Abstract
Background
Pulmonary complications occur most frequently following a transthoracic esophagectomy for esophageal cancer and would get to be lethal occasionally. In this study, we sought to determine the effect of respiratory physiotherapy, corticosteroid administration, and the use of the video-assisted thoracoscopic (VATS) esophagectomy with a small thoracotomy incision, on the incidence of pulmonary complications following a transthoracic subtotal esophagectomy.
Materials and methods
Approximately 184 patients who had undergone a right transthoracic subtotal esophagectomy for squamous cell carcinoma of the thoracic esophagus were studied. To reduce the incidence of pulmonary complications, we performed clinical trials using respiratory physiotherapy, corticosteroid administration, and the VATS-esophagectomy surgical technique.
Results
The independent risk factors for pulmonary complications in the multivariate logistic regression analysis were not administering corticosteroids, blood loss greater than 630 ml, and not providing respiratory physiotherapy. In addition, the use of a small surgical incision, less than 10 cm, for the thoracotomy had no effect on the prevention of pulmonary complications.
Conclusions
We concluded that patients with thoracic esophageal cancer could undergo a three-field dissection in comparative safety if the patients were provided with corticosteroid medication in the perioperative period, if the patients received sufficient respiratory physiotherapy, and if surgical blood loss was reduced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transthoracic subtotal esophagectomy for esophageal cancer is a highly invasive procedure and has been associated with high mortality and morbidity rates [1, 2]. Recent advances in the surgical technique, in the administration of anesthesia, and in the medical management of the perioperative period have resulted in a reduction in postoperative morbidity and mortality [3–6]. Pulmonary complications are the most common, occurring in 10–20% of patients [7–10]. Patients with severe pulmonary complications frequently require extended postoperative intensive care and extended hospitalization [8, 9].
To reduce the incidence of pulmonary complications and the risk of death in patients undergoing esophagectomy, we performed clinical trials using respiratory physiotherapy, corticosteroid administration, and the video-assisted thoracoscopic (VATS) esophagectomy surgical technique. We initiated respiratory physiotherapy in 1999 and added corticosteroid administration to the perioperative medical regimen in 2001. It has been reported that respiratory physiotherapy reduces the incidence of postoperative pulmonary complications following open surgery [11, 12]. Recent clinical studies have also reported that the prophylactic administration of corticosteroid reduces the incidence of pulmonary complications and the morbidity rate [13–15].
Recently, it has been reported that the use of thoracoscopic surgery for performing thoracic esophagectomy with radical lymphadenectomy results in better preservation of pulmonary function, an improved quality of life, and a lower mortality rate [16, 17]. Therefore, we introduced the use of video-assisted thoracoscopic surgery with a small incision in 1996.
The purpose of this study was to identify the factors which affected the rate of pulmonary complication following an esophagectomy during a 15-year period. Of specific interest was an evaluation of the effect of the changes in medical and surgical care which we introduced sequentially beginning in 1996 and determination of whether or not these changes in therapy result in a reduced incidence of pulmonary complications.
Materials and methods
Approximately 184 consecutive patients with squamous cell carcinoma of the thoracic esophagus, who underwent a one-step subtotal esophagectomy, were investigated in this study between 1991 and 2005 at Wakayama Medical University. Patients who had cervical esophageal cancers were excluded because of their different oncological characteristics and operative procedures.
All patients were directed to stop smoking and to quit drinking alcohol at the time of patients’ first visit, which was 3–4 weeks before surgery. Patients with severe esophageal stenosis were provided with intravenous total parenteral nutrition. Perioperative respiratory physiotherapy has been provided by physiatrists and physiotherapists since 1999. The respiratory physiotherapy included breathing exercises with pursed lips, huffing, coughing, abdominal respiration, and expectoration. Information was provided regarding the importance of changing positions in bed and early mobilization. In addition, the patients were instructed to perform systemic exercise, such as riding a bicycle and walking, during about 2 weeks before surgery. Deep breathing with huffing and coughing and postural drainage to assist breathing and expectoration were performed, beginning on the first postoperative day [11, 12].
