Abstract
Purposes
Unfortunately, surgical site infections (SSIs) are a quite common complication and represent one of the major causes of postoperative morbidity and mortality, and may furthermore lead to enormous additional costs for hospitals and health care systems.
Methods
In order to determine the estimated costs due to SSIs, a MEDLINE search was performed to identify articles that provide data on economic aspects of SSIs and compared to findings from a matched case-control study on costs of SSIs after coronary bypass grafting (CABG) in a German tertiary care university hospital.
Results
A total of 14 studies on costs were found. The additional costs of SSI vary between $3,859 (mean) and $40,559 (median). Median costs of a single CABG case in the recently published study were $49,449 (€36,261) vs. $18,218 (€13,356) in controls lacking infection (p < 0.0001). The median reimbursement from health care insurance companies was $36,962 (€27,107) leading to a financial loss of $12,482 (€9,154) each.
Conclusion
Costs of SSIs may almost triple the individual overall health care costs and those additional charges may not be sufficiently covered. Appropriate measures to reduce SSI rates must be taken to improve the patient’s safety. This should also diminish costs for health care systems which benefits the entire community.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical sites infections (SSI) are a serious operative complication and consequences may affect both, the patient (morbidity and mortality) as well as the hospital [presumably by leading to an increased length of hospital stay (LOS) and costs] [1, 2]. Previous studies have reported that SSI rates may range from 0.2% for laparoscopic surgery (abdominal surgery) to 3.7% for open surgery [deep sternal wound infections (DSWI)] [3, 4]. Mortality rates may vary between 15% and 40% [5, 6].
Only few studies have yet described the economic impact of DSWI after coronary artery bypass grafting (CABG) surgery via sternotomy. We herewith present the corresponding findings as determined in a matched case-control study [7]. Furthermore, this article summarizes economic aspects of SSIs from various other surgical disciplines.
Materials and methods
Matched case-control study
As previously described [7], Hannover Medical School is a German tertiary care university hospital. Approximately 2,300 patients per year undergo median sternotomy in the department of cardiac, thoracic, transplantation, and vascular surgery for various reasons. From January 2006 until March 2008 (27 months), prospective surveillance of DSWI was performed continuously by trained infection control personnel. Patients who underwent CABG and developed a nosocomial DSWI according to the criteria as defined by the Centers for Disease Control and Prevention (CDC) [8]. Patients with sterile dehiscence or superficial sternal wound infections were excluded from the study. Readmitted patients were not eligible as case patients also. Control patients also needed to undergo CABG but did not suffer from DSWI afterwards. Controls were matched to cases in 2:1 ratio applying the following matching criteria: age, gender, and identical diagnosis-related group in the same year. Adjusting for time at risk before surgery was done by matching for the preoperative LOS +/− 2 days. Adjusting for time at risk after surgery was done by matching for the LOS after the thoracic surgical procedure of controls being at least as long as that of cases before the onset of DSWI. During the investigation period, the frequency of DSWI occurrence ranged from 1.8% to 3.6%. Costs for the hospital and reimbursement from health insurance companies for DSWI cases and control patients were determined at the time of follow-up and include costs of surgery, treatment on intensive care units (ICUs), stay on peripheral wards, and laboratory tests. Raw data were provided in euro (€) but got converted into US dollar ($) for easier comparison to findings of others using currency rates as valid on February 7, 2011. In order to check for any variables or conditions that might influence the costs of a single patient, we checked for the presence of several potential risk factors and comorbidities (Table 1).
Review of the current literature on SSI
Retrieval of data
To identify articles about costs of SSIs, a MEDLINE search was performed using the following search strategy: (“SURGICAL SITE INFECTION” or “HOSPITAL INFECTION” or “NOSOCOMIAL INFECTION”) and (“COST” or “COSTS” or “ECONOMICS” or “ECONOMIC ASPECTS”).
Inclusion criteria
The study must provide primary data on costs of some kind of SSIs. Reporting facility is located within Europe or USA. Articles must be written in English language. Publication of data must have occurred recently (time frame: January 2005 through December 2010, January 2000 through December 2010 for Cardiothoracic Publications due to the small number of articles).
