Abstract
Purpose
The increasing detection of adrenal tumors and the availability of a more sophisticated biochemical work-up leading to rising numbers of sub-clinical Conn’s and Cushing’s syndromes coincide with a rising number of adrenalectomies worldwide. The aim of our study was to report a single institution’s experience with adrenal surgery.
Methods
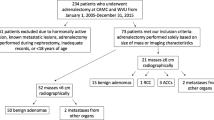
We report data of 528 adrenalectomies, operated at our institution before and after the onset of minimally invasive endoscopic surgery (1986–1994, 1995–2008). Gender, age, indication, imaging, surgical approach, operating time, histology, tumor size, hospital stay, and complications were analyzed retrospectively.
Results
A total of 478 patients underwent adrenal surgery during the time observed. The average number of yearly adrenalectomies increased from 14 to 21 (p = 0.001) after the onset of laparoscopic surgery. Imaging techniques showed a significant shift towards magnetic resonance imaging (p < 0.001) and preoperative assessment of tumor size was significantly correlated to malignancy: 10.8 % (11/102) and 42 % (21/50) of tumors measuring 4–6 cm and ≥6 cm, respectively, were malignant in the final histology report (p < 0.001). Patients operated by minimally invasive endoscopy were significantly younger (mean 49.4 years, p = 0.046), had significantly shorter operating times (mean 118 min, p < 0.001), had shorter hospital stays (mean 7.1 days, p < 0.001), and had less complications (6.9 %, p = 0.004) compared to patients resected through open procedures.
Conclusion
Although adrenalectomy rates increased and minimally invasive endoscopic surgery reduced hospital stay and complications at our institution, the yearly number of procedures was still low with often high surgical complexity. We therefore believe that adrenal surgery remains a highly specialized procedure that should preferably be performed at endocrine surgery centers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The worldwide rise in adrenalectomies has been related to the increasing detection of adrenal tumors and to the availability of minimally invasive endoscopic adrenal surgery [1, 2]. The more frequent use and improvement in the quality of radiographic imaging studies seems to contribute to higher detection rates of incidentally discovered adrenal masses [3, 4], whose normal prevalence is estimated to be 4–7 % of the population [5, 6]. With the introduction of minimally invasive endoscopic adrenal surgery in the mid 1990s [7], the use of traditional open transperitoneal, lateral, and posterior retroperitoneal approaches declined and laparoscopic and retroperitoneoscopic approaches became the standard for endocrine surgery of small and potentially benign adrenal masses [8–10]. Multiple studies have compared open and minimally invasive endoscopic adrenal surgery but are often limited to small patient numbers [9, 11–13]. Reduced postoperative pain and complications, shortened hospital stay, and earlier return to normal activity have been widely accepted as the major advantages of minimally invasive endoscopic adrenalectomy [14, 15], while mortality and morbidity rates are currently reported to be <1 and 8–19 %, respectively [2, 16, 17]. Although minimally invasive endoscopic adrenalectomy for tumors up to 6 cm is in use at many institutions at the present time [18–20], many endocrine surgeons still apply minimally invasive endoscopic procedures only for tumors of suspected benign biology. An open approach is considered to be more radical when malignancy is suspected, and consequently most surgical procedures for suspected or proven malignant tumors of the adrenal gland are still performed through an open approach in many centers [21].
The aim of this study was to report our experience with 528 adrenalectomies performed during more than two decades at our institution and to compare adrenal surgery before and after the onset of minimally invasive endoscopic adrenalectomy.
Methods
Data of patients who underwent adrenal surgery at the Department of General, Visceral, and Pediatric Surgery at the University Hospital Düsseldorf between 1986 and 2008 were collected retrospectively and entered into a database.
Gender, age at surgery, indication for surgery, preoperative diagnostic imaging (ultrasound, computed tomography (CT)), magnetic resonance imaging (MRI), norcholesterol or metajodobenzylguanidine scintigraphy (MIBG), tumor size in imaging, surgical approach (anterior laparotomy, lateral–retroperitoneal or posterior–retroperitoneal approach, transperitoneal or retroperitoneal minimally invasive endoscopy), conversion rate, surgical technique (total or subtotal, unilateral, or bilateral), location of tumor, operative time, histology report, size of tumor, hospital stay, and intra- and postoperative complications were analyzed.
