition 18(11/12):953–959. https://doi.org/10.1016/S0899-9007(02)00988-7
Gallagher-Allred CR, Voss A, Finn SC, McCamish MA (1996) Malnutrition and clinical outcomes: the case for medical nutrition therapy. J Am Diet Assoc 96(4):361–366. https://doi.org/10.1016/S0002-8223(96)00099-5
Pichard C, Kyle U, Morabia A, Perrier A, Vermeulen B, Unger P (2004) Nutritional assessment: lean body mass depletion at hospital admission is associated with an increased length of stay. Am J Clin Nutr 79(4):613–618
Gianotti L, Braga M, Nespoli L et al (2002) A randomized controlled trial of preoperative oral supplementation with a specialized diet in patients with gastrointestinal cancer. Gastroenterology 122(7):1763–1770. https://doi.org/10.1053/gast.2002.33587
Gustafsson UO, Oppelstrup H, Thorell A et al (2016) Adherence to the ERAS protocol is associated with 5-year survival after colorectal surgery: a retrospective cohort study. World J Surg 40(7):1741–1747. https://doi.org/10.1007/s00268-016-3460-y
Horowitz M, Neeman E, Sharon E (2015) Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat Rev Clin Oncol 12(4):213–226. https://doi.org/10.1038/nrclinonc.2014.224
Toh SY, Zarshenas N, Jorgensen J (2009) Prevalence of nutrient deficiencies in bariatric patients. Nutrition 25(11-12):1150–1156. https://doi.org/10.1016/j.nut.2009.03.012
Wells JCK (2013) Obesity as malnutrition: the dimensions beyond energy balance. Eur J Clin Nut 67(5):507–512. https://doi.org/10.1038/ejcn.2013.31
Kerns JC, Arundel C, Chawla LS (2015) Thiamin deficiency in people with obesity. Adv Nutr 6(2):147–153. https://doi.org/10.3945/an.114.007526
Prado CM, Cushen S, Orsso CE, Ryan AM (2016) Sarcopenia and cachexia in the era of obesity: clinical and nutritional impact. Proc Nutr Soc 75(02):188–198. https://doi.org/10.1017/S0029665115004279
Batsis JA, Mackenzie T, Lopez-Jimenez F, Bartels SJ (2014) Sarcopenia, sarcopenic obesity and mortality in older adults: results from the National Health and Nutrition Examination Survey III. Eur J Clin Nut 68(9):1001–1007. https://doi.org/10.1038/ejcn.2014.117
Tsai S (2012) Importance of lean body mass in the oncologic patient. Nutr Clin Pract 27(5):593–598. https://doi.org/10.1177/0884533612457949
Brady MC, Kinn S, Stuart P, Ness V (2003) Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev 4. https://doi.org/10.1002/14651858.CD004423
Reddy SK, Barbas A, Turley RS et al (2011) A standard definition of major hepatectomy: resection of four or more liver segments. HPB 13(7):494–502. https://doi.org/10.1111/j.1477-2574.2011.00330.x
Ciuni R, Biondi A, Grosso G (2011) Nutritional aspects in patient undergoing liver resection. Updat Surg 63(4):249–252. https://doi.org/10.1007/s13304-011-0121-4
Redaelli CA, Wagner M, Krähenbühl L, Gloor B, Schilling MK, Dufour JF, Büchler MW (2002) Liver surgery in the era of tissue-preserving resections: early and late outcome in patients with primary and secondary hepatic tumors. World J Surg 26(9):1126–1132. https://doi.org/10.1007/s00268-002-6321-9
Veteläinen R, van Vliet A, Gouma DJ, van Gulik TM (2007) Steatosis as a risk factor in liver surgery. Ann Surg 245(1):20–30. https://doi.org/10.1097/01.sla.0000225113.88433.cf
Fan ST, Lo C, Lai ECS et al (1994) Perioperative nutritional support in patients undergoing hepatectomy for hepatocellular carcinoma. N Engl J Med 331(23):1300–1306. https://doi.org/10.1056/NEJM199412083312303
Van den Broek MAJ, Olde Damink S, Dejong CHC et al (2008) Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int 28(6):767–780. https://doi.org/10.1111/j.1478-3231.2008.01777.x
