Abstract
Background
Primary hyperparathyroidism with coexisting thyroid nodular disease (TND) has been considered a contraindication for selective parathyroidectomy because the low sensitivity of preoperative localization studies, especially 99mTc-sestamibi scanning (MIBI) and ultrasound. The aim of this study was to assess the impact of concomitant TND in the preoperative image studies.
Methods
A total of 236 consecutive patients who had parathyroidectomy for sporadic hyperparathyroidism and the preoperative localization study that was done with MIBI were reviewed. Patients were divided into three groups: those who did not have any thyroid disease, those who had concomitant TND not necessary to resect, and those in whom thyroid resection due to TND was necessary at the time of parathyroidectomy.
Results
MIBI showed a sensitivity of 78.5% in patients without concomitant TND, 73% in patients with TND but not thyroidectomy needed, and 54.5% in the cases that thyroid resection was necessary. When MIBI and ultrasound were both suspicious for an adenoma, the sensitivity was not influenced by the TND.
Conclusion
In patients with coexisting thyroid disease but not thyroidectomy needed, MIBI scintigraphy contributes to the detection of a solitary adenoma. When thyroid resection is required, MIBI imaging is often negative.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, surgical trends for primary hyperparathyroidism (PHPT) are moving toward selective parathyroidectomy (SP). A coexisting thyroid disease has previously been considered a relative contraindication to SP because of the decrease in the sensitivity of localizing techniques [1].
It is well known that in most cases, PHPT is sporadic and caused by a single adenoma in 85%–95% of the instances [2]. The increasing use and accuracy of 99mTc-sestamibi scanning (MIBI) allow for preoperative localization of solitary adenomas in 75%–90% of the cases; this has led surgeons to progressively implement SP [3, 4]. Sometimes, however, there are some false-positive and false-negative results that may be attributed to coexisting thyroid nodular disease [5].
The prevalence of associated thyroid nodular disease in patients with PHPT has been reported to range from 20% to 60% [6–8], and although the characteristics and outcomes of these “false-images” are not well characterized, it has been speculated that parathyroid glands not visualized with image diagnostic techniques carry a higher risk of multinodular disease, not diagnosed in the preoperative workup. Due to the lower sensitivity of localization techniques, the approach in patients with associated thyroid nodular disease has been a traditional cervicotomy with four gland examination with resection of the abnormally enlarged gland(s), but progressively, the traditional contraindications for SP have been considered relative, except those patients requiring thyroid resections.
The aim of this study was to assess the impact of concomitant thyroid nodular disease on accuracy of 99mTc-sestamibi used for the preoperative image diagnosis.
Methods
Between January 1992 and May 2009, 236 patients with biochemically proven PHPT and preoperative MIBI were identified by retrospective review of the prospectively maintained endocrine surgery database. Patients with hereditary multiple endocrine neoplasia, parathyroid hyperplasia, or previous neck surgery were excluded.
MIBI technique
All patients received an intravenous injection of 450 MBq sestamibi. Planar images were acquired using a low-energy, high-resolution collimator positioned as near as possible to the neck, in a 128 × 128 matrix with a 2-zoom and an energy window of 140 keV ± 10% using a single-head General Electric gamma camera. The initial image (early images) was acquired in the anterior, left and right anterior 30º oblique view 15 min after tracer administration. Similar views were obtained starting 90–120 min after injection (delayed images) and were acquired for identical times.
Ultrasound technique
All cervical ultrasound (US) were performed using a 6- to 13-MHz scanner. If thyroid nodules were found, malignancy was determined on the bases of ultrasonographic features (calcification, shape, echo structure, and echogenicity) and cytological findings (US–fine-needle aspiration biopsy).
Patients were divided into three categories: those with no thyroid disease, those with concomitant thyroid nodular disease without indication for thyroidectomy, and those in whom thyroid resection due to concomitant disease was necessary at the time of parathyroidectomy.
Scintigraphic data were correlated with intraoperative findings and site of the thyroid gland nodularity. A false positive was defined when MIBI showed one abnormal focal accumulation that did not correlate with the site of an excised single adenoma. In false- negative cases, MIBI showed no abnormal accumulation/suspected adenoma. True-positive MIBI tests were named “Right” and false-positive plus false-negative MIBI tests were named “Wrong.” Sensitivity and positive predictive value (PPV) were calculated. Thyroid estimated volume and weight, parathyroid weight, parathyroid oxyphilic cell content, and biochemical outcomes were also recorded.
