Abstract
Background
Patient satisfaction and emotional support are crucial elements of cancer care. Little is known, however, about which areas of care are important from the patient’s perspective and the roles emotional distress and support play in this context.
Methods
Multicenter prospective study was conducted (n = 396 cancer patients; t1 = after admission to hospital, t2 = before discharge). Quality of care was measured with the quality of care from the patient’s perspective questionnaire, and emotional distress was measured with the hospital anxiety and depression scale. Additional questions regarding emotional support wished (at t1) and provided (at t2) were administered.
Results
The patients reported that the domains of care most important to them were as follows: respect and commitment of the physicians, information before procedures, care equipment, and medical care. The areas where improvements are most obviously needed were nutrition, participation, clarity about who is responsible for personal care, and having the possibility of speaking in private with nurses and psycho-oncologists. Fifty-six percent of the patients were highly emotionally distressed, 84% wanted support from physicians, 76% from nurses, 33% from psychologists, and 7% from a pastor.
Conclusion
Emotional support is a crucial part of patient satisfaction and should be provided by several members of the oncological team, especially the patients’ physicians. In turn, it is crucial that medical professionals be equipped with good communication skills.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Care for patients with tumors in Germany is increasingly being provided in large centralized cancer centers in order to improve the quality of oncological treatments, optimize treatment pathways, and enhance patient satisfaction.
The question of which areas of care are currently most in need of improvement to increase patient satisfaction is an important one. Valid and reliable measurement of patient satisfaction is a crucial element in the process of answering this question. A review of 195 studies dealing with patient satisfaction [1] revealed that only 11 studies (6% of the 181 quantitative studies) reported content validity and criterion or construct validity and reliability. “New” instruments designed specifically for the reported study demonstrated significantly less evidence for reliability and validity, respectively, than did “older” established instruments. The author concludes (p. 319): “Moreover, study authors exhibited a poor understanding of the importance of these properties in the assessment of satisfaction. Researchers must be aware that this is poor research practice, and that lack of a reliable and valid assessment instrument casts doubt on the credibility of satisfaction findings.”
Additionally, measurement of patient satisfaction has long been hindered by the lack of content validity in commonly used instruments [2]. Most patient satisfaction instruments have been developed from the perspective of the provider or institution rather than that of the patient [2], resulting in their measurements’ content validity being questionable. In addition, patient satisfaction data often are biased because of the willingness of patients to please the investigators or due to the willingness of the investigator to please his or her sponsor or hospital manager [2].
These problems can be addressed through tool development using a qualitative method designed to obtain the patient’s perspective. A study group from Sweden did this when they developed the instrument quality of care from the patient’s perspective (QPP) [3–6]. With this questionnaire, two dimensions of quality of care are covered. Both the patient’s preferences (humanity and rationality, i.e., strive for order, predictability, and calculability in life) are taken into consideration as is the resource structure of the organization (qualities related to the physical and administrative care environment and person-related qualities). These two dimensions are combined to create the following four domains: medical-technical competence (e.g., physical caring), physical-technical conditions (e.g., comfortable bed), identity-oriented approach (e.g., commitment of doctors), and socio-cultural atmosphere (e.g., possibility of speaking privately with a physician). The QPP also addresses another problem in satisfaction research, the fact that it often goes unrecognized that contentment with a specific situation depends on two aspects, namely, expectations and perceived reality [7]. In this questionnaire, patients are asked to share their view on both aspects of different quality of care domains. The resulting domains are subjective importance (i.e., expectations) and perceived reality (i.e., the evaluation of the care).
The QPP has been validated in a large multinational survey including ward patients from England (n = 1236), France (n = 1051), Norway (n = 226), and Sweden (n = 428), and day-surgery patients from England (n = 887), France (n = 544), Norway (n = 101), and Sweden (n = 742) [8].
