Abstract
Background and aims
Despite the overall excellent prognosis for patients with thyroid papillary microcarcinoma (PMC), these tumors are associated with lymph node metastasis. The aim of this study is to identify the rate of lymph node metastasis and evaluate the clinical and pathological factors affecting metastasis in thyroid PMC.
Methods
Among 475 patients with papillary thyroid carcinoma treated between 1990 and 2003, 81 patients (17%) were diagnosed as PMC and the records of these patients were evaluated retrospectively. Clinicopathologic features were evaluated by univariate and multivariate analyses.
Results
According to age, metastases, extent, and size risk definition, all patients were in low-risk group. Lymph node metastases were determined in 12.3% of patients. Mean follow-up was 7 years (range from 28 to 192 months). Ten-year disease-free and overall survival rates were 97 and 100%, respectively. Both multifocality and thyroid capsular invasion were found to be independent risk factors for lymph node metastasis by multivariate analysis.
Conclusion
Patients with thyroid PMC in low-risk group with multifocal tumors and with capsule invasion may have increased risk of lymph node metastasis, and must be considered in follow-up of the patients who have these factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to World Health Organization classification, thyroid papillary microcarcinoma (PMC) is defined as tumors smaller than 1 cm in diameter [1]. Most of these tumors are nonpalpable and cannot be identified clinically. In the past, most of the PMCs were determined in thyroidectomy specimens because of benign pathologies or in autopsies of patients died because of nonthyroid causes incidentally. However, recently, with ultrasonography-guided fine needle aspiration biopsy, the number of patients diagnosed and treated increased significantly [2]. It has been reported that PMC incidence is as high as 35% in autopsy series; it is probable that the behavior of these tumors are mostly benign [3–7]. The mortality rate of PMC is reported as 0–1% in the literature [8–11]. Locoregional recurrence or distant metastasis can be seen in only a very small number of patients. One study reported a long-term recurrence rate of 6% at 20 years [12].
Although considered as a benign disease, PMC can have a different biological behavior occasionally. While the tumor cannot be identified in the thyroid clinically, palpable lymph node metastasis may be found in a subgroup of patients. Nodal involvement rate is lower in PMC compared to tumors larger than 1 cm. It has been reported that lymph node metastasis were detected in 3.1–18.2% of patients [6, 13]. Lymph node metastasis at diagnosis is a predictive factor for locoregional recurrence and distant metastasis [11]. There are limited studies evaluating the relationship of lymph node metastasis and other risk factors in PMC. The aim of this study is to determine the nodal invasion rates in PMC as well as clinical and pathological factors affecting lymph node metastasis.
Materials and methods
Among 475 patients with papillary thyroid cancer (PTC) treated in Ankara Oncology Training and Research Hospital between 1990 and 2003, 81 patients (17%) were diagnosed as PMC and the records of these patients were evaluated retrospectively. According to age, metastases, extent, and size risk definition, all patients were in low-risk group. The diagnosis of PMC was made incidentally in all patients who had been operated for other benign thyroid pathologies. Five of the patients were operated for toxic goiter, 45 patients for multinodular goiter, 25 patients for solitary nodule, and 6 patients for cystic nodule. Twelve of the patients had palpable cervical lymph node in addition to their thyroid pathologies.
The operative procedures performed on these patients are presented on Table 1. Of the 81 PMC patients, 64 had total and 17 had subtotal thyroidectomy. Among 64 patients who had total thyroidectomy, 54 had subtotal resection on the side with tumor and contralateral subtotal lobectomy in other centers previously. None of patients had frozen section examination because the diagnosis of PMC was made incidentally in all patients who had been operated for other benign thyroid pathologies. After confirmation of microcarcinoma histopathologically, these patients had completion thyroidectomy approximately 6 weeks after the first operation because of incomplete surgical resection, multifocality on the same lobe, suspicious multifocality on residual thyroid tissue with ultrasonography, or having palpable lymph nodes in the neck. Moreover, 10 patients who had their first operation in our hospital had complementary thyroidectomy because of similar reasons. Of 17 PMC patients who had subtotal thyroidectomy, 15 had ipsilateral lobectomy and contralateral partial lobectomy, and 2 had ipsilateral lobectomy and isthmusectomy. Ipsilateral modified radical neck dissection was performed in 12 patients who had their first operation in other centers and referred to our hospital with palpable cervical lymph nodes. Central compartment neck dissection was not performed in any patients because no macroscopic lymph nodes were found in this region in preoperative and intraoperative examination. Pathological evaluation was performed according to classification system recommended by the World Health Organization [1].
