Abstract
Background
One strategy to reduce the consumption of resources associated to specific procedures is to utilize clinical pathways, in which surgical care is standardized and preset by determination of perioperative in-hospital processes. The aim of this prospective study was to establish the impact of clinical pathways on costs, complication rates, and nursing activities.
Method
Data was prospectively collected for 171 consecutive patients undergoing laparoscopic cholecystectomy (n = 50), open herniorrhaphy (n = 56), and laparoscopic Roux-en-Y gastric bypass (n = 65).
Results
Clinical pathways reduced the postoperative hospital stay by 28% from a mean of 6.1 to 4.4 days (p < 0.001), while the 30-day readmission rate remained unchanged (0.5% vs. 0.45%). Total mean costs per case were reduced by 25% from € 6,390 to € 4,800 (p < 0.001). Costs for diagnostic tests were reduced by 33% (p < 0.001). Nursing hours decreased, reducing nursing costs by 24% from € 1,810 to € 1,374 (p < 0.001). A trend was noted for lower postoperative complication rates in the clinical pathway group (7% vs. 14%, p = 0.07).
Conclusions
This study demonstrates clinically and economically relevant benefits for the utilization of clinical pathways with a reduction in use of all resource types, without any negative impact on the rate of complications or re-hospitalization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Costs in health care systems are rising every year, reaching € 35.3 billion (euro) in Switzerland for the year 2005 or 11.6% of the gross domestic product and are estimated to reach € 36.6 billion in 2007. This is the second largest amount spent in countries of the Organisation for Economic Cooperation and Development after the USA, which spends 15.3% of its gross domestic product for the health system. Other countries spent similar proportions (UK 8.3%, France 10.5%, and Germany 10.9%). In Switzerland, € 12.3 billion, or 35% of total health care costs, were generated by hospitals [1]. This figure is similar to other countries, e.g., in the US [2]. It should be noted that surgical departments are responsible for about a third of all hospital costs.
Because rationalization efforts to reduce costs are problematic and reluctantly accepted by the public, other approaches are needed. An acceptable strategy incorporates the reduction of costs without loss of quality. Costs and consumption of resources in hospitals can be reduced by optimization of in-hospital processes. With clinical pathways, also called critical pathways or care maps, surgical care is standardized and preset by determination of perioperative in-hospital processes.
Benefits related to clinical pathways have been shown in some conditions treated by internists [3–5]. In surgery, the impact of clinical pathways on resource utilization remains unclear. A few studies are available, but are restricted to a single procedure, and cost analyses are mainly based on the length of hospital stay [6–15] (see Table 4). Most studies come from the US [16] and two thirds of studies on clinical pathways were classified as of low quality [17]. Notably, the issue of safety related to preset simplified flow sheets has not been addressed. Moreover, no data is available on the impact on nursing activities.
Therefore, we designed a prospective study to investigate the impact of clinical pathways on a variety of clinically relevant parameters, including utilization of a variety of resources and costs. Complications were analyzed using a standardized validated grading system [18]. The nursing activities were assessed in 12 categories and measured in hours of work. A cohort study type using a control group of similar patients treated just before the introduction of the clinical pathways was chosen.
Methods
Study design
To assess the impact of clinical pathways at a major surgical university teaching hospital with a broad spectrum of abdominal procedures, we selected one routine open (hernia repair) and one routine laparoscopic procedure (cholecystectomy) as well as a more complex laparoscopic operation (Roux-en-Y gastric bypass). After the introduction of clinical pathways, the study patients were prospectively registered. This data was compared to a control group of patients treated without clinical pathways.
Implementation of clinical pathways
Clinical pathways were developed in cooperation with all staff surgeons and nurses of the Department for Visceral and Transplantation Surgery, University Hospital Zurich. The clinical pathways consisted of standardized order forms presetting fluid management, nutrition, analgesia, reserve medications, preoperative examinations, detailed laboratory blood testing, and planned discharge (Fig. 1). In addition, a separate document providing clear guidelines and specific explanations for the doctors, the nurses, and the patients was made available. All patients received information on in-hospital care, planned time of discharge, and recovery time in the outpatient clinic prior to hospitalization.