We defined two time periods (1986–1994 and 1995–2008) in order to compare the results of adrenal surgery of over two decades at our institution. The time periods were defined as the era before the onset of minimally invasive endoscopic adrenal surgery (until 1994) and after establishing this technique (from 1995 onward) at our institution. In subgroup analyses, we compared data related to gender, to location of the tumor, to the surgical approach, to tumor size in preoperative imaging, and to the incidence of complications and conversion during minimally invasive endoscopic surgeries. Comparisons between groups were made using the two-tailed t-test for continuous variables and Pearson chi-square test for continuous and categorical variables. A p-value of 0.05 or less was considered as statistically significant. Statistical analysis was performed by using SPSS® software (SPSS Inc., Chicago, IL, USA).
Results
Demographics
A total of 478 patients underwent adrenal surgery at our institution from 1986 to 2008. There were 1.8 times more women (n = 308, 63.5 %) than men (n = 170, 35.1 %) and the mean age at surgery was 51.1 ± 14.6 years. The mean age for men (53.4 ± 14.7 years) was significantly higher than for women (49.8 ± 14.4 years, p = 0.01; CI 95 %, 0.863–6.327). Before the onset of minimally invasive endoscopic adrenal surgery at our institution (1986–1994), the mean age was 50.6 ± 13.5 years compared to 51.3 ± 15 years during the time period after endoscopic surgery was introduced (1995–2008). During the first period, 88 (68.8 %) women with a mean age of 50.2 ± 14.1 and 40 (31.3 %) men with a mean age of 51.5 received adrenal surgery, while in the second time period 220 (62.9 %) women with a mean age of 49.7 ± 14.5 and 130 (37.1 %) men with a mean age of 54 ± 15.4 were operated. The mean age at surgery for men in the second time period was significantly higher than for women (p = 0.009; CI 95 %, 1.095–7.570).
There were more women with minimally invasive endoscopic adrenal surgeries compared to open approaches (p = 0.05), and patients receiving minimally invasive endoscopic adrenalectomies were significantly younger than patients with open procedures (p = 0.046; CI 95 %, 0.052–5.279; Table 1).
Indications to surgery
Table 2 lists all indications for surgery. The most frequent indications to surgery were functioning tumors (n = 280, 58.6 %), including suspicion of pheochromocytoma, primary hyperaldosteronism, hypercortisolism, and other endocrine activity. Among the 18 patients with other functioning tumors were ten patients (2.1 %) who presented with hyperandrogenism due to congenital adrenal hyperplasia, five patients with hyperandrogenemia that was not related to congenital adrenal hyperplasia, two patients suspected to have neuroendocrine tumors, and one patient with excess estrogen secretion. Even though patients with congenital adrenal hyperplasia usually do not require surgery, we sometimes decide to perform an adrenalectomy if specific medical problems of the patients require so. All our patients are discussed in our weekly endocrine meetings and it may occur that surgery is recommended due to a simultaneous risk of malignancy or difficult or unsuccessful pharmacological treatment. Other indications were incidentalomas, suspected primary malignancy, or metastases, and in one case adrenal tuberculosis was suspected. Metastases were only resected after the patient received a current tumor staging and was discussed in our interdisciplinary tumor board meeting. There were no significant differences for the indications to surgery between the two time periods compared. Interestingly, patients with functioning tumors were significantly younger (mean age 47.5 ± 14.4 years) than patients with non-functioning tumors (mean age 54.3 ± 13.3 years) (p < 0.001; CI 95 %, 3.845–9.731).
Preoperative imaging
Preoperative imaging studies included ultrasound, CT, MRI, norcholesterol, or MIBG scintigraphy. Table 3 shows the frequency of the exams during the observed time periods. When both time periods were compared, we found a significant decrease in ultrasound, CT scan, and norcholesterol scintigraphic examinations after 1995 (p < 0.001, p = 0.053, and p = 0.001, respectively), while MRI scans significantly increased (p < 0.001).
