Abstract
Purpose
Resection of the extrahepatic bile duct is not performed uniformly in gallbladder cancer. The study investigated the clinical significance of resection of extrahepatic bile duct (EHBD) in T2 and T3 gallbladder cancer.
Methods
Between 2000 and 2010, 71 T2 or T3 gallbladder cancer patients who underwent R0 resection at Korea University Medical Center were included. Clinicopathological data were reviewed retrospectively. Survival analysis and comparison between EHBD resection and non-resection groups were performed.
Results
The 32 men and 39 women had 49 T2 tumors and 22 T3 tumors. The overall survival rate was 67.8 % at 3 years and 47.2 % at 5 years. In multivariate analysis for overall survival, lymphovascular invasion and lymph node metastasis were significant independent predictors. Comparing the patients according to EHBD resection, the EHBD resection group demonstrated significantly longer hospital stay, longer operative time, more transfusion requirement, more extensive liver resection, and less treatment of neoadjuvant therapy. Significantly higher proportions of perineural invasion and lymph node metastasis were noted in the EHBD resection group. There were no statistically significant differences in survival between the EHBD resection and non-resection groups.
Conclusions
Resection of extrahepatic bile duct was not always necessary in T2 and T3 cancers. However, the patients who undergo resection of extrahepatic bile duct tended to have more aggressive tumor characteristics and undergo more aggressive surgical approach. To enhance overall survival for the patients with T2 and T3 gallbladder cancers, surgeons should try to perform R0 resection including EHBD resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical surgery to achieve R0 resection is the treatment of choice for gallbladder cancer [1–4]. In T1 gallbladder cancer, cholecystectomy with/without lymph node dissection is appropriate [5]. For cancers more than T2, various surgical procedures have been adopted. Depth of tumor invasion and the progression of the disease are the key factors determining the extent of surgery. Depth of invasion, presence of lymph node metastasis, perineural invasion, and negative resection margin are significant prognostic factors affecting overall survival in gallbladder cancer [2–4, 6–8]. However, these factors are not easily detectable preoperatively or intraoperatively.
The extent of liver resection and lymph node dissection and whether to perform extrahepatic bile duct (EHBD) resection remains controversial [9–14]. There is no clear indication whether to include EHBD resection or not in gallbladder cancer surgery, except for early gallbladder cancer. Furthermore, the survival benefit of EHBD resection has not been defined precisely.
The aim of this retrospective study was to investigate the significance of EHBD resection in surgery for T2 and T3 gallbladder cancers. We focused on the oncologic benefit of EHBD resection in the resectable cases of gallbladder cancer excluding early gallbladder cancer (T1). The patients were divided into an EHBD resection group and EHBD non-resection group. Clinicopathological characteristics were compared between the two groups. The survival outcome and prognostic predictors affecting overall survival in patients with T2 and T3 gallbladder cancers after curative resection were analyzed.
Methods
From January 2000 to December 2010, 194 operations for gallbladder cancers were performed at the Department of Surgery, Korea University Medical Center, Korea University College of Medicine, Seoul, Korea. There were 99 resections for T2 and T3 gallbladder cancers. We excluded patients who underwent R1 resection (n = 24) and R2 (n = 4) resections. Seventy-one patients with T2 and T3 gallbladder cancers who underwent R0 resection were included in this study. Of the 71 patients, 49 (69 %) were diagnosed with pT2 tumors and the remaining 22 (31 %) were pT3 tumors. The patients' demographics and clinicopathological information were retrospectively obtained from the medical records and included age, gender, operative procedures, operative time, transfusion requirement, pathological results, postoperative complication, adjuvant therapy, and recurrence.
Lymph nodes were classified according to the TNM classification of the American Joint Committee on Cancer (AJCC) [15]. N1 was defined as metastases to nodes along the cystic duct, common bile duct, hepatic artery, and/or portal vein. N2 was defined as metastases to periaortic, pericaval, superior mesentery artery, and/or celiac artery lymph nodes. N2 disease was not included because R0 resection could not be guaranteed in N2 disease with a possibility of microscopic systemic dissemination.
Pathologically, the gross morphological features were classified into two groups according to the presence of infiltration: infiltrative versus non-infiltrative tumor. Histologic type, differentiation, presence of perineural and lymphovascular invasion, lymph node metastasis, and margin status were investigated. Tumor stage was defined according to the AJCC pathological tumor node metastasis (pTNM) classification [15].
