Abstract
Background
Angiogenesis can be enhanced by several growth factors, like vascular endothelial growth factor-165 (VEGF165) and basic fibroblast growth factor (bFGF). Delayed release of such growth factors could be provided by incorporation of growth factors in fibrin matrices. In this study, we present a slow release system for VEGF165 and bFGF in fibrin sealant.
Materials and methods
In vitro: Pieces of Integra™ matrix of 15 mm in diameter were prepared. Integra™ matrices were divided into four groups (A=control; B=fibrin sealant; C=fibrin sealant+growth factors; D=growth factors). In vivo: The bioartificial dermal templates were transplanted into a full-skin defect of the back of nu–nu mice. Four different groups included each six matrices at 2 and 4 weeks.
Results
In vitro: In groups C and D, continuous release of VEGF165 and bFGF was eminent. The incorporation of growth factors into fibrin sealant evoked a prolonged growth factor release (p < 0.05). In vivo: A significantly higher amount of vessels was quantified in groups C and D compared to groups A and B (p < 0.001).
Conclusions
A model of slow protein release by combining VEGF165 and bFGF with fibrin sealant was produced. This model resulted in a prolonged bioavailability of growth factors in vivo for functional purposes. Fibrin and collagen can release growth factors in vivo and induce significant and faster neovascularisation in bioartificial dermal templates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
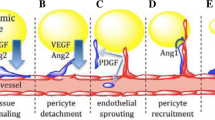
In angiogenesis, vascular cells proliferate and form new capillary structures [1]. Ischaemia causes the release of endogenous biochemical agents, which include growth factors to stimulate angiogenesis [2–4]. All these processes are important in reconstructive strategies using dermal regeneration templates.
In contrast to full thickness skin, bioartificial skin is lacking an original vascular network. This fact has been identified as the main reason for clinical failures due to matrix infection and loss of structural components [5]. The problem can be targeted by creating vascular matrix structures in vitro or inducing angiogenesis in vivo. Angiogenesis can be enhanced by several growth factors as vascular endothelial growth factor-165 (VEGF165) and basic fibroblast growth factor (bFGF). The disadvantage of protein-based therapy is quick protein degradation in vivo, while a prolonged effect is needed to induce stable capillary structures. A delayed release of proteins could be provided by incorporation of growth factors or other substances in slowly degrading fibrin matrices.
In this work, we present a slow release system for VEGF165 and bFGF in fibrin sealant. After studying substance release in vitro, we used the assay in an in vivo model to study whether delayed protein release could induce therapeutic effects.
Materials and methods
Integra™ dermal regeneration template
Integra™ dermal regeneration template (Integra Life Sciences, Plainsboro, NJ) is a bilayered membrane system consisting of a silicone top layer that temporarily replaces the epidermal part of the skin. This layer is meant to retend moisture loss and close the wound bed. A second layer is made of collagen type I and chondroitin-6-sulphate, representing the permanent dermal part [6, 7] (Fig. 1a,b). After harvesting the tissue, the silicone layer was removed to perform quantification of the newly formed blood vessels in the target tissue.
The growth factors VEGF165 and bFGF
Recombinant human VEGF165 was purchased from R&D Systems (Minneapolis, MN, USA). Its source is a DNA sequence encoding the 165 amino acid residue variant of human VEGF that was expressed in Sf 21 insect cells using a baculovirus expression system. The recombinant disulfide-linked homodimeric human VEGF is glycosylated and migrates as a 19–21 kDa protein in sodium dodecyl sulphate-polyacrylamide gel electrophoresis under reducing conditions [8].
Recombinant human bFGF was also purchased from R&D Systems. Its source is a DNA sequence corresponding to the mature human bFGF that was expressed in Escherichia coli. The 157 amino acid residue recombinant protein has a molecular mass of 17.4 kDa [9].
