Abstract
Background
In this study, we ask between patients with graft failure listed for retransplant and patients with hepatocellular carcinoma (HCC) outside of UCSF criteria, who has the greater survival benefit with transplantation?
Methods
This is a retrospective analysis, of liver transplant (LT) patients, done between February 2002 and December 2009 at our center. Patients were included in the “extended HCC” group if their tumor was pathologically beyond UCSF criteria at LT and in the “redo” group if they underwent LT for graft failure occurring more than 3 months after the initial LT. Extended criteria donors (ECDs) were defined as donors above 70 years old, DCD, serology positive for HCV, and split grafts.
Results
There were 25 redos and 37 extended HCC patients. Use of ECDs or high donor risk index organs was associated with poor outcome in both groups (P = 0.005). Overall, the extended HCC population had a much better survival than redos, both at 1 and 3 years.
Conclusion
These two very different but high risk patient populations have very different survival rates. At a time where regulatory agencies demand more and more with regards to transplant outcomes, we think the transplant community has to reflect on whether allocation justice and fair access to transplant are respected if we start allocating organs based on outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number one rate limiting factor to liver transplantation is organ shortage. This sad reality we face forces health care professionals to police organ allocation and sometimes question graft acceptance based on predicted patient outcome. For some patients, imminent liver transplantation is the only hope for even short-term survival. Because these patients are in desperate need of an organ, they often receive a liver of marginal quality owed to the urgency of the situation and irrespective of their status on the list. In an era of organ shortage and outcome monitoring, organ allocation can become complicated, and a prediction of the allograft’s outcome is often included in the process. In this study, we ask between patients with late (more than 3 months post transplant) graft failure listed for retransplant and patients with hepatocellular carcinoma (HCC) outside of University of California, San Francisco (UCSF) criteria, two controversial groups, who has the greater survival benefit with transplantation? We decided to study these two groups of liver transplant recipients with patient and graft survival known to be inferior to the rest of the transplant population to see which group would benefit the most from transplantation and which of the two groups maximizes the graft’s potential. This analysis is merely a hypothetical mental exercise: can we direct organ allocation based on predicted outcome?
The only therapeutic option for patients with a failing liver allograft is retransplantation. Early liver retransplantation for patients with early graft dysfunction or primary nonfunction is generally accepted and rarely questioned; late retransplantation however, more than 3 months following the initial transplant, is often criticized. Prior studies have showed worse patient and graft survival after retransplantation when compared to primary grafting [1–8]. The inferior outcome in this special group of patients has led many to question the rightfulness of late hepatic retransplantation on both economic and ethical grounds [9–12]. Is allocating a standard criteria donor (SCD) graft to retransplant candidates fair given that they already had a precious and rare liver graft and that their outcome is known to be inferior to the primary transplant recipients? Shouldn’t the next patient get his chance now? Should only the late retransplant candidates get access to extended criteria donors (ECDs)? If so, is the retransplant outcome acceptable with ECDs? Are they the group that benefits the most from them? The principal group that desires access to extended criteria donor grafts now is the subset of patients with unresectable HCC listed for transplantation but with tumors outside of Milan criteria (Milan criteria: single lesion ≤5 cm, up to three separate lesions, none larger than 3 cm, no evidence of gross vascular invasion, no regional nodal or distant metastases) [13]. These patients only usually get access to transplantation via ECDs as they are not eligible for exemption points and their model of end-stage liver disease (MELD) score does not reflect their disease severity, waiting for SCD would equal death. Therefore, as an exercise in organ sharing strategy and with a desire to maximize graft potential we ask: can we direct organ allocation based on outcome? If yes, who best benefits from transplantation: patients with HCC outside of Milan criteria or retransplants?
Materials and methods
This is a retrospective analysis of all the liver transplant patients at our center between February 2002 and December 2009. Patients were included in the “extended HCC” group if they had a diagnosis of HCC, their tumor was radiologically or pathologically beyond UCSF criteria, and they were transplanted within the study period. They were included in the “retransplant” group if they underwent liver transplantation within the study period for graft failure occurring more than 3 months after the initial transplant. Patients with primary graft nonfunction were specifically excluded from this group. These patients were identified by retrospective review of our transplant patient tracking database. All the included patients’ medical charts were searched for the following information: age, sex, date of transplant, etiology of pretransplant liver failure, liver donor demographics, use of ECDs, donor risk index (DRI) value, date of last follow-up, graft failure, and death.