In the above-mentioned cancer centers, multidisciplinary care is intended to realize a holistic view of patients and their disease [9]. This involves cooperation of surgical and medical departments, consideration of quality of life issues, communication between health care providers and patients, and the provision of emotional support [10–12]. The extent to which cancer patients need emotional support and the question of who is responsible for providing it are frequently debated issues in need of clarification.
Patients and methods
Design
We conducted a prospective study with consecutive patient accrual in two large acute care hospitals in Leipzig, Germany. All patients who came to the hospitals for diagnosis or treatment of cancer were enrolled. Additional inclusion criteria were as follows: age 18 or older, ability to understand German, physical and mental ability to take part in a survey, and written informed consent.
All eligible patients were contacted, the aims of the study were explained, and the voluntary nature of participation confirmed. If the patient was willing to participate, he or she received a self-administered questionnaire to be completed on his or her first day in the hospital (t1) and one day before being discharged (t2). Data from general and gastrointestinal surgical patients were filtered for the following analyses.
This study was approved by the ethics committee of Leipzig University and was performed in accordance with the ethical standards laid down in the 1964 declaration of Helsinki.
Measures
Participants completed the QPP questionnaire [3] in its revised and shortened version [4, 6]. The QPP was developed using a model derived from grounded theory interviews [3]. Grounded theory is a qualitative research methodology with the aim of generating hypotheses or theories from in-depth interviews. From those interviews, key sentences are marked with a series of codes. The codes are grouped into similar concepts. From these concepts, categories are formed, which are the basis for the creation of a theory or hypothesis. The items cover four domains: medical-technical competence (e.g., “I received the best possible medical care, as far as I can tell.” or “I received examination and treatments within acceptable waiting times.”), physical-technical conditions (e.g., “I received food and drink that I like.” or “I had a comfortable bed.”), identity-oriented approach (e.g., “I received useful information on how examinations and treatments would take place.” or “I had good opportunity to participate in the decisions that applied to my care.”), and socio-cultural atmosphere (e.g., “There was a pleasant atmosphere on the ward.” or “My care was determined by my own request and needs rather than the staff’s procedures.”). One item that was added for this study addressed the issue of providing patients with opportunities to speak with a psycho-oncologist.
Each item is evaluated in two ways by the patient: first, he or she assesses the perceived reality and, afterwards, the subjective importance of that specific issue on a Likert scale. In other words, the patients have to decide to what extent a specific condition is fulfilled or not (absolutely true, almost true, not quite true, not at all true, or not applicable) and whether this particular condition is important for them or not (exceptionally important, very important, somewhat important, or not important). The data of both perceived reality and subjective importance can be combined and weighted into a satisfaction measure, the personal quality index (PQI; see below).
The provisional QPP questionnaire was validated and shortened using factor analysis and structural equation modeling [4]. The internal consistency of the scales ranges from 0.65 (physical-technical conditions) to 0.91 (identity-oriented approach) [6]. Multinational validation was done in 2005 with 2,941 ward and 2,274 day-surgery patients [8]. The patients completed the QPP in our study at t2.
The second questionnaire applied was the hospital anxiety and depression scale (HADS), a widely used scale assessing psychological distress in non-psychiatric patients. The HADS consists of 14 items representing two subscales: anxiety and depression. It has been shown that the total score of the HADS is a good screening method for identifying psychological morbidity in cancer patients, whereby a cutoff point of 13 or more strikes the best balance between sensitivity and specificity [13, 14]. Study participants completed the HADS at both measurement points (t1 and t2).
Additional structured questions about the patient’s wish for psychosocial care were administered. At t1, patients were asked: “Do you want to get emotional support from a physician, nurse, social worker, psychologist, pastoral care, nutritionist, or self help group?” (Yes/no). At t2, the following questions were asked: “Did you get emotional support from…?” (Yes/no). If respondents said they had received support, they were asked to indicate whether the support was helpful or not on a 5-point Likert scale. Sociodemographic and medical data were taken from patients’ medical documents and from structured questions.
