Abstract
Background and aims
Patients with sporadic medullary thyroid carcinoma (MTC) have a variable clinical course. Our aim was to analyse the reduction of tumour markers after thyroidectomy with meticulous dissection and relate it to clinical outcome.
Materials and methods
Twenty consecutive patients with palpable sporadic MTC underwent thyroidectomy with central and uni- or bilateral modified radical neck dissection; three were subjected to mediastinal dissection. Basal (b-) and stimulated (s-) calcitonin (CT) and carcinoembryonic antigen (CEA)-levels were measured before and 6–8 weeks after primary surgery, and the reduction of these tumour markers was determined.
Results
Median CT (b- and s-) were markedly reduced after surgery (98.5% and 99.1%, respectively), and CEA decreased 11 times. CT (b-) fell >99% in seven patients after surgery; in these and four additional patients, CT (s-) showed a similar reduction. During follow-up (median 52.5 months), two patients (stages IV B and C) died of MTC; they had <95% reduction of CT. Four patients (stage IV A) are alive with verified metastases. Eight patients (one stage III, seven stage IV A) are alive with hypercalcitoninemia. Five stages I–III patients and one stage IV A patient are disease-free.
Conclusions
Thyroidectomy and meticulous dissection caused a pronounced reduction of tumour markers. A postoperative reduction of CT (s-) ≥97% seems to be associated with less aggressive clinical course, while CEA had lower predictive value.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medullary thyroid carcinoma (MTC) is characterised by early spread to regional lymph nodes and distant sites. Calcitonin (CT) has an established role as a very sensitive and rather specific tumour marker, both biochemically and histochemically [1]. Carcinoembryonic antigen (CEA) is an integrated part of the cell membrane of MTC tumour cells, from where it can be released and thus serve as a tumour marker [2]. The prognosis of MTC is very variable but relates to tumour stage at diagnosis [3–6]. Sporadic MTC (75% of cases) usually presents clinically as a mass in the neck but can also be diagnosed due to distant metastases and/or diarrhoea symptoms [7]. In palpable, clinically overt MTC, lymph node metastases in the neck are found in 75–80% of patients at diagnosis [8]. The presence and extent of lymph node involvement in MTC is a negative prognostic factor, associated with large size of the primary tumour. Since surgery is the only cure for MTC, the extent of regional lymph node disease and its resectability decides whether the patient is curable or not. More than ten metastatic lymph nodes have been reported to be incompatible with biochemical cure [9–11]. In most series, the biochemical cure rate after extensive primary neck surgery for sporadic MTC is 30–40% [8, 12, 13]. Thus, many patients are not biochemically cured after neck surgery but still live many years free of symptoms. Other patients have a more aggressive course with widespread disease and fatal outcome. The overall 10-year survival is approximately 70% [14]. A prognostic tool to early distinguish patients with indolent clinical course from those with more aggressive course (requiring additional treatment) is needed. In a previous study of 36 patients with MTC, our group could show that the proliferation rate (Ki67) was an independent prognostic factor [15]. The doubling time of either CT or CEA was reported as an efficient tool to assess tumour progression [16]. In this study, we have analysed the reduction of these tumour markers 6–8 weeks after thyroidectomy and related it to clinical outcome. The aim was to evaluate if the magnitude of marker reduction could serve as a reliable prognostic tool early after surgery.
Materials and methods
Between August 1996 and February 2007, 20 consecutive patients (five women and 15 men) with palpable sporadic MTC underwent surgery at the Department of Surgery, Sahlgrenska University Hospital. The median age was 47.5 (24–78) years. Patients with hereditary MTC or recurrent tumours were not included in this series.
Preoperatively, all patients had undergone fine-needle aspiration cytology (FNAC) of their thyroid nodules. Measurements of basal (b-) and pentagastrin-stimulated (s-; Peptavlon®, Cambridge Laboratory, Newcastle, UK, 0.6 μg/kg) CT, as well as basal CEA (reference, <5 μg/l) in serum were performed. Serum CT was measured using a solid-phase two-site immunoradiometric assay [calcitonin ultrasensitive (CT-US), Biosource; reference, <20 ng/l]. Blood samples were drawn at 0, 2 and 5 min after an intravenous bolus injection of pentagastrin. Screening for pheochromocytoma and hyperparathyroidism by analysis of urinary catecholamines and serum calcium was performed. Radiological staging with computed tomography of the neck and thorax was performed in all patients. All patients were also screened for RET mutations before surgery.
The surgical treatment for patients with primary sporadic MTC at our unit includes total thyroidectomy with bilateral central lymph node dissection and ipsi- or bilateral lateral lymph node dissection. Bilateral lymph node dissection is performed if suspect lymph nodes are detected pre- or peroperatively. Mediastinal exploration is performed in individual patients based on radiological findings.