The administration of corticosteroid medication was initiated in 2001. Intravenous methylprednisolone (125 mg) was administered twice to each patient, at the start of the thoracotomy and at the conclusion of the operation.
The patients underwent radical esophagectomy with a two or three-field lymph node dissection via a cervicothoracoabdominal approach. We performed a conventional esophagectomy through a right posterolateral incision of 30 cm length through 1995. Between 1996 and 2000, we performed the VATS-esophagectomy, accomplished via a small anterolateral thoracotomy with a 5–8 cm skin incision, to reduce surgical stress. However, we performed an esophagectomy through an anterolateral thoracotomy (12–13 cm) after 2001 because we could not adequately dissect the superior mediastinal lymph nodes through the smaller incision.
We principally used a gastric conduit through the retrosternal rout or through the posterior mediastinum to reconstruct the anastomosis with the cervical esophagus. However, in patients with a prior gastrectomy or concomitant gastric cancer, the right ileo-colon was used. The circular stapler was mainly used for securing the anastomosis.
Patients were usually admitted to the intensive care unit (ICU) immediately after the operation. The timing of extubation was determined by the results of blood gas analysis, chest radiography, and bronchoscopy. Patients who were able to breathe spontaneously for approximately 6 h, with a positive end-expiratory pressure (PEEP) of 5 cm H2O and pressure support of 5 cm H2O, were extubated so long as they did not fulfill any of the following weaning failure criteria: (1) respiratory rate greater than 25/min, (2) heart rate greater than 120/min, (3) arterial oxygen saturation less than 95%, (4) an increase in sputum volume, (5) blunting of the cough reflex, or (6) restlessness [15]. All of the patients were provided with intravenous total parenteral nutrition after the operation. Epidural analgesia was used routinely for postoperative pain management for 1 week.
The pathologic classification of the primary tumor, the degree of lymph node involvement, and the presence of organ metastasis were characterized according to the tumor–node–metastases (TNM)/International Union Against Cancer (UICC) classification.
Postoperative complications were defined in the following manner. Pulmonary complications were defined by the presence of bronchopneumonia and aspiration pneumonia as diagnosed by their radiologic, clinical, and microbiological features, as well as the presence of respiratory failure requiring ventilatory support [5]. The ICU staffs, medical specialists of respiratory medicine, and surgical staffs defined and diagnosed pulmonary complications. The diagnosis of these complications was not done in a blinded fashion but was done retrospectively from patient charts. Chylothorax was defined as the presence of a pleural effusion with identification of chylomicrons upon lipoprotein electrophoresis of the effusion or by laboratory determination of an effusion triglyceride level greater than 110 mg/dl [18]. Anastomotic leakage was diagnosed by gastrography and based on the clinical features. The occurrence of hepatic failure was defined as a peak total bilirubin level of greater than 3 mg/dl and/or an elevation of either the aspartate aminotransferase or the alanine aminotransferase level to a value of >200 IU/l (normal range is <40 IU/l at our institute) [15]. The 30-day mortality was defined as death within 30 days of esophageal resection. Any death in the hospital after surgery was recorded as a hospital death.
The independent factors influencing the rate of pulmonary complications were specifically studied with logistic regression analyses. The perioperative factors examined included the patients’ sex, age, the percentage of vital capacity (%VC), the percentage of forced expiratory volume in 1 s (FEV1.0%), the use of respiratory physiotherapy, the administration of corticosteroid medication, the presence of preexistent pulmonary or cardiac disease, and the use of neoadjuvant therapy (chemotherapy, radiation therapy, and chemoradiation therapy). Operative factors included the number of lymph-node fields dissected, the length of the thoracotomy incision, the organ used for esophageal substitution, the rout of the reconstruction, the amount of blood loss experienced, and the duration of the operation. The tumor-specific factors considered were the location of the tumor and the TNM stage of the disease.
The study was divided into three time periods: 1991 to 1995 (period I), 1996 to 2000 (period II), and 2001 to 2005 (period III). The rationale for this division is that the VATS-esophagectomy with a small skin incision (5–8 cm) for the anterolateral thoracotomy approach was performed in period II, and the administration of corticosteroid medication was initiated in period III. The purpose of our study was to examine the effect of these therapeutic measures on the rate of pulmonary complications.
