Abstract
Background
Secondary peritonitis causes considerable mortality and morbidity. New strategies have been introduced like relaparotomy and temporary abdominal closure in the management of such persistent intra-abdominal infections.
Materials and methods
Rats were divided into five groups each having ten animals. After induction of peritonitis, relaparotomies were done, and the abdomen was closed by different temporary abdominal closure techniques. After performing two relaparotomies during a 48-h period, all fascias closed primarily and incisional tensile strengths, hydroxyproline contents, and adhesions were measured on the following seventh day.
Results
The median values of tensile strength and hydroxyproline concentrations were lowest in skin-only closure rats. Intraperitoneal adhesion scores were highest in Bogota bag closure group.
Conclusion
Primary, Bogota bag, and polyprolene mesh closures seem to be safe in terms of early fascial wound healing. Although it is easy to perform, skin-only closure technique has deleterious effects on fascial wound healing probably due to fascial retraction. Interestingly, Bogota bag has caused increased intraperitoneal adhesion formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Secondary peritonitis after perforation or postoperative anastomotic disruption of the digestive tract is characterized with considerable mortality and morbidity rates [1]. Currently, timely control or elimination of the source of the infection by surgery, antimicrobial therapy, and critical care support constitutes the main parts of the standard treatment [2]. However, in the presence of persistent or recurrent intra-abdominal infections, this standard therapy consisting of source control, lavage, and primary closure is considered to be insufficient [3]. Correspondingly, new strategies such as relaparotomy and temporary abdominal closure have been introduced [4–6].
Despite well-described advantages of various temporary abdominal closure techniques, the ongoing intraperitoneal sepsis and trauma to the fascial edges during relaparotomies may affect wound healing negatively and contribute in the formation of a ventral hernia [7–12]. The incidence of ventral hernia is reported to be up to 21% even in patients with primary fascial closure in the early postoperative period after temporary abdominal closure [13]. As well as fascial wound healing, the incidence and amount of postoperative adhesion formation after temporary abdominal closure is also another matter of concern for surgeons. Adhesions between the intestine and abdominal wall may be the reason of serious complications and difficult laparotomies in the future management of the patients [14].
Currently, due to lack of prospective randomized clinical studies regarding the best temporary abdominal closure technique, no one method has yet emerged in as clearly superior. The skin-only technique was used to close the abdomen rapidly, thus permitting resuscitation of the clotting system, shock, and hypothermia [15, 16]. Potential disadvantages are evisceration, injury and loss of skin, and a high incidence of abdominal compartment syndrome [16]. The Bogota bag process is observed first in Colombia in the management of devastating abdominal injuries [16]. The technique consists of sewing large sterile polyvinyl chloride genitourinary irrigation bags to the skin or fascia. The advantages are that they are widely available, inexpensive, biologically inert, and minimize fluid loss. Disadvantages include loss of abdominal domain and ease of tearing with subsequent evisceration [7, 9, 17]. Polypropylene meshes are resistant to infection; they allow egress of fluid and are relatively easy to apply either to skin or fascia. However, in a summary of 14 studies involving 128 patients managed with a polypropylene mesh, it is reported that there was a 23% enterocutaneous fistula rate [18]. Because of the difficulties in designing a randomized prospective clinical study, it is obvious that well-designed experimental models are needed to investigate the effects of relaparotomies and temporary abdominal closure techniques on the healing of abdominal fascia and postoperative adhesions. Therefore, in this present study, we investigated the effects of different temporary abdominal closure techniques on the fascial wound healing and adhesion formation in rats with secondary peritonitis.
Materials and methods
The study was performed with Sprague–Dawley rats weighing between 125 and 150 g. The animals were housed in wire-bottom cages at room temperature with a 12-h light–dark cycle and had free access to water and standard rat chow until 12 h before surgery. The use of anesthesia during the surgical procedure and subsequent postoperative care were consistent with the guidelines in the National Institute of Health’s Guide for the Care and Use of Laboratory Animals (National Institutes of Health publication no. 86-23, revised 1985, Bethesda, MD, USA). The study was also approved by the Animal Ethics Committee of the Pamukkale University Medical School.