Altekruse SF, Henley S, Cucinelli et al (2014) Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol 109(4):542–553. https://doi.org/10.1038/ajg.2014.11
Rahib L, Smith B, Aizenberg R, Rosenweig AB, Fleshman JM, Matrisian LM (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74(11):2913–2921. https://doi.org/10.1158/0008-5472.CAN-14-0155
Tang A, Hallouch O, Chernyak V et al (2017) Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol. https://doi.org/10.1007/s00261-017-1209-1
White DL, Thrift A, Kanwal F et al (2017) Incidence of hepatocellular carcinoma in all 50 United States from 2000-2012. Gastroenterology 152(4):812–820. https://doi.org/10.1053/j.gastro.2016.11.020
El-Serag HB, Davila J, Petersen NJ et al (2003) The continuing increase in the incidence of hepatocellular carcinoma. Ann Intern Med 139(10):817–823. https://doi.org/10.7326/0003-4819-139-10-200311180-00009
Bruix J, Reig M, Sherman M (2016) Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma. Gastroenterology 150(4):835–853. https://doi.org/10.1053/j.gastro.2015.12.041
Vitale A, Saracino E, Boccagni P et al (2009) Validation of the BCLC prognostic system in surgical hepatocellular cancer patients. Transpl Proc 41(4):1260–1263. https://doi.org/10.1016/j.transproceed.2009.03.054
Katagiri S, Yamamoto M (2014) Multidisciplinary treatments for hepatocellular carcinoma with major portal vein tumor thrombus. Surg Today 44(2):219–226. https://doi.org/10.1007/s00595-013-0585-6
Kokudo T, Hasegawa K, Matsuyama Y et al (2016) Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol 65(5):938–943. https://doi.org/10.1016/j.jhep.2016.05.044
Lee JM, Jang B, Lee YJ et al (2016) Survival outcomes of hepatic resection compared with transarterial chemoembolization or Sorafenib for hepatocellular carcinoma with portal vein tumor thrombosis. Clin Mol Hepatol 22(16):160–167. 10.18632/oncotarget.8312
Cheung K, Lee S, Raman M (2012) Prevalence and mechanisms of malnutrition in patients with advanced liver disease, and nutrition management strategies. Clin Gastroenterol Hepatol 10(2):117–125. https://doi.org/10.1016/j.cgh.2011.08.016
Huisman EJ, Trip E, Siersema PD et al (2011) Protein energy malnutrition predicts complications in liver cirrhosis. Eur J Gastroenterol Hepatol 23(11):982–989. https://doi.org/10.1097/MEG.0b013e32834aa4bb
Kalaitzakis E, Simrén M, Olsson R et al (2006) Gastrointestinal symptoms in patients with liver cirrhosis: associations with nutritional status and health-related quality of life. Scand J Gastroenterol 41(12):1464–1472. https://doi.org/10.1080/00365520600825117
O’Brien A, Williams R (2008) Nutrition in end-stage liver disease: principles and practice. Gastroenterology 134:1729–1740. https://doi.org/10.1053/j.gastro.2008.02.001
Kondrup J (2006) Nutrition in end stage liver disease. Best Pract Res Clin Gastroenterol 20(3):547–560. https://doi.org/10.1016/j.bpg.2006.02.001
Campillo B, Richardet J, Bories PN (2005) Enteral nutrition in severely malnourished and anorectic cirrhotic patients in clinical practice: benefit and prognostic factors. Gastroenterol Clin Biol 29(6-7):645–651. https://doi.org/10.1016/S0399-8320(05)82150-5
Gunsar F, Raimondo M, Jones S et al (2006) Nutritional status and prognosis in cirrhotic patients. Aliment Pharmacol Ther 24(4):563–572. https://doi.org/10.1111/j.1365-2036.2006.03003.x