ECDs were defined as donors above 70 years old, deceased after cardiac death, steatosis more than 30%, sodium more than 170, serology positive for hepatitis C virus (HCV), and split grafts. The DRI was calculated according to Feng et al. [14]. Graft failure was defined as death secondary to liver failure or retransplantation.
Descriptive statistics are expressed as mean (SD) or median. Chi-square test or Fisher’s test, where appropriate, was used for univariate comparisons. For univariate survival analysis, plots were made by the Kaplan–Meier method and comparisons by the logrank test. The Cox model with the determination of the hazard ratio was applied to evaluate the risk associated with prognostic variables. Differences were considered significant at P = 0.05. Perioperative death was included in the survival analysis. All statistical analyses were performed using MedCalc v11.4.4. Follow-up data were collected up until February 1, 2011.
Results
Between February 1, 2002 and December 31, 2009, we performed a total 497 liver transplants; 62 of these patients were included in the analysis, 25 retransplants and 37 extended HCC patients. The two groups were not different in terms of demographics, but the MELD at transplant was higher in the retransplant group than in the extended HCC group (32 vs 17, P < 0.01). The use of ECDs was greater in the extended HCC group, and the DRI was also significantly higher in the extended HCC group (Table 1). The causes that lead to graft failure and need for graft replacement in the retransplantation group were varied (17 for recurrent disease (15 recurrent hepatitis C, 1 recurrent primary biliary cirrhosis, 1 recurrent autoimmune hepatitis), 3 for chronic rejection, and 5 for secondary sclerosing cholangitis).
The median survival for the retransplant group was 17 months ranging from 0 to 72 months; 13 patients died (52%), 7 of them died within 1 month of retransplantation in the perioperative period (1 from primary graft nonfunction, 2 from sepsis, 1 from pulmonary embolism, 1 from hemothorax, and 2 from hepatic artery complications). 3 patients died of graft failure from recurrent hepatitis C at 15, 16, and 31 months post retransplantation, 2 patients died of sepsis 2 and 11 months post retransplantation, and 1 patient died of recurrent HCC 8 months post retransplantation. Twelve patients are alive and well and being followed from 30 to 72 months post retransplantation.
The median survival for the extended HCC group was 45 months ranging from 1 to 106 months post transplantation; 13 patients died (35%), 2 of sepsis at 1.6 and 1.9 months, 9 of recurrent HCC at a mean time of 24.9 months post transplantation (ranging from 5.5 to 58.8 months), and 2 of graft failure (1 of secondary to recurrent HCV) at 9 and 30 months post transplantation.
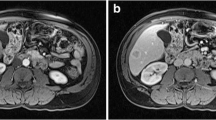
The 1- and 3-year survival for the retransplant group was 60% and 47%, respectively, similar to what is reported in Scientific Registry of Transplant Recipients (SRTR) and in the literature. Analysis for the use of ECDs in the retransplant population showed that the 1- and 3-year survival for the retransplant group who received SCDs was 62% and 53%, respectively (vs 50% and 25% for those who received ECDs). The 1- and 3-year survival for the extended HCC group was superior (81% and 72%), respectively, and this was superior to the retransplant group in a statistically significant manner (P < 0.05) (Fig. 1). Similarly, when this group was analyzed for the use of ECDs, the 1- and 3-year survival was 90% and 84%, respectively, for patients who received SCD graft vs 72% and 61%, respectively, for those who were allocated an ECD graft (P < 0.05) (Fig. 2). Univariate analysis identified the use of ECDs (P = 0.01) and DRI greater than 1.9 (P > 0.05), but not HCV (P = 0.4) as overall markers of poor prognosis. On multivariate analysis, MELD > 30 and the use of ECDs were identified as variables which significantly affect survival, but not HCV or DRI.