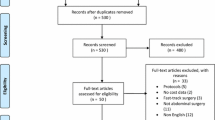
Study population
After an introduction phase of 2 months, each consecutive patient undergoing the abovementioned procedures was prospectively enrolled in the study during a 6-month period. Fifty laparoscopic cholecystectomies, 56 open hernia repairs, and 65 laparoscopic Roux-en-Y gastric bypasses were performed during the study period. The study patients were compared to a control group which underwent the same procedures during a 1-year period prior to the introduction of the clinical pathways. This control group consisted of 106 laparoscopic cholecystectomies, 103 open hernia repairs, and 105 laparoscopic gastric bypass procedures in which data were collected prospectively. The exact period of data collection was only known to the involved investigators.
Study endpoints and cost calculation
The primary study endpoints were chosen with respect to the targeted impact of the clinical pathways, which were costs of medical examinations and hospital stay. The amount of laboratory tests, X-ray examinations, and other additional examinations was assessed and multiplied by the respective costs of each test. Length of hospital stay was multiplied by the actual costs for the room and catering per day, generating infrastructure costs.
Costs for the surgical procedure itself (operation and anesthesia) were not analyzed because the clinical pathways were not designed to influence them.
To evaluate the safety of clinical pathways, severity of in-hospital complications was stratified using a validated, therapy-orientated classification system [18].
Nursing hours
Nursing activities were recorded by the nursing staff for every patient grouped into 12 categories and measured in hours: mutation (check in/out; transfer to another ward, X-ray department, etc.), mobilization, body care, eating/drinking, sanitation, dialogue with the patient, documentation, dialogue with co-workers, surveillance, blood sampling, medication, and treatment (wound dressings, management of iv lines, and so on). Total nursing hours as well as nursing hours per day were recorded to compare the direct influence on nursing intensity. For cost calculations, one nursing hour was equivalent to € 61.9 according to the hospital policy.
Sample size calculation and statistical analysis
Data of a pilot study group without clinical pathways and the theoretical values for the ideal patient following strictly a clinical pathway were entered in a power calculation. As a result, the differences for costs of examinations and hospital stay were 39% and 33% for cholecystectomies, 30% and 18% for hernia repairs, and 54% and 40% for gastric bypass, respectively. With a power of 90% (1 − β) and a type I error α of 5% the calculated sample sizes resulted in 45 cholecystectomies, 55 hernia repairs, and 27 bypass operations.
Statistical analysis was performed using standard software SPSS 11.0 for Windows (SPSS, Chicago, Illinois, USA). To compare continuous variables between the groups, the Mann–Whitney U test was used. Dichotomous variables were compared using the chi-square test or when appropriate, Fischer’s exact test was applied. Results are expressed as means and standard deviation unless otherwise stated. A p-value of less than 0.05 was considered to indicate statistical significance.
Results
Overall, 171 patients treated according to clinical pathways were compared to 314 patients treated prior to the implementation of clinical pathways. The two groups were comparable regarding age, 46.2 vs. 47.3 years (p = 0.6), mean ASA 2.09 vs. 2.07 (p = 0.7) as well as gender distribution, 47 vs. 54% female patients (p = 0.09).
How did clinical pathways reduce the use of perioperative examinations?
No difference could be observed for the amount of preoperative chest X-rays performed in the two groups, but unnecessary ECG and respiratory function testing were significantly reduced by 30% (p < 0.001) and 63% (p < 0.001), respectively. The number of blood tests also decreased significantly, reducing costs of hematograms by 26% (p = 0.002) and blood chemistry by 34% (p < 0.001) (Table 1).
Did clinical pathways influence morbidity?
In-hospital complications occurred in 11% of all patients. There was no significant difference regarding complication rates in the clinical pathway group (7% vs. 14%, p = 0.07). The severity of complications did not change with the introduction of clinical pathways (Table 2).
How did clinical pathways influence nursing activities?
The recorded total nursing hours decreased for all patients from 29.2 to 22.2 h by 24% (p < 0.001), an effect partially accountable to the shortened hospital stay. The total nursing hours per patient and day did not change significantly, from 3.8 to 3.67 h, or −3.5% (p = 0.213). However, after the introduction of clinical pathways, nurses recorded more time for the dialogue with the individual patient, which increased by 34% (p < 0.001). Additionally, more time (+5.1%) was used for documentation, whereas less time was spent performing the duties in most of the other nursing categories (Fig. 2).
How was the compliance to clinical pathways in all patients?