Carvalho L, Parise E (2006) Evaluation of nutritional status of nonhospitalized patients with liver cirrhosis. Arq Gasteroenterol 43(4):269–274. https://doi.org/10.1590/S0004-28032006000400005
Guglielmi FW, Panella C, Buda A et al (2006) Nutritional state and energy balance in cirrhotic patients with or without hypermetabolism: multicentre prospective study by the ‘Nutritional Problems in Gastroenterology’ Section of the Italian Society of Gastroenterology (SIGE). Dig Liver Dis 37(9):681–688. https://doi.org/10.1016/j.dld.2005.03.010
Peng S, Plank L, McCall JL et al (2007) Body composition, muscle function, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr 85(5):1257–1266
Merli M, Nicolini G, Angeloni S et al (2002) Malnutrition is a risk factor in cirrhotic patients undergoing surgery. Nutrition 18(11-12):978–986. https://doi.org/10.1016/S0899-9007(02)00984-X
Muller MJ, Böttcher J, Selberg O (1999) Hypermetabolism in clinically stable patients with liver cirrhosis. Am J Clin Nutr 69(6):1194–1201
Riggio O, Angeloni S, Ciuffa L et al (2003) Malnutrition is not related to alterations in energy balance in patients with stable liver cirrhosis. Clin Nut 22(6):553–559. https://doi.org/10.1016/S0261-5614(03)00058-X
Tsiaousi ET, Hatzitolios A, Trygonis SK et al (2008) Malnutrition in end stage liver disease: recommendations and nutritional support. J Gastroenterol Hepatol 23(4):527–533. https://doi.org/10.1111/j.1440-1746.2008.05369.x
Le Moine O, Marchant A, Groote DD et al (1995) Role of defective monocyte interleukin-10 release in tumor necrosis factor-alpha overproduction in alcoholic cirrhosis. Hepatology 22(5):1436–1439. https://doi.org/10.1002/hep.1840220516
Plauth M, Schütz E (2002) Cachexia in liver cirrhosis. Int J Cardiol 85(1):83–87. https://doi.org/10.1016/S0167-5273(02)00236-X
Marchesini G, Bianchi G, Amodio et al (2001) Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology 120(1):170–178. https://doi.org/10.1053/gast.2001.21193
Owen OE, Reichle F, Mozzoli MA et al (1981) Hepatic, gut, and renal substrate flux rates in patients with hepatic cirrhosis. J Clin Invest 68(1):240–252. https://doi.org/10.1172/JCI110240
Owen OE, Trapp V, Reichard GA Jr et al (1983) Nature and quantity of fuels consumed in patients with alcoholic cirrhosis. J Clin Invest 72(5):1821–1832. https://doi.org/10.1172/JCI111142
Merli M, Leonetti F, Riggio O et al (1999) Glucose intolerance and insulin resistance in cirrhosis are normalized after liver transplantation. Hepatology 30(3):649–654. https://doi.org/10.1002/hep.510300306
Khanna S, Gopalan S (2007) Role of branched-chain amino acids in liver disease: the evidence for and against. Curr Opin Clin Nut Metab Care 10(3):297–303. https://doi.org/10.1097/MCO.0b013e3280d646b8
Mardini HA, Douglass A, Record C (2006) Amino acid challenge in patients with cirrhosis and control subjects: ammonia, plasma amino acid, and EEG changes. Metab Brain Dis 21(1):1–10. https://doi.org/10.1007/s11011-006-9006-5
Moscateillo SM, Marchesini G (2007) Diabetes and liver disease: an ominous association. Nutr Metab Cardiovasc Dis 17(1):63–70. https://doi.org/10.1016/j.numecd.2006.08.004
Areth J, Narra S, Nair S (2010) Prevalence of vitamin D deficiency in chronic liver disease. Dig Dis Sci 55(9):2624–2628. https://doi.org/10.1007/s10620-009-1069-9
Detsky AS, McLaughlin J, Baker JP et al (1987) What is subjective global assessment of nutritional status? J Parenter Enter Nutr 11(1):8–13. https://doi.org/10.1177/014860718701100108