Statistical analysis was performed using the SPSS 15.0 for Windows (SPSS Iberica, Madrid, Spain). Contingency tables of qualitative data were assessed using χ 2 or Fisher's exact test when appropriate. In all analyses, P < 0.05 was accepted as statistically significant. The normality of the distribution of quantitative variables was assessed by Kolmogorov–Smirnov single-sample test. Results were expressed as arithmetic mean ± SD, unless specified otherwise. For quantitative variables, two-tailed Student's t test for nonpaired data was used to assess the significance of differences in means between two groups and analysis of variance for three or more groups.
Results
There were 199 women and 37 men with a mean age 61 ± 14 years (range, 19–89 years). Preoperative mean serum calcium level was 2.8 ± 0.2 mmol/L, and mean parathyroid hormone level was 262 ± 435 ng/L.
A distinct solitary focus of increased MIBI uptake relative to the thyroid gland was considered positive for abnormal parathyroid disease in 187 patients, whereas 49 patients did not have any image suggestive of an enlarged parathyroid gland. In 171 patients, a preoperative cervical ultrasound (US) examination was also obtained before surgery; in 58 patients, a CT scan was done; and in 8 patients, we did not have any thyroid gland image.
Regarding the thyroid gland, 144 patients (62.8%) did not exhibit any thyroid alteration, 52 patients (22.7%) had a concomitant nodular thyroid disease without indication for thyroidectomy, and finally, 33 patients (14.4%) had a uninodular or multinodular goiter that made an associated thyroidectomy necessary at the time of parathyroidectomy. Thyroid nodular disease requiring surgery was defined as suspicion of thyroid cancer by fine-needle aspiration cytology, size of the nodules bigger than 4 cm, and/or presence of compressive symptoms.
In 84 patients (35.6%), the initial approach was an SP, of which in 3 cases (3.6%), the procedure was converted to bilateral neck exploration. In 152 patients (64.4%), the initial procedure was a conventional cervicotomy with four gland exploration.
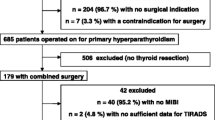
Sensitivity, PPV, false-positive, and negative of the MIBI scan are shown in Fig. 1. Preoperative MIBI was positive in 182 patients. In patients without thyroid disease, the sensitivity was 78.5% and the PPV was 95.8%. Differences of sensitivity and PPV were higher if patients are divided by the need for thyroid surgery (Table 1). When both MIBI and US identified a parathyroid adenoma, the results were not influenced by the thyroid nodular disease, and the sensitivity and PPV were 90.1% and 98.6% in the group without thyroid surgery, and 100% in the patients who needed thyroid resection (Table 2).
Distribution of patients with sporadic PHPT according to coexisting thyroid nodular disease and its effect on the diagnostic accuracy of cervical scintigraphy with 99mTc-sestamibi. Right: MIBI correctly identified the side and position of a pathologic parathyroid gland. Wrong: MIBI did not identify any gland or identified a false gland in the wrong place
In the analysis of the adenoma characteristics, only the adenoma weight was significantly associated to the MIBI performance (P = 0.005). Other features as thyroid gland characteristics or parathyroid gland oxyphilic cell content were not significantly associated with MIBI results (Table 3).
The anatomic position of the adenoma (superior vs. inferior parathyroid glands) was associated with the MIBI accuracy, with MIBI sensitivity being higher in detecting adenomas of inferior parathyroid glands (Table 4).
Discussion
The surgical management of PHPT has evolved over the last two decades toward a more selective approach since first suggested by Tibblin et al [9]. With the advent of more refined preoperative localizing studies and intraoperative tools, focused parathyroidectomy can be performed in 60%–75% of all patients with sporadic PHTP, even under local anesthesia [10]. The accuracy of the preoperative localizing techniques is essential to ensure a successful selective parathyroid approach.
Many clinical researchers have assessed the decrease of the sensitivity and PPV of both MIBI and US as localization preoperative studies when a nodular thyroid disease coexists with PHPT. The hypothesis is that false-positive MIBI results could be originated by MIBI accumulation in thyroid nodules [1, 5, 8, 11–13].
In this clinical study, nodular thyroid disease requiring thyroidectomy had more impact on the MIBI results than the mere presence of thyroid nodular disease. In case of no concomitant thyroid disease, the MIBI had a sensitivity of 77%, and if thyroidectomy was required, the sensitivity fell to 54.5%. This difference was not observed in cases where both MIBI and US coincided in the localization of the parathyroid adenoma, with the sensitivity being higher than 90% in both groups. This distinction is of importance because it shows that MIBI is affected more easily by the nodular thyroid disease requiring thyroidectomy than by the mere presence of benign nodules without surgical indication that coexists in approximately 20%–60% of cases. Patients with PHTP and nodular disease in whose thyroid surgery is not needed, MIBI shows a false-positive result lower than 6% and a sensitivity of 77%.
