Abstract
Purpose
Whole-body thermal and hydration clamps were used to evaluate their independent and combined impact on the electrical activity of the brain. It was hypothesised that those stresses would independently modify the electroencephalographic (EEG) responses, with those changes being greater when both stresses were superimposed.
Methods
Alpha and beta spectral data (eyes closed) were collected from the frontal, central-parietal and occipital cortices of both hemispheres in resting, healthy and habitually active males (N = 8; mean age 25 years). Three dehydration states were investigated (euhydrated and 3% and 5% mass decrements) in each of two thermal states (normothermia [mean body temperature 36.3 °C] and moderate hyperthermia [38.4 °C]). The combination of those passively induced states yielded six levels of physiological strain, with the EEG data from each level separately examined using repeated-measures ANOVA with planned contrasts.
Results
When averaged across the frontal cortices, alpha power was elevated relative to the occipital cortices during moderate hyperthermia (P = 0.049). Conversely, beta power was generally reduced during hyperthermia (P = 0.013). Neither the alpha nor beta power spectra responded to dehydration, nor did dehydration elevate the heat-induced responses (P > 0.05).
Conclusion
Moderate hyperthermia, but neither mild nor moderate dehydration, appeared to independently alter brain electrical activity. Moreover, the combination of moderate hyperthermia with 5% dehydration did not further increase those changes. That outcome was interpreted to mean that, when those states were superimposed, the resulting neurophysiological changes could almost exclusively be attributed to the thermal impact per se, rather than to their combined influences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This communication comes from a large, multi-disciplinary investigation in which the independent and combined influences of dehydration (hypohydration) and moderate hyperthermia were explored using hydration and thermal clamping techniques. In an earlier manuscript, the effects on cognitive performance were reported (van den Heuvel et al. 2017), whilst the third contribution covers a broad range of other physiological responses (van den Heuvel et al. 2020). Herein, the influences of those stresses on the electrical activity of the brain, and in particular upon the alpha and beta power bands of the electroencephalogram, are described.
Evidence from both animal and human studies indicates that thermal strain and dehydration modify central nervous functions (Kiyatkin 2005; Kempton et al. 2011; Nakata et al. 2015; Wittbrodt et al. 2018), with the brain being especially vulnerable to changes in temperature (Becerra et al. 1999; Nunneley et al. 2002; Farrell 2016). Even small thermal disturbances, such as those occurring during sleep, circadian cycling and hibernation, may alter the electrical activity of the brain (Deboer 1998). Given the high dependency of neuronal function on the physical and chemical status of the central nervous system (Wilson and Morley 2003), as well as the integrity of the blood–brain barrier (Maughan et al. 2007), it is not unreasonable to suggest that dehydration-associated changes in the concentration (osmolality) and volume of the extracellular and intracellular fluid compartments may also have an impact on central neural structures and functions.
Indeed, significant body-fluid osmolality and volume changes can substantially influence brain anatomy (Sawka et al. 2015), with structural and functional modifications observed within both hyperthermic (Becerra et al. 1999; Nunneley et al. 2002) and dehydrated individuals (Duning et al. 2005; Kempton et al. 2009; Watson et al. 2010). Most recently, an elevation in cerebrovascular strain indices, including reduced cerebral blood flow, have been reported in humans during extended exercise in the heat, but without adverse cerebral metabolic changes (Trangmar et al. 2015), although blood-flow reductions in resting baboons seem not to occur (Hales et al. 1979). Collectively, those observations could be associated with states that modify brain electrical activity. Therefore, the focus of this experiment was to systematically explore possible thermal- and dehydration-induced alterations in brain electrical activity using a novel experimental design, in which passively modified thermal and hydration states were independently manipulated and clamped (van den Heuvel et al. 2017), thereby permitting an evaluation of their independent and combined effects.
Electroencephalography is one method through which brain electrical activity might be assessed. The resulting electroencephalograph (EEG) is a record of voltage generated by large ensembles of coherent, post-synaptic potentials. Given its strong temporal resolution, the method provides a capability for unambiguously differentiating among the functionally distinct frequencies of brain electrical activity. The method is distinguished from neural imaging techniques (such as functional magnetic resonance imaging and positron emission tomography) in that it can resolve the temporal coding of the brain, but it suffers relative to those methods in that it has a significantly inferior spatial resolution. It is important to note that few have studied EEG responses during these physiologically stressful states. Nevertheless, some investigators have reported significant resting-state EEG changes during both heat-induced physiological strain (Matthews et al. 1979; Dubois et al. 1980, 1981) and dehydration (Szinnai et al. 2005), as well as during their combined application (Nielsen et al. 2001; Nybo and Nielsen 2001).