Fibrin sealant
Fibrin sealant (Tissucol™, Baxter AG, Wien) consists of two human plasma-derived components: (a) a highly concentrated fibrinogen complex composed primarily of fibrinogen and fibronectin along with catalytic amounts of factor XIII and plasminogen and (b) a high potency thrombin. Fibrin sealant clots of varying composition were prepared by mixing diluted solutions of these components. The growth factors were injected into the fibrinogen complex solution before clot formation.
Preparation of fibrin sealant with VEGF165 and bFGF into a matrix
To determine the release of growth factors, pieces of Integra™ matrix of 15 mm in diameter were prepared (Fig. 1a,b).
Integra™ matrices were divided into four groups A–D (Table 1). In group A, the Integra™ matrices were stored in 1,000-μl phosphate-buffered saline (PBS) solution (control). The matrices of group B were impregnated with fibrin sealant solution (once [12 μl], Ersta [12 μl]) Tisseel™ VH (Baxter AG, Vienna, Austria) mixed with PBS solution (12 μl). In group C, a combination of fibrin sealant, VEGF165 and bFGF was used [(growth factors [VEGF165 (1 μg)+bFGF (0.5 μg)]+fibrin sealant (once [12 μl], Ersta [12 μl]). Group D incorporated only growth factors (VEGF165 [1 μg]+bFGF [0.5 μg 1 μg])+288-μl PBS solution; see Table 1 for general overview]. All matrices were stored in 1,000-μl PBS solution and kept in a 24-well plate.
Measurements of growth factor release
In the in vitro experiment, three medium samples of each group were taken at 13 definite time points. One thousand microlitres of PBS were harvested and replaced by 1,000-μl PBS solution every 24 h for 13 days. The collected PBS samples were kept at −80°C and analysed later by using bFGF- and VEGF165-specific enzyme-linked immunosorbent assay (ELISA) kits (Quantikine immunoassay kit nos. DFB 50 and DVE 00, R&D Systems) according to the manufacturer’s instructions. Measurements were performed once for VEGF165 and for bFGF. The ELISA samples were read, and the absorbance was measured in a microplate ELISA reader (Sunrise™ absorbance Reader, Tecan Trading AG, Switzerland) at 450 nm.
Animal model
All procedures were performed with approval of the Institutional Animal Care and Use Committee as well as the University Ethical Committee. nu–nu/mice (weight 18–20 g) served for all experiments using Integra™ matrix as bioartificial dermal templates. All animals were anaesthetised with ketamine (Ketamin 10%®, Pfizer; Karlsruhe, Germany, 0.0108 μg per gram of bodyweight) and xylazine (Rompun®, Bayer; Leverkusen, Germany, 0.0024 μg per gram of bodyweight) via intraperitoneal injection. A full skin defect 15 mm in diameter was created at anatomically identical sites on the right and left side of the back in each mouse. Twelve animals were operated (three per group) with two matrices each; all matrices were processed as described and divided into four groups A–D: (A) Control (500 μl PBS), (B) PBS solution (12 μl)+fibrin sealant (once [12 μl], Ersta [12 μl]), (C) growth factors (VEGF165 [1 μg]+bFGF [0.5 μg])+fibrin sealant ([once [12 μl], Ersta [12 μl]), (D) growth factors (VEGF165 [1 μg]+bFGF [0.5 μg])+288 μl PBS solution. Immediately after preparation, matrices were transplanted into the full skin defects of nu/nu mice (Fig. 2a). After 2 weeks (experiment 1), the animals were killed and the target tissue analysed. In a second set of in vivo experiments (experiment 2), 12 animals (3 animals per group) were used and evenly divided into four groups as described above. Animals were killed 4 weeks after matrix transplantation (Fig. 2b).
Clinical evaluation
All matrix areas were monitored daily for autocannibalism or matrix loss due to infection or other reasons. Photodocumentation of matrix areas was performed in a standard fashion before animal scarification.