Study groups
Rats were divided into five groups each having ten animals. A cecal ligation and puncture (CLP) was performed in all groups except in controls (group I) to induce bacterial peritonitis. On the following day, relaparotomy was done in all rats, the peritoneal cavity was flushed with sterile 0.09% NaCl solution, and the abdomen was closed as follows: In group I (control), the abdomen was closed primarily; in group II, only the skin was closed; and in groups III and IV, a sterile plastic bag (Bogota bag) and polypropylene mesh were used for temporary abdominal closure, respectively. In group V, primary fascial closure was performed as in group I. While controls (group I) underwent no relaparotomy thereafter, two relaparotomies were done with 24-h interval in the other groups. Finally, after completion, a total of 48-h interval with temporary abdominal closure technique, the abdominal fascia were closed primarily in groups I, II, III, IV, and V. On the seventh day of the final closure, rats were killed, tensile strength of fascial suture line was measured in each rat, and tissue samples for biochemical analysis were obtained by different investigators blinded to the operations.
Operative details
Animals were fasted overnight and anesthetized by an intramuscular injection of 50 mg/kg ketamine (Ketalar; Parke Davis, Eczacibasi, Istanbul, Turkey) and xylazine 10 mg/kg (Rompun; Bayer AG, Leverkusen, Germany) and allowed to breathe spontaneously during the surgery. Sterile saline solution (NaCl 0.9%, 10 ml) was given subcutaneously in the dorsal area to prevent dehydration of the rats.
The abdomen was entered through a midline incision. Bacterial peritonitis was induced with CLP as described previously [19]. The cecum was identified, dissected, and ligated with a 3-O silk tie after filling backward with feces. Special care was taken to prevent bowel obstruction and maintain continuity of the intestinal flow. Subsequently, the cecum was punctured once with an 18-G needle at the antimesenteric side, squeezed gently until feces were just visible through the puncture, and then placed back into the abdominal cavity. The abdominal incision was closed with running 4/0 polyglactin suture (Vicryl, Ethicon, UK). After abdominal closure, rats received a single dose of ciprofloxacin 20 mg/kg body weight plus clindamycin 15 mg/kg body weight and 10 ml saline solution subcutaneously for compensation of perioperative fluid loss. After 24 h of CLP, the abdomen was reopened, and the ligated cecum was resected. Samples were taken by swabs for verification of the induced peritonitis. Peritoneal lavage further continued with 40 ml of warm sterile saline. The abdomen was closed continuously with 4/0 polyglactin suture (Vicryl, Ethicon, UK) in groups I and V. In group II, abdominal fascia was left open and only the skin was closed primarily with 4/0 polypropylene suture (Prolene, Ethicon, UK) continuously. In group III, a sterile 150-ml plastic serum bag was adapted to cover the abdominal viscera. The bag was secured to the abdominal fascia with continuous 4/0 polypropylene suture (Prolene, Ethicon, UK). In group IV, a 3 × 4-cm piece of polypropylene mesh was used to close the abdomen, which was sutured to the fascia in the same way with group III. After 24 h, rats were anesthetized again in groups II, III, IV, and V, with the peritoneal cavity reopened and irrigated with warmed sterile saline. Thereafter, the abdomen was closed temporarily in the same manner with the previous relaparotomy in each group, as described above.
Tensile strength
Tensile strength of the fascial suture line was measured by a simple technique, which is a modification of a previously described one elsewhere [20]. First, directly after killing, strips of abdominal wall measuring 1 × 2 cm, including 1-cm length of suture line in the midpoint and 1 cm of fascia on each side of this suture line, were prepared. It was then held from the inferior side with a clamp that was secured to a 1,000-g weight placed on a digital weight scale. The upper side of fascia was held with another clamp that was secured to an electric motor with a 2/0 monofilament suture (Prolene, Ethicon, UK). During the upward steady traction at a speed of 5 mm/s, maximum decrease in the weight just at the time of separation was accepted as tensile strength of the fascial suture line.
