Abstract
Background and aims
Recent results from long-term follow-up of a large number of patients who have undergone gastric resection for early gastric cancer (EGC) have not yet been fully evaluated.
Patients and methods
A total of 848 patients who had undergone gastric resection for EGC (262 female, 586 male; mean age 58.0 years; range 20–86 years) were studied with respect to surgical technique, long-term survival and prognostic factors on the basis of current TNM classification.
Results
Death related to recurrence occurred in only eight patients (0.9%). Hematogenous metastasis to the liver or bone represented the most common pattern of recurrence, developing in six of the eight recurrences (75%). The 5-year and 10-year cancer-related survival rates were 98.6% and 94.8%, respectively. The 5-year and 10-year overall survival rates were 95.2% and 85.0%, respectively. Lymph node metastasis represented an independent prognostic factor when analyzed on the basis of cancer-related survival.
Conclusion
The present findings indicate that long-term survival of patients who undergo gastric resection for EGC is extremely good and that lymph node metastasis represents an independent prognostic factor when analyzed according to cancer-related survival. Future developments for the treatment of EGC are expected to improve quality of life for patients after gastric resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies have shown that surgical resection produces good treatment results in patients with early gastric cancer (EGC), in both Japan and Western countries [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12]. However, recent results from long-term follow-up of a large number of patients who underwent gastric resection for EGC have not yet been fully evaluated. Rate of recurrence is reportedly low, and death from causes other than cancer recurrence is frequently observed in these patients [13, 14, 15, 16]. Reported long-term survival rates vary, due, in part, to differences in statistical methods between studies, as survival figures are influenced by the way deaths from causes other than recurrence are handled.
We present, herein, clinicopathological features, surgical techniques, survival figures and prognostic factors from long-term follow-up of a large number of patients who underwent gastric resection for EGC, including information regarding number of observed survivors and cause of death during the follow-up period. Based on the findings of the present study and other recent reports, we also discuss post-operative quality of life (QOL) for patients who undergo gastric resection for EGC.
Patients and methods
Patients
From June 1986 to May 1998, a total of 851 patients with EGC and no evidence of other malignancy underwent gastrectomy combined with lymphadenectomy at Kitasato University East Hospital, Japan. Of these, three deaths that were considered operation-related were excluded from the present analysis. The remaining 848 patients (262 female, 586 male; mean age 58.0 years; range 20–86 years) were enrolled in this study.
Clinicopathological factors were recorded, including type of gastrectomy, splenectomy, extent of lymphadenectomy, tumor size, location, macroscopic type, histopathological grading, depth of invasion and extent of lymph node metastasis. Among these factors, depth of invasion (Tis: carcinoma in situ, intra-epithelial tumor without invasion of lamina propria; or T1: tumor invasion of lamina propria or submucosa), extent of lymph node metastasis (N0: no regional lymph node metastasis; N1: metastasis in 1–6 regional nodes; N2: metastasis in 7−15 regional lymph nodes; N3: metastasis >15 regional nodes), distant metastasis (M0: no distant metastasis; M1: distant metastasis) and histopathological grading (G1: well differentiated; G2: moderately differentiated; G3: poorly differentiated) were determined according to TNM classifications [17]. For determination of TNM histopathological grading, papillary adenocarcinoma or well-differentiated tubular adenocarcinoma, as classified by the Japanese classification of gastric carcinoma (JCGC) [18], was considered G1; moderately differentiated tubular adenocarcinoma, classified by JCGC, was considered G2; signet ring cell carcinoma, poorly differentiated adenocarcinoma or mucinous carcinoma, classified by JCGC, was considered G3. In addition, extent of lymphadenectomy and macroscopic tumor type were reclassified according to the following guidelines, based on the JCGC. Limited lymphadenectomy was considered as incomplete dissection of second-tier nodes (D1 dissection), and extended lymphadenectomy as complete dissection of both first-tier and second-tier nodes (D2 dissection). Protruded and superficial elevated carcinomas were grouped together as elevated type, while superficial depressed carcinomas, excavated carcinomas and flat carcinomas were grouped together as depressed type. In the present patients, 91 (10.7%) displayed multiple simultaneous EGCs (85 double carcinomas, four triple carcinomas, two quadruple carcinomas). For such cases, the lesion that displayed the deepest level of invasion, or the largest diameter when multiple lesions had invaded to the same layer, was considered representative of all tumors.