Blood vessel quantification
To quantify blood vessel growth into the matrices, the target tissue was harvested and placed upside down on a petri dish. The silicon layer and the sutures were removed, and the inside of the target tissue was turned up. The dish containing the tissue was put on a transilluminator (Fig. 3a), and a picture in tagged image file format (TIFF) quality was taken and segmented (Fig. 3b,c). The amount of newly formed blood vessels in the target tissue was quantified by a VesSeg programme as described before [10]. Briefly, in this programme, vessels are recognised as longitudinal structures. A black and white image is created in which vessels are indicated as white pixels (Fig. 3c). The total area of white pixels reflects the area of blood vessels that allows calculation of the area of blood vessels in the target area (matrix) and in the control area (surrounding tissue). A ratio in between both was formed.
Histology
Cross sections of four matrices of each group from both experiments were analysed. Immunohistochemical cluster of differentiation-31 (CD31) and haematoxylin/eosin staining was performed. Immunohistochemical CD31 staining was done using a standard three-step immunoperoxidase technique and diaminobenzidine as chromogen. Briefly, 5 μm thick paraffin sections were pre-treated for 45 min in a decloaker (in PBS buffer, pH 9.5) and then incubated for 25 min with the primary polyclonal goat antibody platelet endothelial cell adhesion molecule-1 (dilution 1:60; clone M-20; Santa Cruz, CA, USA), followed by incubation with the secondary antibody (biotin-SP-conjugated mouse anti-goat immunoglobulin G; Dianova, Hamburg, Germany; dilution 1:50). Next, the slides were incubated for 15 min with horse-raddish peroxidase (Dako, Glostrup, Denmark). After another incubation for 10 min with DAB (Dako), the slides were counterstained with Meyer’s haematoxilin (Merck, Darmstadt, Germany).
Statistical analysis
All data obtained from in vitro experiments (protein concentrations ng/ml) and in vivo experiments (newly formed blood vessels in percentage) were normally distributed and evaluated for statistical significance by the Student’s t-test. The level of significance in the in vitro experiments was p < 0.05, in the in vivo experiments (p < 0.05 and p < 0.001).
Results
Release of growth factors in vitro
At the first measurement of the growth factor concentration after 24 h, 9.7 and 6.6% of the initially administered amount of VEGF165 were detected in the medium in groups C and D, respectively (97.21 ± 13.45 and 66.37 ± 10.25 ng/ml). The corresponding values for bFGF were 1.7 and 0.19% (8.53 ± 0.25 and 0.96 ± 0.21 ng/ml). In groups A and B, we detected no proteins.
In groups C and D, we detected a continuous release of VEGF165 and bFGF over 13 days, but amounts rapidly declined (Fig. 4a,b). After 48 h, VEGF165 concentration already diminished to 48.71 ± 8.12 and 31.59 ± 4.51 ng/ml in groups C and D with corresponding values for bFGF of 0.98 ± 0.23 and 0.33 ± 0.07 ng/ml. VEGF165 almost levelled zero after 9 days in group C and 4 days in group D. bFGF concentration dropped below 0.05 ng/ml after 10 days in group C and 6 days in group D.
Release of bFGF (a) and VEGF165 (b) in vitro. In groups C and D, we detected a continuous release of VEGF165 and bFGF. At days 1 to 12, there was a significant difference in protein release between groups C and D (p < 0.05) for bFGF (a). At days 1, 2, 4, 5, 6 and 8, a significant difference in protein release was obtained between groups C and D (p < 0.05) for VEGF165. bFGF release was less compared to VEGF165 in groups C and D. FS Fibrin sealant; GF growth factor
However, over 12 days, there was still a significant higher release of bFGF in the fibrin sealant containing group C than in group D (p < 0.05). VEGF165 release was significantly increased over 8 days at last (p < 0.05).
Results in vivo
Newly formed blood vessels in the dermal template were specified as the percentage of those of the surrounding tissue (Fig. 5).