Biochemical analysis
Another 2 × 1-cm portion of the abdominal wall sample, including the suture line in the middle, was frozen in liquid nitrogen and stored at −80°C for further biochemical analysis. As previously described in detail, tissue hydroxyproline concentrations were determined by using a modified procedure based on alkaline hydrolysis of the tissue homogenate and subsequent determination of the free hydroxyproline in hydrolyzates [21]. Results were expressed in micrograms of hydroxyproline per milligram of tissue (μ/mg, wet weight).
Scoring of adhesions
Density of adhesions was scored according to the classification of Zuhlke et al. [22]. Sites of adhesions scored included the midline, adnexial/epididymal fat bodies, the upper abdomen (liver), the parietal peritoneum, the omentum, and between the bowel loops. The total score of these six locations was noted as the total adhesion score (0–24). Two independent investigators, who were blinded to the group assignment of the rats, performed scoring of adhesions and incorporation. In case of inter-observer variance, the median was scored.
Statistical analysis
The results were expressed as mean±SEM and median (range) where appropriate. The differences among the groups were evaluated using Kruskal–Wallis variance analysis and Mann–Whitney U test. Differences were considered statistically significant when P < 0.05. Data were analyzed by statistical software [Statistical Package for the Social Sciences (SPSS) for Windows 11.5; SPSS, Chicago, IL, USA].
Results
A total of five animals died during the study, two of them from group II and one from each group except the controls (group I). There were symptoms and peritoneal findings of sepsis such as lethargy, piloerection, exudation, and pus formation with filmy adhesions around cecum 1 day after CLP in all rats.
Tensile strength
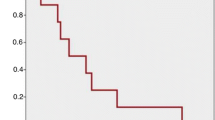
All wounds were mechanically disrupted at the fascia-to-fascia interface. The median tensile strength measurements were significantly different among the groups (X 2 = 10.333, df = 4, P < 0.05; Fig. 1). While groups I, III, IV, and V have almost similar median tensile strength values, skin-only closure rats (group II) have significantly lower values when compared with values in the other four groups (P < 0.05).
Hydroxyproline concentrations in fascial healing tissue
The median tissue hydroxyproline concentrations were significantly different among the groups (X 2 = 12.748, df = 4, P < 0.05; Fig. 2). Parallel with the tensile strength values, median tissue hydroxyproline concentrations were significantly lower in skin-only closure rats when compared to all other groups (P < 0.05).
Adhesion score
The median adhesion scores were significantly different among the groups (X 2 = 20.839, df = 4, P < 0.05; Fig. 3). Only the Bogota bag closure rats (group III) have significantly increased adhesion scores when compared to the other four groups (P < 0.05).
Body weight analyses
The mean body weights were reduced in all of the groups during the study period (Table 1). There was no statistically significant difference in the rate of weight reduction among the groups (X 2 = 5.089, df = 4, P > 0.05).
Discussion
This current study has shown that temporary abdominal closure with skin-only technique has a negative effect on early fascial wound healing in an experimental model of intra-abdominal infection. Additionally, as a temporary closure technique, usage of Bogota bag resulted in a statistically significant high rate of postoperative intraperitoneal adhesions.