Preoperative imaging with assessment of the tumor’s size was available for 386 primary adrenal tumors of patients with no malignant disease in their medical history. These tumors had a median tumor size of 3.6 ± 2.7 cm. There were no differences between the two time periods or between tumor localisation, but we found a significant correlation of the preoperatively measured tumor size and malignancy in the final histology report (Table 4). While only 0.5 % of the tumors <4 cm turned out to be malignant, 10.8 % of tumors between 4 and 6 cm and 42 % of tumors >6 cm were diagnosed malignant in the final histology report (p < 0.001).
Surgical procedures
In 478 patients, a total of 528 adrenal glands were operated in the analyzed time frame. The average number of adrenal surgeries significantly increased from 14 to 25 in the two time periods analyzed (p = 0.019; CI 95 %, 41.92–19.64) (Table 5).
Table 5 shows how frequent adrenalectomies were performed through an anterior laparotomy, through minimally invasive endoscopic approaches (144 (29.7 %) laparoscopic and 30 (6.2 %) retroperitoneoscopic adrenalectomies), and through posterior and lateral–retroperitoneal open approaches during the analyzed time frames. The amount of all open approaches significantly decreased after the onset of minimally invasive endoscopic adrenalectomy (p < 0.001). From 1995 onwards, half of the patients were operated by a minimally invasive endoscopic procedure (144 laparoscopically (41.1 %) and 30 retroperitoneoscopically (8.6 %)). Minimally invasive endoscopic procedures were performed significantly less often for the indication of pheochromocytoma and for the suspicion of malignancy (data not shown).
In 18 cases (10.3 %), minimally invasive endoscopic surgery had to be converted to an open approach, whereby the relative portion of the laparoscopically operated (7/30, 23.3 %) patients was significantly greater than the portion of the retroperitoneoscopically operated (11/144, 7.6 %) patients (p = 0.01). Conversion was due to bleeding (n = 4), cardiovascular arrest (n = 1), and a condition where liver resection of a suspicious liver lesion was required (n = 1). In ten cases, the tumor could not be reached (adhesions) or the tumor was too large. Most of these cases occurred in the first 5 years of our minimally invasive endoscopic era and are probably related to less experience of the surgeons at that time. One operation had to be converted due to technical problems and one due to an injury of the pleural cavity. After a gentle learning curve in the first year of minimally invasive endoscopic adrenal surgery at our institution, the conversion rate could be reduced to median 7.7 % per year.
Table 5 also gives an overview as to how frequent total, subtotal, right, left, or bilateral adrenalectomies were performed in our institution. The number of total left adrenalectomies increased significantly (p = 0.019), while total bilateral procedures decreased significantly (p = 0.001) after 1995. A total of 24 bilateral adrenalectomies were performed for suspected bilateral pheochromocytoma, 18 cases were operated for a therapy-resistant Cushing’s disease, and in four and two cases suspected bilateral metastases and bilateral malignancy, respectively, were the indication for surgery.
The mean operating time of minimally invasive endoscopic adrenal surgeries was significantly shorter than that of open procedures (p < 0.001; Table 1). Although retroperitoneoscopic approaches had a shorter operating time than the transperitoneal laparoscopies, the difference was not statistically significant.
Histology
The histological work-up of all specimen resulted in the postoperative diagnosis of adrenal adenomas, pheochromocytomas, adrenal hyperplasias (micro- and macronodular), adrenal metastases, adrenocortical carcinomas, adrenal angio-/myelolipomas, adrenal cysts, ganglioneuromas, and other histological diagnoses including 13 adrenal glands without any abnormality, four adrenal hematomas or hemangiomas, four adrenal glands with fibrotic and inflammatory changes, one malignant hemangioendothelioma, one adrenal calcification, one intraadrenal bleeding, two neuroendocrine tumors, one inflammatory myofibroblastic tumor, and two paragangliomas without affecting the adjacent adrenal gland. Table 6 gives an overview on the different histological entities in total and for each time period.
The 112 pheochromocytomas included five malignant tumors (4.5 %). Adrenocortical carcinomas were diagnosed in 39 cases (7.5 %) and 46 adrenal glands (8.8 %) were resected because of metastatic disease due to renal cell carcinoma (n = 11, 23.9 %), lung cancer (n = 7, 15.2 %), colon cancer (n = 4, 8.7 %), hepatocellular carcinoma (n = 4, 8.7 %), cancer of unknown primary (n = 4, 8.7 %), lymphoma (n = 3, 6.5 %), endometrial cancer (n = 2, 4.3 %), sarcoma (n = 2, 4.3 %), and neuroblastoma, cervix cancer, breast cancer, malignant melanoma, urothelial cancer, esophagal cancer, neuroendocrine cancer, and thyroid cancer (each n = 1, 2.2 %).