Survival analysis of the 71 R0 resection patients was performed. The survival rates were compared between R0 and R1 patients. Furthermore, the survival time of the R0 resection patients who demonstrated recurrence was compared with that of the R1 patients. The clinicopathological characteristics between the EHBD resection and EHBD non-resection group were compared. Significant prognostic factors affecting overall survival were investigated by univariate and multivariate analyses. Statistical calculations were performed using SPSS version 13.0 for Windows (SPSS, Chicago, IL, USA). Survival was measured from the date of surgery. Disease-free survival was measured from the date of surgery to the diagnosis of recurrence. Follow-up of patients was completed when death occurred or on November 31, 2012. Comparisons between groups were tested using Pearson's chi-square test and independent t test. Overall survival was calculated using the Kaplan–Meier method. Clinicopathologic prognostic factors were analyzed by the univariate Kaplan–Meier method and compared by the log-rank test to identify the prognostic predictors for survival. Multivariate analysis was performed using Cox proportional hazards model to identify the independent prognostic factors for survival. Variables to be entered into the multivariate analysis were selected on the basis of the results of univariate analysis (p < 0.1). A p value < 0.05 was considered statistically significant.
Results
Clinicopathological characteristics
The patients comprised of 32 men and 39 women, aged 22 to 82 years (mean age 64 years). Gallstones were present in 25 patients (35 %). Fifty-four patients were diagnosed as definite or suspicious for gallbladder malignancy based on preoperative computed tomography scan. However, 17 patients were diagnosed with incidental gallbladder cancers during or after laparoscopic cholecystectomy. Of them, 16 patients received additional liver and/or EHBD resection and lymph node dissection immediately during the laparoscopic cholecystectomy or sometime after cholecystectomy. One patient received only an additional lymph node dissection. The operative procedures were cholecystectomy in 11 patients, cholecystectomy with EHBD resections in 9 patients, cholecystectomy with liver resection in 30 patients, and cholecystectomy with liver and EHBD resections in 21 patients. All patients received lymph node dissection. EHBD resection was performed in 30 patients and liver resection in 51 patients. Most of the liver resections (n = 39) consisted of a wedge resection of liver around the gallbladder with a margin of approximately 2 cm. More extensive liver resections were performed in 12 patients and involved a right hemihepatectomy in four patients, central bisectionectomy in three patients, and segment 4b and 5 bisegmentectomy in 5 patients. Combined other organ resections were performed in five patients involving the stomach in two patients, colon in three patients, and pancreaticoduodenectomy in the remaining patient. Mean operative time was 256 ± 138 min and mean postoperative hospital stay was 14.6 ± 14.8 days. Postoperative complications occurred in 13 patients (18 %) and comprised with intra-abdominal abscess (n = 4), surgical site infection (n = 5), pleural effusion (n = 2), acute renal failure (n = 1), and angina (n = 1). There was no postoperative mortality.
Adjuvant therapy was performed in 38 (54 %) patients and involved chemotherapy in 29 patients, radiation therapy in 2 patients, and concurrent chemoradiation therapy in 7 patients. Adjuvant radiation therapy was performed with external beam radiotherapy, and adjuvant chemotherapy was performed systemically using a 5-flurouracil, cisplatin, or gemcitabine-based regimen.
Pathologically, 22 patients were classified into T3 tumors as follows: perforating serosa (n = 4), invasion to the liver (n = 12), stomach (n = 1), colon (n = 1), omentum (n = 3), and EHBD (n = 4). Three patients had tumors invading the liver and other extrahepatic organs simultaneously.
The clinicopathological differences according to depth of invasion (T stage) are shown in Table 1. More extensive liver resections were performed in T3 tumors than in T2 tumors. T3 tumors were significantly greater in size. Significantly higher proportions of lymphovascular invasion, perineural invasion, and lymph node metastasis were detected in T3 tumors. There were no differences in EHBD resection, laparoscopic approach (proportion of incidentally diagnosed gallbladder cancer), adjuvant therapy, proportion of infiltrative tumor, and differentiation.