To evaluate the compliance with the clinical pathways, the number of patients who strictly followed their predicted course in respect to hospital stay was analyzed. Patients had a hospital stay of precisely or less than the proposed value after gastric bypass in 69%, after cholecystectomy in 70%, and after hernia repair in 86%.
How did clinical pathways impact hospital stay and costs?
The mean length of hospital stay decreased from 7.6 to 5.8 days (23%) using clinical pathways (p < 0.001); the postoperative length of stay was shortened by 28% (p < 0.001). The readmission rate within 30 days after discharge was unchanged (0.5% vs. 0.45%).
Overall, the total costs for all examinations per patient were reduced by 33% from € 1,097 to € 739 (p < 0.001). Total infrastructure costs decreased by 23% from a mean of € 3,483 to € 2,687 (p < 0.001). Nursing cost decreased by 24% from € 1,810 to € 1,374 (p < 0.001).
Total mean costs per case were reduced by 25% from € 6,390 to € 4,800 (p < 0.001); Table 3.
How did clinical pathways impact the different surgical procedures?
For the laparoscopic cholecystectomy, the postoperative length of stay was shortened by 24% whereas total costs of all examinations decreased significantly by 44%; the corresponding figures for hernia repairs were 34% and 53% and for laparoscopic gastric bypass 32% and 27%, respectively. Overall mean total costs per laparoscopic cholecystectomy were reduced by 24% from € 5,092 to € 3,879 (p < 0.001); for hernia repairs by 30% from € 3,906 to € 2,722 (p < 0.001); for laparoscopic gastric bypass by 28% from € 10,132 to € 7,296 (p < 0.001); Table 3.
Discussion
This study was designed to evaluate the impact of clinical pathways on cost saving, nursing activities, and postoperative morbidity on three elective general surgery procedures. This study demonstrates a positive impact on all examined endpoints. The length of hospital stay, as well as number of examinations, was significantly reduced without a negative impact of increased morbidity, which underscores the safety of the routine use of clinical pathways. The nursing hours decreased significantly and the pattern of nursing activities shifted, allowing nurses more time for a dialogue with patients. As a consequence, total costs, including costs for examinations, infrastructure costs, and nursing costs, were dramatically reduced.
Health care costs are rising throughout western health systems [19, 20] and pressure is increasing from governments and insurance institutions to attain an “economic” utilization of medical resources with the aim to lower expenses. On the other hand, the patient population is growing older with an increasing incidence of comorbidities. Thusly, treatment options are becoming more diversified and more expensive. This area of conflict may leave only a small scope for improvements in the daily practice [21].
One possibility of improvement is the optimization of in-hospital processes. Clinical pathways, which originate from evidence-based guidelines, are designed to standardize and optimize the current practice. The length of hospital stay is defined and unnecessary investigations are omitted. Additionally, this treatment plan is available for all health care professionals and the patient can be orientated well in advance facilitating the organization of the post-hospital recovery period. Thus, clinical pathways have the potential to save resources.
The available surgical literature on clinical pathways in Europe is sparse [11, 16]. Most studies are focusing on one single operation and on length of hospital stay [6–15] (Table 4). Costs were only analyzed with the help of general model calculations and resource utilization was not analyzed in detail [22–24]. All these studies found a reduction of hospital stay ranging between 14% and 46% as well as cost savings up to 47%. Other surveys from nursing institutions have described the use of clinical pathways, but no data was presented [25–28]. A systematic review by El Baz found that 91.3% of all studies on clinical pathways were retrospective, 59% adopted parametric statistical test, and overall 67% were classified as of low quality [17]. In the current study, we calculated detailed costs based on the used resources. The data collection was done prospectively and statistical analyses were made with non-parametric tests. We could show that not only the use of diagnostic tests could be decreased, with an associated decrease of costs by 33%, but also the length of the hospital stay, therefore reducing infrastructure costs by 23%. This resulted in a total cost reduction of 25%.
The savings effect of clinical pathways was considerably related to the reduction of the length of hospital stay. There are different reasons accounting for this effect. First, with clinical pathways, residents had clear guidelines when to discharge patients. Hence, individual variability of discharge policy was limited. Second, the day of discharge was already known to the hospital staff and, most importantly, to the patient at admission facilitating acceptance for discharge as both the patient and his relatives were prepared. However, the average length of hospitalization in Switzerland is still longer than in some other countries, for example 12.8 days vs. 7.0 days in the US [29]. This is connected to different factors related to the available health care system (e.g., low percentage of same day admissions and operations) and cultural issues. Nevertheless, clinical pathways can provide a first step in reducing length of stay, and thereby saving costs.