Statistical analysis
With the data of the QPP, we computed a personal quality of care index on the basis of the relationship between the two scores using the formula PQI = subjective importance × (2 × perceived reality − subjective importance) as suggested by Nathorst-Böös et al. [5]. The PQI can vary between −8 and 16 with high values indicating high levels of satisfaction and low values suggesting that action should be taken to increase satisfaction with care.
The areas with the highest importance and with the lowest quality indices were investigated in more detail regarding possible influencing factors. In order to avoid underpowered testing, several potential associated variables were first investigated in a non-parametric correlation analysis. Only the significantly correlated variables were subsequently entered into a multivariate analysis model (general linear model).
Chi-square coefficients were calculated to measure the association between the desire and need for support and the help actually received during the patient’s time in the hospital. A Yates continuity correction was performed to assure statistical safety. The score indicating helpfulness of support was transformed to a 100-point scale to facilitate comparisons with the percentage of patients who desired and/or received support. All statistical analysis was done using SPSS®, version 15.
Results
Sample
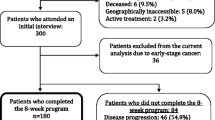
There were 396 patients enrolled in accordance with the inclusion and filter criteria, 194 (49%) men and 202 (51%) women with an average age of 61 years (range, 22–87 years). Of the patients, 119 had stage I cancer, 103 had stage II, 110 had stage III, and 64 had stage IV (tumor stages according to the Union International Contre le Cancer). Patients’ cancer was localized at the following sites: breast (n = 116), colon/rectum (n = 134), other gastrointestinal locations (n = 42), lungs (n = 36), and other (n = 68). The majority of the patients (n = 287, i.e., 73%) were treated for primary cancer, 22 were treated for recurring disease, and 67 had metastases. In 14 cases, a second tumor had occurred, and three patients came for other reasons. In 39 cases (10%), the treating physician estimated the patient’s life expectancy to be less than 6 months. The average time spent in the hospital was 19 days (range, 3–78 days).
Quality of care
The five most important areas of care from the patients’ perspective are respect and commitment of the physicians, receiving information before procedures, care equipment, and medical care (Fig. 1).
The PQIs, indicating the subjective importance to patients and their evaluation of a specific area of care, are displayed in Fig. 2. The five highest satisfaction scores were given for the following areas of care: care equipment (14.3), medical care (13.8), doctors’ commitment (13.6), respect of the doctors (13.5), and the feeling that family and friends received friendly treatment (13.4). The five lowest quality indices were given for nutrition (7.2), shared decision making (9.2), clarity about who was responsible for personal care (10.2), possibility of speaking in private with nurses (10.4), and possibility of speaking in private with psycho-oncologists (10.5).
Factors associated with satisfaction
In the first step, different variables that were considered as potentially associated with satisfaction with care according to the literature were investigated in non-parametric correlation analyses. These variables were gender, age, level of formal education, tumor stage, tumor site, reason for treatment (primary cancer, recurring disease, metastases, second tumor, or other), life expectancy as assessed by the treating physician, time spent in the hospital, and clinic.
The five most important areas of quality of care from the patients’ perspective revealed the following correlations: gender and life expectancy with medical care and age with care equipment. These variables were entered into a multivariate analysis of variance. Results show that gender is the only factor that is associated with patients’ satisfaction in the most important areas of care (F = 3.02, p = 0.01). From the tests of between-subjects effects, we can conclude that females are on average more satisfied with medical care (F = 4.25, p = 0.04).
The five areas with lowest satisfaction were correlated as follows: age and time spent in hospital with possibility to talk with psycho-oncologist and education with clarity about which nurse was responsible for personal care. Of these variables, entered into a multivariate analysis of variance, only time spent in the hospital was associated with satisfaction (F = 2.63, p = 0.03). The longer patients stay in the hospital, the more they are satisfied with the possibility to talk with a nurse (F = 4.40, p = 0.04) and/or a psycho-oncologist (F = 11.61, p = 0.001) in private and with shared decision making (F = 4.42, p = 0.04).