Discussion
Our results show that liver transplantation for extended criteria HCC has far superior outcome than retransplantation for any cause. Moreover, retransplant patients do worse than the first transplant patients overall, but they actually do much worse with extended criteria organs, whereas patients with extended criteria HCC do relatively well with such organs. The fact that our results show that MELD score at transplant above 30 negatively affects outcomes is confounding as only 3 extended HCC patients had a MELD score beyond 30. Moreover, the higher MELD score in the redo group compared with the HCC group may be a factor contributing to the difference in outcomes; however, we do not believe it is the sole reason.
There is unfortunately no other option for patients with failing liver allograft than retransplantation. The worse patient and graft survival than primary liver transplantation has led many to question the rationale for this procedure for ethical and economical reasons [9]. These concerns are even more relevant when discussing transplant access for different group of patients. Many feel that this cohort of patients has already been provided access to transplantation, and it should now be another’s turn. In the MELD era, the cohort of patients suffering form HCC is also on the spotlights in relation to access to transplant. Patients with tumors within Milan criteria have been given priority on the waiting list, and as a result, the number of patients who undergo transplantation for HCC is rising. [15] Liver transplantation offers very good outcomes to those with small tumors confined only to the liver [13]. There is however still a debate how aggressively patients should be considered for transplantation, with some regions being more aggressive than others [16]. Patients with tumors beyond Milan criteria and unresectable disease confined to the liver are being considered for liver transplantation in various centers, but are not receiving priority on the waiting list; their score reflects the quality of their liver function, and not their imminent mortality.
To access transplantation, with reported dropout rates of up to 30% while waiting for a donor even for patients with small tumors, extended HCC patients must consider ECDs or live donor liver transplant [17, 18]. When considering liver transplantation for extended HCC patients, there is no generally accepted rule, but many think that a predicted 5-year survival of at least 50% should be considered [19]. What of retransplants then? In an era where organ shortage is at a critical stage, maximizing graft life is in everyone’s mind, and one wonders, must we then also change the rules of access to transplant [20]?
For HCC patients within Milan criteria, UNOS has changed waitlist priority thereby modifying access to transplantation in order to decrease waitlist mortality; why stop there? Would it be fair? Are we directing organ allocation based on outcome? Our data, which conform with SRTR data and the related literature, show that extended HCC patients achieve acceptable long-term survival with liver transplantation, even with marginal organs. On the other hand, retransplants do really poorly with a lesser quality organ and do really well with a good quality graft, probably owing to the increased complexity and length of the surgery. This also is consistent with the literature. Therefore, we question, would it be fair to mainly allocate the best grafts to those who already had one? Specifically, when will we know that patients like the extended HCC cohort do well with ECDs but do even better with SCDs (Table 2)? These are difficult questions and decisions often need to be made on a case by case basis.
Many centers are already tailoring organ allocation when dealing with patients with hepatitis C; for example, most programs do not offer marginal grafts to these patients as many reports show earlier disease recurrence and lower graft survival than with SCDs [21, 22]. But the transplant community needs to discuss whether we want to continue to provide universal access (across the board of diseases and indications) and deal with graft failures as they come or whether we should architect an allocation system that considers maximization of graft years, a LYFT [23] of the liver if you will.
Conclusion
This small single center analysis really is just an excuse for the greater discussion. As patients are dying on the waitlist, it is not always feasible to wait for the perfect organ. Organ shortage has become so critical, and more and more marginal organs are being considered for transplantation. However, not every cohort of patients does well with fragile organs. Our results show that ECDs should not be considered for retransplant candidates, as is already well known, but when the organs are rare, low chances sometimes sound better than no chances. When it comes to choosing a patient for an ECD, HCCs outside of UCSF criteria have a very good outcome and truly have a greater benefit from transplantation than retransplant candidates. It is true that HCC patients already have a great access to liver transplantation, but they also have a very good outcome with organs that other patients do not tolerate as well. Very extensive evaluation of transplant outcome for HCC has been done, and very restrictive criteria are imposed upon HCC patients awaiting transplantation. It seems that other subgroups of patients with transplant outcomes demonstrated to be lower than expected do not receive such a restrictive access to treatment. At the time of an organ offer, the decision to accept either the risk of transplantation or the risk of waiting remains with the transplant surgeon. The decision requires parameters about the quality of the particular graft being offered and the risk of death from progressive liver disease if the current offer is declined. Since the quality of the donor organ and the medical condition of the recipient is such an important component of this decision, it appears to us that the transplant community should reflect on the following questions: Are restrictions to transplantation applied homogeneously among the different risk groups? Are the restrictions to transplantation based on outcome? Once a disease has an established therapy, does it matter that a patient subgroup has a greater benefit or better outcome if no other therapy exists? Does that answer change when resources are scarce?