Overall survival and recurrence
Overall survival rates for the 71 patients who underwent R0 resection for T2 and T3 gallbladder cancers were 67.8 % at 3 years and 47.2 % at 5 years with median survival time of 51.4 months (Fig. 1). Comparing the survival of R0 and R1 (n = 24) patients, the 3- and 5-year survival rates of R1 patients were 14.3 % and 7.2 %, respectively, with a median survival time of 11.6 months, which was significantly poorer than R0 patients (p < 0.001). Univariate analysis of the 71 R0 resection patients revealed that infiltrative tumor (p = 0.002), lymphovascular invasion (p < 0.001), lymph node metastasis (p = 0.001), and advanced AJCC stage were significantly poor predictors for survival (Table 2). There was no survival difference between the EHBD resection group and EHBD non-resection group. The extent of liver resection, adjuvant therapy, size, and differentiation did not affect overall survival significantly. Five-year survival rate of T2 and T3 gallbladder cancers after R0 resection was 49.9 % and 38.5 %, respectively, showing no statistically significant difference (p = 0.304). Perineural invasion was not a significant prognostic factor for overall survival (p = 0.099). Multivariate analysis using a Cox proportional hazards model demonstrated that lymphovascular invasion (p = 0.001; hazard ratio (HR), 5.729; confidence interval (CI), 2.096–15.331) and lymph node metastasis (p = 0.012; HR, 2.826; CI, 1.259–6.345) were significant independent predictors of overall survival.
Recurrence occurred in 30 patients (42.3 %). Of them, four patients had unknown recurrent time and sites. Disease-free survival rates were 77.0 % at 1 year and 58.5 % at 3 years. Comparing the overall survival between the R0 resection patients who demonstrated recurrence (n = 30) with patients who had R1 resection (n = 24), median survival time of the former (27.7 months) was superior to those of the latter (11.6 months) (p = 0.031). The sites and patterns of recurrence were as follows: locoregional recurrence (n = 6), liver (n = 11), lung (n = 4), peritoneum (n = 6), and distant lymph nodes (paraaortic, aortocaval lymph nodes, n = 13). Twelve patients demonstrated more than two recurrent sites and/or pattern at the initial diagnosis of the recurrent disease. Only one patient demonstrated solitary local recurrence. The other five patients who demonstrated local recurrence had combined other distant recurrent disease. All recurrent patients except one demonstrated distant metastasis as a recurrent pattern. The liver and distant lymph nodes were common.
Comparison between EHBD resection and EHBD non-resection groups
The EHBD resection group demonstrated significantly longer operative time (p < 0.001), more transfusion requirement (p = 0.022), more extensive liver resection (p = 0.039), and longer postoperative hospital stay (p = 0.034) than the EHBD non-resection group. Significantly, more occurrences of complication (p = 0.007) and less treatment of adjuvant chemo- and/or radiation therapy (p = 0.028) were evident in the EHBD resection group. Pathologically, significantly higher incidence of perineural invasion (p = 0.019), lymph node metastasis (p = 0.021), and advanced stage (p = 0.035) were present in the EHBD resection group than the EHBD non-resection group. There were no differences in size, proportion of infiltrative tumors, differentiation, presence of lymphovascular invasion, and T stage between the EHBD resection and EHBD non-resection groups (Table 3). According to the survival analysis for EHBD resection, the EHBD resection group did not achieve better survival and disease-free survival than the EHBD non-resection group. The 3- and 5-year survival rates of EHBD resection group were 55.6 % and 34.8 %, respectively, and those of EHBD non-resection group were 76.4 % and 54.2 %, respectively (p = 0.112). The 3- and 5-year disease-free survival of EHBD resection groups were 48.4 % and 36.3 %, respectively, and those of EHBD non-resection group were 66.8 % and 45.9 %, respectively (p = 0.246) (Fig. 2).
Discussion
In the current study of T2 and T3 gallbladder cancer following R0 resection, lymphovascular invasion and lymph node metastasis were independent prognostic factors for survival by multivariate analysis, while perineural invasion was not. R0 resection, presence of lymph node metastasis [2, 4, 10, 14, 16], and perineural invasion [6, 10] have been reported to be significant prognostic factors for survival. Several studies have focused on the clinical significance of hepatoduodenal ligament invasion and EHBD resection [6, 11, 17–20].
The surgical extent of T2 and T3 gallbladder cancer remains controversial. Although R0 resection is the treatment of choice, whether or not to perform EHBD resection is still debatable [17–20]. In the current study, patients who underwent EHBD tended to have more aggressive tumor characteristics and to be treated by more extensive liver resection. Significantly higher proportion of perineural invasion and lymph node metastasis were detected in the EHBD resection group than the EHBD non-resection group. However, there was no survival difference between the groups, perhaps reflecting a selection bias in which more aggressive tumors tended to be addressed using a more aggressive surgical approach including EHBD resection. Therefore, it seems reasonable to conclude that EHBD resection might offer some survival benefit.