Emotional distress and wish for emotional support
According to the HADS, 56% of the patients at t1 and 48% of the patients at t2 were emotionally distressed and therefore in need of psycho-oncological support. Mean values of the total scale were 14.5 (SD 7.9) at t1 and 12.9 (SD 8.0) at t2, respectively.
Respondents expressed a desire upon entering acute care (t1) for emotional support from physicians, nurses, social workers, psychologists, pastors, nutritionists, and self-help groups at the following percentages: 83.5, 76.1, 40.1, 33.3, 6.7, 27.5, and 21.7 (see Fig. 3).
Desire for emotional support (percent of patients saying “yes”), received support during stay at acute hospital (percent of patients saying “yes”), and perceived helpfulness of support (mean value, 0 = not at all helpful, 100 = very helpful) by different members of the oncological team. Assessment was made at the beginning (t1) and end (t2) of the stay in the hospital
Received emotional support
Upon discharge from the hospital (t2), patients indicated having received emotional support from physicians, nurses, social workers, psychologists, pastors, nutritionists, and self-help groups at the following percentages: 91.7, 95.2, 45.9, 33.7, 3.7, 8.6, and 4.2 (see Fig. 3).
Patients considered the support they received from nurses to be the most helpful (82%). Seventy-eight percent said the support of the physicians was helpful, and 62% of the patients who had received support from a psychologist rated this as helpful. The lowest satisfaction rates were those measuring support received from self-help groups (17%) and pastoral care (22%; Fig. 3).
In the gynecology department of Leipzig University, there was a psycho-oncological semi-liaison service introduced 1 year before the investigation started. This service included weekly visit from a psycho-oncologist on the ward and staff physicians being asked to report whether a patient needed emotional support. In all other university wards, psycho-oncological services were offered on a consultation basis, meaning that the physicians on the ward had to initiate calling for a psycho-oncologist when they thought a patient needed support. Therefore, a comparison was made between those two service modalities. It showed that 61% of the patients in the gynecology department received emotional support from a psycho-oncologist; whereas, that service was far less frequently received by patients in other departments of Leipzig University (surgical department: 32%, radiation oncology department: 31%). In the non-university hospital studied, 17% of the patients received emotional support from a psycho-oncologist.
Association between need for, desire for, and provision of emotional support
To answer the question of whether provision of emotional support is oriented to the need and/or the desire for it, chi-square values were calculated between the HADS and the desire for support at t1 and the received support at t2, which are displayed in Table 1. Results indicate that there is some evidence for an association between desire for and provision of support in nurses, social workers, psychologists, pastors, and nutritionists. The need for support, according to the HADS, was not associated with received support from any profession. Patients who wanted emotional support from a psychologist and/or another patient from a self-help group had high HADS scores far more frequently. Desire for support from other members of the oncological team was not associated with mental distress. Emotional support received from physicians depended neither on a desire nor a need for support on the part of the patient.
Unfortunately, the distribution of the data for support by physicians, nurses, pastors, nutritionists, and self-help groups did not allow performing subsample analyses. Either most of the patients or only few of them desired and/or received support from those professions. Hence, the number of patients in some “cells” of the analysis is too small for further partition into groups. We did however perform a logistic regression analysis for support by psychologists and social workers as we have more equally distributed data for those. Exposure variables entered in the model were gender, tumor stage, life expectancy, desire for support, and need for support. The outcome variables were received support by social workers and psychologists, respectively. Desire for support remained the only variable with explanatory power in both models. The odds ratios for received support by social workers in those who wanted that was 3.5 (95% confidence interval 1.8–6.6) and 3.2 (95% confidence interval 1.6–6.3) for support by psychologists, respectively. All other variables did not significantly contribute to the variance of the dependent variable “received support”.