All patients also had total body scan with 131I scintigraphy for diagnostic purposes to identify if any thyroid tissue remained or to determine possible metastatic deposits. Thirty patients who had risk factors such as multifocality, thyroid capsular invasion, vascular invasion, bilaterality, age >40 years, microscopic lymph node metastasis, and follicular variant had radioactive iodine (RAI) treatment at ablative doses of 100–150 mCi. All patients had suppression with l-thyroxin to keep thyroid-stimulating hormone (TSH) levels at about 0.1 Ul/dl. Patients were followed-up at 3, 6, and 12 months after treatment, and then on a yearly basis. Postoperative follow-up consisted of clinical evaluation and measurement of serum thyroglobulin levels. Patients with suspicious lymph nodes in the neck were evaluated by cervical ultrasonography. Other imaging techniques, such as chest X-rays, computed tomography scan, and 131I scintigraphy, were performed when appropriate. During the follow-up period, 12 patients had RAI treatment because of high serum thyroglobulin levels, although no tumor focus was identified by 131I scanning scintigraphy.
Results are expressed as mean±SD. The effects of age at diagnosis, gender, histological type, tumor size, multifocality, bilaterality, thyroid capsular invasion, and vascular invasion on lymph node metastasis were evaluated by univariate and multivariate analysis. Survival rates were computed by Kaplan–Meier method. Fisher’s exact test was used for univariate analysis to determine clinical and pathological variables affecting lymph node metastasis. Logistic regression test was used for multivariate analysis of factors found to be significant by univariate analysis. P value <0.05 was considered statistically significant by two-tailed testing. Statistical analysis of the data was performed by using the program Statistical Package for the Social Sciences, version 10.0 for Windows (SPSS, Chicago, IL, USA).
Results
Clinical and pathological characteristics of patients are presented in Table 2. Total number of patients was 81 (66 females and 15 males) and the mean age was 37 ± 10 years (range from 16 to 61). Mean follow-up was 83 ± 43 months (range from 28 to 192). No mortality was recorded during the follow-up period. Ten-year disease-free and overall survival rates were 97 and 100%, respectively. No distant metastasis was determined during the follow-up period. Only one patient had ipsilateral cervical nodal recurrence 68 months later (1.2%). Total thyroidectomy was performed for this patient who had multifocal disease, without thyroid capsular invasion, and tumor size was larger than 5 mm and had no lymph node dissection during the initial surgical treatment. Radical neck dissection was performed on the site with nodal recurrence and the patient is still being followed up for 13 years without any recurrence. Of the patients, 79% had total and 21% had subtotal thyroidectomy. Thirty patients who had risk factors had postoperative RAI treatment for ablation. Histologically 66 (81.5%) patients had papillary cancer while 15 (18.5%) had follicular variant of papillary cancer. Mean tumor diameter was 0.6 ± 0.2 cm. When the patients were analyzed according to tumor size, 27% had tumors ≤5 mm and 73% had >5 mm. The median age of the patients with tumors ≤5 mm was 32 years, in contrast to those tumors >5 mm where the median age was 42 years. Multifocality, thyroid capsular invasion, and lymph node metastasis were seen more frequently in patients with tumors >5 mm; however, this did not reach a statistically significant level (P > 0.05). Pathological tumor size in a patient who had nodal recurrence was 0.8 cm.
Tumor was multifocal in 9 patients (11.1%). Thyroid capsular invasion was determined in 8 patients (9.9%). Ipsilateral modified radical neck dissection was performed in 12 patients because of palpable cervical lymph nodes and in 10 of these patients histopathological nodal involvement was defined (12.3%). The localization of the lymph nodes in patients with lymph node metastasis were N1b (unilateral cervical lymph nodes).