Quantitative results are expressed as the mean ± the standard deviation. Statistical analysis was performed by analysis of variance and Fisher’s test. A univariate and multivariate analysis of the factors influencing the rate of pulmonary complication was performed with logistic regression. p Values of less than 0.05 were considered significant. All statistical analyses were carried out using the StatView program (SAS Institute, Cary, NC, USA).
Results
Table 1 details the clinical characteristics of the patients studied in each of the three time periods. The mean age of patients was 64 years, and the sample was predominantly male (83.7 %, n = 154). The percentage of male patients was higher in period II than in periods I and III (p = 0.02), and the FEV1.0% of patients in period I was significantly lower than in periods II and III (p = 0.01). Eight patients (44.4%) had neoadjuvant therapy in period I (chemotherapy, 1; radiation, 5; chemoradiation, 1). No significant difference in the other clinical characteristics of the patients was noted between the three time periods.
In the surgical procedure performed, obvious differences were present. In period I, we usually used a conventional posterolateral incision. In period II, most patients underwent esophagectomy with lymphadenectomy via an anterolateral thoracotomy with a small skin incision (less than 10 cm), assisted by thoracoscopy (84.4%). Twelve of the patients underwent complete thoracoscopic esophagectomy without any skin incision. In period III, we principally performed an anterolateral thoracotomy using a medium-sized incision (12–13 cm) to allow for thorough dissection of the superior mediastinal lymph nodes. There was a significant difference in the size of the skin incisions utilized between period II and periods I and III (p < 0.0001). A three-field lymph-node dissection was performed in a limited number of cases, although the frequency increased during periods II and III (p < 0.0001). The differences in the surgical procedures performed influenced the duration of surgery in period III (p < 0.0001). There was no significant difference noted in considering either the method of esophageal reconstruction or the operative blood loss between periods I, II, and III.
The postoperative complications and the mortality rates are listed in Table 2. The most common pulmonary complications were pneumonia and atelectasis, occurring in 36 patients (19.6 %); acute respiratory distress syndrome (ARDS) occurred in eight patients. An anastomotic leak occurred in 17 patients (9.2%), and 3 patients experienced permanent recurrent laryngeal nerve palsy (1.6%). The morbidity rate was 42.4 %, and the mortality rate was 3.3 %.
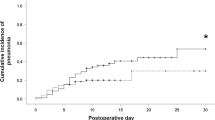
The changes in the rate of pulmonary complications and the morbidity and mortality rates, from 1991 to 2005, are shown in Fig. 1. No significant difference was noted in the incidence of pulmonary complications or in the rates of morbidity and mortality between periods I and II. However, the frequency of pulmonary complications decreased in period III, as did the rates of morbidity and mortality. The incidence of pulmonary complications in period III was significantly lower than in periods I and II (8.0 vs 26.9 and 36.2%; p < 0.05, p < 0.0001), and the morbidity rate in period III was also lower than in periods I and II (29.0 vs 53.8 and 60.3%; p < 0.05, p = 0.0002). Moreover, the mortality rate was lower in period III (2.0%) than in either period I (3.8%) or period II (5.2%).
Change in pulmonary complications, morbidity rates, and mortality rates after an esophagectomy from 1991 to 2005. The changes in pulmonary complications, the morbidity rates, and mortality rates from 1991 to 2005 are shown. The incidence of pulmonary complications in period III was significantly lower than in periods I and II (8.0 vs 26.9 and 36.2%; p < 0.05, p < 0.0001), the morbidity rate in period III was also lower than in periods I and II (29.0 vs 53.8 and 60.3%; p < 0.05, p = 0.0002). Moreover, the mortality rate was lower in period III (2.0%) than in periods I (3.8%) and II (5.2%)
To determine which factors were associated with pulmonary complications, a logistic regression analysis was performed (Table 3). Risk factors for pulmonary complications identified by univariate analysis were as follows: no administration of respiratory physiotherapy, no administration of corticosteroid medication, reduced length of the thoracotomy incision, increased blood-volume loss, and advanced stage of disease (Table 3). These factors were incorporated as independent variables, with pulmonary complications which were considered to be a dependent variable, and an analysis via logistic regression was performed. Factors that were independently associated with an increased risk for pulmonary complications in a multivariate analysis were as follows: no administration of corticosteroids (p = 0.0010), blood loss more than 630 ml (p = 0.0105), and no respiratory physiotherapy (p = 0.0371). A small incision for thoracotomy had no effect on the prevention of pulmonary complications. These p values and odds ratios are shown in Table 4.