Discussion
High quality care includes recognizing that patients’ needs, preferences, and satisfaction must be taken into consideration [15]. This is not only an ethical imperative but, nowadays, also an important factor of competition between health care institutions. Therefore, studies of patient satisfaction have often been performed from a perspective of quality assurance [16, 17]. Unfortunately, the quality assurance managers behind these efforts seem at times to be unfamiliar with survey research [1, 18], resulting in a “quality literature of poor quality”. Most notably, there is a lack of studies that have used reliable, valid assessment tools.
With this prospective study, the perceived quality of care from the inpatient cancer patient’s perspective and the desire and need for emotional support were investigated using validated theory-based questionnaires. We wanted to find out which areas of care are important to patients and which areas need improvement. Since emotional support is known to be an essential part of cancer care but it is unclear which members of the oncological teams should be providing it [11], additional attention was paid to these aspects.
Our results show that cancer patients consider “soft factors” such as respect and commitment of the physicians as well as receiving comprehensive information before and after procedures to be very important. In accordance with this, Baberg et al. [17] found that patients focus more on how knowledgeable and attentive their doctors are than they do on medical equipment or whether or not they have a single room.
Interestingly, patients received more information before undergoing treatment than afterward. This may be because physicians are required by law to inform patients about the surgical, medical, or diagnostic procedures they are about to undergo. Physicians are also only legally allowed to operate on a patient after having received that person’s written informed consent. It is noteworthy that the patients also wanted to receive information after the completion of procedures. This is an area of care where improvement could be made with relative ease.
Other areas where action should be taken are patient participation in decision making and clarity about who is responsible for physical care. Both domains are related to communication issues and could be improved with additional training and education of health care providers.
Improving other “low quality” areas of routine care could prove more difficult, as the necessary changes would probably present more up-front costs. Examples of these are nutrition and the possibility of having confidential conversations with nurses and psycho-oncologists. The latter were, in our data, associated with time spent in hospital, indicating that patients probably have more possibilities to talk in private with nurses and psycho-oncologists the longer they stay in the hospital, resulting in higher satisfaction.
Our data also reveal that 56% of the patients at the beginning of their hospital stays were highly distressed emotionally and in need of psycho-oncological support as were 48% of the patients upon hospital discharge. Of these, 33% would like to have gotten professional support from a psychologist. This result is in concordance with Faller et al. [11] who found that 36% of breast cancer patients wanted to talk with a psychotherapist. Interestingly, he also asked physicians and nurses whether they thought patients wanted support from a psychotherapist. Those percentages were much higher. The physicians thought that 86% wanted psychosocial support from a psychotherapist, while nurses even thought that all of the patients would prefer this. They also thought that all of the patients wanted help from a pastor (43% of the physicians thought that), though, in fact, only 12% of the patients responded accordingly. In our study, only 7% wanted to see a pastor. This could be explained by the fact that our survey was performed in eastern Germany where fewer people are members of a church than in western Germany.
Most importantly, 84% of our study patients said they wanted to receive psychosocial support from their doctors. In fact, they often did receive support from physicians. This support, however, turned out to be related neither to their needs nor desires. How can this be? We cannot give any good explanation based on either our data or the literature. It could be that the amount and quality of emotional support provided by physicians was due singly to the personality or internal attitude of particular doctors of being helpful and attentive, but this is only a vague hypothesis. Further studies should investigate this more in detail.
Another one of our findings was that only a portion of the 34% of the patients who wanted to talk with a psychotherapist received such support. Many more patients in the liaison service condition got emotional support from a psychologist than in the consultation service condition. Of the patients who received support from a psychologist, 62% rated this as having been very helpful (in contrast to the support of self-help groups and pastoral care). This leads us to a certain dilemma—support from self-help groups and pastors are gratuitous for hospitals; whereas, psychologists must be paid. The patients in our study, however, preferred seeing a psychologist and rated the helpfulness of this service much higher. Some of the patients also wanted to see a member of a self-help group or a nutritionist but did not get to do this. The discrepancy between desired and received support in those two groups is especially high.