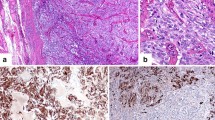
All specimens from resected primary tumours and metastases were investigated histopathologically and analysed immunohistochemically for expression of CT. The tumour stage was classified according to the International Union Against Cancer, 6th edition, 2002 [17]. The mean Ki67 index was determined by counting the total number of tumour cells and the number of Ki67-positive nuclei in randomly selected high-power fields (MIB-1, monoclonal, code no. M7240, 1:100 dilution, DakoCytomation Denmark A/S Glostrup Denmark).
The first postoperative evaluation, including both basal and stimulated CT, was made 6–8 weeks after primary surgery. Depending on tumour stage, the patients were examined every 3, 6 or 12 months in the outpatient clinic. For patients with elevated CT (b- and/or s-) postoperatively or during follow-up, our localisation protocol included ultrasound of the neck or computed tomography or magnetic resonance imaging of the neck, thorax and abdomen. In patients with elevated tumour markers (persistent or recurrent disease) without radiologically visualised lesions, catheterisation of the cervical veins combined with measurement of CT (b- and s-), 18F-FDG-PET, octreotide scintigraphy, bone scintigraphy and a diagnostic laparoscopy with liver biopsies were performed.
Results
The preoperative FNAC with immunocytochemical demonstration of CT gave correct diagnosis in all cases. The histopathology after primary surgery demonstrated MTC (tumour cells immunopositive for CT and CgA but negative for thyroglobulin). All patients underwent total thyroidectomy with bilateral central lymph node dissection; 13 patients underwent ipsilateral and seven patients bilateral modified radical neck dissection. In three of the seven patients with bilateral modified radical neck dissection, sternotomy with mediastinal lymph node dissection was performed as well.
Preoperatively, the median CT (b- and s-) was 4,740 (119–28,700) ng/l and 69,000 (211–412,000) ng/l. The median CEA level was 84 (1.2–710) μg/l. Biochemical screening for pheochromocytoma and hyperparathyroidism was negative in all patients. No patient had a RET mutation.
After formalin fixation, the median tumour size was 31.5 (6–55) mm. In 15 out of 20 patients, the thyroid tumour was solitary. Multiple unilateral tumours and bilateral tumours were seen in two and three patients, respectively. Tumour capsule invasion was seen in 13 out of 20 (65%) thyroid specimens. The median Ki67 index in the primary tumour was 0.81% (<0.1–20.9%). The median number of examined cervical lymph nodes was 42 (23–73), and the median number of positive lymph nodes was 12 (0–37). The median number of positive cervical lymph nodes in the central and lateral compartments was 3 (0–18) and 8 (0–28), respectively.
Sixteen out of 20 (80%) patients demonstrated cervical lymph node metastases at primary surgery; 12 (75%) patients had both central and lateral lymph node metastases. Two patients had only central lymph node metastases, and two patients had skip lesions (lateral metastases but no central). Of the seven patients undergoing bilateral modified radical neck dissection, three demonstrated lymph node metastases in the contra-lateral lateral compartment. Only one patient had visualised distant metastatic disease at primary surgery (Table 1).
At the first visit 6–8 weeks postoperatively, the median CT (b- and s-) was 69.1 (1–5,090) ng/l and 616 (1.5–93,500) ng/l for the entire group (Table 2). The reduction was very prominent for patients with stages I–III tumours (except basal CT in patient no. 1, Table 3). The median CEA was 7.65 (0.76–100) μg/l postoperatively. The median reduction of CEA was less pronounced than for CT. It should be noted that 96% reduction of CEA was seen in two patients (nos. 19 and 20) with very large tumour burden with macroscopically residual disease (Table 3).
In eight out of 12 patients with stage IV A, CT (s-) was decreased by ≥97%. All these eight patients were resected for cure, but only one patient (no. 7) is currently judged to be disease-free. In the entire series, seven patients had a reduction of postoperative b-CT >99% vs. preoperative values. In these and four additional (55%) patients, s-CT fell ≥99% vs. preoperative values (Table 3).
During follow-up, ten patients with stages IV A and C underwent repeat surgery because of radiological findings and/or elevated CT; six patients had removal of tumour tissue but were not biochemically cured. In all, 24 repeat procedures have been performed in these patients to date. Four patients (nos. 8, 14, 16 and 17) with stage IV A had <90% CT reduction; two of these developed distant metastatic disease (Table 3).
At latest follow-up at 52.5 (range 9–132) months, two patients (stages IV B and C) had died from their MTC. Four patients, all stage IV A, were alive with radiologically verified disease. Eight patients (one stage III and seven stage IV A) had elevated CT without radiologically detectable MTC. Finally, six patients (five stages I–III and one stage IV A) are considered to be free of disease (Table 3).