Planned abdominal re-explorations are increasingly taking place in the current management of severe secondary peritonitis. Recurrent or persistent peritonitis is the main reason, which requires multiple operative interventions. Re-evaluation of known injuries, control of gastrointestinal continuity, and delayed closure to avoid abdominal compartment syndrome are major concerns in the emergency setting. On the other hand, fascial dehiscence and finally ventral hernias constitute the other challenging issues in the long term. As an alternative to primary fascial closure, numerous methods of temporary abdominal closure have been proposed but, currently, there is no consensus regarding the best technique [7–11, 13, 23, 24]. It is logical that the optimal technique should protect the bowel from adhesions and desiccation, preserve the skin and fascial edges for definitive closure, and permit visual inspection of the abdominal cavity [3, 16, 23]. Some previous experimental studies focused on the optimal prosthetic material in the presence of peritonitis [25, 26]. Despite the fact that prosthetic mesh grafts are commonly preferred for temporary abdominal closure in the clinical setting, skin-only closure or even primary fascial closure may well be used especially when the abdominal compartment syndrome is not a problem [7]. Therefore, in an effort to compare all these temporary abdominal closure options including the Bogota bag, this experimental study consisted of five groups.
Collagen is important in all phases of wound healing and is critical for the regaining of tissue integrity and strength [27]. In our study, we determined the levels of hydroxyproline content in the abdominal fascia at the incision site as an indicator of collagen synthesis and wound healing. The tensile strength of the wound depends on the equilibrium between collagen lysis, which occurs early, and collagen synthesis, which takes a few days to initiate [27]. However, ultimate wound strength is not always related to the absolute amount of collagen, and the structure and arrangement of the collagen matrix may be also important [28]. The mechanical stability of laparotomy incision is achieved after 5–7 days in rats [29–32]. Therefore, we also measured the tensile strength in addition to tissue hydroxyproline content analysis on the seventh day of final closure of the abdomen.
The important role of nutritional status is also a well-recognized factor that influences wound healing. Because body weight changes were similar in all study groups, it seems unlikely that differences in the nutritional status are responsible for the differences in wound healing observed in the current study. There was no statistically significant difference between the groups in terms of body weight loss, and in experimental studies it has been shown that weight loss of less than 20% of body weight did not have an effect on wound healing [33, 34]. Therefore, the percentage of weight reduction in animals are not enough to describe that the malnutrition is a factor that might affect the fascial wound healing in our study.
Skin-only closure of the abdominal incision is perhaps the most rapid of the temporary closure techniques. Additional advantages are low cost and minimization of heat and fluid losses. It is performed using a running nonabsorbable suture or towel clips placed to the skin approximately 1 cm apart. Disadvantages include possible evisceration, injury and loss of skin, and a high incidence of abdominal compartment syndrome [7, 11]. In our study, the worst results in terms of fascial wound healing were obtained in the skin-only closure group. According to these results, suturing only skin seems to be the most disadvantageous method with regard to early fascial wound healing and thus preventing ventral hernia formation in the long term. Although it was not evaluated in our study, fascial retraction was considered to be a factor as causing a tension in the suture line at the moment of definitive closure and resulting in a failure of wound healing [16, 23]. Supporting this idea, high suture tension has been previously shown to affect the mechanical quality of midline laparotomies inadvertently [35, 36].
Several types of mesh materials have been used for temporary closure of the abdominal wall, including polypropylene, polyglactin, and polytetrafluoroethylene [9, 11, 26]. As predominating materials for temporary abdominal closure, meshes permit drainage of infected fluids, visualization of the underlying viscera, and mobilization of the patient [23]. The interaction between usage of mesh and the occurrence of ventral hernia was analyzed in a clinical study, which reveals a 16% increased risk of ventral hernia for each day of open abdomen with prosthetic mesh [12]. In the same study, it was concluded that this increased rate of ventral hernia was also related to the severity of the abdominal injury because the more time that fascial edges remains far apart, the more fixed in the position they become and less likely they are to ever be approximated. Therefore, according to these findings, due to the natural differences of abdominal injury scores, it is not possible to compare statistically the relation between hernia formation and usage of mesh itself. Therefore, designing an experimental model that minimizes the differences between the degrees of abdominal injury makes it possible to compare the results of mesh usage with the other temporary abdominal closure techniques. In this present work, to provide comparable study groups by means of the severity of the abdominal injury, the same procedure (CLP) was performed. Polypropylene was utilized in our study, and there was no harmful effect on fascial wound healing when compared to other groups. The degree of intraperitoneal adhesions with polypropylene mesh was also similar with the other groups except the Bogota bag group, which has the highest adhesion scores.