Henkel AS, Buchman A (2006) Nutritional support in patients with chronic liver disease. Nat Clin Pract Gastroenterol Hepatol 3(4):202–209. https://doi.org/10.1038/ncpgasthep0443
Huynh DK, Selvanderan S, Harley HAJ et al (2015) Nutritional care in hospitalized patients with chronic liver disease. World J Gasteroenterol 21(11):12835–12842. https://doi.org/10.1097/MEG.0b013e32834aa4bb
Plauth M, Cabré E, Riggio O et al (2006) ESPEN guidelines on enteral nutrition: liver disease. Clin Nut 25(2):285–294. https://doi.org/10.1016/j.clnu.2006.01.018
Selberg O, Selberg D (2002) Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol 86(6):509–516. https://doi.org/10.1007/s00421-001-0570-4
Pinato DJ, North B, Sharma R (2012) A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer 106(8):1439–1445. https://doi.org/10.1038/bjc.2012.92
Chan AWH, Chan S, Wong GLH et al (2015) Prognostic nutritional index (PNI) predicts tumor recurrence of very early/early stage hepatocellular carcinoma after surgical resection. Ann Surg Oncol 22(13):4138–4148. https://doi.org/10.1245/s10434-015-4516-1
Okamura Y, Ashida R, Ito T et al (2015) Preoperative neutrophil to lymphocyte ratio and prognostic nutritional index predict overall survival after hepatectomy for hepatocellular carcinoma. World J Surg 39(6):1501–1509. https://doi.org/10.1007/s00268-015-2982-z
Takagi K, Yagi T, Umeda Y (2017) Preoperative controlling nutritional status (CONUT) score for assessment of prognosis following hepatectomy for hepatocellular carcinoma. World J Surg 41(9):2353–2360. https://doi.org/10.1007/s00268-017-3985-8
Iseki Y, Shibutani M, Maeda K et al (2015) Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS One 10(7):e0132488. https://doi.org/10.1371/journal.pone.0132488
Ignacio de Ulíbarri J, G-Ma N, de Villar GP et al (2005) CONUT: a tool for controlling nutritional status: first validation in a hospital population. Nutr Hosp 20(1):38–45
Bolder U, Brune A, Schmidt S et al (1999) Preoperative assessment of mortality risk in hepatic resection by clinical variables: a multivariate analysis. Liver Transpl Surg 5(3):227–237. https://doi.org/10.1002/lt.500050302
Schütte K, Schuls C, Malfertheiner P (2015) Nutrition and hepatocellular cancer. Gastrointest Tumors 2(4):188–194. https://doi.org/10.1159/000441822
Miwa Y, Shiraki M, Kato M et al (2000) Improvement of fuel metabolism by nocturnal energy supplementation in patients with liver cirrhosis. Hepatol Res 18(3):184–189. https://doi.org/10.1016/S1386-6346(99)00100-X
Plank LD, Gane E, Peng S et al (2008) Nocturnal nutritional supplementation improves total body protein status of patients with liver cirrhosis: a randomized 12-month trial. Hepatology 48(2):557–566. https://doi.org/10.1002/hep.22367
Matos C, Porayko M, Francisco-Ziller N (2002) Nutrition and chronic liver disease. J Clin Gasteroenterol 35(5):391–397. https://doi.org/10.1097/00004836-200211000-00007
Gluud L, Dam G, Les I, Marchesini G, Borre M, Aagaard N, Vilstrup H (2017) Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev 5. https://doi.org/10.1002/14651858.CD001939.pub4
Morihara D, Iwata K, Hanano T (2012) Late-evening snack with branched-chain amino acids improves liver function after radiofrequency ablation for hepatocellular carcinoma. Hepatol Res 42(7):658–667. https://doi.org/10.1111/j.1872-034X.2012.00969.x
Nishikawa H, Osaki Y, Iguchi E et al (2013) The effect of long-term supplementation with branched-chain amino acid granules in patients with hepatitis C virus-related hepatocellular carcinoma after radiofrequency ablation. J Clin Gastroenterol 47(4):359–366. https://doi.org/10.1097/MCG.0b013e31826be9ad