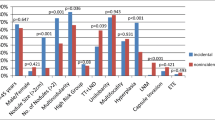
Age, gender, tumor size, histological type of the tumor, bilaterality, and vascular invasion were found to be not effective on lymph node metastasis by univariate analysis (P > 0.05, Table 3). However, multifocality of the tumor was found to be one of the factors significantly increasing the risk of metastasis (P = 0.001). Similarly, thyroid capsular invasion was another factor that significantly affect lymph node metastasis (P = 0.007). Both multifocality [P = 0.004, hazard ratio (HR) 5.5, 95% confidence interval (CI) 1.2–12.4] and thyroid capsular invasion (P = 0.03, HR 2.8, 95% CI, 1.3–6.2) were found to be independent risk factors for cervical lymph node metastasis by logistic regression analysis (Table 4).
Discussion
Most of the thyroid microcarcinomas are diagnosed as papillary type by histopathological evaluation [14, 15]. The frequency of PMC, a specific subgroup of PTCs, has increased parallel to the developments in imaging techniques and improved accuracy of cytopathological evaluation. This retrospective study, covering approximately 13-year period, determined the incidence of PMC to be 17% among the patients treated with the diagnosis of PTC. In autopsy studies, according to geographic differences incidence of small PTC varies from 1.0 to 35.6% [6, 13, 14].
The mortality rates of PMC is reported to be 0–1% [8–11]. In this study, no mortality was seen during the mean 7-year follow-up period and 10-year overall survival rate was 100%. It has been reported that the rate for local recurrence in the tumor bed was 2.5%, for lymph node recurrence 1–5%, and for distant metastasis 1–2.5% [11, 16]. In the presented study only one lymph node recurrence was seen and there was no distant metastasis. This good prognosis may be explained by low-risk factors of the patients, indolent biological behavior of the disease, and tendency to prefer lobectomy or total thyroidectomy as curative surgical treatment. The alternatives for the management of PMC is still controversial. No prospective clinical trials have been performed to determine the ideal treatment for PMC. The choice for treatment may differ from follow-up without surgery to total thyroidectomy with or without RAI treatment. Ito et al. [17] reported that PMC patients without poor prognostic factors may be observed without surgery. Despite patients with PMC have favorable long-term prognosis, recurrences in the neck and distant metastases have been reported. Allo et al. [18] specified that prognosis in PMC is generally excellent, but several patients have rapidly fatal disease. Chow et al. [11] have reported that despite the overall excellent prognosis for patients with PMC, the treatment of patients with PMC should be no different from the treatment of patients with conventional PTC. In the presented series, although all patients were in low-risk group, some of those had risk factors such as multifocality and/or thyroid capsular invasion. And also most of patients who underwent complementary thyroidectomy had only subtotal resection on the side with tumor and contralateral subtotal lobectomy as initial procedure in other centers. Furthermore, several of those had suspicious nodules on residual thyroid tissue ultrasonographically, or palpable lymph nodes in the neck. We preferred observation for patients who had unifocal tumor with no thyroid capsular invasion and in whom ultrasonography showed normal residual thyroid tissue and who had at least ipsilateral total lobectomy and isthmusectomy. Prophylactic ipsilateral lymph node dissection for PTCs >1 cm is performed in some centers from Japan, whereas centers from North America and Europe only perform therapeutic lymph node dissection. In general, lymph node dissection in the presence of clinically palpable lymph nodes is performed for PMC. Wada et al. [19] reported that prophylactic node dissection is not beneficial in PMC patients without lymphadenopathy. We also prefer lymph node dissection for only patients with palpable lymph nodes. In this study, 12 patients had lymph node dissection for palpable lymph nodes and histopathologically 10 showed laterocervical lymph node metastasis. A recent study demonstrated that, in contrast to lateral node metastasis, metastasis in the central compartment does not influence the disease-free survival of PMC patients [20]. In this series, central compartment neck dissection was not performed in any patients because no macroscopic lymph nodes were found in this region in preoperative and intraoperative examination. The rate of lymph node metastasis for the whole series is 12.3%, which is similar to those reported in the literature.