Median tumor size was 4 ± 3.4 cm and there were no significant differences between the compared time eras, but tumors resected by minimally invasive endoscopy were significantly smaller than those resected in open procedures (p < 0.001; CI 95 %, 1.674–3.046; Table 1).
Hospital stay and complications
The mean duration of postoperative hospital stay was 10.9 ± 8.8 days. It decreased significantly from 13.4 ± 9.8 days during the first time period to 9.9 ± 8.3 days during the second period (p < 0.001; CI 95 %, 1.679–5.212). Patients after minimally invasive endoscopic adrenal surgeries (7.1 ± 4.3 versus 13 ± 10 days, p < 0.001; CI 95 %, 4.335–7.460), patients without postoperative complications (9.4 ± 55 versus 17.4 ± 15.4 days, p < 0.001; CI 95 %, 6.163–9.976), and patients without conversion during a minimally invasive endoscopic procedure (6.7 ± 3.9 versus 10.7 ± 4.9 days, p = 0.004; CI 95 %, 1.463–6.473) had a significantly shorter hospital stay, but no difference could be observed between the transperitoneal and retroperitoneal minimally invasive endoscopic procedures. There were 11 (2.3 %) intraoperative and 51 (10.7 %) major postoperative complications. Adrenal insufficiency developed in seven cases (1.4 %) and presented as Addisonian Crisis in four of them (0.8 %) despite glucocorticoid replacement therapy. A total of 16 patients (3.3 %) developed mild wound healing complications. Among the intraoperative complications, three bleedings and three cardiovascular complications occurred in the open group. Two bleedings happened during multivisceral resections and one (spleen rupture) during the resection of bilateral pheochromocytomas. One asystoly and one atrial fibrillation occurred during multivisceral tumor resections and one hypertensive crisis happened during surgery in a patient with pheochromocytoma. In the minimally invasive endoscopic surgery group, a total of five intraoperative complications occurred. Three led to conversion to an open approach because of one splenic rupture, one uncontrollable bleeding, and one asystoly during resection of a pheochromocytoma. Two were pneumothoraces that could be drained intraoperatively. Ten of the major postoperative complications occurred after anterior laparotomies of multivisceral resections and were not related to adrenal surgery per se. Eleven postoperative complications occurred after anterior laparotomies, two after posterior retroperitoneal laparotomy, two after lateral retroperitoneal laparotomy, and ten after minimally invasive endoscopic procedures. Seven patients received reoperations due to postoperative complications. There was no difference in complication rates between the two time periods, but rates of surgical complications could be significantly reduced when minimally invasive endoscopic procedures were used (Table 1). There were also significantly less wound healing complications (1.2 versus 4.6 %, p = 0.007, chi-square test) and less non-surgical complications (1.7 versus 4.3 %, p = 0.007, chi-square test) after minimal invasive endoscopic adrenalectomy. No differences were detected when transperitoneal and retroperitoneal minimally invasive endoscopic procedures were compared. No operative or postoperative deaths have been reported.
Discussion
During the recent years, many reports showed an increase in adrenal surgery that was most likely related not only to the more frequent detection of adrenal tumors in high resolution imaging but also to the increasing use of minimally invasive endoscopic procedures [1, 2, 5, 22, 23]. Better imaging techniques and probably also improved diagnostic tests are responsible for the rise in adrenal tumor detection, whereas less morbidity of minimally invasive endoscopic adrenalectomy makes the procedure more tolerable for many patients [1, 4]. Over the past years, minimally invasive endoscopic resection of adrenal tumors became the well-recognized gold standard of the disease [24, 25]. Although the contraindication of suspected malignancy has been overcome in parts and many experts nowadays perform laparoscopic or retroperitoneoscopic adrenalectomies for small malignant lesions, this remains controversial among endocrine specialists and many surgeons still perform open adrenalectomies when malignancy is suspected [26, 27]. So far, a major limitation in adrenal surgery is the relatively small number of surgeries per year with very few specialized centers and endocrine surgeons worldwide. Morbidity is still reported to be up to 19 % and only very few clinical studies have been published in the literature reporting long-term data from high-volume centers and high-volume surgeons. This clearly limits the significance of smaller studies and demands prospective multi-center analyses with higher patient numbers [14, 28, 29].