Nishikawa H, Osaki Y, Inuzuka T et al (2012) Branched-chain amino acid treatment before transcatheter arterial chemoembolization for hepatocellular carcinoma. World J Gasteroenterol 18(12):1379–1384. https://doi.org/10.3748/wjg.v18.i12.1379
Ichikawa K, Okabayashi T, Maeda H et al (2012) Oral supplementation of branched-chain amino acids reduces early recurrence after hepatic resection in patients with hepatocellular carcinoma: a prospective study. Surg Today 43(7):720–726. https://doi.org/10.1007/s00595-012-0288-4
Mikagi K, Kawahara R, Kinoshita H, Aoyagi S (2011) Effect of preoperative immunonutrition in patients undergoing hepatectomy; a randomized controlled trial. Kurume Med J 58:1–8
Rayes N, Seehofer D, Hansen S et al (2002) Early enteral supply of lactobacillus and fiber versus selective bowel decontamination: a controlled trial in liver transplant recipients. Transplantation 74(1):123–128. https://doi.org/10.1097/00007890-200207150-00021
Rayes N, Seehofer D, Theruvath T et al (2005) Supply of pre- and probiotics reduces bacterial infection rates after liver transplantation—a randomized, double-blind trial. Am J Transplant 5(1):125–130. https://doi.org/10.1111/j.1600-6143.2004.00649.x
Usami M, Miyoshi M, Kanbara Y et al (2011) Effects of perioperative synbiotic treatment on infectious complications, intestinal integrity, and fecal flora and organic acids in hepatic surgery with or without cirrhosis. J Parenter Enter Nutr 35(3):317–328. https://doi.org/10.1177/0148607110379813
Kanazawa H, Nagino M, Kamiya S et al (2005) Synbiotics reduce post-operative infectious complications: a randomized controlled trial in biliary cancer patients undergoing hepatectomy. Langenbeck's Arch Surg 390(2):104–113. https://doi.org/10.1007/s00423-004-0536-1
Sugawara G, Nagino M, Nishio H et al (2006) Perioperative synbiotic treatment to prevent postoperative infectious complications in biliary cancer surgery: a randomized controlled trial. Ann Surg 244(5):706–714. https://doi.org/10.1097/01.sla.0000219039.20924.88
Richter B, Schmandra T, Golling M, Bechstein WO (2006) Nutritional support after open liver resection: a systematic review. Dig Surg 23(3):139–145. https://doi.org/10.1159/000094345
Pessaux P, Chenard M, Bachellier P, Jaeck D (2010) Consequences of chemotherapy on resection of colorectal liver metastases. J Visc Surg 147(4):e193–e201. https://doi.org/10.1016/j.jviscsurg.2010.06.004
Ribeiro HSC, Costa WL Jr, Diniz AL et al (2013) Extended preoperative chemotherapy, extent of liver resection and blood transfusion are predictive factors of liver failure following resection of colorectal liver metastasis. EJSO 39(4):380–385. https://doi.org/10.1016/j.ejso.2012.12.020
Read JA, Boris Choy S, Beale PJ et al (2006) Evaluation of nutritional and inflammatory status of advanced colorectal cancer patents and its correlation with survival. Nutr Cancer 55(78–85):78–85. https://doi.org/10.1207/s15327914nc5501_10
Kleiner DE, Brunt E, Van Natta M et al (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41(6):1313–1321. https://doi.org/10.1002/hep.20701
Reeves JG, Suriawinata A, Ng DP, Holubar SD, Mills JB, Barth RJ Jr (2013) Short-term preoperative diet modification reduces steatosis and blood loss in patients undergoing liver resection. Surgery 154(5):1031–1037. https://doi.org/10.1016/j.surg.2013.04.012