Also, in accordance with some recently published studies, in our analysis, the adenoma weight in true-positive scans was significantly larger than those in false-negative scans, and those in the upper position are less likely to be localized. In our series, however, we have not identified a relationship of the MIBI accuracy with the oxyphilic cell content of the parathyroid adenoma [14, 15].
We have observed that in patients with coexisting thyroid disease but not thyroidectomy needed, MIBI scintigraphy contributes to the detection of a solitary adenoma and allows unilateral exploration, but when thyroid resection is planned, parathyroid scintigraphy is much less accurate.
References
Krausz Y, Lebensart PD, Klein M, Weininger J, Blachar A, Chisin R et al (2000) Preoperative localization of parathyroid adenoma in patients with concomitant thyroid nodular disease. World J Surg 24:1573–1578
Sitges-Serra A, Prieto R, Valero M, Membrilla E, Sancho JJ (2008) Surgery for sporadic primary hyperparathyroidism: controversies and evidence-based approach. Langenbecks Arch Surg 393:239–244
Moure D, Larrañaga E, Domínguez-Gadea L, Luque-Ramírez M, Nattero L, Gómez-Pan A et al (2008) 99MTc-sestamibi as sole technique in selection of primary hyperparathyroidism patients for unilateral neck exploration. Surgery 144:454–459
Grant CS, Thompson G, Farley D, van Heerden J (2005) Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy: Mayo Clinic experience. Arch Surg 140:472–478
Prager G, Czerny C, Ofluoglu S, Kurtaran A, Passler C, Kaczirek K et al (2003) Impact of localization studies on feasibility of minimally invasive parathyroidectomy in an endemic goiter region. J Am Coll Surg 196:541–548
Prinz RA, Barbato AL, Braithwaite SS, Brooks MH, Emanuele MA, Gordon DL et al (1982) Simultaneous primary hyperparathyroidism and nodular thyroid disease. Surgery 92:454–458
Bentrem DJ, Angelos P, Talamonti MS, Nayar R (2002) Is preoperative investigation of the thyroid justified in patients undergoing parathyroidectomy for hyperparathyroidism? Thyroid 12:1109–1112
Morita SY, Somervell H (2008) B, Dackiw A P, Zeiger MA. Evaluation for concomitant thyroid nodules and primary hyperparathyroidism in patients undergoing parathyroidectomy or thyroidectomy. Surgery 144:862–866
Tibblin S, Bondeson A-G, Ljungberg O (1982) Unilateral parathyroidectomy in hyperparathyroidism due to single adenoma. Ann Surg 195:245–252
Bergenfelz A, Kanngiesser V, Zielke A, Nies C, Rothmund M (2005) Conventional bilateral cervical exploration versus open minimally invasive parathyroidectomy under local anaesthesia for primary hyperparathyroidism. Br J Surg 92:190–197
Monroe DP, Edeiken-Monroe BS, Lee JE, Evans DB, Perrier ND (2008) Impact of preoperative thyroid ultrasonography in the surgical management of primary hyperparathyroidism. Br J Surg 95:957–960
Masatsugu T, Yamashita H, Noguchi S, Nishii R, Koga Y, Watanabe S et al (2005) Thyroid evaluation in patients with primary hyperparathyroidism. Endocr J 52:177–182
Ogawa T, Kammori M, Tsuji E, Kanauchi H, Kurabayashi R, Terada K et al (2007) Preoperative evaluation of thyroid pathology in patients with primary hyperparathyroidism. Thyroid 17:59–62
Stephen AE, Roth SI, Fardo DW, Finkelstein DM, Randolph GW, Gaz RD et al (2007) Predictors of an accurate preoperative sestamibi scan for single gland parathyroid adenomas. Arch Surg 142:381–386
Erbil Y, Kapran Y, Işsever H, Barbaros U, Adalet I, Dizdaroğlu F et al (2008) The positive effect of adenoma weight and oxyphil cell content on preoperative localization with 99mTc-sestamibi scanning for primary hyperparathyroidism. Am J Surg 195:34–39
Conflict of interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gómez-Ramírez, J., Sancho-Insenser, J.J., Pereira, J.A. et al. Impact of thyroid nodular disease on 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism. Langenbecks Arch Surg 395, 929–933 (2010). https://doi.org/10.1007/s00423-010-0680-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-010-0680-8