Our report of 22 years of experience with adrenal surgery at a single institution was described to compare the era before and after the onset of minimally invasive endoscopic adrenalectomy. Similar patient characteristics regarding the ratio of female-to-male patients and age at the time of surgery have been reported by other authors, suggesting that the composition of our cohort is comparable [2, 5, 22, 30]. Although the number of surgeries increased over time, we were not able to relate this to an increase of incidentalomas at our institution. However, since adrenal incidentalomas are hormonally inactive adrenocortical tumors in the majority, our retrospective analysis of archived patient’s surgery data may have very likely missed cases of incidentally discovered adrenal masses. Nevertheless, we saw differences in other indications when the time before and after the onset of minimally invasive endoscopic surgery was compared. In accordance to Sidhu et al. who described an increase in aldosterone-producing adenomas recommended for surgery [28], we also saw a significant increase in patients with primary hyperaldosteronism as indication for adrenalectomy. This increase might be due to a better understanding of the disease and due to the availability of more sensitive diagnostic tools, including application of the aldosterone-to-rennin ratio in the screening for primary aldosteronism or the recently described SUSPPUP ratio [31]. We also saw a slight decrease in indications for pheochromocytoma and hypercortisolism. Indications for suspected adrenal metastasis almost doubled and reached statistical significance in our cohort. Surgery for metastatic disease became more common in the last years and might provide an improvement in the quality of life for patients if the indication for surgery is properly evaluated. It has been described that lung cancer, breast cancer, melanoma, hypernephroma, and other malignancies frequently metastasize to the adrenal gland and that patients with single and resectable metastasis eventually benefit from their removal [32–34]. Due to the increasingly improving follow-up of tumor patients, the number of detected adrenal masses suspected to be metastases increased significantly over the past years. One study was able to show that 70 % of resected adrenal tumors in oncologic patients turned out to be metastases [35]. In what way these patients really benefit from the procedure still needs to be evaluated, but it most likely depends on the kind of primary malignancy and on coexisting tumor-related factors influencing the patient’s course at the time of surgery.
Since MRI is now available for routine imaging studies in more hospitals, the number of examinations grew constantly in the preoperative evaluation of adrenal tumors [36]. We observed not only a significant increase in MRI after the onset of endoscopic surgery but also a significant decrease in CT studies, ultrasound, and norcholesterol scintigraphy. Nevertheless, CT is still used predominantly for preoperative evaluation of adrenal tumors, and in our cohort the majority of patients received this imaging technique. Although most authors and the NIH Consensus and State-of-the-Science statements recommend to consider adrenalectomy for lesions of the adrenal gland larger than 4 cm, others still consider close follow-up as a reasonable approach [37–42]. In our cohort, the rate of malignant tumors was significantly correlated to the tumor size measured in preoperative imaging. The use of high-resolution imaging along with the application of special radiologic protocols and criteria to exactly measure and characterize adrenal tumors seems to be crucial for a better preoperative discrimination of benign and malignant adrenal lesions.
The increasing use of minimally invasive endoscopic adrenalectomy after 1995 at our institution occurred at the expense of all open procedures, and although we observed the most commonly known advantages of minimally invasive surgery, we did not reach the percentage rate usually reported for minimally invasive endoscopic adrenal surgery [14, 43, 44]. This might be due to the fact that some surgeons at our institution preferred open surgery as the gold standard for any suspected malignant disease. Additionally, a high-volume university hospital in Germany like our institution usually treats many patients with multiple comorbidities and prior surgeries that make minimally invasive endoscopic approaches more difficult.
Nevertheless, we now try to always perform retroperitoneoscopoic adrenalectomies if feasible, also in the case of reoperation. We believe that this faster and less difficult approach is also easier to learn for young surgeons with little experience on minimally invasive endoscopy. [45]
As expected, minimally invasive endoscopic adrenalectomy significantly decreased the patients’ operating times, postoperative hospital stay, and complication rates in our hospital. Our hospital stay is still much longer than in other reports, but it has to be taken into account that this is mostly related to our health care system. Certain cases only bring the maximum profit for the hospital if they stay for a defined time period in the hospital.