Vascularisation of the matrix in vivo after 2 and 4 weeks. After 2 weeks, significantly more blood vessels could be seen in groups C and D, compared to groups A and B (p < 0.001). Significantly more blood vessels appeared in group D, compared to group C (p < 0.001). After 4 weeks, significantly more blood vessels were detected in groups C and D, compared to groups A and B (0.001). Significantly more blood vessels were evident in group C, compared to group D (p < 0.05). FS Fibrin sealant; GF growth factor
Group A was compared to group D, group B was compared to group C and group C was compared to group D (2 and 4 weeks).
After 2 and 4 weeks, group A obtained 17.5 ± 1.3 and 21.9 ± 1.0% newly formed blood vessels and group B 22.8 ± 1.9 and 27.0 ± 2.9%. Corresponding values for group C were 55.7 ± 2.9 and 80.0 ± 4.0% and for group D 82.6 ± 4.0 and 62.3 ± 4.0%, respectively.
At both time points, the application of VEGF165 and bFGF (groups C and D) leads to a significant higher vascularisation in the dermal template when compared to groups A and B (p < 0.001). Differences between the sole use of PBS or fibrin sealant (groups A and B) were significant in favour of group B after 2 weeks (p < 0.05), but not after 4 weeks (p = 0.1). Whereas vascularisation prevailed in group D after 2 weeks (p < 0.05), more blood vessels could be detected after 4 weeks in the growth factor and fibrin sealant combining group C (p < 0.001).
Pictures of the different groups after harvesting the target tissue at 2 and 4 weeks are shown in Fig. 6a,b. The deep-red colorations of the templates were evoked by haemoglobin (bleeding during harvesting). They were not interpreted by the VesSeg programme as blood vessels. The programme selectively recognises only longitudinal structures, but no corpuscular bodies as blood vessels.
Pictures of the different groups after harvesting the target tissue at 2 and 4 weeks. The deep-red colorations of the templates are evoked by haemoglobin (bleeding during harvesting). They are not interpreted by the VesSeg programme as blood vessels. The programme selectively recognises longitudinal structures, but no corpuscular bodies as blood vessels
Histology
Four matrices of each group from both experiments were analysed. Paraffin sections (5 μm) were stained with haematoxylin and eosin (Fig. 7a) and CD31 (Fig. 7b). Well-defined blood vessels were found in all groups, but it seemed as if more blood vessels were found in the groups treated with growth factors (as well after 2 and after 4 weeks). However, a quantification of the newly formed blood vessels was not performed, because histology is representing only a small part of the target tissue and varies within each sample. Representative pictures are shown in Fig. 7a and b.
Discussion
This article emphasises on the use of biodegradable carriers as vehicles for local and controlled delivery of angiogenic proteins, such as VEGF165 and bFGF.
A number of specific factors are known to stimulate or inhibit angiogenesis, including vascular growth factors, inflammatory cytokines, adhesion molecules and nitric oxide. Importantly, regulation of these factors is critical for efficient neovascularisation. Different biological activities are required in the different phases of angiogenesis from initiation to maturation [11]. Several growth factor families and cytokines that are capable to induce physiological blood vessel formation have been identified. In our study, we can confirm previous findings that demonstrate that angiogenesis can be enhanced by several growth factors like VEGF165 and bFGF [12].
Growth factors are bioactive proteins that play important roles in regulating growth and differentiation of specific cell types and act as cell–cell signalling messengers in the complex process of wound repair [13, 14]. Several of these growth factors, including VEGF and bFGF, are involved in regulating the formation of new blood vessels through angiogenesis [15].