Discussion
Pulmonary complications have been reported to be the most common cause of postoperative death [5, 8, 9] and also have a large negative impact on survival after esophagectomy for cancer [19]. We have tried to reduce the incidence of pulmonary complications and to improve the patient morbidity and mortality rates by introducing surgical and medical changes during the past 15 years. As a result, the incidence of pulmonary complications has decreased to 8.0%, and the mortality rate has decreased to 2.0% in the most recent 5 years. Although it is possible that the improved results were partially due to subtle improvements in operative technique, it is very important to review all factors which contribute to the improvement of the surgical outcome.
In the present study, we analyzed the factors affecting the pulmonary complications in 184 patients undergoing esophagectomy and identified the following as independent factors affecting the rate of pulmonary complications: the administration of corticosteroids, blood-loss volume, and respiratory physiotherapy. In recent studies, several factors have been identified as contributing to a decreased incidence of pulmonary complications, including epidural analgesia, bronchoscopy, a decreased history of smoking, decreased surgical blood-volume loss, advanced age, tumor location, and operative duration [5, 8, 9, 20]. In this study, epidural analgesia and bronchoscopy were not included in the analysis because all patients had epidural analgesia and bronchoscopy was not performed prophylacticly.
The administration of corticosteroid medication was identified as a most important contributor to the reduction of pulmonary complications in our patient cohort. Several studies, including one randomized controlled trial, have demonstrated the benefit of preoperative administration of corticosteroid medication in patients undergoing esophagectomy for esophageal cancer [15, 21]. The perioperative administration of a bolus of an active steroid was reported to alleviate surgical stress by decreasing postoperative serum levels of IL-6 [13, 14]. Consideration must also be given to the possibility that perioperative steroid administration may adversely affect the patient’s wound healing and immune response. We based our regimen on the previously reported data that steroid administration had no effect on serum cytokines which were already released but suppressed cytokine production from monocytes and macrophages [22, 23]. Therefore, we administered steroid medication at the start of the thoracotomy and following the completion of the operation. The findings of this study demonstrate that corticosteroid administration could improve the postoperative early condition of the patient undergoing esophagectomy without evoking any adverse effects, these findings being similar to those described in a previous report [21].
The use of respiratory physiotherapy also played an important role in the reduction of pulmonary complications in this study. Several studies have demonstrated that respiratory physiotherapy reduces the incidence of postoperative pulmonary complications after open abdominal surgery [11, 12]. On the other hand, Pasquina et al. [24] have reported that the benefit of respiratory physiotherapy for the prevention of pulmonary complications after cardiac surgery remains unproven. There have been no reports mentioning the importance of perioperative physical therapy administered and supervised by physiatrists and physiotherapists after an esophagectomy. Our results showed that perioperative respiratory physiotherapy and systemic exercises were a preventive factor relative to the occurrence of pulmonary complications. Most patients with esophageal cancer have a history of smoking and often suffer from chronic obstructive pulmonary disease. In addition, radical esophagectomy with upper mediastinal lymph-node dissection may have an adverse effect on the patient’s respiratory function. Therefore, it is important to improve the respiratory function prior to the operation and to actively assist in the recovery of respiratory function as soon after the surgery as is possible. Moreover, we considered that motivation for operation would be advanced by preoperative respiratory physiotherapy.
We evaluated the effects of respiratory physiotherapy using the %VC and the FEV1.0% before and after respiratory physiotherapy. However, they were not improved significantly after respiratory physiotherapy. At present, we have started the prospective clinical study analyzing changes of preoperative maximum oxygen uptake (VO2max) by respiratory physiotherapy to prove improvement of respiratory function.