Women and patients of younger age received minimally invasive endoscopic surgery for adrenal diseases significantly more often than men and older patients, an observation consistent with the report of Lee et al. [9]. The fact that younger patients also had significantly higher number of functioning tumors is most likely due to the fact that functioning tumors lead to earlier symptoms and are therefore detected earlier in life, while non-functioning tumors are often detected by coincidence in imaging studies performed for other medical problems related to increasing age. Our initial minimally invasive endoscopic cohort was probably biased for non-pheopchromocytomas and non-malignant (big) tumors because those tumors were suspected to be more difficult to resect. Currently, we do resect both entities by minimally invasive endoscopy at our institution and the significant difference observed in our retrospective analysis cannot be detected anymore.
Complication rates after adrenalectomy have been reported to be 8–19 % [9, 22, 46]. With 7.5 % significant complications after endoscopic adrenalectomy and a conversion rate of 5 %, Henry et al. reported similar data to our results [47]. In fact, minimally invasive endoscopic adrenalectomy could significantly reduce surgical, non-surgical, and wound healing complications in our patients. It has been discussed in the literature that not only the surgeon’s experience but also the size of the hospital correlate with outcome after adrenalectomy, suggesting that high-volume surgeons and high-volume hospitals perform better [5]. In addition, tumor size, comorbidities, and previous abdominal surgery among other factors influence the patient’s outcome [48]. These inter-individual risk factors make it difficult to actually compare different cohorts and only prospective multi-center studies could help to better understand all factors predicting outcome after adrenalectomy. Our relatively high postoperative complication rate in patients who were operated by open procedures might be explained by the high amount of multivisceral resections of malignant and metastatic tumors in this group. Nevertheless, Gumbs et al. also reported a mean complication rate of 8.9 % (2.9–16 %) in 2,565 adrenalectomies analyzed in a meta-analysis of 19 papers, suggesting a big inter-surgeon and inter-hospital variety [15]. With our experience of over 500 adrenalectomies performed, we believe that it is always worth to consider the open procedure for complicated and advanced cases, appreciating that minimally invasive endoscopic surgery clearly provides the best rehabilitation and quality of life for the majority of the patients.
Conclusion
The introduction of minimally invasive endoscopic adrenal surgery changed the field of adrenalectomy. A rise in hyperaldosteronism and suspected adrenal metastasis significantly increased the number of adrenalectomies performed at our institution each year. Minimally invasive endoscopic adrenalectomy clearly decreased operating times, hospital stay, and complication rates in our patients as expected. Nevertheless, adrenal surgery remains a highly specialized procedure with a relatively high incidence of surgical and non-surgical complications. Advanced malignancies, hormone-producing tumors, and unexpected anatomic difficulties demand experienced endocrine surgeons at specialized endocrine centers. Our herein reported data of 528 adrenalectomies of a single institution before and after the beginning of endoscopic endocrine surgery might be a useful reference for future case analyses and epidemiologic studies.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MIBG:
-
Metajodobenzylguanidine
- NIH:
-
National Institutes of Health
References
Gallagher SF, Wahi M, Haines KL, Baksh K, Enriquez J, Lee TM et al (2007) Trends in adrenalectomy rates, indications, and physician volume: a statewide analysis of 1816 adrenalectomies. Surgery 142(6):1011–1021, discussion 1011-1021