Results
Matched case-control study
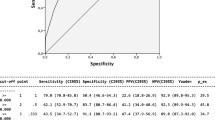
During the study period, a total of 4,130 cardiac surgical procedures were performed. One hundred twenty case patients with DSWI were detected by surveillance (SSI rate: 2.9%), and, thus, got included in cost calculation study. One hundred (83%) cases were diagnosed during their hospital stay in our facility already or during their subsequent stay in a rehabilitation clinic. The remaining 20 (17%) patients were diagnosed after readmission to our hospital. Overall 27 (23%) events of DSWI occurred after the initial discharge of the patient. Causative microorganisms were cultured in specimens from a total of 112 (93%) sites of clinical DSWI. Most frequently, cultured isolates were coagulase negative staphylococci (39%), Staphylococcus aureus (23%; with a proportion of 52% methicillin-resistant S. aureus (MRSA), and enterococci (10%). Up to four different microorganisms were detected in swab from a single DSWI site. The mean time after surgery until the diagnosis of DSWI was 13.4 days (median: 19 days). Treatment of cases included debridement, vacuum therapy, and omental reconstruction if considered necessary. After applying the matching criteria as described above, 17 cases remained for which 34 controls were found (out of 120 potential control patients). The total number of patient days of cases was 585 days compared to 560 day of controls. As shown in Table 2, the median hospital LOS was twice as long in cases compared to controls (34.4 days vs. 16.5 days, p = 0.0006). The median LOS on ICU was also increased for cases but failed to reach statistical significance (6.3 days vs. 5.3 days). The median postoperative LOS was approximately four times longer in cases (32.2 days) compared to all controls without infection (8.0 days; p = 0.04). In a 30-day follow-up, the mortality rates of the cases were 17.6% vs. 8.8% in controls. Table 3 indicates that, besides the preoperative LOS, the control patients as chosen for our case-control study are a representative subgroup of all patients lacking DSWI. Table 4 presents an overview on costs of cases and controls. The median cost of cases which required DSWI treatment was $49,449. These include costs for ward care (24.7%), surgical costs (19.0%), costs for ICU care (27.7%), costs for laboratory tests (15.0%), and other costs (13.6%). The median reimbursement from health care insurance companies was $36,962 per case patient (equivalent to a financial loss of $12,482 per case). The median reimbursement of controls undergoing CABG without developing SSI was $18,674 per control patient (equivalent to a financial profit of $484 per control). Noteworthy, the financial loss most probably underestimates the situation as costs of cases due to additional admissions were not even included in this calculation. In contrast, the median cost of cardiac surgery procedure in control patients was $18,218 comprising ward care (13.0%), surgical costs (28.3%), ICU care (29.6%), laboratory tests (16.4%), and other (12.7%). More detailed information on the findings of this study are described elsewhere [7].
Review of the current literature on SSI
Included studies
Overall, 14 articles were identified by the search strategy as described. Six of those were performed in hospitals in USA [4, 9–13]. The remaining eight studies took place in European countries (Sweden, UK, Turkey, Spain, Switzerland, and France) [5, 14–20]. No other study on DSWI cost calculation from Germany was found. Authors from 11 studies described in detail that infections were identified based on the abovementioned CDC guidelines [8]. The exact way of data acquisition remains unknown in some studies as only in 11 articles the collection of data by specialized infection control personnel was stated.
Cost of SSI in medical literature
Depending upon the type of surgical procedure, the median costs (presented as either “additional” or “total” costs) of SSI varied from $2,342 to $38,554 per patient. A detailed overview about costs of SSI in general and DSWI costs in particular are shown in Table 5. The additional LOS due to SSI ranged between 6 and 14 days in median, being DSWI, the type of infection causing the longest extent of LOS (14 days). There were only three studies that provided either data on total costs due to DSWI [4, 5] or on costs of DSWI therapy only [19]. The additional costs of DSWI were calculated between $6,851 [5, 21] and $20,012 [4, 22] for the first 12 months after the surgical procedure, while the corresponding extra LOS were 35 days [5] and 46 days [4], respectively (statistically not significant).
Discussion
Our analysis confirms once again that SSIs increase the mean LOS and costs. The results of the present study as well as the findings of others [4, 5, 19] clearly demonstrate that especially DSWI in thoracic surgery are a severe complication combined with an exceptionally strong clinical and economical impact compared to SSIs after other types of surgical procedures [19, 23]. The DSWI infection rate after open heart surgery of at least 1.8% as determined in our facility is in line with earlier reported rates of 0.5% through 3.2% [24, 25]. The choice of inclusion criteria for cases in our case-control study also fits the patient characteristics as defined by others before [26–29]. Thus, we believe that our data are both valid and representative.