Statistics
Postoperative course was reviewed for all patients and included patient records at outpatient clinics and cause of death in patients who had died during the follow-up period. Survival curves of all 848 patients were analyzed by Kaplan–Meier methods and log-rank tests. Median follow-up time for the 774 survivors was 77.7 months, and 566 survivors (73.1%) were followed ≥60 months after surgery. Cox’s proportional hazard model was used for multivariate analysis, and model selection was based on a forward stepwise procedure (adopted P value <0.05). Data were analyzed independently by either overall survival (cause of death not considered) or cancer-related survival (patients who died from causes other than recurrence were considered to be alive for the duration of the follow-up). Stat View software (version 5.0, SAS Institute, N.C., USA) was used for all statistical analyses, and values of P<0.05 were considered to be statistically significant.
Results
Clinicopathological features of all patients with EGC are shown in Table 1. Total gastrectomy was performed in 97 patients (11%), and splenectomy in 77 patients (9%). Extended lymphadenectomy was performed in 454 patients (54%). A total of 25,960 lymph nodes (mean 30.6 nodes/patient; range 1–136 nodes/patient) were dissected, and metastasis was histologically identified in 166 lymph nodes (0.6% of dissected nodes; mean 2.4 metastatic nodes/patient with lymph node metastasis; range 1–22 metastatic nodes/patient with lymph node metastasis). A total of 490 tumors (58%) was <30 mm in diameter; 731 (86%) were located in the distal two-thirds of the stomach, and 170 (20%) were elevated type. A histological diagnosis of G1 or G2 was made in 464 cases (55%) (340 G1 tumors,124 G2 tumors), while 384 tumors (45%) were classified as G3, 509 tumors (60%) as Tis and 339 tumors (40%) as T1. One patient had lymph node metastasis beyond regional nodes (M1), and another patient had liver metastasis (M1) at the time of gastrectomy. Except for these patients, curative resection was performed for all patients. Lymph node metastasis was seen in 69 patients (8%; 62 patients with N1 tumor; two patients with N2; one patient with N3; one patient with metastasis to distant nodes (M1); three unclassified patients). Stage grouping could not be classified by TNM in seven patients, as four patients had Tis tumors and lymph node metastasis, and ≥15 regional nodes were not dissected in another three patients with lymph node metastasis. Consequently, 505 patients were classified as stage 0, 273 as stage IA, 58 as stage IB, two as stage II, and three as stage IV, according to TNM classifications.
Death within 10 years after gastrectomy was observed in 70 patients. Table 2 shows cause of death in these patients. Death related to recurrence was found in only eight patients (11%), and survival time in patients who died from recurrence ranged between 11 and 117 months (mean 38.1 months). Most common cause of death after surgical resection was secondary malignancy in another organ (19 patients, 27%), followed by unknown cause (17 patients, 24%) and respiratory disease (11 patients, 16%). Table 3 shows clinicopathological findings for the eight patients who died from recurrence. Death related to recurrence was found not only in patients with T1 tumor, but also in patients with Tis tumor. Hematogenous metastasis to the liver or bone represented the most common pattern of recurrence and was found in six of the patients (75%) who died from recurrence.
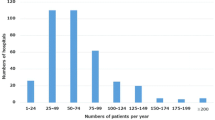
Figure 1 shows survival curves for the 848 patients who underwent gastrectomy for EGC. The 5-year and-10 year overall survival rates were 95.2% and 85.0%, respectively. The 5-year and-10 year cancer-related survival rates were 98.6% and 94.8%, respectively. Table 1 also shows results of univariate analysis of prognostic factors in patients who underwent gastrectomy for EGC. When analyzed using overall survival, significant differences in survival rate were found with respect to age (P<0.0001), gender (P=0.0190), tumor size (P=0.0163), macroscopic type (P=0.0010), histopathological grading (P=0.0100), depth of invasion (P=0.0008) and lymph node metastasis (P=0.0027). When analyzed using cancer-related survival, significant differences in survival rate were found with respect to depth of invasion (P=0.0411) and lymph node metastasis (P=0.0021).
