Abstract
Purpose
Umbilical and epigastric hernia repairs are minor, but are commonly conducted surgical procedures. Long-term results have only been sparsely investigated.
Our objective was to investigate the risk of chronic complaints after a simple sutured repair for small umbilical and epigastric hernias.
Methods
A retrospective cohort study with a 5-year questionnaire and clinical follow-up was conducted. Patients undergoing primary elective, open non-mesh umbilical or epigastric sutured hernia repair were included. Patients completed a structured questionnaire regarding chronic complaints during work and leisure activities using a verbal rating scale. The primary outcome was chronic complaints.
Results
A total of 295 patients were included for analysis after a median of 5.0-year (range 2.8–8.0) follow-up period. Follow-up results were achieved from 262 of the included patients (90 % response rate). Up till 5.8 % of the patients reported moderate or severe pain and discomfort. Work and leisure activities were restricted in 8.5 and 10.0 % of patients, respectively. Patients with chronic complaints had a higher incidence of recurrence (clinical and reoperation), than patients with none or mild complaints (78.6 vs. 22.2 % (P < 0.001)). The recurrence rate was significantly higher after a repair with absorbable suture (20.1 %) compared with non-absorbable suture repair (4.2 %) (P < 0.001).
Conclusion
We found that chronic complaints after a simple sutured umbilical or epigastric repair was in the level of 5.5 % and could in part be explained by recurrence. Furthermore, absorbable suture should be omitted to reduce risk of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Umbilical and epigastric hernia repairs are minor general surgical procedures [1]. However, there is no consensus on the optimal repair technique [2].
Recurrence rates after mesh repairs are significantly lower than after sutured repair [3–5], but sutured repair is still the most frequently used technique for repair of smaller umbilical and epigastric hernia defects [2]. Only few retrospective and heterogenic studies using a mixture of mesh and sutured repairs have investigated chronic complaints after umbilical and epigastric hernia repairs [6–8].
Our primary objective was to study the risk of chronic complaints after simple sutured repair for umbilical and epigastric hernias and the influence of recurrence (clinical recurrence and operation for recurrence) on chronic complaints.
Material and methods
Patients
This was a retrospective cohort study with a questionnaire follow-up enrolling consecutive patients from two university hospitals with free referral. Patients were identified by national code numbers for open umbilical and epigastric hernia repair (JAF10-20-30-96 and JAE 10) during the period of 1st of January 2000–31st of December 2004.
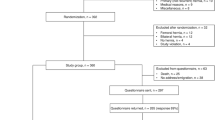
Several predefined exclusion criteria were defined before the study started, as listed in Fig. 1. Only patients ≥18 years undergoing primary elective open non-mesh umbilical or epigastric hernia repair using a simple suture technique were analysed. Demographic data and perioperative results were collected retrospectively from hospital files. Information about the patient and the primary repair (size of hernia defect, type of the suture material used for the repair, age, gender, smoking and alcohol habits, and recurrence) were analysed for possible influence on study endpoints.
Questionnaire and follow-up
All included patients were prospectively contacted by letter and asked to complete a structured questionnaire regarding pain and discomfort localised at the umbilical or epigastric scar during work and leisure activities. Questions were about instant pain and discomfort as well as pain and discomfort in average covering the last week. For this purpose, a verbal rating scale was used (no = 0, light = 1, moderate = 2, severe = 3). Instant pain and discomfort were registered at rest and during mobilisation from supine to sitting position. Patients were also asked about their physical workload (sedentary/moderate or strenuous) and whether work and leisure activities were restricted by chronic complaints due to their previous hernia repair. Finally, patients noted the date of first suspicion of clinical recurrence.
Patients with suspected recurrence or moderate to severe pain and/or discomfort (answers based on the structured questionnaire) qualified for clinical examination. All patients were clinically examined in their private homes by an experienced general surgeon and, when in doubt, further diagnostic work-up was performed with abdominal CAT-scan or trans-abdominal ultrasonography.
Statistics and ethics
Data are presented with exact numbers, medians (ranges), and percentages as appropriate. Age, BMI, and hernia size were divided according to ≤ or > median values. Incidence of moderate or severe complaints (chronic complaints) was analyzed against incidence of none or mild complaints (no complaints) in relation to recurrence (clinical and reoperation for recurrence) using Fisher's exact test and 95 % confidence intervals (CI).
Five different variables were investigated for impact on the rate of chronic complaints: size of hernia defect, type of the suture, age, gender, and recurrence. The risk of mass significance due to multiple testing was minimised by the Bonferroni correction. Thus, P = 0.05/5 = 0.010 was considered statistically significant.