In this study, hernia repairs were not done ambulatorily. Indeed, hernia repairs can be done in an ambulatory setting. There are several reasons why, in this hospital, this is not the case. First, this is a tertiary referral center and patients with more complicated diseases (recurrences) and more comorbidities (patients under anticoagulation, immunosuppression, cardiovascular diseases, etc.) are referred. Second, patients in the hernia repair group are older than the other groups (median 60 years) and many older patients are reluctant to early discharge because they lack care at home. Third, this hospital, at the time of the study, did not offer same day admissions for organizational reasons as anesthetists did not see patients in the outpatient setting. Thus, 46% of the savings effect in hernia repair was related to the shortening of the hospital stay, whereas 25% were related to reduction of test used.
When using preset order forms, like in clinical pathways, the threat of uncritical adoption by residents is eminent; this could have an impact on safety issues. The impact on patients’ safety is not directly measurable because adequate tests are lacking. For example, it cannot be predicted how an omitted measurement of a C-reactive protein level can delay a timely diagnosis and treatment of a possible complication, and therefore obviate a potentially hazardous course of the hospitalization. The lack of standardized measurement of morbidity also prevents conclusive comparisons among groups of patients [30]. Most important in this study, using a recent morbidity scale system [18], we could show that clinical pathways had no measurable negative influence on the patients’ safety. Furthermore, readmission rates were similar between patients treated with or without clinical pathways.
An advantage of clinical pathways is the integration of the latest recommendations of medical societies into the preoperative patient management in respect of anesthesiology [31] or cardiology [32]. This assures that preoperative tests, such as chest X-rays or blood analyses, are done only according to state-of-the-art recommendations. The use of clinical pathways is also very helpful for teaching purposes, especially for residents in training. However, the residents’ fear of blind automatisms (“cookbook medicine”) has to be taken seriously. It is crucial that senior surgeons maintain their teaching and supervising function because clinical pathways can certainly not replace the surgical education [33].
The compliance rate with the clinical pathways in this study was 75%, which is higher than in other reports (66%) [11]. This was partially accountable to the fact that all key users, doctors, and nurses were involved in the design and implementation of the clinical pathways, an effect that was also confirmed in another study [34]. Clinical pathways have often been introduced and assessed by nursing professionals and doctors were blamed “to be slow to buy in” [28]. If the costs of their practices are well displayed, doctors and nurses can be easily convinced to change their clinical practice [35]. However, to keep in compliance with clinical pathways, an increased amount of ongoing education [33, 36] and re-evaluation has to be guaranteed. In a recent study, the implementation of clinical pathways in combination with continuous education led to a 3.5-fold reduction of inappropriate prescription of medications [4].
Nursing work hours have never been analyzed in combination with the use of clinical pathways. The total nursing hours per patient for the three analyzed operations decreased in the study population, whereas the mean nursing hours per patient increased for other operations in the same hospital. Interestingly, the pattern of activities shifted to 35% providing more time for dialogue with the patient whilst saving time in other activities such as transporting or accompanying the patient to the X-ray department or for surveillance. Medical instructions have to be explained more intensively to the patients. Shortening the hospital stay may need more medical instructions and organization time to reduce the patients’ fear and insecurity.
Ferri et al. found in a study of clinical pathways in foregut surgery that 95% of all patients were satisfied with their nursing care [37]. In this study, patient satisfaction was not specifically analyzed, but patient satisfaction, as regularly measured in the department, was not altered during the study period.
Would a randomized cost study be better to establish the value of clinical pathways? This would only be possible if patients could be allotted to independent units and if nurses and doctors would not switch between them. Otherwise, the influence of clinical pathways could not be withheld from confounding the control group. Consequently, we chose a cohort study methodology using a control group of patients treated just prior to the introduction of the clinical pathways. This “before-after” methodology is used in most trials as has been recently shown in a review article by Ronellenfitsch et al. [16]. We also included a 2-month “learning” phase with the clinical pathways to optimize their use. The methodology, however, does not account for possible secular trends that lead to a general reduction of hospital stay without the intervention of clinical pathways as has been found in a study by Dy et al. [38] in 2003. Contrariwise, before, during, and after the study period, overall mean hospital stay per patient in the department increased: 7.7 days (2004), 7.7 days (2005), 8.4 days (2006), and 8.5 days (2007). Additionally, clinical pathways have proven to reduce costs beyond secular trends as has been shown in a recent study by Vanounou et al. [39].