Long-term cohort studies by Mazzafferi and Jhiang [21] and DeGroot et al. [22] demonstrated that postoperative RAI therapy reduces recurrence and provides a small improvement in survival, even in low-risk patients. In our study, 30 patients who had risk factors had RAI treatment at ablative doses. TSH suppression reduces tumor recurrence rates, especially in young patients in papillary and follicular thyroid cancer. In this series, thyroxine was administered to ensure that the patients remained euthyroid, with circulating TSH levels at about 0.1 UI/dl.
Some reports showed that advanced age is a poor prognostic factor for well-differentiated thyroid carcinoma [23, 24]. However, in a further study, there was found no effect of age on aggressiveness and metastasis of PMC [11]. In the presented study the mean age was higher in patients with lymph node metastasis, but this was not statistically significant. In this retrospective series male–female distribution of PMC was 1:4.4, a ratio similar with previous studies [16, 25]. Although a study indicated that gender is a prognostic factor in the high-risk group of patients with PMC [23], others showed contrary results [11, 26]. In our report gender was not an effective predictor for lymph node metastasis.
In a study by Kasai et al. [27] evaluating 78 patients with PMC, the patients were grouped according to tumor size as ≤5 mm and >5 mm, lymph node metastasis was reported to be significantly increased in patients with tumor diameters >5 mm. Another study reported that lateral lymph node metastasis is significantly increased in patients with tumor size ≥7 mm [17]. However, there is also report suggesting that tumor size is not a factor affecting lymph node metastasis [19]. In our study, of the ten patients with lymph node metastasis, tumor size was >5 mm in 8 and ≤5 mm in 2, but the effect of tumor size on lymph node metastasis did not reach a significant level. Similarly, the histopathological subtype of the tumor, bilaterality, and vascular invasion were also not found to be factors increasing the risk of nodal involvement. Multifocality and thyroid capsular invasion were determined as predictive factors increasing lymph node metastasis in this cohort.
The multifocal location of the tumor in PMC is reported to be a risk factor both for lymph node metastasis and local recurrence [4, 8, 11, 17, 19]. In this study, lymph node metastasis was determined in five of the nine patients with multifocal tumors, and multifocality was determined as an independent risk factor. It has been reported that thyroid capsular invasion increases recurrence rates and is one of the poor prognostic factors [8, 12]. Although thyroid capsular invasion is generally reported to be a poor prognostic factor in these studies, its effects on lymph node metastasis were not evaluated in detail. Pelizzo et al. [25] reported the rate of thyroid capsular invasion as little as 0.02%. In this series, this rate was 9.9%, and of the eight patients with thyroid capsular invasion, 4 had lymph node metastasis and thyroid capsular invasion was found to be another independent risk factor significantly increasing lymph node metastasis.
Conclusion
Seventeen percent of patients with PTC were PMC and 12.3% of these patients had lymph node metastasis. According to the results of this study, multifocal location of the tumor and thyroid capsular invasion were found to be risk factors affecting cervical lymph node metastasis, and must be considered in follow-up of the patients who have these factors.