The Local Ethics Committee (reg. no. KF07329141) and Data Protection Agency (reg. no. 2008-58-0020) approved the study. The study was registered at ClinicalTrials.gov (NCT0174740).
Results
During the inclusion period, 587 patients underwent umbilical or epigastric hernia repair of whom 292 were excluded leaving 295 patients for analysis (Fig. 1). The follow-up period was 5.0 years (2.8–8.0). Follow-up results were achieved from 262 of the included patients (90 % response rate). Patient characteristics of the included patients are given in Table 1. General anaesthesia was used in 270 (91.5 %) patients, and local anaesthesia in 25 (8.5 %) patients. Hospital stay was median 0 day (0–6 days). No deaths were recorded.
Fourteen (5.5 %) and 15 (5.8 %) of the patients reported chronic moderate or severe pain or discomfort, respectively (Table 2). Work and leisure activities were restricted in 8.5 and 10.0 % of the patients, respectively. There were 165 employed patients (76 % reported sedentary/moderate work, 20 % strenuous work; 4 % no information). The most frequently reported reason for restriction was complaints during lifting.
Based on the returned questionnaires, 35 patients suspected recurrence and/or had moderate/severe pain or discomfort. Thirty-three patients presented a clinical recurrence at the follow-up and another 33 patients had undergone reoperation leading to a total of 66 (25.2 %) patients with recurrence.
Patients with moderate or severe complaints had a significantly higher incidence of recurrence (clinical and reoperation) than patients with none or mild complaints (78.6 %, (CI = 57.1–100.1) vs. 22.2 %, (CI = 17.0–27.4) (P < 0.001) (Table 3). The other study variables had no significant influence on the incidence of moderate or severe complaints (P = 0.13–0.76).
Defect closure was with fast absorbable (e.g. polyglactin) in 210 (71.2 %), and with non-absorbable suture (e.g. polypropylene) in 85 (28.8 %) of the patients. The recurrence rate was significantly higher after a repair with absorbable suture (20.1 %) compared with non-absorbable suture repair (4.2 %) (P < 0.001). The other study variables had no significant influence on the recurrence rate (P = 0.1–0.8).
Discussion
This study found that 5.5 % of patients undergoing a simple sutured repair for an umbilical or epigastric hernia suffered from moderate or severe pain 5 years after primary repair. Moreover, 8.5–10.0 % of the patients were restricted from work and leisure activities, due to chronic complaints after repair.
Previous studies on umbilical and epigastric hernia repairs focused mainly on early postoperative results as wound complications or recurrence rates [9–12]. As in groin hernia surgery, chronic pain and discomfort may evolve to become an important target for future research areas [13]. A recent retrospective study with questionnaire follow-up (n = 132) in patients undergoing mesh or sutured repairs for umbilical or epigastric hernia repairs found a 10 % risk of moderate to severe pain or discomfort 3 years after surgery [6]. No differences were seen between the mesh and sutured repair groups. In another retrospective study with a 32-month follow-up after mesh repair of incisional or umbilical hernias, 18 % of the patients reported deteriorated self-estimated general health after their hernia repair [7]. Finally, a retrospective study of 97 patients undergoing umbilical hernia repair with a 5-year follow-up reported a 21 % risk of pain and discomfort [8]. These studies underline a substantial risk of chronic complaints after simple sutured or mesh repair after umbilical and epigastric hernias. A rough qualitative comparison of the literature and the present study, which included only sutured repairs, revealed a somewhat lower incidence of chronic complaints in the present study, although high restriction for work and leisure activities in up to 10 % of the patients.
Interestingly, the majority (78, 6 %) of patients reporting moderate to severe pain or discomfort had a recurrent hernia. This rate is probably higher compared with the conditions following repair of groin hernia, although exact data is not available [14]. The findings of this study call for future evaluation of a policy offering all patients with chronic complaints a diagnostic work-up in order to offer re-surgery for confirmed recurrent disease.
In the present study, a high (25.2 %) rate of recurrence was found, even though primarily small hernias with a median of 1-cm defect were included. Most hernias were sutured with fast absorbable suture (Polyglactin) (71.2 %). Previously, it has been suggested that the type of suture may influence recurrence rates in groin hernia repairs [15]. This study did not investigate results after small hernia repair using mesh reinforcement, since the aim was not to compare mesh repair with sutured repair. The included patients had primary hernias with small defects (median 1 cm.). We investigated the risk of chronic complaints, if any, after elective repair of very small defects using sutured repair technique. The present results represent data from a uniform selected population of patients undergoing a small and simple elective surgical procedure.