With this study, we aimed to provide some insight into areas of care that could be improved in order to enhance cancer patients’ satisfaction. Some of our results have ramifications for daily clinical care as well. The study does, however, have several limitations, and our results should be interpreted accordingly. First of all, the subjective importance of the different aspects of care was assessed at the end of patients’ time in the hospital. It is possible that participants would have rated these things differently at the beginning of their stays. Secondly, the perceived quality of care was not assessed a second time after discharge. As Giebel and Groeben [19] have shown, satisfaction tends to be lower over the course of time due to social desirability. We, however, measured satisfaction shortly before discharge so that patients need not feel fearful of receiving worse treatment as a result of criticizing the staff or the institution.
Conclusion
We can conclude that the QPP is a useful instrument for evaluating patients’ perspective on quality of care. It can easily be amended by additional items for specific research questions [20, 21] and reveals areas that can be improved in the clinic. Some of these, e.g., providing more information to patients after procedures, would be relatively easily to change simply by identifying the problem. Others, such as providing support from a psycho-oncologist for example, require financial and personal resources that have to be agreed upon by hospital owners or health insurance providers, making for a more involved process of change. The third area involves physician-patient communication. Thorough and continuous education of medical students and physicians is a key to equipping hospital staffs with these skills [22, 23]. We have seen, however, in accordance with others [24], that commitments of the physicians and the possibility to talk to them in private as well as patients’ involvement in the treatment are important factors of satisfaction with care.
The fourth finding of our study, namely the fact that the present provision of emotional support by doctors is not related to the desires or needs of patients, needs further studies, presumably with in-depth analyses.
The main result of our study is the recognition that emotional support is a crucial part of patient satisfaction and should be delivered by several members of oncological teams, particularly physicians trained in this area.
References
Sitzia J (1999) How valid and reliable are patient satisfaction data? An analysis of 195 studies. Int J Qual Health Care 11:319–328. doi:10.1093/intqhc/11.4.319
Lynn MR, McMillen BJ (2004) The scale product technique as a means of enhancing the measurement of patient satisfaction. Can J Nurs Res 36:66–81
Wilde B, Larsson G, Larsson M, Starrin B (1994) Quality of care. Development of a patient-centered questionnaire based on a grounded theory model. Scand J Caring Sci 8:39–48
Larsson G, Larsson BW, Munck IME (1998) Refinement of the questionnaire ‘quality of care from the patient's perspective’ using structural equation modelling. Scand J Caring Sci 12:111–118. doi:10.1080/02839319850163048
Nathorst-Böös J, Munck IME, Eckerlund I, Ekfeldt-Sandberg C (2001) An evaluation of the QSP and the QPP: two methods for measuring patient satisfaction. Int J Qual Health Care 13:257–264. doi:10.1093/intqhc/13.3.257
Wilde Larsson B, Larsson G (2002) Development of a short form of the quality from the patient’s perspective (QPP) questionnaire. J Clin Nurs 11:681–687. doi:10.1046/j.1365-2702.2002.00640.x
Schmidt C, Möller J, Reibe F, Güntert B, Kremer B (2003) Patientenzufriedenheit in der stationären Versorgung. Stellenwert, Methoden und Besonderheiten. Dtsch Med Wochenschr 128:619–624. doi:10.1055/s-2003-38055