Another method for temporary abdominal closure applies an empty and sterile plastic bag (Bogota bag) of the type used for intravenous fluid administration or for urological irrigation, which is secured to the edges of fascia with a continuous monofilament suture [7, 9]. These materials are inexpensive, easy to apply and remove, biologically inert, minimize fluid loss, prevent musculoaponeurotic necrosis, and allow the drainage of infectious material and the inspection of the intestine [3, 16]. Disadvantages include loss of abdominal domain and ease of tearing with subsequent evisceration [16]. To our knowledge, applying a Bogota bag in a rat model was not used previously despite relatively common preference of this technique among the clinicians. Rather the short time of usage may be sensed by the surgeons that it would not have any problem with the fascial wound healing and also intraperitoneal adhesion formation. In our study, while the parameters of fascial wound healing were not different compared to controls, intraperitoneal adhesions were interestingly highest in Bogota bag group. The mechanism of this high rate of postoperative intraperitoneal adhesions related with the usage of Bogota bag is not clear. The initiation of adhesion formation begins with configuration of a fibrin matrix, which typically occurs during coagulation. Surgical injury to tissues produces ischemia, which leads to local persistence of fibrin matrix. Eventually, this matrix is replaced by vascular granulation tissue and covered by mesothelium that contains blood vessels and connective tissue fibers [37]. Some factors such as abdominal infection, inconvenient surgical techniques, and foreign bodies have been described to increase the amount of adhesion formation [37, 38]. The cecal ligation puncture model that we used in our study seems to be one of the main promoting factors for adhesions. It is also known that the foreign bodies that left the abdomen cause adhesion formation by inducing allergic reactions [37, 39]. Recently, Zografos et al. [40] have showed in an animal study that pieces of polyurethane, Teflon, silicone, and polyvinyl chloride, which were placed intraperitoneally, all caused adhesion formation. Similarly in our study, higher adhesion scores in group III rats may be explained in part by the effect of Bogota bag as a foreign body. Although the Bogota bag cannot be considered as an intraperitoneal foreign body, it has wide-enough surfaces that are in direct connection with the visceral peritoneum. Based on the relationship between the surface area and the adhesion formation, it may be speculated that the foreign bodies, which have a mesh pattern, cause less reaction in the peritoneum because of a decreased surface contact with the material. Therefore, less adhesion formation in the propylene mesh group when compared to Bogota bag group may be explained by this theory.
As previously mentioned, the primary fascial closure technique can be used when there are no clinical signs of abdominal compartment syndrome. The advantages of this technique are that it ensures optimal environment by covering the fascial repair with skin and subcutaneous tissue; it also maintains the integrity of the fascia and limits its retraction [16]. In our model, primary fascial closure group had favorable results as expected. Both the hydroxyprolin content and tensile strength of the fascia were not different from the controls. As for the adhesions, there is also no difference from the other groups except Bogota bag group.
In conclusion, in this current study, temporary abdominal closure with skin-only technique has a negative effect on fascial wound healing in the management of secondary peritonitis when compared to other techniques such as polypropylene mesh, Bogota bag, and primary fascial closure. In practice, Bogota bag is an inexpensive, non-adherent, widely available, and biologically inert material. It also minimizes heat and fluid loss, permits re-exploration of the abdomen, and decreases the rate of abdominal compartment syndrome [15, 16]. However, despite the relatively short duration, Bogota bag usage increased the rate of intraperitoneal adhesions in this current study. Further studies are needed to elucidate the mechanisms that cause increased adhesions related to Bogota bag.