The proportion of costs savings is a function of percentage of procedures that can be standardized by clinical pathways and the mean saving per procedure. In a surgical department, not all procedures can be standardized, but the main workload consists of general surgical procedures. If we extrapolate from the data of this study to the general surgical department, we believe the total saving per department could exceed 20%. This extrapolation does not take into account the fact that, with a shorter hospital stay, even more patients could be treated in the same period allowing for a higher patient turnover.
In conclusion, this study demonstrates a dramatic impact of clinical pathways on hospital stay and costs, while patients’ safety remains unaffected. Additionally, the pattern of nursing activities shifted towards more time for a dialogue with the patient. Therefore, clinical pathways should become routine in all hospitals as medical resource utilization can be optimized and costs can be significantly lowered.
References
Bundesamt für Statistik: Gesundheitskosten in der Schweiz: Bundesamt für Statistik. www.bfs.admin.ch/bfs/portal/de/index/themen/gesundheit.html 2007
Smith C, Cowan C, Heffler S, Catlin A (2006) National health spending in 2004: recent slowdown led by prescription drug spending. Health Aff (Millwood) 25(1):186–196
Pfau PR, Cooper GS, Carlson MD, Chak A, Sivak MV Jr, Gonet JA et al (2004) Success and shortcomings of a clinical care pathway in the management of acute nonvariceal upper gastrointestinal bleeding. Am J Gastroenterol 99(3):425–431
Buckmaster ND, Heazlewood V, Scott IA, Jones M, Haerer W, Hillier K (2006) Using a clinical pathway and education to reduce inappropriate prescribing of enoxaparin in patients with acute coronary syndromes: a controlled study. Intern Med J 36(1):12–18
Lemberg DA, Day AS, Brydon M (2005) The role of a clinical pathway in curtailing unnecessary investigations in children with gastroenteritis. Am J Med Qual 20(2):83–89
Archer SB, Burnett RJ, Flesch LV, Hobler SC, Bower RH, Nussbaum MS et al (1997) Implementation of a clinical pathway decreases length of stay and hospital charges for patients undergoing total colectomy and ileal pouch/anal anastomosis. Surgery 122(4):699–703, discussion 703–705
Pritts TA, Nussbaum MS, Flesch LV, Fegelman EJ, Parikh AA, Fischer JE (1999) Implementation of a clinical pathway decreases length of stay and cost for bowel resection. Ann Surg 230(5):728–733
Porter GA, Pisters PW, Mansyur C, Bisanz A, Reyna K, Stanford P et al (2000) Cost and utilization impact of a clinical pathway for patients undergoing pancreaticoduodenectomy. Ann Surg Oncol 7(7):484–489
Melbert RB, Kimmins MH, Isler JT, Billingham RP, Lawton D, Salvadalena G et al (2002) Use of a critical pathway for colon resections. J Gastrointest Surg 6(5):745–752
Huerta S, Heber D, Sawicki MP, Liu CD, Arthur D, Alexander P et al (2001) Reduced length of stay by implementation of a clinical pathway for bariatric surgery in an academic health care center. Am Surg 67(12):1128–1135
Soria V, Pellicer E, Flores B, Carrasco M, Candel Maria F, Aguayo JL (2005) Evaluation of the clinical pathway for laparoscopic cholecystectomy. Am Surg 71(1):40–45
Tan JJ, Foo AY, Cheong DM (2005) Colorectal clinical pathways: a method of improving clinical outcome. Asian J Surg 28(4):252–256
Murphy MA, Richards T, Atkinson C, Perkins J, Hands LJ (2007) Fast track open aortic surgery: reduced post operative stay with a goal directed pathway. Eur J Vasc Endovasc Surg 34(3):274–278
Kennedy EP, Rosato EL, Sauter PK, Rosenberg LM, Doria C, Marino IR et al (2007) Initiation of a critical pathway for pancreaticoduodenectomy at an academic institution—the first step in multidisciplinary team building. J Am Coll Surg 204(5):917–923, discussion 923–924
Kariv Y, Delaney CP, Senagore AJ, Manilich EA, Hammel JP, Church JM et al (2007) Clinical outcomes and cost analysis of a “fast track” postoperative care pathway for ileal pouch-anal anastomosis: a case control study. Dis Colon Rectum 50(2):137–146