Recently, Luketich et al. [16] have demonstrated that minimally invasive esophagectomy offered results as good as, or better than, open operation in the areas of mortality, quality of life, and patient survival. Taguchi et al. [17] have shown that thoracoscopic surgery is associated with a better preservation of the pulmonary function, such as vital capacity and performance status, than open surgery, even in cases requiring three-field esophagectomy for esophageal cancer. In the present study, the length of the thoracotomy incision was not a significant factor in the prevention of pulmonary complications, as determined by multivariate analyses. This may result from the fact that the anterolateral thoracotomy performed in our present surgical procedure, with an incisional length of 13–15 cm, can preserve the serratus anterior muscle and the latissimus dorsi muscle. In addition, the bronchial artery and the bronchial branches of the vagus nerve are usually preserved in the upper mediastinal lymphadenectomy, resulting in preservation of the physiological tolerance to surgical stress [25].
The volume of the blood loss was found to be an independent factor affecting the pulmonary complication rate. A decreased blood loss has been reported to be associated with a decreased hospital death rate, as well as long-term survival after major surgery, such as a hepatectomy [26]. Increased intraoperative blood loss has been shown to be associated with an increased incidence of pulmonary complications and hospital death after an esophagectomy [8]. These findings imply that the surgeon can reduce the risk of pulmonary complications by refining and improving his surgical technique for resection. Obviously, the surgeon should make every effort to reduce blood loss during the operation.
Some Japanese groups have reported that a three-field dissection improved a long-term survival and was the same as a two-field dissection in the mortality rates, postoperative course, and quality of life in patients with cancer of the thoracic esophagus [20, 27–29]. In this study, the number of lymph node fields dissected and the duration of the operation had no influence on the rate of pulmonary complication. We therefore conclude that patients with thoracic esophageal cancer can undergo a three-field dissection in comparative safety with the perioperative administration of corticosteroid medication and with sufficient respiratory physiotherapy in the perioperative period.
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- ICU:
-
Intensive Care Unit
- OR:
-
odds ratio
- CI:
-
confidence interval
References
Earlam R, Cunha-Melo JR (1980) Oesophageal squamous cell carcinoma: 1. A critical review of surgery.. Br J Surg 67:381–390
Muller JM, Erasmi H, Stelzner M, Zieren U, Pichlmaier H (1990) Surgical therapy of oesophageal carcinoma. Br J Surg 77:845–857
Swisher SG, Hunt KK, Holmes EC, Zinner MJ, McFadden DW (1995) Changes in the surgical management of esophageal cancer from 1970 to 1993. Am J Surg 169:609–614
Kakegawa T (2003) Forty years’ experience in surgical treatment for esophageal cancer. Int J Clin Oncol 8:277–288
Whooley BP, Law S, Murthy SC, Alexandrou A, Wong J (2001) Analysis of reduced death and complication rates after esophageal resection. Ann Surg 233:338–344
Walsh TN, Noonan N, Hollywood D, Kelly A, Keeling N, Hennessy TP (1996) A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335:462–467
Bailey SH, Bull DA, Harpole DH, Rentz JJ, Neumayer LA, Pappas TN, Daley J, Henderson WG, Krasnicka B, Khuri SF (2003) Outcome after esophagectomy: a ten-year prospective cohort. Ann Thorac Surg 75:217–222
Law S, Wong KH, Kwok KF, Chu KM, Wong J (2004) Predictive factors for postoperative pulmonary complications and mortality after esophagectomy for cancer. Ann Surg 240:791–800
Fang W, Kato H, Tachimori Y, Igaki H, Sato H, Daiko H (2003) Analysis of pulmonary complications after tree-field lymph node dissection for esophageal cancer. Ann Thorac Surg 76:903–908