Several studies have verified the efficacy of EHBD resection or the indication of EHBD resection in gallbladder cancer. Sakamoto et al. reported no survival benefit of EHBD resection in patients with T2 or higher grader gallbladder cancer, with or without lymph node metastasis [6]. However, in gallbladder cancers with the presence of perineural invasion, patients with EHBD resection showed significantly better survival than those without EHBD resection, prompting the conclusion that EHBD resection might offer a prognostic advantage when perineural invasion exists. However, the precise assessment of lymph node metastasis and perineural invasion was limited preoperatively, leading the authors to suggest routine EHBD resection in all patients with gallbladder cancer higher than T2 [6]. In another study [18], modes of hepatoduodenal ligament invasion were classified into four groups: direct invasion of bile duct, continuous intramural interstitial spread, distant spread separated from the primary tumor, and metastatic lymph node. The survival of the patients with direct invasion of bile duct was poorer than the other three types. The authors also suggested that strong consideration should be given to resection of EHBD in patients with gallbladder cancer higher than T2.
On the contrary, the recent Japanese Society of Biliary Surgery survey reported that there was no difference in overall survival between the EHBD resection and EHBD non-resection groups in patients with lymph node metastasis at each T2, T3, and T4 stage gallbladder cancer [19]. Therefore, EHBD resection might be unnecessary in advanced gallbladder cancer without a direct infiltration of the hepatoduodenal ligament and the cystic duct [17, 19]. EHBD resection has a potential adverse effect of bilioenteric anastomosis [17] and is associated with a significantly higher occurrence of postoperative complications [19] similar to our result. Moreover, presently, the EHBD resection group demonstrated significantly longer operation time and postoperative hospital stay, and more transfusion requirement; these factors are associated with a higher occurrence of complications. However, these factors will be overcome by efforts to improve the surgical technique, anesthesia, and postoperative care.
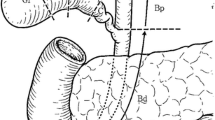
Tumor cells spread into the interstitial tissues of the hepatoduodenal ligament, which are abundant in lymphatic and nerve tissues [11, 18]. The interstitial tissue invasion progresses not only to the hepatoduodenal ligament, head of the pancreas, and the paraaortic fat but also to Glisson's sheath in the liver, followed by invasion of the interstitial tissue around the hilar bile duct [11]. As shown presently, most of the recurrent pattern was distant metastasis not local recurrence. Liver and the paraaortic and aortocaval lymph node were common sites for recurrence. Therefore, EHBD resection requires complete clearance of the interstitial tissues and lymph nodes of the hepatoduodenal ligament as systemic control, as well as regional control to minimize lymphatic and interstitial spread.
In this retrospective study, to decide whether or not to perform EHBD resection was dependent on the surgeons' policy or the patients' general condition including age and comorbidity. Although the indications of EHBD resection were not always clear-cut in the retrospective basis of this study, EHBD resection was performed in patients with suspected direct invasion of cancer cells in the bile duct by intraoperative finding although the final pathology are not always positive of cancer cell, or positive cystic duct margin, or performed for complete clearance of the hepatoduodenal ligament.
The efficiency of adjuvant therapy was controversial in a review of literature [21–23]. There was no influence of adjuvant therapy on survival when R0 resection was performed, and adjuvant therapy was less administered in EHBD resection group than EHBD non-resection group in the current study. From a meta-analysis of the adjuvant therapy in the treatment of biliary tract cancer including gallbladder cancer [23], there was not a significant survival benefit in adjuvant therapy group comparing with surgery alone group. However, in patients who had lymph node-positive disease or advanced gallbladder cancer and R1 disease, adjuvant therapy was beneficial [22, 23]. Although there was no efficacy of adjuvant therapy after R0 resection from this study, however, in patients with advanced gallbladder cancer with lymph node metastasis, adjuvant therapy could be considered.
In conclusion, lymphovascular invasion and lymph node metastasis were significant independent prognostic factor for overall survival in T2 and T3 gallbladder cancer following R0 resection. EHBD resection groups tended to have more aggressive tumor characteristic than the EHBD non-resection group. Furthermore, there was no survival difference between the two groups. Therefore, EHBD resection was not always necessary in T2 and T3 cancers. However, to enhance the overall survival for patients with T2 and T3 gallbladder cancer, especially demonstrating aggressive tumor characteristics, surgeons should try to perform R0 resection including EHBD resection.