From some of that research, it appeared that those stresses resulted in increased alpha and decreased beta power (Nielsen et al. 2001; Nybo and Nielsen 2001; Ftaiti et al. 2010). Those power bands refer to two discrete, EEG spectral bands (~ 8–13 and ~ 13–30 Hz, respectively), which have historically been assumed to index relaxed and attentive neural states (respectively). However, that interpretation has been shown to be an oversimplification, with the functional relation to each index being strongly dependent upon the specific task requirements. For example, alpha power can underlie a number of cognitive processes, ranging from a relaxed and unfocused state, through to the focussed attention resulting from the activation of a thalamo-cortical inhibitory network (see Cooper et al. 2006). Consequently, in the present paper, the authors did not attempt to interpret the functional significance of those EEG indices. Instead, the primary focus was on investigating the influences of moderate hyperthermia and dehydration on those power spectra.
Whilst others have investigated some aspects of those inter-related physiological challenges (Matthews et al. 1979; Dubois et al. 1980, 1981; Nielsen et al. 2001; Nybo and Nielsen 2001; Szinnai et al. 2005; Ftaiti et al. 2010), none of those experiments was designed to differentiate between their potentially independent influences on the EEG responses. For instance, hyperthermia and dehydration were induced using techniques such as passive heating, exercise and fluid deprivation. Moreover, the magnitude of those stresses was rarely controlled during data collection, EEG data collection was often restricted to specific cortical regions and confounding influences, such as arousal (Barry et al. 2007), were not necessarily considered. As a consequence, whilst it is broadly accepted that both of these stresses can modify central nervous function, as reflected within the electroencephalogram, which of those stresses might have the greater impact, and whether or not their combined application might further elevate changes in the electrical activity of the brain, remained uncertain.
Therefore, the emphasis of this experiment was to determine whether or not independent relationships existed between hyperthermia and dehydration, and their neurophysiological consequences. On separate occasions, three hydration states were induced (euhydration, 3% dehydration and 5% dehydration), based entirely upon body-mass changes, which were then clamped. When caloric balance is maintained, such mass changes provide a valid index of hydration state manipulation in resting individuals (Cheuvront and Montain 2017). The thermal status of participants was then modified between normothermia (mean body temperature: 36.3 °C) and moderate hyperthermia (38.4 °C), with those states also clamped throughout experimentation. Finally, the impact of each level of dehydration was evaluated within both of those clamped thermal states. Thus, six separate trials were completed, during which resting EEG data were recorded from the frontal, central-parietal and occipital cortices of both hemispheres, with absolute power in the alpha and beta spectral bands being determined. It was hypothesised that moderate hyperthermia in euhydrated individuals would affect both alpha and beta power, but perhaps not to the same extent, and possibly in opposite directions. Secondly, it was speculated that mild (3% mass decrement) and moderate (5%) dehydration would similarly increase alpha power, and reduce beta power, relative to the euhydrated state, with those changes being proportional to the level of dehydration. Finally, it was anticipated that the combination of hyperthermia and dehydration would produce a synergistic effect, resulting in electrical perturbations that would be greater than observed when those stresses were independently applied.
Methods
Participants
Eight non-smoking males without a history of heat illness were recruited (mean age 25 years [standard deviation (SD) 7], height 1.79 m [SD 0.08], body mass 74.3 kg [SD 8.8]). All participants were similarly and habitually active, with each person completing six experimental trials (labelled A–F). Those subjects were drawn from an initial pool of 17 individuals, nine of whom were excluded due to the presence of sub-clinical renal disease (N = 1), musculoskeletal injury (N = 1), inadequate visual acuity (N = 1) and very low, thermally induced sweat rates (N = 6). As this experiment also involved exploring the influences of heat strain and dehydration on cognitive performance (van den Heuvel et al. 2017), visual acuity was a pre-requisite for those cognitive challenges. All participants provided written, informed consent to procedures approved by a Human Research Ethics Committee (University of Wollongong; HE09/373) in accordance with the regulations of the National Health and Medical Research Council (Australia), and in compliance with the Declaration of Helsinki.
Procedures
Procedural overview
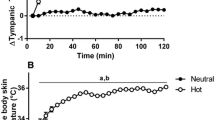
Participants completed six resting trials at the same time each day (within subjects), each with a different combination of the two experimental treatments (thermal- and hydration-state manipulations), and separated by at least 7 days to avoid thermal adaptation (Barnett and Maughan 1993). Dehydration was induced using intermittent, passive heating (warm-water immersion; van den Heuvel et al. 2017), and was defined by sweat-induced changes in the pre-experimental body mass. The three hydration targets were achieved using complete, partial and zero fluid replacement: euhydrated (normal body mass), 3% and 5% body-mass reductions (respectively). Once attained, those targets were clamped throughout subsequent thermal treatment and experimentation, using strictly controlled, isotonic-fluid administration. Within each hydration state, two whole-body thermal states were passively induced: normothermia (normal resting mean body temperature: 36.3 °C) and moderate hyperthermia (mean body temperature of 38.4 °C); those temperatures were measured during the EEG data collection (Fig. 1), and differ slightly from values reported in our companion paper (van den Heuvel et al. 2020), which were obtained during subsequent physiological data collection. The thermal states were also induced using whole-body water immersion, and, following the establishment of each hydration target, those targets were sustained during the thermal treatments. Once each thermal target was obtained, clamping was used to maintain stable mean body temperatures throughout testing, using an insulated water-perfusion garment.