In our study, patients with sternotomy who developed DSWI had a doubled mortality rate, a need for 18 additional (expensive) days of hospital LOS, and caused significantly increased attributive costs ($31,199 per case) when compared to controls undergoing sternotomy but lacking developing DSWI which is concordat in principle to previous descriptions [30]. The main share of costs in DSWI case patients were split among care on peripheral wards, costs for additional surgical procedures, and costs for prolonged ICU care. Because DSWI are associated with by far more costly outcomes already [19], we refrained from including superficial chest infections and leg infections in our cost estimates, too.
As the implementation and/or enforcement of infection control measures may lower infection rates, a multimodal but hence cost-effective approach is desired. One should always keep in mind the SSI pathogens may endogenously derive from the patient’s physiological flora, e.g., from the skin, or they may be transmitted to him from others or from the environment, e.g., through leaking gloves during the operation [31, 32]. An appropriate infection control method must take both of these sources into account. In the following, we would like to highlight a selection of valuable measures for SSI prevention that, unfortunately, get frequently neglected.
Surveillance of SSI by infection control staff is important for the hospital to get an overview of the current situation and will also contribute to the prevention of infection. Evaluation procedures, prospective recording of SSI, comparison of infection rates to reference data, and (confidential) feedback of results to the corresponding surgical department are integral parts of a successful intervention program. By this, SSI rates may be reduced up to 50% [1, 33, 34].
One of the main risk factors for SSI is nasal carriage of S. aureus by the patient [35]. Although it is well-known that approximately one third of inpatients in fact are carriers, a corresponding nasal screening is not widely performed [36–38]. However, this should be encouraged because preoperative decolonization measures will most probably reduce the incidence of SSI due to gram-positive aerobic bacteria [39]. This is true especially in the case that screening results will not be available before beginning of the surgical procedure. If elective surgery procedures are planned, nasal screening of both, MRSA and methicillin-sensitive S. aureus could be done in advance. This way, appropriate decolonization measures could be accomplished in the ambulant setting (before admission to the hospital), and infection control measures could also get implemented at an early most time point. Without doubt, this tactic will reduce the risk of transmission and, thus, the frequency of nosocomial infections [35].
Another important item is timely administration of perioperative antimicrobial prophylaxis. Unfortunately, the optimal time point chosen is often inconsistent with recommendations from international guidelines, and application of substances occurs too late [40]. Furthermore, the overall duration of perioperative prophylaxis should be reconsidered in many surgical departments. An antibiotic prophylaxis longer than 24 h rarely has a positive impact on the SSI rate, but rather promotes the selection of multi-drug resistant organisms or Clostridium difficile-associated disease [41]. This way, good antimicrobial stewardship will benefit both epidemiology and economy.
Particularly the site of incision deserves attention. Preoperative hair removal should be done by using clipping machines instead of razor blades, as those are likely to injure the surrounding skin and significantly increase the risk of SSI [42, 43]. The initial dressing of the wound should remain for at least 48 h post-surgery [44], and removal of any plastic devices should be done postoperatively as soon as wound secretion has terminated and drainages are no longer required [45].
Finally, proper hand hygiene by the use of alcohol-based hand rub of staff should be general practice in the field of surgery [46].
There are several guidelines addressing to prevention of SSI [47–49], but to our knowledge, a bundle of hygiene measures is useful for the reduction of SSI, as it was shown before [50].
Some limitations have to be kept in mind particularly when interpreting the data presented in our study. (a) As mortality rates were determined by a 30-day follow-up only, we do not know for sure whether all fatal cases were detected by our surveillance. A longer post-discharge surveillance time frame would be necessary in order to clarify this issue. Thus, our data might even underestimate the true mortality rate due to DSWI. (b) We only included the costs of patients with DSWI that derived from their first stay in our hospital but not from readmissions later on. Thus, our data might also even underestimate the true costs due to DSWI. (c) This is a single institution survey in a tertiary care German university hospital. Thus, generalization of results should be done with caution as our findings may not apply the same way for thoracic surgery departments in every other setting, e.g., in hospitals in other countries. (d) Costs as calculated in this study were based on the hospital costs as generated by the financial controlling department of our hospital only. Thus, we cannot rule out that there might have been some additional—hidden—costs that have been missed by our approach of cost determination. (e) Finally, although highly suggestive, we cannot prove for sure that the prolonged stay of cases after developing DSWI is caused by the infection itself only or if other comorbidities may rather have had an influence on the LOS.