References
Wittmann DH, Schein M, Condon RE (1996) Management of secondary peritonitis. Ann Surg 224(1):10–18
Koperna T (2000) Surgical management of severe secondary peritonitis. Br J Surg 87(3):378
Schachtrupp A, Fackeldey V, Klinge U, Hoer J, Tittel A, Toens C, Schumpelick V (2002) Temporary closure of the abdominal wall (laparostomy). Hernia 6(4):155–162
Lamme B, Boermeester MA, Belt EJ, van Till JW, Gouma DJ, Obertop H (2004) Mortality and morbidity of planned relaparotomy versus relaparotomy on demand for secondary peritonitis. Br J Surg 91(8):1046–1054
Koperna T, Schulz F (2000) Relaparotomy in peritonitis: prognosis and treatment of patients with persisting intraabdominal infection. World J Surg 24(1):32–37
Hutchins RR, Gunning MP, Lucas DN, Allen-Mersh TG, Soni NC (2004) Relaparotomy for suspected intraperitoneal sepsis after abdominal surgery. World J Surg 28(2):137–141
Feliciano DV, Burch JM (1991) Towel clips, silos, and heroic forms of wound closure. Adv Trauma Crit Care 6:231–250
Brock WB, Barker DE, Burns RP (1995) Temporary closure of open abdominal wounds: the vacuum pack. Am Surg 61(1):30–35
Ghimenton F, Thomson SR, Muckart DJ, Burrows R (2000) Abdominal content containment: practicalities and outcome. Br J Surg 87(1):106–109
Sherck J, Seiver A, Shatney C, Oakes D, Cobb L (1998) Covering the “open abdomen”: a better technique. Am Surg 64(9):854–857
Tremblay LN, Feliciano DV, Schmidt J, Cava RA, Tchorz KM, Ingram WL, Salomone JP, Nicholas JM, Rozycki GS (2001) Skin only or silo closure in the critically ill patient with an open abdomen. Am J Surg 182(6):670–675
Mayberry JC, Burgess EA, Goldman RK, Pearson TE, Brand D, Mullins RJ (2004) Enterocutaneous fistula and ventral hernia after absorbable mesh prosthesis closure for trauma: the plain truth. J Trauma 57:157–162
Howdieshell TR, Proctor CD, Sternberg E, Cue JI, Mondy JS, Hawkins ML (2004) Temporary abdominal closure followed by definitive abdominal wall reconstruction of the open abdomen. Am J Surg 188(3):301–306
Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, McGuire A, Lower AM, Hawthorn RJ, O’Brien F, Buchan S, Crowe AM (1999) Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 353(9163):1476–1480
Fabian TC (2007) Damage control in trauma: laparotomy wound management acute to chronic. Surg Clin North Am 87:73–93
Rutherford EJ, Skeete DA, Brasel KJ (2004) Management of the patient with an open abdomen: techniques in temporary and definitive closure. Curr Probl Surg 41(10):815–876
Myers JA, Latenser BA (2002) Nonoperative progressive “Bogota bag” closure after abdominal decompression. Am Surg 68:1029–1030
Jones JW, Jurkovich GJ (1989) Polypropylene mesh closure of infected abdominal wounds. Am Surg 55:73–76
Wichterman KA, Baue AE, Chaudry IH (1980) Sepsis and septic shock—a review of laboratory models and a proposal. J Surg Res 29(2):189–201
Aytekin FO, Tekin K, Kabay B, Erdem E, Erbis H, Ozden A (2004) Role of a hyaluronic-acid derivative in preventing surgical adhesions and abscesses related to dropped bile and gallstones in an experimental model. Am J Surg 188(3):288–293
Reddy GK, Enwemeka CS (1996) A simplified method for the analysis of hydroxyproline in biological tissues. Clin Biochem 29:225–229
Zuhlke HV, Lorenz EM, Straub EM, Savvas V (1990) Pathophysiology and classification of adhesions. Langenbecks Arch Chir Suppl II Verh Dtsch Ges Chir:1009–1016