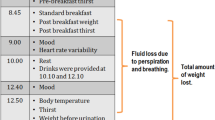
Experimental timeline (~ 9 h) showing all stages of every trial, which included three instrumentation phases (diagonally marked bars), two baseline data-collection periods (black bars), the preparatory dehydration and thermal treatments (bars with wave patterns), intermediate recovery and transfer phases (white bars), the hydration and thermal clamping durations (thick horizontal arrows), and finally the cognitive-function (van den Heuvel et al. 2017), electroencephalographic (EEG) and psychophysical data-acquisition period (rightmost black bar). This communication deals with EEG data collected from resting individuals. However, this was just one part of a multi-disciplinary study with neurophysiological and physiological data also collected during every trial. Those data are communicated in separate manuscripts (van den Heuvel et al. 2017, 2020), the latter of which included both resting and exercising states. For completeness, those data-collection periods are indicated by the grey bars beyond the second transfer period
The combination of those conditions provided six, physiologically unique trials: Trial A (normothermic and euhydrated); Trial B (normothermic and 3% dehydrated); Trial C (normothermic and 5% dehydrated); Trial D (moderately hyperthermic and euhydrated); Trial E (moderately hyperthermic and 3% dehydrated); and Trial F (moderately hyperthermic and 5% dehydrated; see Fig. 1a of van den Heuvel et al. 2020). Due to the need to individualise the dehydration protocol, a fully balanced experimental design was not possible, with four participants commencing with 5% dehydration, three completed 3% dehydration first and one commenced with the euhydration trial. However, the sequence of the hyperthermic and normothermic trials was balanced within each hydration state.
Familiarisation and standardisation
Pre-experimental screening, establishing the dehydration protocol for each participant and the recording of preliminary data, necessitated the completion of at least one familiarisation session. Some individuals required additional days to optimise the dehydration protocol, but all such days were completed at least four days before the first trial. Those pilot trials consisted of alternating water immersion (39–41 °C) with intermittent body-mass measurements (60–90-min intervals). The resulting mass changes enabled the determination of the optimal dehydration protocol for each individual. Three days prior to testing, participants commenced a drinking- and dietary-standardisation period, during which fluid intake and diet were controlled. The former required the consumption of 2 L of isotonic drink (provided by the investigators) between 06:00 and 18:00 h each day, with additional fluid consumption encouraged throughout the day. For the 12 h before each trial, strenuous exercise, alcohol and caffeine were avoided. Immediately prior to testing, subjects were instructed to eat an evening meal and breakfast high in carbohydrate and low in fat (not provided), to abstain from consuming dietary supplements and to drink an additional 500 mL of fluid (in any form) before retiring, and again with breakfast. Following the establishment of each hydration target, clamping was initiated by providing controlled volumes of an isotonic drink (sodium chloride at ~ 40 mmol L−1; Merson et al. 2008). Due to the length of each experimental day, subjects were also provided with mass-dependent servings of pre-selected foods at fixed time intervals.
Experimental protocol
Each trial followed an identical timeline (Fig. 1; ~ 9 h), with three instrumentation periods, two pre-experimental treatment phases (hydration and thermal [whole-body water immersion]), two baseline periods and an experimental stage. Participants arrived at the air-conditioned laboratory (20 °C) at 07:00 h, and hydration state was immediately checked. Two people initially failed the euhydration criterion (urine specific gravity < 1.021) and were tested on subsequent days. Participants donned a swimming costume, the first instrumentation period then commenced (deep-body temperature [auditory canal] and heart rate sensors), followed by the first baseline data collection. Individualised, passive dehydration followed immediately thereafter (treatment one; intermittent, supine water immersion [electronic winch]), but with body-fluid losses either fully replaced (euhydrated; Trials A and D), partially replaced with isotonic drinks (3% dehydration; Trials B and E) or not replaced at all (5% dehydration; Trials C and F). From that point onwards, those hydration targets were clamped using structured, isotonic-fluid administration (as described below), until each trial was completed.