VEGF possesses various biological activities. It enhances microvascular permeability, exerts mitogenic effects on endothelial cells, stimulates the proliferation and migration of endothelial cells, induces the expression of interstitial collagenase and promotes macrophage migration. VEGF is a key mediator of angiogenesis, as it is a potent mitogen for endothelial cells and induces endothelial cell migration and sprouting by upregulation of several endothelial integrin receptors [16]. However, VEGF alone is known to induce instable vessel structures (leaky vessels) [17]. Previous in vivo studies have shown that VEGF165 can induce temporary angiogenesis within several days [18].
bFGF, another well-studied angiogenic factor, elicits diverse biological effect on numerous cell types, including endothelial cells, and has been used in clinical trials to induce angiogenesis. bFGF has been incorporated into various polymers, such as gelatine, collagen, chitosan and polylactic acid. bFGF reversibly binds to heparin-like molecules and heparin sulphate proteoglycans [19]. This can be exploited to increase the FGF-binding capacity to polymeric delivery vehicles, resulting in a more gradual and sustained release of FGF and an enhancement of angiogenesis [19].
The development of new therapeutic approaches that aim to help the body to exert its natural mechanisms for vascularised tissue growth (therapeutic angiogenesis) has become one of the most active areas of tissue engineering.
One of these areas represents the development of biodegradable carriers. They may facilitate restoration of structure and function of damaged or dysfunctional tissues. Such biodegradable carriers are used in cell-based therapies. They are also used in acellular therapies where materials induce ingrowth and differentiation of cells from healthy residual tissues in situ [20].
In general, the use of acellular biodegradable carriers to support matrix vascularisation is beneficial because it can be used in many different ways, e.g. as matrices for cell infiltration to induce regeneration and remodelling in vivo or as carriers for transplanted cells, which are grafted into tissue defects. But working with cell-based therapies often means difficulties, e.g. purification of the cells or pathogen transmission. For clinical application, protein- or matrix-based therapies comprise the advantage of not including cellular components. This allows the use under the German Act on Medical Devices (Medizinproduktegesetz). This way, an extensive survey that is necessary for advanced cellular therapies according to the new German Tissue Law (Gewebegesetz) can be avoided.
A promising attempt to improve angiogenic performance is presented by biomaterials that allow sequential delivery of growth factors. Biodegradable carriers can serve as a slow release system for angiogenetic proteins.
The use of fibrin-based biomaterials in wound healing therapies is based on the fact that physiologic fibrin clots are an important provisional matrix in normal tissue repair. The ability of fibrin clots to stimulate and support the growth of new blood vessels is well documented and plays an important role in re-establishing the blood supply in injured areas. A fibrin network is critical for effective wound healing, and it is biodegradable through routine tissue fibrinolysis [15]. As fibrin is lysed slowly, it can serve as a vehicle to deliver various agents that may act to help healing wounds and to promote new vessel growth or to store and slowly release antibiotics and other therapeutic agents. Additionally, fibrin acts as a natural reservoir for the binding and release of certain growth factors as bFGF and VEGF165 [1].
Controlling the concentration, local duration and spatial distribution of these factors is a key to their utility and efficiency. To address this challenge, controlled delivery systems that incorporate growth factors into polymeric biomaterials have been developed to prolong the tissue exposure time and to maintain growth factor stability [16].
Attempts have been made to apply growth factors directly or to encode DNA for such factors [21, 22], but it is unknown whether these factors remain at the target site long enough to be effective. A prolonged effect of protein based therapy is needed to induce stable capillary structures. Synergistic effects of bFGF and VEGF to induce mature angiogenesis in vitro and in vivo have been described by several authors [23, 24]. Some found evidence that a combined therapy for these factors will decrease vessel leakage by reduction in vessel fenestration [25]. This data is also supported by Kondoh et al. [26], who found a significant increase in smooth muscle cell-positive density in an ischaemic rabbit hind limb model.
Stable angiogenesis can be induced by combined expression of VEGF165 and bFGF [27]. The combination of VEGF and bFGF has been reported to have potent synergistic effects on neovascular formation in experimental conditions both in vivo and in vitro [28].