Discussion
In this study, we found that patients with palpable sporadic MTC subject to meticulous surgery leading to a reduction of the most sensitive tumour marker, CT (s-), exceeding 97% seem to have less aggressive clinical course; for patients with stages I–III tumours, all except one were judged to be biochemically cured, and only one out of eight patients with stage IV A tumours was considered to be biochemically cured. Thus, it seems as if the early postoperative reduction in CT levels may be used as an early prognostic marker in patients with sporadic MTC but must be combined with tumour stage for more accurate prognostication. Since this study was limited to 20 consecutive patients, the validity of this finding needs to be studied in a larger series of MTC patients.
CEA is another tumour marker in MTC. It has been demonstrated that there is an almost linear relationship between abnormal preoperative CEA levels and increasing tumour size and number of lymph node metastases, both reflecting the overall tumour cell mass [18]. Since CEA is not released upon pentagastrin stimulation, this marker is not used for screening of occult disease [18, 19]. Machens et al. reported that CEA levels over 30 ng/ml indicated presence of central or ipsilateral lymph node metastases; levels over 100 ng/ml indicated presence of contralateral and distant metastases [20]. In this study, the postoperative reduction of CEA was less reliable in predicting clinical outcome, and it seems unlikely that CEA will serve as an early prognostic marker. Analysis of CEA at later stage may better correlate with the clinical course, since minimal residual tumours or recurrent tumours then have grown to detectable size.
The tumour cell proliferative index (Ki67) was previously reported by our group to be an independent prognostic factor in a study of 36 patients with MTC and long follow-up [15]. By using a Poisson model, it was possible to estimate the median survival time for individual patients using the Ki67 index (10.000 nuclear profiles in each specimen) for the primary tumour and patient age at surgery. To predict prognosis, three cut-off levels for Ki67 were defined: 1.0, 2.0 and 4.5. In this series, one of the patients (no. 6) with stages I–III tumours had a Ki67 index >2.0, while only two out of 12 patients with stage IV A tumours exceeded this level. One patient with a stage IV B tumour (no. 19) had very high Ki67 index (20.9) and died within the first year after surgery. The other deceased patient (no. 20) had distant metastases at diagnosis but a very low Ki67 index (0.4%) and lived for more than 3 years. Other authors have not been able to show that the Ki67 index, or mitotic rate, was significantly associated with disease progression [16]. Whether the Ki67 index in association with age at surgery will fall out as an independent prognostic factor in this series with longer observation time remains to be seen.
Known prognostic factors in MTC are age at diagnosis, tumour stage and number of lymph node metastases [1, 14, 21], which all can be collected shortly after surgery. Since MTC confined to the neck is a surgically curable disease, an early prognostic tool to predict the clinical course would be most valuable. Patients with less favourable prognosis could then be subject to additional therapy or more intense surveillance. Assessment of CT and CEA doubling times in series with longer observation time has been reported to be efficient prognostic tools in MTC patients [16]. The results of the present study indicate that CT (s-) 6–8 weeks after surgery, judged together with tumour stage, could be a useful prognosticator in patients with sporadic MTC.
Conclusion
Thyroidectomy with meticulous neck dissection in patients with clinically detected sporadic MTC led to a marked reduction of tumour markers (basal and stimulated CT and CEA) in peripheral blood. A postoperative reduction of stimulated CT ≥97% was associated with excellent prognosis in patients with stages I–III tumours. Similar reduction in patients with stage IV tumours was seldom associated with cure, but these patients seemed to have less aggressive clinical course.