Following the dehydration treatments, participants rested in the laboratory (2 h) to ensure thermal recovery back to the normothermic state and body-fluid equilibration (Maw et al. 2000), although it was assumed those fluid compartments would only be partially restored to their euhydrated state (Patterson et al. 2014). Additional deep-body (oesophageal and rectal) and skin temperature sensors, as well as EEG and electro-oculographic (EOG) electrodes were positioned and secured (instrumentation B). Six scalp electrodes were mounted within an elastic cap, four electrodes were attached to the facial surface, while an additional electrode was attached to the scalp over each mastoid. The second period of baseline data collection followed (baseline two, Fig. 1), whereupon the second (thermal) preparatory treatment commenced (continuous, seated water immersion [electronic winch]), using either of two water temperatures (normothermia: 34–35 °C; hyperthermia: 40–41 °C). To ensure that variations in the pre-experimental hydrostatic forces encountered during immersion did not introduce measurement artefacts (Stocks et al. 2004), the duration of the normothermic immersions matched those of the hyperthermic trials. Beyond that point, both the hydration and thermal states of every participant were clamped (Fig. 1). Representative body-tissue temperatures during this thermal treatment, and the subsequent data-collection stages, are presented in Fig. 2 of the companion manuscript (van den Heuvel et al. 2020).
To initiate thermal clamping, subjects were immediately transferred from the water tank to an adjacent climate-controlled chamber (5 m). A water-perfusion garment and thermally equilibrated, insulation clothing (firefighter thermal protective clothing) were donned, with the former being perfused with water (portable water bath and pump) at a temperature compatible with each thermal clamp. When thermally stable, the subject and ancillary equipment were transferred to a third air-conditioned laboratory (wheelchair: < 10 min). On arrival, the final instrumentation period commenced (electrophysiological indices: instrumentation C, Fig. 1), but now with the subject positioned in a comfortable chair, and with the water bath and pump operating (pump noise was barely distinguishable from background laboratory noise). A brief physiological stabilisation period followed, during which the thermal clamp was verified, electrical impedance was confirmed and the EEG traces were inspected, and checked to confirm appropriate responses to standard eye actions and movements (opening and closing, blinking, upward-downward movements and lateral movements). Following those verifications, resting EEG and EOG data were recorded, and psychophysical data were collected. After completing that data-collection block, subjects were transported back to the climate chamber (wheelchair), and, following a 20-min stabilisation period, they commenced a series of resting and exercising data-collection stages (Fig. 1; see van den Heuvel et al. 2020). At the end of each experiment, there was a supervised recovery, during which the final body mass was determined and a final urine sample was collected.
Manipulating and clamping whole-body hydration
This experiment was based on the combined assumptions that acute, whole-body water losses could be tracked from changes in body mass (Baker et al. 2009) and that, within the short term, corrections for variations in metabolism and respiratory gas exchanges would not be necessary (Montain and Cheuvront 2008). Moreover, under iso-caloric conditions, body-mass changes provide a valid surrogate for changes in hydration state (Cheuvront and Montain 2017).
The first experimental treatment involved three, passively induced hydration states (Fig. 1; euhydration, and 3% and 5% dehydration). Each treatment involved an identical whole-body immersion protocol (within subjects), and was achieved using repeated, supine immersions (5° head-toe declined litter with an electronic winch) in water regulated at 39–41 °C. Each participant had an individualised protocol, during which he was removed from the water for intermittent weighing, but also when the auditory canal temperature reached 38.5 °C. The latter was for subject comfort, with participants resting above the water, and recommencing immersion when that temperature had decreased to 37.5 °C. The total immersion duration averaged 185 min (range 137–242 min) across participants, and elicited near-maximal sweating, without undue discomfort. Individualised protocols were replicated in all subsequent trials. Once each dehydration target was achieved, hydration clamping was initiated, using isotonic fluids to prevent progressive mass reductions. Drinks were provided at the appropriate trial-specific, deep-body temperature every 15–20 min, with a 300 mL limit for any one drink. That procedure was developed through extensive pilot testing, and, in combination with intermittent weighing, resulted in successful hydration-state clamping.
Manipulating and clamping mean body temperature
The second pre-experimental treatment (seated, head-out immersion [electronic winch]) followed thermal recovery from the dehydration phase (2 h). The aim of treatment two was to either maintain normothermia (water temperature: 34–35 °C) or to induce moderate hyperthermia (water temperature: 40–41 °C), as reflected in the weighted summation of the deep-body and mean skin temperatures (mean body temperature). The respective mean body temperature targets were 36.5 and 38.5 °C, which were then clamped using a water-perfusion garment (Cotter et al. 1995; Cool Tubesuit, Med-Eng, Ottawa, Canada and pump: Delta Wing, Med-Eng, Ottawa, Canada; 325 mL min−1). In addition, subjects entered an adjacent, climate-controlled chamber, regulated at either 25 °C (normothermia) or 48 °C (hyperthermia), and immediately donned the thermally equilibrated clothing.
For the hyperthermic clamp, water pumped to the perfusion suit was initially heated to 50 °C (portable water bath: DC210, Med-Eng, Canada; water-bath pump and thermostat: GD120, Grant Instruments, U.K.; 17 mL min−1), as the water-cooled en route to the skin, and participants immersed both feet in 40 °C water (water bath: Type VFP, Grant instruments, U.K.). Body temperatures were closely monitored, and adjustments to heat storage were made by changing the perfusion-suit water flow, or by intermittently removing the feet from the water bath. In the normothermic trials, water in the suit was not heated, the pump was not activated and the feet were not immersed. Instead, participants wore running shoes to maintain local skin temperature.