Young WF Jr (2007) Clinical practice. The incidentally discovered adrenal mass. N Engl J Med 356(6):601–610
Beuschlein F (2007) Adrenal incidentalomas: presentation and clinical work-up. Horm Res 68(Suppl 5):191–194
Bovio S, Cataldi A, Reimondo G, Sperone P, Novello S, Berruti A et al (2006) Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest 29(4):298–302
Park HS, Roman SA, Sosa JA (2009) Outcomes from 3144 adrenalectomies in the United States: which matters more, surgeon volume or specialty? Arch Surg 144(11):1060–1067
Song JH, Chaudhry FS, Mayo-Smith WW (2008) The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol 190(5):1163–1168
Gagner M, Lacroix A, Bolte E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327(14):1033
Jacobs JK, Goldstein RE, Geer RJ (1997) Laparoscopic adrenalectomy. A new standard of care. Ann Surg 225(5):495–501, discussion 501-492
Lee J, El-Tamer M, Schifftner T, Turrentine FE, Henderson WG, Khuri S et al (2008) Open and laparoscopic adrenalectomy: analysis of the National Surgical Quality Improvement Program. J Am Coll Surg 206(5):953–959, discussion 959-961
Smith CD, Weber CJ, Amerson JR (1999) Laparoscopic adrenalectomy: new gold standard. World J Surg 23(4):389–396
Hallfeldt KK, Mussack T, Trupka A, Hohenbleicher F, Schmidbauer S (2003) Laparoscopic lateral adrenalectomy versus open posterior adrenalectomy for the treatment of benign adrenal tumors. Surg Endosc 17(2):264–267
Imai T, Kikumori T, Ohiwa M, Mase T, Funahashi H (1999) A case–controlled study of laparoscopic compared with open lateral adrenalectomy. Am J Surg 178(1):50–53, discussion 54
Yousef HB, Al Zahrani A, Ahmed M, Al Arifi A, Mahfouz A, Hussain R et al (2003) Laparoscopic vs. open adrenalectomy: experience at King Faisal Specialist Hospital and Research Centre, Riyadh. Ann Saudi Med 23(1-2):36–38
Brunt LM (2006) Minimal access adrenal surgery. Surg Endosc 20(3):351–361
Gumbs AA, Gagner M (2006) Laparoscopic adrenalectomy. Best Pract Res Clin Endocrinol Metab 20(3):483–499
Brunaud L, Kebebew E, Sebag F, Zarnegar R, Clark OH, Duh QY (2006) Observation or laparoscopic adrenalectomy for adrenal incidentaloma? A surgical decision analysis. Med Sci Monit 12(9):CR355–CR362
Gonzalez R, Smith CD, McClusky DA 3rd, Ramaswamy A, Branum GD, Hunter JG et al (2004) Laparoscopic approach reduces likelihood of perioperative complications in patients undergoing adrenalectomy. Am Surg 70(8):668–674
Rosoff JS, Raman JD, Del Pizzo JJ (2008) Laparoscopic adrenalectomy for large adrenal masses. Curr Urol Rep 9(1):73–79
McCauley LR, Nguyen MM (2008) Laparoscopic radical adrenalectomy for cancer: long-term outcomes. Curr Opin Urol 18(2):134–138
Eto M, Hamaguchi M, Harano M, Yokomizo A, Tatsugami K, Naito S (2008) Laparoscopic adrenalectomy for malignant tumors. Int J Urol 15(4):295–298
Kuruba R, Gallagher SF (2008) Current management of adrenal tumors. Curr Opin Oncol 20(1):34–46
Toniato A, Boschin I, Bernante P, Foletto M, Guolo AM, Pelizzo MR et al (2008) Factors influencing the rising rates of adrenal surgery: analysis of a 25-year experience. Surg Endosc
Singh PK, Buch HN (2008) Adrenal incidentaloma: evaluation and management. J Clin Pathol 61(11):1168–1173
Kotzampassakis N, Maweja S, Defechereux T, Meurisse M, Hamoir E (2005) Surgical management of adrenal tumours. Lessons from a 10 years personal experience. Acta Chir Belg 105(2):156–160
Gil-Cardenas A, Cordon C, Gamino R, Rull JA, Gomez-Perez F, Pantoja JP et al (2008) Laparoscopic adrenalectomy: lessons learned from an initial series of 100 patients. Surg Endosc 22(4):991–994
Zafar SS, Abaza R (2008) Robot-assisted laparoscopic adrenalectomy for adrenocortical carcinoma: initial report and review of the literature. J Endourol 22(5):985–989
Kirshtein B, Yelle JD, Moloo H, Poulin E (2008) Laparoscopic adrenalectomy for adrenal malignancy: a preliminary report comparing the short-term outcomes with open adrenalectomy. J Laparoendosc Adv Surg Tech A 18(1):42–46