References
Shawn B, Gordon R, Iwatsuki S, Starzl T (1985) Hepatic retransplantation. Transplant Proceedings 17(1):264–271
Markmann JF et al (1997) Long-term survival after retransplantation of the liver. Ann Surg 226(4):408–418, discussion 418-20
Ringe B, Neuhaus P, Lauchart W, Pichlmayr R (1986) Experience with hepatic retransplantation. Transplant Proceedings 18(5):1207–1209
Morel P et al (1991) Liver retransplantation in adults: overall results and determinant factors affecting the outcome. Transplant Proc 23(6):3029–3031
Anthuber M et al (1992) Liver retransplantation—indications, frequency, results. Transplant Proc 24(5):1965–1966
Lemmens HP et al (1993) Comparison of perioperative morbidity following primary liver transplantation and liver retransplantation. Transplant Proc 25(2):1923–1924
Fangmann J et al (1993) Hepatic retransplantation: the Hannover experience of two decades. Transplant Proc 25(1 Pt 2):1077–1078
D’Alessandro AM et al (1993) Retransplantation of the liver—a seven-year experience. Transplantation 55(5):1083–1087
Evans RW et al (1993) Is retransplantation cost effective? Transplant Proc 25(1 Pt 2):1694–1696
Jurim O, Busuttil RW (1996) Retransplantation. In: Bussutil RK, Klintman GB (eds) Transplantation of the liver. Saunders, Philadelphia, pp 497–502
Ubel PA, Arnold RM, Caplan AL (1993) Rationing failure. The ethical lessons of the retransplantation of scarce vital organs. Jama 270(20):2469–2474
Powelson JA et al (1993) Hepatic retransplantation in New England—a regional experience and survival model. Transplantation 55(4):802–806
Mazzaferro V et al (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334(11):693–699
Feng S et al (2006) Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant 6(4):783–790
Yao FY et al (2004) Liver transplantation for hepatocellular carcinoma: lessons from the first year under the Model of End-Stage Liver Disease (MELD) organ allocation policy. Liver Transpl 10(5):621–630
Yao FY et al (2001) Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 33(6):1394–1403
Soejima Y et al (2007) Extended indication for living donor liver transplantation in patients with hepatocellular carcinoma. Transplantation 83(7):893–899
Gondolesi GE et al (2004) Adult living donor liver transplantation for patients with hepatocellular carcinoma: extending UNOS priority criteria. Ann Surg 239(2):142–1429
Zimmerman MA et al (2008) Recurrence of hepatocellular carcinoma following liver transplantation: a review of preoperative and postoperative prognostic indicators. Arch Surg 143(2):182–188, discussion 188
Brown RS et al (2004) Liver and intestine transplantation. Am J Transplant 4(Suppl 9):81–92
Ghobrial RM et al (2001) A 10-year experience of liver transplantation for hepatitis C: analysis of factors determining outcome in over 500 patients. Ann Surg 234(3):384–393, discussion 393-394
Yagci G et al (2008) The impact of donor variables on the outcome of orthotopic liver transplantation for hepatitis C. Transplant Proc 40(1):219–223
Wolfe RA et al (2008) Calculating life years from transplant (LYFT): methods for kidney and kidney-pancreas candidates. Am J Transplant 8(4 Pt 2):997–1011
Conflicts of interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rochon, C., Sheiner, P., Mahadevappa, B. et al. Can we direct organ allocation based on predicted outcome? Hepatocellular carcinoma outside of UCSF criteria or retransplant?. Langenbecks Arch Surg 397, 711–715 (2012). https://doi.org/10.1007/s00423-012-0910-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-0910-3