Electrophysiological and physiological measurements
Electroencephalographic data acquisition
Electroencephalographic data were collected from electrodes positioned over the frontal (F3, F4), central-parietal (CP3, CP4) and occipital (O1, O2) cortices of both hemispheres, and from the right and left mastoids (Ag–AgCl electrodes: SynAmps2 Quick-Cap, Neuroscan, Compumedics Limited, Abbotsford, Australia), according to the international 10–20 system (Jasper 1958). Each scalp location was taken as a surrogate for the neural activity of the underlying cortical tissue. However, the electroencephalographic activity can also be recorded at sites far from their neural origins, although inferences drawn from those data can be problematic. Similarly, scalp locations cannot be taken to represent particular cognitive functions, making it necessary to perform dedicated research to determine the functional relevance of those spectra. Continuous electrical contact was sustained using the combination of conductance gel (NuPrep Skin Prep Gel, Weaver and Company, CO, U.S.A.) and an elasticised cap. Since sweating enhances electrical conductivity, no further preparations were required. That conductivity change does not have a significant, adverse impact on electroencephalographic activity (Kalevo et al. 2020).
Electroencephalographic data acquisition lasted 2 min, during which participants were seated and instructed to: ‘relax, try not to move too much, and close your eyes’ (Fig. 1). Instructions concerning this were provided in both written and spoken form, and were designed to ensure the uniformity of the bioelectrical status of every participant across all trials. Electrodes were grounded midway between Fz and FPz, and referenced midway between Cz and CPz. To monitor ocular artefacts, an electro-oculogram was recorded using electrodes placed above (E1) and below (E3) the left eye, and at the outer canthi of the left (E5) and right (E6) eyes. All electrode impedances were below 5 kΩ at the start of the recording. Both the EEG and EOG data were amplified with a gain of 1500, digitised at 500 Hz and filtered using a 0.05–40 Hz (24 dB/octave roll-off) bandpass filter (NuAmps, Neuroscan, Compumedics Limited, Abbotsford, Australia). Continuous EEG and EOG data were stored on the computer for subsequent analysis.
Physiological measurements
For the three days preceding every trial, participants were provided with portable scales (± 0.05 kg: A&D, Model UC-321, CA, U.S.A.) to record their post-void, preprandial body masses each morning. Those data were averaged to represent each individual’s baseline mass (Cheuvront et al. 2004). During each trial, semi-nude body mass was recorded during baselines one and two (Fig. 1), intermittently during dehydration and recovery, and immediately before and after each experimental stage (± 0.02 kg: A&D, Model Fw-150 k, CA, U.S.A.). Mid-stream urine specimens were collected in sterile containers upon arrival (Sarstedt Australia, Pty. Ltd., Ingle Farm, SA, Australia), during baselines one and two, and after completion of the experiment. Samples were also used to measure urine specific gravity (Clinical refractometer, Model 140, Shibuya Optical, Tokyo, Japan). In the accompanying manuscript (van den Heuvel et al. 2020), details are provided for the other surrogate indices of hydration state recorded during this experiment; body mass, urine specific gravity, urine and serum osmolality, and plasma-volume changes.
Deep-body temperature was estimated from the unweighted average of three indices: auditory canal, oesophageal and rectal temperatures. This approach yields a superior, thermometric estimation of whole-body heat storage (Taylor et al. 2014). Auditory canal temperature was measured during all preparatory and experimental phases; the former were monitored but not recorded. This temperature was measured within the external auditory meatus using an ear-moulded plug, with a protruding thermistor (Edale Instruments Ltd. Cambridge, UK), that was secured and insulated from the external environment (cotton wool). That method provides valid and responsive data (Todd et al. 2014), which, due to the vascular configuration of the tympanum and the auditory canal, enables rapid tracking of temperature changes within the central blood volume (Cooper et al. 1964; Hayward et al. 1984; Taylor et al. 2014). During the second instrumentation stage (Fig. 1), an oesophageal thermistor (Edale Instruments Ltd. Cambridge, UK) was inserted transnasally and positioned behind the heart (after Mekjavić and Rempel 1990). That index provides a superior surrogate of brain temperature (Taylor et al. 2014). A rectal thermistor (YSI type 401, Yellow Springs Instruments Co. Ltd., Yellow Springs, OH, U.S.A.) was positioned 10 cm beyond the anal sphincter (Lee et al. 2010).