Sidhu S, Bambach C, Pillinger S, Reeve T, Stokes G, Robinson B et al (2002) Changing pattern of adrenalectomy at a tertiary referral centre 1970–2000. ANZ J Surg 72(7):463–466
Kasperlik-Zaluska AA, Otto M, Cichocki A, Roslonowska E, Slowinska-Srzednicka J, Zgliczynski W et al (2008) 1,161 patients with adrenal incidentalomas: indications for surgery. Langenbecks Arch Surg 393(2):121–126
Schreinemakers JM, Elias SG, Borel Rinkes IH (2008) Retroperitoneal endoscopic versus conventional open adrenalectomy: a cost-effectiveness analysis. J Laparoendosc Adv Surg Tech A 18(5):707–712
Willenberg HS, Kolentini C, Quinkler M, Cupisti K, Krausch M, Schott M et al (2009) The serum sodium to urinary sodium to (serum potassium)2 to urinary potassium (SUSPPUP) ratio in patients with primary aldosteronism. Eur J Clin Invest 39(1):43–50
Luketich JD, Burt ME (1996) Does resection of adrenal metastases from non-small cell lung cancer improve survival? Ann Thorac Surg 62(6):1614–1616
Kim SH, Brennan MF, Russo P, Burt ME, Coit DG (1998) The role of surgery in the treatment of clinically isolated adrenal metastasis. Cancer 82(2):389–394
Higashiyama M, Doi O, Kodama K, Yokouchi H, Imaoka S, Koyama H (1994) Surgical treatment of adrenal metastasis following pulmonary resection for lung cancer: comparison of adrenalectomy with palliative therapy. Int Surg 79(2):124–129
Frilling A, Tecklenborg K, Weber F, Kuhl H, Muller S, Stamatis G et al (2004) Importance of adrenal incidentaloma in patients with a history of malignancy. Surgery 136(6):1289–1296
Honigschnabl S, Gallo S, Niederle B, Prager G, Kaserer K, Lechner G et al (2002) How accurate is MR imaging in characterisation of adrenal masses: update of a long-term study. Eur J Radiol 41(2):113–122
NIH (2002) NIH State-of-the-Science Conference statement for the management of the clinically inapparent adrenal mass (incidentaloma). Bethesda, February 4–6, 2002
Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR (2004) The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev 25(2):309–340
Ilias I, Sahdev A, Reznek RH, Grossman AB, Pacak K (2007) The optimal imaging of adrenal tumours: a comparison of different methods. Endocr Relat Cancer 14(3):587–599
Herrera MF, Grant CS, van Heerden JA, Sheedy PF, Ilstrup DM (1991) Incidentally discovered adrenal tumors: an institutional perspective. Surgery 110(6):1014–1021
Grumbach MM, Biller BM, Braunstein GD, Campbell KK, Carney JA, Godley PA et al (2003) Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med 138(5):424–429
Brunt LM, Moley JF (2001) Adrenal incidentaloma. World J Surg 25(7):905–913
Cyriac J, Weizman D, Urbach DR (2006) Laparoscopic adrenalectomy for the management of benign and malignant adrenal tumors. Expert Rev Med Devices 3(6):777–786
Ariyan C, Strong VE (2007) The current status of laparoscopic adrenalectomy. Adv Surg 41:133–153
Walz MK, Peitgen K, Hoermann R, Giebler RM, Mann K, Eigler FW (1996) Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg 20(7):769–774
Gupta PK, Natarajan B, Pallati PK, Gupta H, Sainath J, Fitzgibbons RJ Jr (2011) Outcomes after laparoscopic adrenalectomy. Surg Endosc 25(3):784–794
Henry JF, Defechereux T, Raffaelli M, Lubrano D, Gramatica L (2000) Complications of laparoscopic adrenalectomy: results of 169 consecutive procedures. World J Surg 24(11):1342–1346
Tessier DJ, Iglesias R, Chapman WC, Kercher K, Matthews BD, Gorden DL et al (2009) Previously unreported high-grade complications of adrenalectomy. Surg Endosc 23(1):97–102
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lachenmayer, A., Cupisti, K., Wolf, A. et al. Trends in adrenal surgery: institutional review of 528 consecutive adrenalectomies. Langenbecks Arch Surg 397, 1099–1107 (2012). https://doi.org/10.1007/s00423-012-0973-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-0973-1