Survival curves for 848 patients with early gastric cancer who underwent surgical resection. Curve a the 5-year and 10-year overall survival rates were 95.2% and 85.0%, respectively. Curve b the 5-year and 10-year cancer related survival rates were 98.6% and 94.8%, respectively. The number of patients eligible for analysis at each point is given
All 11 factors listed in Table 1 were examined by multivariate analysis using Cox’s hazard model. The results are shown in Tables 4 and 5. Multivariate analysis indicated that age (P<0.0001; relative risk 0.308), gender (P=0.0449; relative risk 0.059), tumor diameter (P=0.0361; relative risk 0.608), macroscopic type (P=0.0384; relative risk 1.664) and depth of invasion (P=0.0188; relative risk 1.747) represented independent prognostic factors when analyzed on the basis of overall survival. Only lymph node metastasis represented an independent prognostic factor (P=0.0081; relative risk 6.908) when analyzed on the basis of cancer-related survival.
Discussion
Post-operative recurrence has been reported as being relatively rare, occurring in 1.4–6.5% of patients with EGC [9, 14, 15, 16]. In the present study, death from recurrence was observed in only eight patients (0.9%) during the follow-up period. The most common pattern of recurrence was blood-borne metastasis, and prognosis of patients with recurrence was very poor, confirming previous reports on recurrence from EGC [9, 13, 14, 15, 16]. Most deaths were from unrelated causes, and death due to secondary malignancy in another organ was common, as reported elsewhere [13, 14, 15, 16]. These findings indicate that post-operative follow-up of other organs in patients who undergo gastric resection for EGC seems to be important for improving prognosis.
Previous studies have reported that the 5-year and 10-year overall survival rates are 70.0–82.8% and 70.4–77.3%, respectively [2, 6, 8], and that 5-year and 10-year cancer-related survival rates are 91.7–98.3% and 87.8–95.2%, respectively [1, 2, 4, 6, 14, 19]. The present results also showed excellent survival rates (5-year and 10-year overall survival rates: 95.2% and 85.0%; 5-year and 10-year cancer-related survival rates: 98.6% and 94.8%). Moreover, Farley et al. [2] demonstrated that the overall survival rate of patients with EGC was equivalent to that of an age-matched and gender-matched control population. These findings indicate that long-term survival of patients who undergo gastric resection is extremely good when analyzed according to cancer-related survival.
Using univariate analysis, several authors have identified lymph node metastasis [1, 4, 6, 7, 8, 14], macroscopic type [9], tumor size [6, 7, 9, 14], depth of invasion [3, 6, 7, 8, 9], age [2, 8, 14], lymph node dissection [4], DNA ploidy status [2], Eastern Cooperative Oncology Group (ECOG) score [2] and histological type [14], as important prognostic factors in patients who undergo gastric resection for EGC. In the present study, significant differences in survival rate were found with respect to age, gender, tumor size, macroscopic type, histological grading, depth of invasion and lymph node metastasis, when analyzed using overall survival. Significant differences were found with respect to lymph node metastasis and depth of invasion when analyzed using cancer-related survival. Previous multivariate analyses have demonstrated that depth of invasion [6], lymph node metastasis [4, 6, 11, 14], histological type [8, 11, 14], tumor size [6], lymph node dissection [4], DNA ploidy status [2], ECOG score [2] and age [8, 11], are independent prognostic factors that influence survival. In the present study, age, gender, tumor diameter and macroscopic type represented independent prognostic factors when analyzed on the basis of overall survival. However, only lymph node metastasis was an independent prognostic factor when analyzed on the basis of cancer-related survival. Treatment factors, including type of gastrectomy, splenectomy and lymph node dissection, were not found to be important factors influencing survival under either univariate or multivariate analysis. Comparison of results from previous studies and the present investigation with regard to prognostic factors is difficult, due to differences in statistical methods and patient populations. However, the present findings indicate that age is the most important factor when analyzed by overall survival, and that lymph node metastasis is an independent prognostic factor when analyzed by cancer-related survival.