Mean skin temperature was determined as an area-weighted summation of eight local temperatures (Hardy and DuBois 1938), with thermistors attached (single layer of waterproof tape) to the following sites (Type EU, Yellow Springs Instruments Co. Ltd., Yellow Springs, OH, U.S.A.): forehead, scapula, upper chest, lateral mid-upper arm, dorsal mid-forearm, dorsal hand, anterior mid-thigh and mid-calf. This skin index was then added to the average deep-body temperature using condition-specific, mixing coefficients (80% deep-body [normothermia] or 90% deep-body [hyperthermia]; Vallerand et al. 1992). All temperatures were sampled at 15-s intervals (1206 Series Squirrel, Grant Instruments Pty. Ltd., Cambridge, UK), with thermistors calibrated across the relevant physiological ranges (stirred water bath) and against a certified reference thermometer (± 0.05 °C; Dobros total immersion thermometer, Dobbie Instruments, Sydney, NSW, Australia).
Heart rates were monitored continuously (15-s intervals) from ventricular depolarisation (Polar S610i, Polar Electro Oy, Finland). Brachial systolic and diastolic blood pressures were measured using an automated monitor (Omron M6 Comfort, Omron Healthcare Co. Ltd., Kyoto, Japan) during baselines one and two (Fig. 1), and at the end of the experiment, with mean arterial pressure calculated as one-third systolic pressure plus two-thirds of the diastolic pressure.
Psychophysical indices
Subjective ratings of three psychophysical variables (thermal sensation, thermal discomfort and thirst sensation), as well as sleepiness, were collected at the end of baseline two, and following the neurophysiological data-acquisition periods (Fig. 1). Participants were provided with the relevant subjective scales prior to each trial, along with written and oral instructions. Thermal sensation was assessed using a 13-point, modified version of the Gagge scale (Gagge et al. 1967) ranging from unbearably cold (1) to unbearably hot (13). A modified Gagge discomfort scale (9 points: Gagge et al. 1967) was used to evaluate thermal discomfort (range: comfortable [1] to extremely uncomfortable [5]). Participants rated thirst sensation using another 9-point scale (Engell et al. 1987: not thirsty [1] to extremely thirsty [9]), whilst the Karolinska sleepiness scale (9-points: Åkersted and Gillberg 1990) was used to describe alertness or sleepiness during each trial (range: extremely alert [1] to extremely sleepy—fighting sleep [9]). Subjects also completed a visual analogue mood scale during baseline two (Bond and Lader 1974), and following EEG data acquisition. Three mood and mental-state classifications were evaluated (binary decisions): (i) alertness, which consisted of nine states (alert/drowsy, attentive/dreamy, energetic/lethargic, clear-headed/muzzy, well-coordinated/clumsy, quick-witted/mentally slow, strong/feeble, interested/bored, proficient/incompetent); (ii) calmness, with two states (calm/excited, relaxed/tense) and (iii) contentedness, as derived from five states (happy/sad, amicable/antagonistic, tranquil/troubled, contented/discontented, sociable/withdrawn).
Data analysis
Electroencephalographic analyses
Electroencephalographic data were analysed offline (Scan 4.5, Neuroscan, Compumedics Limited, Abbotsford, Australia). The vertical EOG was calculated as E1 minus E3, the horizontal EOG as E5 minus E6, and the radial EOG as the average of E1 and E3. Data were re-referenced to digitally linked mastoids, lowpass filtered at 30 Hz (12 dB/octave roll-off), EOG corrected (after Croft and Barry 2000), epoched into 2-s sweeps and DC-corrected. Automatic artefact rejection was then applied to all scalp channels, using a ± 100 µV rejection criterion. For each participant, average power spectra were calculated using fast-Fourier transforms with a 2-s cosine window. At each electrode, absolute power in the alpha (8–13 Hz) and beta bands (13–30 Hz) was calculated, with resultant values log transformed to improve distribution normality. Each power band was examined for differences associated with the hydration- and thermal-state treatments, as well as electrode topography (i.e., sagittal and lateral dimensions). For the sagittal dimension, EEG data were averaged for three regions separately: frontal (F3, F4), central-parietal (CP3, CP4) and occipital cortices (O1, O2). For the lateral dimension, EEG data were separately averaged for each hemisphere: left (F3, CP3, O1) and right (F4, CP4, O2).
Statistical analyses
For the electrophysiological data, repeated measures planned with contrasts (Analysis of Variance) were conducted to determine whether hyperthermia, dehydration or their combination affected EEG power as a function of scalp topography. Analyses were performed separately for the dependent variables (alpha and beta bands) using log-transformed data, but not the absolute values. The independent variables were mean body temperature (normothermia, hyperthermia), hydration state (euhydrated, 3% and 5% dehydrated), sagittal plane (frontal, central-parietal, occipital) and lateral plane (left and right hemispheres). Given the small sample size for research of this nature, only linear contrasts were used. Physiological and psychophysical data were analysed using two-way Analysis of Variance with repeated measures, followed by Tukey’s HSD post hoc tests to isolate sources of significant differences. Alpha was set at the 0.05 level for all statistical comparisons, with data reported as means and standard errors of the means ( ±), unless stated otherwise (SD).