This study was limited by its retrospective design, although with prospective follow-up, and the lack of certain preoperative demographic variables, which may be a significant risk factor for chronic complaints after surgery [15]. Moreover, there is a potential risk of undiagnosed recurrent hernias in the group of patients reporting none to mild chronic symptoms, but it is indeed questionable whether these cases are relevant from a clinical point of view.
A future large-scale study on chronic complaints after the different types of small ventral hernia repair techniques including mesh reinforcement and identification of potential risk factors for chronic pain is needed to approach the optimal repair technique for umbilical and epigastric hernias. Furthermore, more studies are needed to evaluate whether or not the benefit of mesh reinforcement for reduction of hernia recurrence is outbalanced by an increased rate of chronic complaints.
Conclusion
In conclusion, we found a 5.5 % rate of chronic complaints after a simple sutured umbilical or epigastric repair. These complaints were in part associated with recurrence and restricted 8.5–10 % of the patients from work and leisure activities. Our study also indicated that fast absorbable sutures should be avoided to reduce the risk of recurrence after small umbilical or epigastric non-mesh hernia repair.
References
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev 16, CD007781
Witherspoon P, O’Dwyer PJ (2009) Surgeons’ perspectives on options for ventral abdominal hernia repair: results of a postal questionnaire. Hernia 9:259–262
Aslani N, Brown CJ (2010) Does mesh offers an advantage over tissue in the open repair of umbilical hernias? A systematic review and meta-analysis. Hernia 14:455–462. doi:10.1007/s10029-010-0705-9
Arroyo A, García P, Pérez F, Andreu J, Candela F, Calpena R (2001) Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Br J Surg 88:1321–1323. doi:10.1046/j.0007-1323.2001.01893.x
Halm JA, Heisterkamp HF, Weidema WF (2005) Long-term follow-up after umbilical hernia repair: are there risk factors for recurrence after simple and mesh repair. Hernia 9:334–337. doi:10.1007/s10029-005-0010-1
Erritzøe-Jervild L, Christoffersen MW, Helgstrand F, Bisgaard T (2013) Long-term complaints after elective repair for small umbilical or epigastric hernias. Hernia 17:211–215. doi:10.1007/s10029-012-0960-z
Iversen E, Lykke A, Hensler M, Jorgensen LN (2010) Abdominal wall hernia repair with composite ePTFE/polypropylene mesh: clinical outcome and quality of life in 152 patients. Hernia 14:555–560. doi:10.1007/s10029-010-0729-1
Venclauskas L, Silanskaite J, Kiudelis M (2008) Umbilical hernia: factors indicative of recurrence. Med (Kaunas) 44:855–859
Polat C, Dervisoglu A, Senyurek G, Bilgin M, Erzurumlu K, Ozkan K (2005) Umbilical hernia repair with the prolene hernia system. Am J Surg 90:61–64. doi:10.1016/j.amjsurg.2004.09.021
Asolati M, Huerta S, Sarosi G, Harmon R, Bell C, Anthony T (2006) Predictors of recurrence in veteran patients with umbilical hernia: single center experience. Am J Surg 192:627–630. doi:10.1016/j.amjsurg.2006.08.022
Farrow B, Awad S, Berger DH, Albo D, Lee L, Subramanian A, Bellows CF (2008) More than 150 consecutive open umbilical hernia repairs in a major Veterans Administration Medical Center. Am J Surg 196:647–651. doi:10.1016/j.amjsurg.2008.07.018
Sanjay P, Reid TD, Davies EL, Arumugam PJ, Woodward A (2005) Retrospective comparison of mesh and sutured repair for adult umbilical hernias. Hernia 9:248–251. doi:10.1007/s10029-005-0342-x
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95:69–76. doi:10.1093/bja/aei019
Bay-Nielsen M, Perkins FM, Kehlet H, Danish Hernia Database (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7. doi:10.1097/00000658-200101000-00001
Nordin P, Haapaniemi S, Kald A, Nilsson E (2003) Influence of suture material and surgical technique on risk of reoperation after non-mesh open hernia repair. Br J Surg 90:1004–1008
Conflicts of interest
No authors have conflicts of interest regarding the present study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was approved by the Danish Data Protection Agency (reg. no. 2008-58-0020) and the Ethics Committee of the Capital Region (reg.no.: KF07329141), and registered by clinicaltrials.gov (ID: NCT0174740).
Rights and permissions
About this article
Cite this article
Westen, M., Christoffersen, M.W., Jorgensen, L.N. et al. Chronic complaints after simple sutured repair for umbilical or epigastric hernias may be related to recurrence. Langenbecks Arch Surg 399, 65–69 (2014). https://doi.org/10.1007/s00423-013-1119-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1119-9