Conclusion
Obviously, SSI represents a serious clinical complication. In addition, our data show that SSIs also have a high impact on the overall expenses for hospitals and health care systems. SSI may almost triple the individual costs with DSWI being the most expensive ones—but those additional charges may not be sufficiently covered. Considering the clinical consequences of SSI, it is crucial that all appropriate measures for the reduction of SSI rates are implemented or get enforced—primary for the patient’s safety. Furthermore, any effort taken in the field of infection control will also subsequently diminish the costs for health care systems which will bring benefit for the entire population. Further studies that deal with cost-effectiveness of infection control in surgery and especially in thoracic surgery due to the small number of currently existing studies are therefore very much appreciated.
References
Gastmeier P et al (2005) Reduction of orthopaedic wound infections in 21 hospitals. Arch Orthop Trauma Surg 125:526–530
Gaynes RP et al (2001) Surgical site infection (SSI) rates in the United States, 1992–1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis 33(Suppl 2):S69–S77
Biscione FM (2009) Rates of surgical site infection as a performance measure: are we ready? World J Gastrointest Surg 1:11–15
Hollenbeak CS et al (2000) The clinical and economic impact of deep chest surgical site infections following coronary artery bypass graft surgery. Chest 118:397–402
Coskun D, Aytac J, Aydinli A, Bayer A (2005) Mortality rate, length of stay and extra cost of sternal surgical site infections following coronary artery bypass grafting in a private medical centre in Turkey. J Hosp Infect 60:176–179
Romaniszyn D et al (2006) Epidemiological and microbiological surveillance of surgical site infections in orthopedic unit. Ortop Traumatol Rehabil 8:639–645
Graf K et al (2010) Economic aspects of deep sternal wound infections. Eur J Cardiothorac Surg 37:893–896
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
McGarry SA, Engemann JJ, Schmader K, Sexton DJ, Kaye KS (2004) Surgical-site infection due to Staphylococcus aureus among elderly patients: mortality, duration of hospitalization, and cost. Infect Control Hosp Epidemiol 25:461–467
Herwaldt LA et al (2006) A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Infect Control Hosp Epidemiol 27:1291–1298
Anderson DJ et al (2007) Underresourced hospital infection control and prevention programs: penny wise, pound foolish? Infect Control Hosp Epidemiol 28:767–773
Sparling KW et al (2007) Financial impact of failing to prevent surgical site infections. Qual Manag Health Care 16:219–225
Olsen MA et al (2008) Hospital-associated costs due to surgical site infection after breast surgery. Arch Surg 143:53–60
Coello R et al (2005) Adverse impact of surgical site infections in English hospitals. J Hosp Infect 60:93–103
Monge JV, de Los Terreros SL Sainz, Diaz-Agero PC, Saa Requejo CM, Plana FN (2006) Excess length of stay attributable to surgical site infection following hip replacement: a nested case-control study. Infect Control Hosp Epidemiol 27:1299–1303
Pollard TC, Newman JE, Barlow NJ, Price JD, Willett KM (2006) Deep wound infection after proximal femoral fracture: consequences and costs. J Hosp Infect 63:133–139
Alfonso JL et al (2007) Are we really seeing the total costs of surgical site infections? A Spanish study. Wound Repair Regen 15:474–481
Penel N et al (2008) Additional direct medical costs associated with nosocomial infections after head and neck cancer surgery: a hospital-perspective analysis. Int J Oral Maxillofac Surg 37:135–139
Mokhtari A et al (2008) The cost of vacuum-assisted closure therapy in treatment of deep sternal wound infection. Scand Cardiovasc J 42:85–89
Weber WP et al (2008) Economic burden of surgical site infections at a European university hospital. Infect Control Hosp Epidemiol 29:623–629
Coskun D, Aytac J (2006) The decrease in healthcare-associated methicillin-resistant Staphylococcus aureus infections and savings from glycopeptide use. Infect Control Hosp Epidemiol 27:1131–1132
Hollenbeak CS, Alfrey EJ, Sheridan K, Burger TL, Dillon PW (2003) Surgical site infections following pediatric liver transplantation: risks and costs. Transpl Infect Dis 5:72–78
Upton A, Smith P, Roberts S (2005) Excess cost associated with Staphylococcus aureus poststernotomy mediastinitis. N Z Med J 118:1210, U1316
Lopez Gude MJ et al (2006) Case-control study of risk factors for mediastinitis after cardiovascular surgery. Infect Control Hosp Epidemiol 27:1397–1400
