Abstract
Background
Due to the complex embryologic development, pancreatic anatomy can be very variable.
Discussion
The authors present the second ever reported case in the literature of a complete pancreatic encasement of the portal vein which forced us to alter the standard operative procedure of pancreatic head resection, thus enabling possible dangerous complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Due to the complex embryologic development the pancreas has a broad spectrum of anatomic variants like pancreas divisum or pancreas annulare [1–3]. This knowledge is important for the visceral surgeon performing pancreatic surgery [4]. We present a concurrent finding of an extremely rare anomaly of a complete pancreatic encasement of the portal vein. This anatomic variant is well known in pigs but in humans, it has been described just once before in the literature [5].
Case report
A 65-years-old female patient presented with gastric outlet obstruction and weight loss of 5 kg over 2 months. The gastroscopic finding showed a considerable swelling of the antric mucosa; there was no histological evidence of a malignancy. The computed tomography (CT) scan taken at an external hospital solely showed an irregular swelling of the gastric posterior wall without metastasis. The pylorus was completely obstructed so that under clinically urgent suspicion for malignancy, an operative exploration was indicated.
Intraoperatively, we found a tumor of 5 × 5 cm in the distal antral wall which infiltrated the mesocolon transversum and the pancreatic head. To achieve a R0 resection, we performed a subtotal gastrectomy, a right hemicolectomy, and a pancreatic head resection. While transecting the pancreatic parenchyma on the portal vein, we detected the parenchyma of the uncinate process communicating behind the portal vein with the pancreatic body. This area (3 × 1 cm) caused a complete encasement of the portal vein (Figs. 1 and 2). A typical anatomic situation is depicted in Fig. 3. The aberrant connection was dissected with a GIA on the right border of the portal vein and sewn with PDS 4/0. The pancreaticojejunostomy was carried out in typical manner in front of the portal vein in duct-to-mucosa technique. Histology of the retroportal dissection showed, as suspected, pancreatic parenchyma (Fig. 4). Pathology confirmed a gastric cancer (pT4, pN0, cM0, R0).
Intraoperative finding. Pancreatic tissue transected in front of the portal vein. Portal vein (PV), axis of superior mesenteric vein (SMV), axis of splenic vein (SPV), pancreatic head (PH), duodenum (Duo), transection in front of the portal vein (A), aberrant pancreatic tissue behind the portal vein (X)
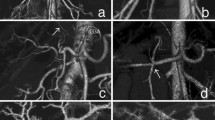
Postoperatively, the patient received octreotide (3 × 100 μg/d) for 5 days. The postoperative course was uneventful and the patient was dismissed on POD 18. The patient was readmitted with fever, pain in the upper abdomen, and slightly increased levels of CRP (10.9 mg/dl, norm <0.5) on POD 22. CT scan showed a liquid collection in direct contact to the aberrant pancreatic parenchyma (Fig. 5c,d). Additionally, the CT scan demonstrated a direct connection of the transected aberrant pancreatic parenchyma behind the portal vein to the pancreatic body (Fig. 5a,b). The liquid collection was drained interventionally with a transhepatic catheter revealing a putrid liquid with a high activity of lipase and amylase (lipase 3,506 U/l—norm 13–60; amylase 202 U/I–norm 13–53). Under antibiotic therapy the inflammation parameters as well as the lipase and amylase values were decreasing. The drain was removed on day 14 after insertion. The patient was dismissed three days later.
Contrast enhanced postoperative CT scan after second admission to hospital revealing the transection line (clips) (light arrow in a, b, and d) and part of the aberrant pancreatic tissue (bold arrow in a and b) behind the portal vein (open arrow in a). Cauda and corpus of the pancreas (arrowhead in a and b) are inconspicuous. Note a liquid collection (asterisk in c and d) with connection to the stapler line (light arrow in d) indicating a pancreatic fistula starting from the aberrant pancreatic tissue
Discussion
We report the second case ever published of a complete encasement of the portal vein by pancreatic parenchyma in humans.
The pancreas develops from the ventral (uncinate process and part of the pancreatic head) and foregut endoderm. During the process of the embryogenesis, both pancreatic primordia rotate and join behind the duodenum. A complete fusion of the uncinate process with the dorsal primordium has been described once by Hamanaka et al. [1, 2, 5]. This very rare anomaly has lead us to modify the operative procedure—a second transection of the accessory pancreatic parenchyma was necessary and thus a potentially dangerous complication resulted. Considering the CT scans, we assume that the origin of the pancreatic fistula was a small leakage in the stapler line of the transected aberrant pancreatic tissue. Because the stapler line appeared to be sufficient, we did not consider a complete transection of the pancreatic body on the left side of the portal vein and anastomosis to the jejunal loop. Retrospectively, this could have lowered the risk of a pancreatic leakage. Pancreatic leakage constitutes a clinically relevant complication especially in tumor patients despite of an improved suture technique of the pancreatojejunostomy [6, 7]. In designated centers, there is a prevalence of 10% with a mortality rate up to 12%—in most cases a treatment with a drainage is possible [8–10]. This case report shows that in pancreatic surgery, it is important to recognize even rare anomalies and to modify the operative procedure to minimize postoperative morbidity.
References
Nijs E, Callahan MJ, Taylor GA (2004) Disorders of the pediatric pancreas: imaging features. Pediatr Radiol 35(4):358–373
Johansson KA, Grapin-Botton A (2002) Development and diseases of the pancreas. Clin Genet 62:14–23
Rizzo RJ, Szucs RA, Turner MA (1995) Congenital abnormalities of the pancreas and biliary tree in adults. Radiographics 15:49–68 (quiz 147–148)
Skandalakis LJ, Rowe JS Jr, Gray SW, Skandalakis JE (1993) Surgical embryology and anatomy of the pancreas. Surg Clin North Am 73:661–697
Hamanaka Y, Evans J, Sagar G, Neoptolemos JP (1997) Complete pancreatic encasement of the proximal hepatic portal vein: a previously undescribed congenital anomaly. Br J Surg 84:785
Tani M, Onishi H, Kinoshita H et al (2004) The evaluation of duct-to-mucosal pancreaticojejunostomy in pancreaticoduodenectomy. World J Surg 29(1):76–79
Rau C, Candinas D, Gloor B (2003) Technique of pancreatic anastomosis. Swiss Surg 9:135–139
Sato N, Yamaguchi K, Chijiiwa K, Tanaka M (1998) Risk analysis of pancreatic fistula after pancreatic head resection. Arch Surg 133:1094–1098
Adam U, Makowiec F, Riediger H, Benz S, Liebe S, Hopt UT (2002) Pancreatic leakage after pancreas resection. An analysis of 345 operated patients. Chirurg 73:466–473
Buchler MW, Friess H, Wagner M, Kulli C, Wagener V, Z’Graggen K (2000) Pancreatic fistula after pancreatic head resection. Br J Surg 87:883–889
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marjanovic, G., Obermaier, R., Benz, S. et al. Complete pancreatic encasement of the portal vein—surgical implications of an extremely rare anomaly. Langenbecks Arch Surg 392, 489–491 (2007). https://doi.org/10.1007/s00423-006-0123-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-006-0123-8