Results
Verification of basal states and the pre-experimental treatments
Since the objective of this study was to systematically explore possible thermal- and dehydration-induced alterations in the electrical activity of the brain, it was crucial to firstly verify that the pre-experimental basal conditions (baseline one) were both physiologically normal and equivalent across trials. Secondly, it was essential to confirm that the hydration and thermal manipulations were successfully and uniformly achieved. As a consequence of extensive standardisation procedures, participants commenced every pre-experimental treatment in a euhydrated state (urine specific gravity < 1.021), with minimal inter-individual variability in the critical physiological variables across the six pre-experimental baseline periods (Table 1; all P > 0.05). Moreover, those data equated with values expected in healthy, resting adults (DuBois 1941; Taylor et al. 2014), permitting one to conclude that neurophysiological differences between the experimental conditions were wholly associated with normal physiological function, as influenced by the hydration and thermal treatments imposed during the pre-experimental treatments.
A second design objective centred around modifying, and then clamping, the hydration and thermal states, both independently and in combination. The dehydration protocol resulted in average body-mass losses, across both thermal states, that represented 0.4% (Trials A and D), 3.1% (Trials B and E) and 5.0% (Trials C and F) of each participant’s pre-experimental body mass, with those hydration levels differing significantly within each thermal state (Table 1; all P < 0.05). Fluid was principally lost as eccrine sweat, as opposed to renal flows, with significantly greater sweating during the hyperthermic conditions (Table 1; P < 0.05). The thermal targets were also successfully achieved using a combination of whole-body immersion and isothermal clamping (Table 1). Significant thermal differences within each hydration state were established for both the average deep-body and mean skin temperatures (Table 1; all P < 0.05), resulting in significantly different mean body temperatures, which averaged 36.3 °C in the normothermic trials (Trials A–C) and 38.4 °C in the hyperthermic conditions (Trials D–F; P < 0.05). In addition, none of the within-trial body masses differed significantly across those thermal states during hydration clamping (Table 1; P > 0.05). Finally, mean body temperature did not vary significantly during thermal clamping (Table 1; P > 0.05). Thus, these rigidly controlled experimental conditions resulted in distinctly different hydration and thermal states, thereby permitting one to assume that differences in EEG responses could be attributed to either their independent, or their combined neurophysiological influences.
Dehydration resulted in significant plasma-volume changes relative to the euhydrated, normothermic trial (A), averaging −8.9%, and −11.5% when normothermic participants were 3% and 5% dehydrated (Trials B and C respectively; both P < 0.05; Table 2 of van den Heuvel et al. 2020). When moderately hyperthermic, the respective changes were −20.9% and −21.9% (Trials E and F; both P < 0.05). When euhydrated, but moderately hyperthermic (Trial D), an average change of −13.9% was observed (P < 0.05). Readers are directed to the companion communication for data describing these and other physiological responses during the rest and exercise periods that immediately followed these tests.
Since neurophysiological responses are influenced by emotions and mood states (Segrave et al. 2012), relevant psychophysical variables were also evaluated during these experiments. As expected, participants reported feeling thermally neutral (range: 6.8–7.5) and comfortable (range: 1.1–1.6) when they were normothermic (Trials A–C), but hot (range: 10.0–10.6) and uncomfortable (range: 2.8–3.4) when moderately hyperthermic (Trials D–F; Table 1; P < 0.05). Furthermore, participants were moderately thirsty (range: 5.4–5.6) when 5% dehydrated (Trials C and F), and not thirsty (range: 1.3–1.9) when euhydrated (Trials A and D; Table 1; P < 0.05). Nevertheless, their state of alertness was unaffected by either of these thermal or hydration states (P > 0.05), nor were there any significant interactions among those psychophysical variables (P > 0.05). Across all possible comparisons, the only significant difference observed for changes in mood state was for the interaction between temperature and 3% dehydration under the classification of contentedness (P < 0.05).
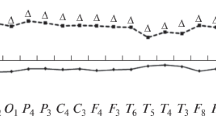
Neurophysiological influences of body temperature and hydration state
Power spectra calculated from the EEG recordings (eyes-closed) in the three hydration states (euhydrated, 3% and 5% dehydrated), and during both normothermia and moderate hyperthermia, are illustrated in Figs. 2 and 3. For clarity, only data from the frontal left site (F3) are illustrated, with all other electrode sites (i.e., F4, CP3, CP4, O1 and O2) following a very similar pattern. Indeed, each of the six electrode sites displayed power-spectrum functions typical of those reported in the literature (Barry et al. 2005; Curcio et al. 2005), with no clear separation evident between the six experimental conditions. Those data indicate that controlled changes in mean body temperature, hydration state or their combination had minimal impact on the electrical activity of the brain, at least as quantified within this experiment.