Metastasis to the regional nodes is found in 9.1–20.1% of patients who undergo gastrectomy with lymph node dissection for EGC [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11]. Treatment results for EGC patients with lymph node metastasis are reportedly worse than for patients without lymph node metastasis [3, 6, 7, 8, 9]. Previous reports have demonstrated that most patients with lymph node metastasis are also curable by radical surgery, suggesting that metastasis to regional lymph nodes can be managed locally in this carcinoma [1, 3, 5, 6, 7, 8, 9, 10, 20]. However, the optimal extent of lymph node dissection for EGC remains controversial [4, 7, 12, 19, 21, 22, 23, 24, 25, 26]. Low incidence of lymph node metastasis and recurrence in EGC has led us to consider post-operative QOL by avoiding radical surgery. Recently, greater efforts have been made to improve post-operative QOL for patients with EGC by reducing the extent of gastrectomy (wedge resection, segmental resection) [27, 28, 29, 30], preserving the vagal nerve [28, 30, 31], conducting reconstruction with jejunal pouch interposition [31, 32, 33], and reducing abdominal wall destruction by using laparoscopic surgery [27, 34, 35]. Further developments for the treatment of EGC in these fields are expected to improve QOL after gastric resection in the future.
In conclusion, the findings of the present study indicate that long-term survival of patients who undergo gastric resection for EGC is extremely good, and that lymph node metastasis represents an independent prognostic factor when analyzed according to cancer-related survival. Future developments for the treatment of EGC are expected to improve QOL after gastric resection.
References
Folli S, Dente M, Dell’amore D, Gaudio M, Nanni O, Saragoni L, Vio A (1995) Early gastric cancer: prognostic factors in 223 patients. Br J Surg 82:952–956
Farley DR, Donohue JH, Nagorney DM, Carpenter HA, Katzmann JA, Ilstrup DM (1992) Early gastric cancer. Br J Surg 79:539–542
Moreaux J, Bougaran J (1993) Early gastric cancer: a 25-year surgical experience. Ann Surg 217:347–355
Miwa K, Miyazaki I, Sahara H, Fujimura T, Yonemura Y, Noguchi M, Falla R (1995) Rationale for extensive lymphadenectomy in early gastric carcinoma. Br J Cancer 72:1518–1524
Ito H, Oohara Y, Nakamura K, Nagata T, Mibu R, Nakayama F (1989) Complete ten-year post-operative follow-up of early gastric cancer. Am J Surg 158:14–16
Ranaldi R, Santinelli A, Verdolini R, Rezai B, Mannello B, Bearzi I (1995) Long-term follow-up in early gastric cancer: evaluation of prognostic factors. J Pathol 177:343–351
Lawrence M, Shiu MH (1991) Early gastric cancer: twenty-eight-year experience. Ann Surg 213:327–334
Guadagni S, Reed PI, Johnston BJ, Bernardinis GD, Catarci M, Valenti M, di Orio F, Carboni M (1993) Early gastric cancer: follow-up after gastrectomy in 159 patients. Br J Surg 80:325–328
Shiozawa N, Kodama M, Chida T, Arakawa A, Tur GE, Koyama K (1994) Recurrent death among early gastric cancer patients: 20-years’ experience. Hepatogastroenterology 41:244–247
Seto Y, Nagawa H, Muto T (1997) Impact of lymph node metastasis on survival with early gastric cancer. World J Surg 21:186–190
Maehara Y, Okuyama T, Oshiro T, Baba H, Anai H, Akazawa K, Sugimachi K (1993) Early carcinoma of the stomach. Surg Gynecol Obstet 177:593–597
Heesakkers JPFA, Gouma DJ, Thunnissen FBJM, Bemelmans MHA, Von Meyenfeldt MF (1994) Non-radical therapy for early gastric cancer. Br J Surg 81:551–553
Koga S, Kaibara N, Tamura H, Nishidoi H, Kimura O (1984) Cause of late post-operative death in patients with early gastric cancer with special reference to recurrence and the incidence of metachronous primary cancer in other organs. Surgery 96:511–516
Moriguchi S, Odaka T, Hayashi Y, Nose Y, Maehara Y, Korenaga D, Sugimachi K (1991) Death due to recurrence following curative resection of early gastric cancer depends on age of the patients. Br J Cancer 64:555–558
Furusawa M, Notsuka T, Tomoda H (1991) Recurrence of early gastric cancer. Semin Surg Oncol 7:344–350