Sullivan S (2010) Implications of diet on nonalcoholic fatty liver disease. Curr Opin Gastroenterol 26(2):160–164. https://doi.org/10.1097/MOG.0b013e3283358a58
Gholam PM, Flancbaum L, Machan JT, Charney DA, Kotler DP (2017) Nonalcoholic fatty liver disease in severely obese subjects. Am J Gastroenterol 102(2):399–408. https://doi.org/10.1111/j.1572-0241.2006.01041.x
de Meijer VE, Kalish B, Pruder M, Ijzermans JNM (2010) Systematic review and meta-analysis of steatosis as a risk factor in major hepatic resection. Br J Surg 97(9):1331–1339. https://doi.org/10.1002/bjs.7194
Gomez D, Malik H, Bonney GK, Wong V, Toogood GJ, Lodge JPA, Prasad KR (2007) Steatosis predicts postoperative morbidity following hepatic resection for colorectal metastasis. Br J Surg 94(11):1395–1402. https://doi.org/10.1002/bjs.5820
Kooby DA, Fong Y, Suriawinata A et al (2003) Impact of steatosis on perioperative outcome following hepatic resection. J Gastrointest Surg 7(8):1034–1044. https://doi.org/10.1016/j.gassur.2003.09.012
Zhao J, van Mierlo K, Gómez-Ramírez J et al (2017) Systematic review of the influence of chemotherapy-associated liver injury on outcome after partial hepatectomy for colorectal liver metastases. BJS 104(8):990–1002. https://doi.org/10.1002/bjs.10572
Nomura F, Ohnishi K, Ochiai T, Okuda K (1987) Obesity-related nonalcoholic fatty liver: CT features and follow-up studies after low-calorie diet. Radiology 162(3):845–847. https://doi.org/10.1148/radiology.162.3.3809503
Fris RJ (2004) Preoperative low energy diet diminishes liver size. Obes Surg 14(9):1165–1170. https://doi.org/10.1381/0960892042386977
Ryan P, Nanji S, Pollett A, Moore M, Moulton CA, Gallinger S, Guindi M (2010) Chemotherapy-induced liver injury in metastatic colorectal cancer: semiquantitative histologic analysis of 334 resected liver specimens shows that vascular injury but not steatohepatitis is associated with preoperative chemotherapy. Am J Surg Pathol 34(6):784–791. https://doi.org/10.1097/PAS.0b013e3181dc242c
Nakano H, Oussoultzoglou E, Rosso E et al (2008) Sinusoidal injury increases morbidity after major hepatectomy in patients with colorectal liver metastases receiving preoperative chemotherapy. Ann Surg 247(1):118–124. https://doi.org/10.1097/SLA.0b013e31815774de
Vauthey JN, Pawlik T, Ribero D et al (2006) Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol 24(13):2065–2072. https://doi.org/10.1200/JCO.2005.05.3074
Pawlik TM, Olino K, Gleisner A, Torbenson M, Schulick R, Choti MA (2007) Preoperative chemotherapy for colorectal liver metastases: impact on hepatic histology and postoperative outcome. J Gastrointest Surg 11(7):860–868. https://doi.org/10.1007/s11605-007-0149-4
Wolf PS, Park J, Bao F et al (2013) Preoperative chemotherapy and the risk of hepatotoxicity and morbidity after liver resection for metastatic colorectal cancer: a single institution experience. J Am Coll Surg 216(1):41–49. https://doi.org/10.1016/j.jamcollsurg.2012.08.030
Sahajpal A, Vollmer CM Jr, Dixon E et al (2007) Chemotherapy for colorectal cancer prior to liver resection for colorectal cancer hepatic metastases does not adversely affect peri-operative outcomes. J Surg Oncol 95(1):22–27. https://doi.org/10.1002/jso.20632
Scoggins CR, Campbell M, Landry CS, Slomiany BA, Woodall CE, McMasters KM, Martin RCG (2009) Preoperative chemotherapy does not increase morbidity or mortality of hepatic resection for colorectal cancer metastases. Ann Surg Oncol 16(1):35–41. https://doi.org/10.1245/s10434-008-0190-x