Fok M, Law SYK, Wong J (1994) Operable esophageal carcinoma: current results from Hong Kong. World J Surg 18:355–360
Hall JC, Tarala RA, Tapper J, Hall JL (1996) Prevention of respiratory complications after abdominal surgery: randomized clinical trial. BMJ 312:148–152
Fagevik Olsen M, Hahn I, Nordgren S, Lonroth H, Lundholm K (1997) Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg 84:1535–1538
Shimada M, Saitoh A, Kano T, Takenaka K, Sugimachi K (1996) The effect of a perioperative steroid pulse on surgical stress in hepatic resection. Int Surg 81:49–51
Matsutani T, Onda M, Sasajima K, Miyashita M (1998) Glucocorticoid attenuates a decrease of antithrombin III following major surgery. J Surg Res 79:158–163
Sato N, Koeda K, Ikeda K, Kimura Y, Aoki K, Iwaya T, Akiyama Y, Ishida K, Saito K, Endo S (2002) Randomized study of the benefits of preoperative corticosteroid administration on the postoperative morbidity and cytokine response in patients undergoing surgery for esophageal cancer. Ann Surg 236:184–190
Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR, Schauer PR, Close JM, Fernando HC (2003) Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 238:486–495
Taguchi S, Osugi H, Higashino M, Tokuhara T, Takada N, Takemura M, Lee S, Kinoshita H (2003) Comparison of three-field esophagectomy for esophageal cancer incorporating open or thoracoscopic thoracotomy. Surg Endosc 17:1445–1450
Avendano CE, Flume PA, Silvestri GA, King LB, Reed CE (2002) Pulmonary complications after esophagectomy. Ann Thorac Surg 73:922–926
Rizk NP, Bach PB, Schrag D, Bains MS, Turnbull AD, Karpeh M, Brennan MF, Rusch VW (2004) The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg 198:42–50
Fujita H, Kakegawa T, Yamana H, Shima I, Toh Y, Tomita Y, Fujii T, Yamasaki K, Higaki K, Noake T, Ishibashi N, Mizutani K (1995) Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 222:654–662
Shimada H, Ochiai T, Okazumi S, Matsubara H, Nabeya Y, Miyazawa Y, Arima M, Funami Y, Hayashi H, Takeda A, Gunji Y, Suzuki T, Kobayashi S (2000) Clinical benefits of steroid therapy on surgical stress in patients with esophageal cancer. Surgery 128:791–798
Kohase M, Henriksen-Destefano D, Sehgal PB, Vilcek J (1987) Dexamethasone inhibits feedback regulation of the mitogenic activity of tumor necrosis factor, interleukin-1, and epidermal growth factor in human fibroblasts. J Cell Physiol 132:271–278
Sironi M, Gadina M, Kankova M, Riganti F, Mantovani A, Zandalasini M, Ghezzi P (1992) Differential sensitivity of in vivo TNF and IL-6 production to modulation by anti-inflammatory drugs in mice. Int J Immunopharmac 14:1045–1050
Pasquina P, Tramer MR, Walder B (2003) Prophylactic respiratory physiotherapy after cardiac surgery: systematic review. BMJ 327:1379–1384
Fujita H, Hawahara H, Yamana H, Shirohazu G, Yoshimura Y, Minami T, Negoto Y, Irie H, Shima I, Machi J, Kakegawa T (1988) Mediastinal lymph node dissection procedure during esophageal cancer operation—carefully considered for preserving respiratory function. Jpn J Surg 18:31–34
Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J (1999) Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg 229:322–330
Akiyama H, Tsurumaru M, Udagawa H, Kajiyama Y (1994) Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 220:364–373
Isono K, Sato H, Nakayama K (1991) Results of a nationwide study on the three-field lymph node dissection of esophageal cancer. Oncology 48:411–420
Kato H, Watanabe H, Tachimori Y, Iizuka T (1991) Evaluation of neck lymph node dissection for thoracic esophageal carcinoma. Ann Thorac Surg 51:931–935
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakamura, M., Iwahashi, M., Nakamori, M. et al. An analysis of the factors contributing to a reduction in the incidence of pulmonary complications following an esophagectomy for esophageal cancer. Langenbecks Arch Surg 393, 127–133 (2008). https://doi.org/10.1007/s00423-007-0253-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-007-0253-7