References
Chan SY, Poon RT, Lo CM et al (2008) Management of carcinoma of the gallbladder: a single-institution experience in 16 years. J Surg Oncol 97:156–164
Kai M, Chijiiwa K, Ohuchida J et al (2007) A curative resection improves the postoperative survival rate even in patients with advanced gallbladder carcinoma. J Gastrointest Surg 11:1025–1032
Yagi H, Shimazu M, Kawachi S et al (2006) Retrospective analysis of outcome in 63 gallbladder carcinoma patients after radical resection. J Hepatobiliary Pancreat Surg 13:530–536
Behari A, Sikora SS, Wagholikar GD et al (2003) Longterm survival after extended resections in patients with gallbladder cancer. J Am Coll Surg 196:82–88
You DD, Lee HG, Paik KY et al (2008) What is an adequate extent of resection for T1 gallbladder cancers? Ann Surg 247:835–838
Sakamoto Y, Kosuge T, Shimada K et al (2006) Clinical significance of extrahepatic bile duct resection for advanced gallbladder cancer. J Surg Oncol 94:298–306
Shimada H, Endo I, Togo S et al (1997) The role of lymph node dissection in the treatment of gallbladder carcinoma. Cancer 79:892–899
Sasaki R, Uesugi N, Itabashi H et al (2005) Clinicopathological study of depth of subserosal invasion in patients with pT2 gallbladder carcinoma. J Surg Oncol 92:83–88
Shimada H, Endo I, Fujii Y et al (2000) Appraisal of surgical resection of gallbladder cancer with special reference to lymph node dissection. Langenbecks Arch Surg 385:509–514
Chijiiwa K, Nakano K, Ueda J et al (2001) Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer. J Am Coll Surg 192:600–607
Endo I, Shimada H, Fujii Y et al (2001) Indications for curative resection of advanced gallbladder cancer with hepatoduodenal ligament invasion. J Hepatobiliary Pancreat Surg 8:505–510
Araida T, Higuchi R, Hamano M et al (2009) Hepatic resection in 485 R0 pT2 and pT3 cases of advanced carcinoma of the gallbladder: results of a Japanese Society of Biliary Surgery survey–a multicenter study. J Hepatobiliary Pancreat Surg 16:204–215
Kondo S, Nimura Y, Hayakawa N et al (2000) Regional and para-aortic lymphadenectomy in radical surgery for advanced gallbladder carcinoma. Br J Surg 87:418–422
Kohya N, Miyazaki K (2008) Hepatectomy of segment 4a and 5 combined with extra-hepatic bile duct resection for T2 and T3 gallbladder carcinoma. J Surg Oncol 97:498–502
Edge SB, Byrd DR, Compton CC et al (eds) (2009) AJCC Cancer staging manual, 7th edn. Springer, New York
Shimizu H, Kimura F, Yoshidome H et al (2007) Aggressive surgical approach for stage IV gallbladder carcinoma based on Japanese Society of Biliary Surgery classification. J Hepatobiliary Pancreat Surg 14:358–365
Kosuge T, Sano K, Shimada K et al (1999) Should the bile duct be preserved or removed in radical surgery for gallbladder cancer? Hepatogastroenterology 46:2133–2137
Shimizu Y, Ohtsuka M, Ito H et al (2004) Should the extrahepatic bile duct be resected for locally advanced gallbladder cancer? Surgery 136:1012–1017, discussion 1018
Araida T, Higuchi R, Hamano M et al (2009) Should the extrahepatic bile duct be resected or preserved in R0 radical surgery for advanced gallbladder carcinoma? Results of a Japanese Society of Biliary Surgery Survey: a multicenter study. Surg Today 39:770–779
Kaneoka Y, Yamaguchi A, Isogai M et al (2003) Hepatoduodenal ligament invasion by gallbladder carcinoma: histologic patterns and surgical recommendation. World J Surg 27:260–265
Park HS, Lim JY, Yoon DS et al (2010) Outcome of adjuvant therapy for gallbladder cancer. Oncology 79:168–173
Mojica P, Smith D, Ellenhorn J (2007) Adjuvant radiation therapy is associated with improved survival for gallbladder carcinoma with regional metastatic disease. J Surg Oncol 96:8–13
Horgan AM, Amir E, Walter T et al (2012) Adjuvant therapy in the treatment of biliary tract cancer: a systematic review and meta-analysis. J Clin Oncol 30:1934–1940
Acknowledgments
The research was supported by a grant from Korea University.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, S.B., Han, H.J., Kim, W.B. et al. Surgical strategy for T2 and T3 gallbladder cancer: is extrahepatic bile duct resection always necessary?. Langenbecks Arch Surg 398, 1137–1144 (2013). https://doi.org/10.1007/s00423-013-1120-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1120-3