In our in vitro experiment, we observed that proteins can be incorporated into the collagen structure of the Integra™ matrix. We were able to produce a model of slow protein release by combining VEGF165 and bFGF with fibrin sealant. The incorporation of the growth factors in fibrin sealant resulted in a prolonged growth factor release, which is represented by a significantly higher concentration of growth factors over several days in group C compared to group D (p < 0.05; Fig. 4a,b).
The matrices initially contained 1 μg of VEGF165 and 0.5 μg bFGF in groups C and D. Only small amounts of the applied proteins were detected in the medium, especially in the case of bFGF. A fast complete protein diffusion into the medium should have caused a primary peak in the growth factor concentration. But the amount of protein that degrades under physiologic conditions at 37°C before the medium is taken for the first measurement after 24 h would not appear in the values.
As protein measurements were performed only every 24 h, a continuous degradation of both proteins may therefore be responsible for the overall reduced concentration at the time of medium harvesting and processing. Values may only represent the protein release of a markedly shorter time period than the last 24 h. To conclusively answer this question, it would have been necessary to measure total amount of protein at the end of experiment within the matrix. This, however, was not performed.
Another explanation for the low detectable growth factor concentrations could be an interaction of the proteins with collagen or the fibrin sealant altering the function and detectability of the growth factors. At the 24-h time point, 9.7 and 6.6% of the initially administered amount of VEGF165 were detected in the medium in groups C and D, respectively. The corresponding values for bFGF were 1.7 and 0.19%. bFGF apparently underwent faster degradation, or it showed a stronger, maybe irreversible, binding to fibrin or collagen. To support this assumption, detection of VEGF165 and bFGF by immunohistochemistry in the dermal templates would be desirable. But detection could not be performed due to strong collateral staining of the collagen matrix and due to cross reactions with rodent VEGF165 and bFGF in vivo.
However, the higher levels of growth factors in the fibrin sealant containing group C compared to group D correspond to the in vivo findings of a better long lasting vascularisation in group C after 4 weeks.
In our in vivo experiments, we observed that the administration of VEGF165 and bFGF with or without incorporation in a fibrin sealant lead to a significant and faster neovascularisation of the bioartificial dermal collagen templates (Figs. 5, 6a,b). The incorporation in fibrin sealant initially lead to a minor angiogenetic effect compared to the free protein injection into the collagen. This effect was represented by a higher blood vessel concentration in group D (growth factor). However, after 4 weeks, this ratio reversed, resulting in a higher blood vessel density in the fibrin sealant and growth factor containing group C (growth factor+fibrin sealant).
This change is probably caused by the stronger retention of growth factors in the slow release system formed by fibrin sealant. A fast flow of the proteins into the surrounding tissue in group D probably resulted in an early stage boost of neovascularisation. But an increased, stable and long lasting vascularisation could only be evoked by the continuous growth factor supply in group C. As mentioned before, bFGF was retained for a longer time in the matrix than VEGF165. This could contribute to the following biological effect: VEGF is responsible for ‘vessel sprouting’ and the ingrowth of the vessels into the matrix. The part of bFGF left in the matrix is responsible for the stabilisation of the blood vessels [16]. This could be another reason why more blood vessels were detected in group C after 4 weeks.
Due to our developed new segmentation technique, a computer programme called VesSeg, designed by Condurache and Aach [10], we were able to quantify vascularisation of the whole matrix area in groups A to D (Figs. 3a–c and 6a,b). The programme only recognises longitudinal structures as blood vessels. After adjustment of the electronic photograph of the tissue, vessel quantification is nearly completely automated. We were the first to apply this technique for evaluation of the vessel density. The segmentation of the neovascularisation of the target tissue is more representative than the microvessel density shown by the histochemistry. Histology is representing only a small part of the target tissue, while the segmentation technique is showing the entirety. Therefore, we chose the latter for quantification.