References
Hedinger C, Williams ED, Sobin LH (1988) Histological typing of thyroid tumors, vol. 11. Springer, Berlin Heidelberg New York
Ito Y, Takasaki U, Nakano K (2003) An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 13:381–387
Sampson RJ, Key CR, Buncher CR, Iijima S (1969) Thyroid carcinoma in Hiroshima and Nagasaki: prevalence of thyroid carcinoma at autopsy. JAMA 209:65–70
Sampson RJ, Oka H, Key CR, Buncher CR, Iijima S (1970) Metastases from occult thyroid carcinoma: an autopsy study from Hiroshima and Nagasaki, Japan. Cancer 25:803–811
Fukunaga FH, Yatani R (1975) Geographic pathology of occult thyroid carcinomas. Cancer 36:1095–1099
Harach HR, Franssila KO, Wasenius VM (1985) Occult papillary carcinoma of the thyroid: a “normal” finding in Finland. A systematic autopsy study. Cancer 56:531–538
Lang W, Borrusch H, Bauer L (1988) Occult carcinomas of the thyroid. Evaluation of 1,020 sequential autopsies. Am J Clin Pathol 90:72–76
Baudin E, Travagli JP, Ropers J, Mancusi F, Bruno-Bossio G, Caillou B, Cailleux AF, Lumbroso JD, Parmentier C, Schlumberger M (1998) Microcarcinoma of the thyroid gland: the Gustave–Roussy Institute experience. Cancer 83:553–559
Appetecchia M, Scarcello G, Pucci E, Procaccini A (2002) Outcome after treatment of papillary thyroid microcarcinoma. J Exp Clin Cancer Res 21:159–164
Furlan JC, Bedard Y, Rosen IB (2001) Biologic basis for the treatment of microscopic, occult well-differentiated thyroid cancer. Surgery 130:1050–1054
Chow SM, Law SCK, Chan JKC, Au SK, Yau S, Lau WH (2003) Papillary microcarcinoma of the thyroid: prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Hay ID, Grant CS, van Heerden JA, Goellner JR, Ebersold JR, Bergstralh EJ (1992) Papillry thyroid microcarcinoma: a study of 535 cases observed in a 50-year period. Surgery 112:1139–1147
Bramley MD, Harrison BJ (1996) Papillary microcarcinoma of the thyroid gland. Br J Surg 83:1674–1683
Bisi H, Fernandes VS, de Camargo RY, Koch L, Abdo AH, de Brito T (1989) The prevalence of unsuspected thyroid pathology in 300 sequential autopsies, with special reference to the incidental carcinoma. Cancer 64:1888–1893
Fink A, Tomlinson G, Freeman JL, Rosen IB, Asa SL (1996) Occult micropapillary carcinoma associated with benign folliculary thyroid disease and unrelated thyroid neoplasms. Mod Pathol 9:816–820
Orsenigo E, Beretta E, Fiacco E, Scaltrini F, Veronesi P, Invernizzi L, Gini P, Fiorina P, Di Carlo V (2004) Management of papillary microcarcinoma of the thyroid gland. Eur J Surg Oncol 30:1104–1106
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi A, Matsuzuka F, Kuma K, Miyauchi A (2004) Papillary microcarcinoma of the thyroid: how should it be treated? World J Surg 28:1115–1121
Allo M, Christianson W, Koivunen D (1988) Not all ‘occult’ papillary carcinomas are ‘minimal’. Surgery 104:971–976
Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T, Ito K, Takami H, Takanashi Y (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas. Frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 3:399–407
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K, Miyauchi A (2006) Clinical significance of metastasis to the central compartment from papillary microcarcinoma of the thyroid. World J Surg 30:91–99
Mazzafferi EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418
DeGroot LJ, Kaplan EL, McCormick M, Straus FH (1990) Natural history, treatment and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 71:414–424
Lin JD, Chen ST, Chao TC, Hsueh C, Weng HF (2005) Diagnosis and therapeutic strategy for papillary thyroid microcarcinoma. Arch Surg 140:940–945
Sugino K, Ito K Jr, Ozaki O, Mimura T, Iwasaki H, Ito K (1998) Papillary microcarcinoma of the thyroid. J Endocrinol Invest 21:445–448
Pelizzo MR, Boschin IM, Toniato A, Pagetta C, Piotto A, Bernante P, Casara D, Pennelli G, Rubello D (2004) Natural history, diagnosis, treatment and outcome of papillary thyroid microcarcinoma (PTMC): a mono-institutional 12-year experience. Nucl Med Commun 25:547–552
Schindler AM, van Melle G, Evequoz B, Scazziga B (1991) Prognostic factors in papillary carcinoma of the thyroid. Cancer 68:324–330
Kasai N, Sakamoto A (1987) New subgrouping of small thyroid carcinomas. Cancer 60:1767–1770
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gülben, K., Berberoğlu, U., Çelen, O. et al. Incidental papillary microcarcinoma of the thyroid—factors affecting lymph node metastasis. Langenbecks Arch Surg 393, 25–29 (2008). https://doi.org/10.1007/s00423-007-0213-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-007-0213-2