Sano T, Sasako M, Kinoshita T, Maruyama K (1993) Recurrence of early gastric cancer: follow-up of 1475 patients and review of the Japanese literature. Cancer 72:3174–3178
Sobin LH, Wittekind C (2002) TNM classification of malignant tumors, 6th edn. Wiley, New York, pp 65–68
Japanese Research Society for Gastric Cancer (1995) Japanese classification of gastric carcinoma, 1st edn. Kanehara, Tokyo, pp 1–71
Tsujitani S, Oka S, Saito H, Kondo A, Ikeguchi M, Maeta M, Kaibara N (1999) Less invasive surgery for early gastric cancer based on the low probability of lymph node metastasis. Surgery 125:148–154
Kikuchi S, Sato M, Katada N, Sakuramoto S, Kobayashi N, Shimao H, Sakakibara Y, Kakita A (2000) Surgical outcome of node-positive early gastric cancer with particular reference to nodal status. Anticancer Res 20:3695–3700
Sowa M, Kato Y, Nishimura M, Kubo T, Maekawa H, Umeyama K (1989) Surgical approach to early gastric cancer with lymph node metastasis. World J Surg 13:630–636
Maekawa S, Takeo S, Ikejiri K, Anai H, Saku M (1995) Clinicopathological features of lymph node metastasis in early gastric cancer. Int Surg 80:200–203
Hayes N, Karat D, Scott DJ, Raimes SA, Griffin SM (1996) Radical lymphadenectomy in the management of early gastric cancer. Br J Surg 83:1421–1423
Yokota T, Saito T, Teshima S, Kikuchi S, Kunii Y, Yamauchi H (1998) Lymph node metastasis in early gastric cancer: how can surgeons perform limited surgery? Int Surg 83:287–290
Gotoda T, Sasako M, Ono H, Katai H, Sano T, Shimoda T (2001) Evaluation of the necessity for gastrectomy with lymph node dissection for patients with submucosal invasive gastric cancer. Br J Surg 88:444–449
Kunisaki C, Shimada H, Nomura M, Akiyama H (2000) Appropriate lymph node dissection for early gastric cancer based on lymph node metastases. Surgery 129:153–157
Ohgami M, Otani Y, Kumai K, Kubota T, Kim Y, Kitajima M (1999) Curative laparoscopic surgery for early gastric cancer: five years experience. World J Surg 23:187–193
Kodama M, Koyama K (1991) Indications for pylorus preserving gastrectomy for early gastric cancer located in the middle third of the stomach. World J Surg 15:628–634
Tomita R, Fujisaki S, Tanjoh K (2003) Pathophysiological studies on the relationship between postgastrectomy syndrome and gastric emptying function at 5 years after pylorus-preserving distal gastrectomy for early gastric cancer. World J Surg 27:725–733
Nomura E, Isozaki H, Fujii K, Toyoda M, Niki M, Sako S, Mabuchi H, Nishiguchi K, Tanigawa N (2003) Postoperative evaluation of function-preserving gastrectomy for early gastric cancer. Hepatogastroenterology 50:2246–2250
Tomita R, Fujisaki S, Tanjoh K, Fukuzawa M (2001) Operative technique on nearly total gastrectomy reconstructed by interposition of a jejunal J pouch with preservation of vagal nerve, lower esophageal sphincter, and pyloric sphincter for early gastric cancer. World J Surg 25:1524–1531
Kono K, Iizuka H, Sekikawa T, Sugai H, Takahashi A, Fujii H, Matsumoto Y (2003) Improved quality of life with jejunal pouch reconstruction after total gastrectomy. Am J Surg 185:150–154
Takeshita K, Saito N, Saeki I, Honda T, Tani M, Kando F, Endo M (1997) Proximal gastrectomy and jejunal pouch interposition for the treatment of early gastric cancer in the upper third of the stomach: surgical techniques and evaluation of postoperative function. Surgery 121:278–286
Shimizu S, Noshiro H, Nagai E, Uchiyama A (2003) Laparoscopic gastric surgery in a Japanese institution: analysis of the initial 100 procedure. J Am Coll Surg 197:372–378
Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y (2002) A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery 131:306–311
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kikuchi, S., Katada, N., Sakuramoto, S. et al. Survival after surgical treatment of early gastric cancer: surgical techniques and long-term survival. Langenbecks Arch Surg 389, 69–74 (2004). https://doi.org/10.1007/s00423-004-0462-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-004-0462-2