Despite of the knowledge regarding the use of dermal regeneration templates in skin defects to induce vascularisation, issues remain in knowing how to give a stable structure to the new developing blood vessels. In other yet unpublished experiments, we could retrieve a stable formation of newly formed blood vessels over more than 6 months in a cell-based bioartificial dermal template after cell transfection with DNA sequences encoding VEGF165 and bFGF.
Blood vessel development after administration of growth factors combined with fibrin sealant seems to be more effective in producing a patent and stable vasculature than administration of growth factors alone. Our findings indicate that VEGF165 and bFGF were retained more strongly by the fibrin clots, and thus delivered more slowly. It is the first time this model has been applied for supporting neovascularisation in an artificial dermal substitute. This kind of slow release system may be also promising in the use of other proteins in dermal regeneration templates, for example chemokines, such as stromal cell-derived factor-1 or hypoxia-inducible factor-1α.
In our experiments, we were able to create a slow release system for VEGF165 and bFGF by protein incorporation into a slowly degrading fibrinclot placed in a bioartificial dermal regeneration template. The prolonged protein release proved to be beneficial for dermal regeneration. This approach is a promising system for a wide scope of functions in further research in tissue engineering.
References
Kipshidze N, Chekanov V, Chawla P, Shankar LR, Gosset JB, Kumar K, Hammen D, Gordon J, Keelan MH (2000) Angiogenesis in a patient with ischemic limb induced by intramuscular injection of vascular endothelial growth factor and fibrin platform. Texas Heart Inst J 27:196–200
Engler DA (1996) Use of vascular endothelial growth factor for therapeutic angiogenesis. Circulation 94:1496–1498
Shou M, Thirumurti V, Rajanayagam S, Lazarous DF, Hodge E, Stiber JA, Pettiford M, Elliott E, Shah SM, Unger EF (1997) Effect of basic fibroblast growth factor on myocardial angiogenesis in dogs with mature collateral vessels. J Am Coll Cardiol 29:1102–1106
Thompson JA, Anderson KD, DiPietro JM, Zwiebel JA, Zametta M, Anderson WF, Maciag T (1988) Site-directed neovessel formation in vivo. Science 241:1349–1352
Machens HG, Berger AC, Mailaender P (2000) Bioartificial skin. Cells tissues. Organs 167:88–94
Tompkins RG, Hilton JF, Burke JF, Schoenfeld DA, Hegarty MT, Bondoc CC, Quinby WC Jr, Behringer GE, Ackroyd FW (1989) Increased survival after massive thermal injuries in adults: preliminary report using artificial skin. Crit Care Med 17:734–740
Yannas IV, Burke JF (1980) Design of an artificial skin. I. Basic design principles. J Biomed Mater Res 14:65–81
Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N (1989) Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 246:1306–1309
Sommer A, Brewer MT, Thompson RC, Moscatelli D, Presta M, Rifkin DB (1987) A form of human basic fibroblast growth factor with an extended amino terminus. Biochem Biophys Res Commun 144:543–550
Machens HG, Grzybowski S, Bucsky B, Spanholtz T, Niedworok C, Maichle A, Stockelhuber B, Condurache A, Liu F, Egana JT, Kaun M, Mailander P, Aach T (2006) A technique to detect and to quantify fasciocutaneous blood vessels in small laboratory animals ex vivo. J Surg Res 131:91–96
Fam NP, Verma S, Kutryk M, Stewart DJ (2003) Clinician guide to angiogenesis. Circulation 108:2613–2618