Ronellenfitsch U, Rossner E, Jakob J, Post S, Hohenberger P, Schwarzbach M (2008) Clinical Pathways in surgery—should we introduce them into clinical routine? A review article. Langenbecks Arch Surg 393(4):449–457
El Baz N, Middel B, van Dijk JP, Oosterhof A, Boonstra PW, Reijneveld SA (2007) Are the outcomes of clinical pathways evidence-based? A critical appraisal of clinical pathway evaluation research. J Eval Clin Pract 13(6):920–929
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Woolhandler S, Campbell T, Himmelstein DU (2003) Costs of health care administration in the United States and Canada. N Engl J Med 349(8):768–775
Berk PD (1993) Restructuring American health care financing: first of all, do no harm. Hepatology 18(1):206–215
Wilson G (1997) A dilemma—public health care. Gesundheitswesen 59(2):117–122
Calland JF, Tanaka K, Foley E, Bovbjerg VE, Markey DW, Blome S et al (2001) Outpatient laparoscopic cholecystectomy: patient outcomes after implementation of a clinical pathway. Ann Surg 233(5):704–715
Cooney RN, Bryant P, Haluck R, Rodgers M, Lowery M (2001) The impact of a clinical pathway for gastric bypass surgery on resource utilization. J Surg Res 98(2):97–101
Uchiyama K, Takifuji K, Tani M, Onishi H, Yamaue H (2002) Effectiveness of the clinical pathway to decrease length of stay and cost for laparoscopic surgery. Surg Endosc 16(11):1594–1597
Hampton DC (1993) Implementing a managed care framework through care maps. J Nurs Adm 23(5):21–27
Ellis BW, Johnson S (1999) The care pathway: a tool to enhance clinical governance. Clin Perform Qual Health Care 7(3):134–144
Riley K (1998) Care pathways. Paving the way. Health Serv J 108(5597):30–31
(1997) Lap choly pathway leads to efficiency, savings. Hosp Case Manag 5(7):125–128
Herzlinger RE, Parsa-Parsi R (2004) Consumer-driven health care: lessons from Switzerland. JAMA 292(10):1213–1220
Clavien PA, Sanabria JR, Strasberg SM (1992) Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 111(5):518–526
American Society of Anesthesiologists Task Force on Preanesthesia Evaluation (2002) Practice advisory for preanesthesia evaluation: a report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 96(2):485–496
Eagle KA, Berger PB, Calkins H, Chaitman BR, Ewy GA, Fleischmann KE et al (2002) ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 39(3):542–553
Antioch K, Chapman R, Elliott B, Santamaria N, Crawford R, Fiddes K (2001) Cost-effective clinical pathways at the Alfred Hospital: international lessons from Bayside Health, Australia. Aust Health Rev 24(4):21–29
Kinsman L, James E, Ham J (2004) An interdisciplinary, evidence-based process of clinical pathway implementation increases pathway usage. Lippincotts Case Manag 9(4):184–196
Allen JW, Hahm TX, Polk HC Jr (2003) Surgeon-led initiatives cut costs and enhance the quality of endoscopic and laparoscopic procedures. JSLS 7(3):243–247
Warner BW, Rich KA, Atherton H, Andersen CL, Kotagal UR (2002) The sustained impact of an evidenced-based clinical pathway for acute appendicitis. Semin Pediatr Surg 11(1):29–35
Ferri LE, Feldman LS, Stanbridge DD, Fried GM (2006) Patient perception of a clinical pathway for laparoscopic foregut surgery. J Gastrointest Surg 10(6):878–882
Dy SM, Garg PP, Nyberg D, Dawson PB, Pronovost PJ, Morlock L et al (2003) Are critical pathways effective for reducing postoperative length of stay. Med Care 41(5):637–648
Vanounou T, Pratt W, Fischer JE, Vollmer CM Jr, Callery MP (2007) Deviation-based cost modeling: a novel model to evaluate the clinical and economic impact of clinical pathways. J Am Coll Surg 204(4):570–579
Competing interest statements
Nothing to disclose
Role of funding source
No funding
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Müller, M.K., Dedes, K.J., Dindo, D. et al. Impact of clinical pathways in surgery. Langenbecks Arch Surg 394, 31–39 (2009). https://doi.org/10.1007/s00423-008-0352-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0352-0