Karoui M, Penna C, Amin-Hashem M et al (2006) Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg 243(1):1–7. https://doi.org/10.1097/01.sla.0000193603.26265.c3
Kishi Y, Zorzi D, Contreras CM et al (2010) Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol 17(11):2870–2876. https://doi.org/10.1245/s10434-010-1166-1
Quan D, Gallinger S, Nhan C et al (2012) The role of liver resection for colorectal cancer metastases in an era of multimodality treatment: a systematic review. Surgery 151(6):860–870. https://doi.org/10.1016/j.surg.2011.12.018
Eriksson S, Eriksson K, Bondesson L (1986) Nonalcoholic steatohepatitis in obesity: a reversible condition. Acta Med Scand 220(1):83–88. https://doi.org/10.1111/j.0954-6820.1986.tb02733.x
Jones JC, Coombes J, Macdonald GA (2012) Exercise capacity and muscle strength in patients with cirrhosis. Liver Transpl 18(2):146–151. https://doi.org/10.1002/lt.22472
Bohannon RW, Magasi S, Bubela DJ et al (2012) Grip and knee extension muscle strength reflect a common construct among adults. Muscle Nerve 46(555–558):555–558. https://doi.org/10.1002/mus.23350
Campillo B, Fouet P, Bonnet JC et al (1990) Submaximal oxygen consumption in liver cirrhosis: evidence of severe functional aerobic impairment. J Hepatol 10(2):163–167. https://doi.org/10.1016/0168-8278(90)90046-T
Lemyze M, Dharancy S, Wallaert B (2013) Response to exercise in patients with liver cirrhosis: implications for liver transplantation. Dig Liver Dis 45(5):362–366. https://doi.org/10.1016/j.dld.2012.09.022
Terziyski K, Andonov V, Marinov B et al (2008) Exercise performance and ventilatory efficiency in patients with mild and moderate liver cirrhosis. Clin Exp Pharmacol Physiol 35(0):135–140. https://doi.org/10.1111/j.1440-1681.2007.04751.x
Weisinger GF, Quittan M, Zimmermann K et al (2001) Physical performance and health-related quality of life in men on a liver transplantation waiting list. J Rehabil Med 33:260–265
Epstein SK, Ciubotaru R, Zilberberg MD et al (1998) Analysis of impaired exercise capacity in patients with cirrhosis. Dig Dis Sci 43(8):1701–1707. https://doi.org/10.1023/A:1018867232562
Pieber K, Crevenna R, Nuhr MJ et al (2006) Aerobic capacity, muscle strength and health-related quality of life before and after orthotopic liver transplantation: preliminary data of an Austrian transplantation centre. J Rehabil Med 38(5):322–328. https://doi.org/10.1080/16501970600680288
Bernal W, Martin-Mateos R, Lipcsey M et al (2014) Aerobic capacity during cardiopulmonary exercise testing and survival with and without liver transplantation for patients with chronic liver disease. Liver Transpl 20(1):54–62. https://doi.org/10.1002/lt.23766
Dharancy S, Lemyze M, Boleslawski E et al (2008) Impact of impaired aerobic capacity on liver transplant candidates. Transplantation 86(8):1077–1083. https://doi.org/10.1097/TP.0b013e318187758b
Andersen H, Borre M, Jakobsen J et al (1998) Decreased muscle strength in patients with alcoholic liver cirrhosis in relation to nutritional status, alcohol abstinence, liver function, and neuropathy. Hepatology 27(5):1200–1206. https://doi.org/10.1002/hep.510270503
Tartar RE, Panzak G, Switala J et al (1997) Isokinetic muscle strength and its association with neuropsychological capacity in cirrhotic alcoholics. Alcohol Clin Exp Res 21(2):191–196. https://doi.org/10.1111/j.1530-0277.1997.tb03748.x
Montano-Loza AJ, Meza-Junco J, Prado CMM (2012) Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol 10(2):166–173. https://doi.org/10.1016/j.cgh.2011.08.028