Lucet JC (2006) Surgical site infection after cardiac surgery: a simplified surveillance method. Infect Control Hosp Epidemiol 27:1393–1396
Braxton JH et al (2000) Mediastinitis and long-term survival after coronary artery bypass graft surgery. Ann Thorac Surg 70:2004–2007
Braxton JH et al (2004) 10-year follow-up of patients with and without mediastinitis. Semin Thorac Cardiovasc Surg 16:70–76
Ridderstolpe L, Gill H, Granfeldt H, Ahlfeldt H, Rutberg H (2001) Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardiothorac Surg 20:1168–1175
Ridderstolpe L, Gill H, Borga M, Rutberg H, Ahlfeldt H (2005) Canonical correlation analysis of risk factors and clinical outcomes in cardiac surgery. J Med Syst 29:357–377
Boyce JM, Potter-Bynoe G, Dziobek L (1990) Hospital reimbursement patterns among patients with surgical wound infections following open heart surgery. Infect Control Hosp Epidemiol 11:89–93
Tammelin A, Domicel P, Hambraeus A, Stahle E (2000) Dispersal of methicillin-resistant Staphylococcus epidermidis by staff in an operating suite for thoracic and cardiovascular surgery: relation to skin carriage and clothing. J Hosp Infect 44:119–126
Tammelin A, Hambraeus A, Stahle E (2001) Source and route of methicillin-resistant Staphylococcus epidermidis transmitted to the surgical wound during cardio-thoracic surgery. Possibility of preventing wound contamination by use of special scrub suits. J Hosp Infect 47:266–276
Barwolff S et al (2006) Reduction of surgical site infections after Caesarean delivery using surveillance. J Hosp Infect 64:156–161
Brandt C et al (2006) Reduction of surgical site infection rates associated with active surveillance. Infect Control Hosp Epidemiol 27:1347–1351
Bode LG et al (2010) Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 362:9–17
Munoz P et al (2008) Nasal carriage of S. aureus increases the risk of surgical site infection after major heart surgery. J Hosp Infect 68:25–31
Halablab MA, Hijazi SM, Fawzi MA, Araj GF (2010) Staphylococcus aureus nasal carriage rate and associated risk factors in individuals in the community. Epidemiol Infect 138:702–706
Berthelot P et al (2010) Is nasal carriage of Staphylococcus aureus the main acquisition pathway for surgical-site infection in orthopaedic surgery? Eur J Clin Microbiol Infect Dis 29:373–382
Young LS, Winston LG (2006) Preoperative use of mupirocin for the prevention of healthcare-associated Staphylococcus aureus infections: a cost-effectiveness analysis. Infect Control Hosp Epidemiol 27:1304–1312
Bratzler DW, Houck PM (2004) Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis 38:1706–1715
Gagliotti C, Ravaglia F, Resi D, Moro ML (2004) Quality of local guidelines for surgical antimicrobial prophylaxis. J Hosp Infect 56:67–70
Niel-Weise BS, Wille JC, van den Broek PJ (2005) Hair removal policies in clean surgery: systematic review of randomized, controlled trials. Infect Control Hosp Epidemiol 26:923–928
Dizer B et al (2009) The effect of nurse-performed preoperative skin preparation on postoperative surgical site infections in abdominal surgery. J Clin Nurs 18:3325–3332
Segers P, de Jong AP, Spanjaard L, Ubbink DT, de Mol BA (2007) Randomized clinical trial comparing two options for postoperative incisional care to prevent poststernotomy surgical site infections. Wound Repair Regen 15:192–196
Bassi C et al (2010) Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Ann Surg 252:207–214
Le TA et al (2007) Reduction in surgical site infections in neurosurgical patients associated with a bedside hand hygiene program in Vietnam. Infect Control Hosp Epidemiol 28:583–588
Anderson DJ et al (2008) Strategies to prevent surgical site infections in acute care hospitals. Infect Control Hosp Epidemiol 29(Suppl 1):S51–S61
Robert Koch Institute (2007) Prevention of postoperative surgical wound infection: recommendations of the Hospital Hygiene and Infection Prevention Committee of the Robert Koch Institute. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50:377–393
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol 20:250–278
Graf K et al (2009) Decrease of deep sternal surgical site infection rates after cardiac surgery by a comprehensive infection control program. Interact Cardiovasc Thorac Surg 9:282–286
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Graf, K., Ott, E., Vonberg, RP. et al. Surgical site infections—economic consequences for the health care system. Langenbecks Arch Surg 396, 453–459 (2011). https://doi.org/10.1007/s00423-011-0772-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0772-0