Larsson BW, Larsson G, Chantereau MW, Von Holstein KS (2005) International comparisons of patients’ views on quality of care. Int J Health Care Qual Assur Inc Leadersh Health Serv 18:62–73
Beger HG (2005) 145 years of Langenbeck’s archives: the oldest journal worldwide in scientific surgery. Langenbecks Arch Surg 390:75–76. doi:10.1007/s00423-005-0548-5
Weis J, Koch U, Matthey K (1998) Need for psychosocial care of oncology patients—analysis of present state and need in Germany. Psychother Psychosom Med Psychol 48:417–425
Faller H, Olshausen B, Flentje M (2003) Emotional distress and needs for psychosociol support among breast cancer patients at start of radiotherapy. Psychother Psychosom Med Psychol 53:229–235. doi:10.1055/s-2003-38864
Muthny FA, Faller H, Küchenmeister U, Mücke K, Oberpennig R, Rodi B, Schlömer-Doll U, Schmitz-Huebner U, Stecker R, Winter B (1998) Psychoonkologie: Bedarf, Maßnahmen und Wirkungen am Beispiel des ‘Herforder Modells’. Pabst Science Publishers, Lengerich
Singer S, Danker H, Dietz A, Hornemann B, Koscielny S, Oeken J, Matthäus C, Vogel H-J, Krauß O (2008) Screening for mental disorders in laryngeal cancer patients: a comparison of six methods. Psychooncology 17:280–286. doi:10.1002/pon.1229
Singer S, Kuhnt S, Götze H, Hauss J, Hinz A, Liebmann A, Krauß O, Lehmann A, Schwarz R (2009) Hospital anxiety and depression scale cut-off scores for cancer patients in acute care. Br J Cancer 100:908–912. doi:10.1038/sj.bjc.6604952
Ronellenfitsch U, Rössner E, Jakob J, Post S, Hohenberger P, Schwarzbach M (2008) Clinical pathways in surgery—should we introduce them into clinical routine? A review article. Langenbecks Arch Surg 393:449–457. doi:10.1007/s00423-008-0303-9
Tisch M, Schettilin J, Maier H (2002) Patient satisfaction in the hospital. Results of a prospective study in an ENT department. HNO 50:70–75. doi:10.1007/s106-002-8071-4
Baberg HT, Jäger D, Bojara W, Lemke B, Von Dryander S, De Zeeuw J, Barmeyer J, Kugler J (2001) Expectations and satisfaction among patients during inpatient stay. Gesundheitswesen 63:297–301. doi:10.1055/s-2001-14213
Sitzia J, Wood N (1998) Response rate in patient satisfaction research: an analysis of 210 published studies. Int J Qual Health Care 10:311–317. doi:10.1093/intqhc/10.4.311
Giebel GD, Groeben N (2008) Social desirability in the measuring of patient satisfaction after treatment of coloproctologic disorders. Langenbecks Arch Surg 393:513–520. doi:10.1007/s00423-008-0310-x
Persson F, Wilde Larsson B (2005) Quality of care after ostomy surgery: a perspective study of patients. Ostomy Wound Manage 51:40–48
Muntlin A, Gunningberg L, Carlsson M (2006) Patients’ perceptions of quality of care at an emergency department and identification of areas for quality improvement. J Clin Nurs 15:1045–1056. doi:10.1111/j.1365-2702.2006.01368.x
Fallowfield L (1995) Can we improve the professional and personal fulfillment of doctors in cancer medicine? Br J Cancer 71:1132–1133
Fallowfield L, Lipkin M, Hall A (1998) Teaching senior oncologists communication skills: results from phase I of a comprehensive longitudinal program in the United Kingdom. J Clin Oncol 16:1961–1968
Janssen C, Ommen O, Neugebauer E, Lefering R, Pfaff H (2007) How to improve satisfaction with hospital stay of severely injured patients. Langenbecks Arch Surg 392:747–760. doi:10.1007/s00423-007-0186-1
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the German Federal Ministry of Education and Research (# 01ZZ0106).
The manuscript has not been published or submitted elsewhere.
Rights and permissions
About this article
Cite this article
Singer, S., Götze, H., Möbius, C. et al. Quality of care and emotional support from the inpatient cancer patient’s perspective. Langenbecks Arch Surg 394, 723–731 (2009). https://doi.org/10.1007/s00423-009-0489-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-009-0489-5