References
Machens A, Hauptmann S, Dralle H (2007) Increased risk of lymph node metastasis in multifocal hereditary and sporadic medullary thyroid cancer. World J Surg 31:1960–1965
Osamura RY, Yasuda O, Kawakami T, Itoh Y, Inada K, Kakudo K (1997) Immunoelectron microscopic demonstration of regulated pathway for calcitonin and constitutive pathway for carcinoembryonic antigen in the same cells of human medullary carcinomas of thyroid glands. Mod Pathol 10:7–11
Girelli ME, Nacamulli D, Pelizzo MR, De Vido D, Mian C, Piccolo M, Busnardo B (1998) Medullary thyroid carcinoma: clinical features and long-term follow-up of seventy-eight patients treated between 1969 and 1986. Thyroid 8:517–523
Gharib H, McConahey WM, Tiegs RD, Bergstralh EJ, Goellner JR, Grant CS, van Heerden JA, Sizemore GW, Hay ID (1992) Medullary thyroid carcinoma: clinicopathologic features and long-term follow-up of 65 patients treated during 1946 through 1970. Mayo Clin Proc 67:934–940
Modigliani E, Cohen R, Campos JM, Conte-Devolx B, Maes B, Boneu A, Schlumberger M, Bigorgne JC, Dumontier P, Leclerc L, Corcuff B, Guilhem I (1998) Prognostic factors for survival and for biochemical cure in medullary thyroid carcinoma: results in 899 patients. The GETC Study Group. Groupe d’étude des tumeurs à calcitonine. Clin Endocrinol 48:265–273
Hundahl SA, Cady B, Cunningham MP, Mazzaferri E, McKee RF, Rosai J, Shah JP, Fremgen AM, Stewart AK, Hölzer S (2000) Initial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the united states during 1996. U.S. and German Thyroid Cancer Study Group. An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer 89:202–217
Moley JF, Fialkowski EA (2007) Evidence-based approach to the management of sporadic medullary thyroid carcinoma. World J Surg 31:946–956
Moley JF, DeBenedetti MK (1999) Patterns of nodal metastases in palpable medullary thyroid carcinoma: recommendations for extent of node dissection. Ann Surg 229:880–887
Machens A, Gimm O, Ukkat J, Hinze R, Schneyer U, Dralle H (2000) Improved prediction of calcitonin normalization in medullary thyroid carcinoma patients by quantitative lymph node analysis. Cancer 88:1909–1915
Weber T, Schilling T, Frank-Raue K, Colombo-Benkmann M, Hinz U, Ziegler R, Klar E (2001) Impact of modified radical neck dissection on biochemical cure in medullary thyroid carcinomas. Surgery 130:1044–1049
Scollo C, Baudin E, Travagli JP, Caillou B, Bellon N, Leboulleux S, Schlumberger M (2003) Rationale for central and bilateral lymph node dissection in sporadic and hereditary medullary thyroid cancer. J Clin Endocrinol Metab 88:2070–2075
Fleming JB, Lee JE, Bouvet M, Schultz PN, Sherman SI, Sellin RV, Friend KE, Burgess MA, Cote GJ, Gagel RF, Evans DB (1999) Surgical strategy for the treatment of medullary thyroid carcinoma. Ann Surg 230:697–707
Gimm O, Ukkat J, Dralle H (1998) Determinative factors of biochemical cure after primary and reoperative surgery for sporadic medullary thyroid carcinoma. World J Surg 22:562–567
Pelizzo MR, Boschin IM, Bernante P, Toniato A, Piotto A, Pagetta C, Nibale O, Rampin L, Muzzio PC, Rubello D (2007) Natural history, diagnosis, treatment and outcome of medullary thyroid cancer: 37 years experience on 157 patients. Eur J Surg Oncol 33:493–497
Tisell LE, Oden A, Muth A, Altiparmak G, Mölne J, Ahlman H, Nilsson O (2003) The Ki67 index a prognostic marker in medullary thyroid carcinoma. Br J Cancer 89:2093–2097
Laure Giraudet A, Al Ghulzan A, Aupérin A, Leboulleux S, Chehboun A, Troalen F, Dromain C, Lumbroso J, Baudin E, Schlumberger M (2008) Progression of medullary thyroid carcinoma: assessment with calcitonin and carcinoembryonic antigen doubling times. Eur J Endocrinol 158:239–246
TNM classification of malignant tumours (2002) Wiley-Liss, New York
Busnardo B, Girelli ME, Simioni N, Nacamulli D, Busetto E (1984) Nonparallel patterns of calcitonin and carcinoembryonic antigen levels in the follow-up of medullary thyroid carcinoma. Cancer 53:278–285
Wells SA Jr, Haagensen DE Jr, Linehan WM, Farrell RE, Dilley WG (1978) The detection of elevated plasma levels of carcinoembryonic antigen in patients with suspected or established medullary thyroid carcinoma. Cancer 42:1498–1503
Machens A, Ukkat J, Hauptmann S, Dralle H (2007) Abnormal carcinoembryonic antigen levels and medullary thyroid cancer progression: a multivariate analysis. Arch Surg 142:289–293
Miccoli P, Minuto MN, Ugolini C, Molinaro E, Basolo F, Berti P, Pinchera A, Elisei R (2007) Clinically unpredictable prognostic factors in the outcome of medullary thyroid cancer. Endocr Relat Cancer 14:1099–1105
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors reported any conflict of interest.
Best of Endocrine Surgery in Europe 2008.
Rights and permissions
About this article
Cite this article
Bümming, P., Ahlman, H., Nilsson, B. et al. Can the early reduction of tumour markers predict outcome in surgically treated sporadic medullary thyroid carcinoma?. Langenbecks Arch Surg 393, 699–703 (2008). https://doi.org/10.1007/s00423-008-0375-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0375-6