Ruiz-del-Árbol L, Serradilla R (2015) Cirrhotic cardiomyopathy. World J Gasteroenterol 21(41):11502–11521. https://doi.org/10.3748/wjg.v21.i41.11502
Carey EJ, Steidley D, Aqel BA (2010) Six-minute walk distance predicts mortality in liver transplant candidates. Liver Transpl 16(12):1373–1378. https://doi.org/10.1002/lt.22167
Tandon P, Low G, Mourtzakis M (2016) A model to identify sarcopenia in patients with cirrhosis. Clin Gastroenterol Hepatol 14(10):1473–1480. https://doi.org/10.1016/j.cgh.2016.04.040
Zenith L, Meena N, Ramadi A et al (2014) Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin Gastroenterol Hepatol 12(11):1920–1926. https://doi.org/10.1016/j.cgh.2014.04.016
Debette-Gratien M, Tabouret T, Antonini MT et al (2014) Personalized adapted physical activity before liver transplantation: acceptability and results. Transplantation 99(1):145–150. https://doi.org/10.1097/TP.0000000000000245
Garcίa-Pagán JC, Santos C, Barberá JA et al (1996) Physical exercise increases portal pressure in patients with cirrhosis and portal hypertension. Gastroenterology 111(5):1300–1306. https://doi.org/10.1053/gast.1996.v111.pm8898644
Bandi JC, García-Pagán J, Escorsell A et al (1998) Effects of propranolol on the hepatic hemodynamic response to physical exercise in patients with cirrhosis. Hepatology 28(3):667–682. https://doi.org/10.1002/hep.510280312
Hulzebos EHJ, Smit Y, Helders PP JM, van Meeteren NLU (2014) Preoperative physical therapy for elective cardiac surgery patients (review). Cochrane Database Syst Rev (11). https://doi.org/10.1002/14651858.CD010118.pub2
Garcia RS, Yáñez-Brage M, Moolhuyzen EG, Riobo MS, Paz AL, Mate JMB (2017) Preoperative exercise training prevents functional decline after lung resection surgery: a randomized, single-blind controlled trial. Clin Rehab 31(8):1057–1067. https://doi.org/10.1177/0269215516684179
Carver TE, Mayo N, Andersen RE, Zavorsky GS (2011) Pilot investigation to evaluate changes in exercise capacity following a prehabilitation intervention among seriously obese patients awaiting bariatric surgery. Can J Diabetes 35(2):149. https://doi.org/10.1016/S1499-2671(11)52045-3
Hijazi Y, Gondal U, Aziz (2017) A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg 39:156–162. https://doi.org/10.1016/j.ijsu.2017.01.111
Dunne DEJ, Jack S, Jones RP et al (2016) Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg 103(5):504–512. https://doi.org/10.1002/bjs.10096
Mayo NE, Feldman L, Scott S et al (2011) Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery 150(3):505–514. https://doi.org/10.1016/j.surg.2011.07.045
Wijeysundera DN, Pearse R, Shulman MA et al (2016) Measurement of Exercise Tolerance before Surgery (METS) study: a protocol for an international multicentre prospective cohort study of cardiopulmonary exercise testing prior to major non-cardiac surgery. BMJ Open 6(3):e010359. https://doi.org/10.1136/bmjopen-2015-010359
Author information
Authors and Affiliations
Contributions
Study conception and design: Billingsley; acquisition of data: Walcott-Sapp; analysis and interpretation of data: Billingsley and Walcott-Sapp; drafting of manuscript: Billingsley and Walcott-Sapp; critical revision of manuscript: Billingsley and Walcott-Sapp.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Walcott-Sapp, S., Billingsley, K.G. Preoperative optimization for major hepatic resection. Langenbecks Arch Surg 403, 23–35 (2018). https://doi.org/10.1007/s00423-017-1638-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-017-1638-x