Koolwijk P, van Erck MG, de Vree WJ, Vermeer MA, Weich HA, Hanemaaijer R, van HV (1996) Cooperative effect of TNFalpha, bFGF, and VEGF on the formation of tubular structures of human microvascular endothelial cells in a fibrin matrix. Role of urokinase activity. J Cell Biol 132: 1177–1188
Kim WJ (2000) Cellular signaling in tissue regeneration. Yonsei Med J 41:692–703
Pierce GF, Mustoe TA (1995) Pharmacologic enhancement of wound healing. Annu Rev Med 46:467–481
Wong C, Inman E, Spaethe R, Helgerson S (2003) Fibrin-based biomaterials to deliver human growth factors. Thromb Haemost 89:573–582
Elcin YM, Dixit V, Gitnick G (2001) Extensive in vivo angiogenesis following controlled release of human vascular endothelial cell growth factor: implications for tissue engineering and wound healing. Artif Organs 25:558–565
Carmeliet P (2005) VEGF as a key mediator of angiogenesis in cancer. Oncology 69(Suppl 3):4–10
Machens HG, Spanholtz T, Maichle A, Niedworok C, Lindenmaier W, Herbort-Brand S, Görg G, Kropf K, Stöcklhuber B, Reichert B, Siemers F, Krapohl B, Mailaender P (2003) Ein neues gentechnologisches Modell zur Angiogeneseinduktion mittels ex vivo transfizierter isogener Fibroblasten. Chir Forum Exp Klin Forsch 32:237–240
Boontheekul T, Mooney DJ (2003) Protein-based signaling systems in tissue engineering. Curr Opin Biotechnol 14:559–565
Lutolf MP, Hubbell JA (2005) Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nat Biotechnol 23:47–55
Bauters C, Asahara T, Zheng LP, Takeshita S, Bunting S, Ferrara N, Symes JF, Isner JM (1995) Site-specific therapeutic angiogenesis after systemic administration of vascular endothelial growth factor. J Vasc Surg 21:314–324
Tsurumi Y, Takeshita S, Chen D, Kearney M, Rossow ST, Passeri J, Horowitz JR, Symes JF, Isner JM (1996) Direct intramuscular gene transfer of naked DNA encoding vascular endothelial growth factor augments collateral development and tissue perfusion. Circulation 94:3281–3290
Pepper MS, Ferrara N, Orci L, Montesano R (1992) Potent synergism between vascular endothelial growth factor and basic fibroblast growth factor in the induction of angiogenesis in vitro. Biochem Biophys Res Commun 189:824–831
Asahara T, Bauters C, Zheng LP, Takeshita S, Bunting S, Ferrara N, Symes JF, Isner JM (1995) Synergistic effect of vascular endothelial growth factor and basic fibroblast growth factor on angiogenesis in vivo. Circulation 92:II365–II371
Cao R, Eriksson A, Kubo H, Alitalo K, Cao Y, Thyberg J (2004) Comparative evaluation of FGF-2-, VEGF-A-, and VEGF-C-induced angiogenesis, lymphangiogenesis, vascular fenestrations, and permeability. Circ Res 94:664–670
Kondoh K, Koyama H, Miyata T, Takato T, Hamada H, Shigematsu H (2004) Conduction performance of collateral vessels induced by vascular endothelial growth factor or basic fibroblast growth factor. Cardiovasc Res 61:132–142
Cao R, Brakenhielm E, Pawliuk R, Wariaro D, Post MJ, Wahlberg E, Leboulch P, Cao Y (2003) Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a combination of PDGF-BB and FGF-2. Nat Med 9:604–613
Kano MR, Morishita Y, Iwata C, Iwasaka S, Watabe T, Ouchi Y, Miyazono K, Miyazawa K (2005) VEGF-A and FGF-2 synergistically promote neoangiogenesis through enhancement of endogenous PDGF-B-PDGFRbeta signaling. J Cell Sci 118:3759–3768
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wilcke, I., Lohmeyer, J.A., Liu, S. et al. VEGF165 and bFGF protein-based therapy in a slow release system to improve angiogenesis in a bioartificial dermal substitute in vitro and in vivo. Langenbecks Arch Surg 392, 305–314 (2007). https://doi.org/10.1007/s00423-007-0194-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-007-0194-1