Losanoff JE, Richman BW, Jones JW (2002) Temporary abdominal coverage and reclosure of the open abdomen: frequently asked questions. J Am Coll Surg 195(1):105–115
Navsaria PH, Bunting M, Omoshoro-Jones J, Nicol AJ, Kahn D (2003) Temporary closure of open abdominal wounds by the modified sandwich-vacuum pack technique. Br J Surg 90(6):718–722
Bellon JM, Garcia-Honduvilla N, Carnicer E, Serrano N, Rodriguez M, Bujan J (2004) Temporary closure of the abdomen using a new composite prosthesis (PL-PU99). Am J Surg 314–320
Nagy KK, Perez F, Fildes JJ, Barrett J (1999) Optimal prosthetic for acute replacement of the abdominal wall. J Trauma 47(3):529–532
Barbul A (2005) Wound healing. In: Brunicardi FC (ed) Schwartz’s principles of surgery, 8th edn. McGraw-Hill, New York, pp 223–249
Hoer JJ, Junge K, Schachtrupp A, Klinge U, Schumpelick V (2002) Influence of laparotomy closure technique on collagen synthesis in the incisional region. Hernia 6(3):93–98
Poole GV Jr, Meredith JW, Kon ND, Martin MB, Kawamoto EH, Myers RT (1984) Suture technique and wound-bursting strength. Am Surg 50(10):569–572
Seid MH, McDaniel-Owens LM, Poole GV Jr, Meeks GR (1995) A randomized trial of abdominal incision suture technique and wound strength in rats. Arch Surg 130(4):394–397
Sitges-Serra A, Hernandez R, Maestro S, Fernandez N, Girvent M, Sancho JJ (2001) Influence of parenteral nutrition on postoperative recovery in an experimental model of peritonitis. Clin Nutr 20(5):439–443
Franz MG, Smith PD, Wachtel TL, Wright TE, Kuhn MA, Ko F, Robson MC (2001) Fascial incisions heal faster than skin: a new model of abdominal wall repair. Surgery 129(2):203–208
Haciyanli M, Fuzun M, Unek T, Tokgoz Z (2001) Does the administration route of leucovorin have any influence on the impairment of colonic healing caused by intraperitoneal 5-fluorouracil treatment? Eur Surg Res 33(2):80–85
Irvin TT (1978) Effects of malnutrition and hyperalimentation on wound healing. Surg Gynecol Obstet 146(1):33–37
Hoer J, Klinge U, Schachtrupp A, Tons C, Schumpelick V (2001) Influence of suture technique on laparotomy wound healing: an experimental study in the rat. Langenbecks Arch Surg 386(3):218–223
Hogstrom H, Haglund U, Zederfeldt B (1990) Tension leads to increased neutrophil accumulation and decreased laparotomy wound strength. Surgery 107(2):215–219
diZerega GS, Campeau JD (2001) Peritoneal repair and post-surgical adhesion formation. Hum Reprod Update 7(6):547–555
Ellis H (1982) The causes and prevention of intestinal adhesions. Br J Surg 69(5):241–243
Luijendijk RW, de Lange DC, Wauters CC, Hop WC, Duron JJ, Pailler JL, Camprodon BR, Holmdahl L, van Geldorp HJ, Jeekel J (1996) Foreign material in postoperative adhesions. Ann Surg 223(3):242–248
Zografos GC, Simeonidis KM, Messaris EG, Parasi AS, Sotiriou HG, Dontas IA (2005) Adhesion formation and intraperitoneal catheters: histologic findings in a rat model. Fertil Steril 83(2):516–518
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aydin, C., Aytekin, F.O., Yenisey, C. et al. The effect of different temporary abdominal closure techniques on fascial wound healing and postoperative adhesions in experimental secondary peritonitis. Langenbecks Arch Surg 393, 67–73 (2008). https://doi.org/10.1007/s00423-007-0189-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-007-0189-y