Mean power spectra calculated from 2-min EEG recordings at the frontal, left site (F3) in euhydrated (0%; solid), 3% dehydrated (dashed) and 5% dehydrated individuals (stippled) in both normothermic (grey) and moderately hyperthermic states (black; N = 8). Data were recorded during seated rest (eyes-closed)
Alpha power spectra
When log-transformed data were averaged across both hemispheres, alpha power was greater over the frontal than the occipital cortices (F[1,7] = 6.55; P = 0.038; partial eta2 = 0.48; Tables 2 and 3). When averaged across the three cortices, alpha power was higher over the right than the left hemisphere (F[1,7] = 27.74; P < 0.001; partial eta2 = 0.80; Tables 2, 3 and 4). However, there were no apparent interactions between those topographical patterns (F[1,7] = 1.04; P = 0.343; partial eta2 = 0.13).
Moderate hyperthermia (Trials D–F) did not significantly affect alpha power when log-transformed data from all sites were pooled (F[1,7] = 0.02; P = 0.895; partial eta2 < 0.01), nor was there evidence of an interaction of body temperature and laterality (F[1,7] = 0.37; P = 0.562; partial eta2 < 0.05; Tables 2, 3 and 4). Nevertheless, when averaged as a sagittal function, alpha power was elevated over the frontal cortices relative to the occipital cortices during whole-body heating (F[1,7] = 5.66; P = 0.049; partial eta2 = 0.45; Tables 2 and 3). A three-way interaction was also evident (F[1,7] = 14.34; P = 0.007; partial eta2 = 0.67), and this was believed to be due to moderate hyperthermia increasing alpha power frontally (Table 2), whilst simultaneously reducing power over the occipital cortex of the left (but not the right) hemisphere (Table 3).
Log-transformed alpha power did not vary with any of the changes in hydration state when all sites were pooled (F[1,7] = 0.14; P = 0.724; partial eta2 = 0.02), nor were there any interactions with hydration state or hemisphere (F[1,7] = 1.65; P = 0.240; partial eta2 = 0.19; Tables 2, 3 and 4). However, the sagittal pattern revealed that the greater alpha power in the frontal, relative to the occipital cortices, was reduced during dehydration (F[1,7] = 8.83; P = 0.021; partial eta2 = 0.56; Tables 2 and 3), although the interaction of the sagittal and lateral variations was not affected by dehydration (F[1,7] = 1.83; P = 0.218; partial eta2 = 0.21).
No interaction was apparent within the log-transformed alpha data between changes in mean body temperature and hydration state (F[1,7] = 1.34; P = 0.228; partial eta2 = 0.20). Furthermore, these combined treatments did not interact with the sagittal (F[1,7] = 0.14; P = 0.72; partial eta2 = 0.02), lateral (F[1,7] = 1.79; P = 0.222; partial eta2 = 0.20) or the sagittal-by-lateral contrasts (F[1,7] < 0.01; P = 0.996; partial eta2 < 0.01).
Beta power spectra
Beta power (log-transformed) was similarly larger over the frontal than the occipital cortices (F[1,7] = 15.48; P = 0.006; partial eta2 = 0.69; Tables 2 and 3), but did not differ as a function of hemisphere (F[1,7] = 2.70; P = 0.144; partial eta2 = 0.28). There was also no interaction between the sagittal and lateral planes (F[1,7] = 2.55; P = 0.154; partial eta2 = 0.27).
Unlike alpha power, the log-transformed beta power (for all sites combined) was reduced when subjects were moderately hyperthermic (Trials D-F; F[1,7] = 10.76; P = 0.013; partial eta2 = 0.61; Tables 2, 3 and 4). When combined with changes in the alpha band of the frontal cortices, those observations permit the partial acceptance of the first hypothesis. That thermal influence on beta power did not interact with variations in the sagittal plane (F[1,7] = 2.98; P = 0.128; partial eta2 = 0.30), the lateral plane (F[1,7] = 2.30; P = 0.646; partial eta2 = 0.03) or their interaction (F[1,7] = 1.32; P = 0.288; partial eta2 = 0.16). Beta power (log-transformed) was unresponsive to changes in hydration state (F[1,7] = 1.20; P = 0.311; partial eta2 = 0.15; Tables 2, 3 and 4), nor was there an interaction between hydration state and data from the sagittal plane (F[1,7] = 1.16; P = 0.318; partial eta2 = 0.14), the lateral plane (F[1,7] = 0.69; P = 0.435; partial eta2 = 0.09) or the sagittal-by-lateral plane interaction (F[1,7] = 0.59; P = 0.469; partial eta2 = 0.08). Accordingly, the second hypothesis was not accepted.
Finally, no interaction was apparent with beta power and the simultaneous manipulations of these thermal and hydration states (F[1,7] = 1.82; P = 0.222; partial eta2 = 0.20). Similarly, there was no interactive effect with the sagittal (F[1,7] = 0.47; P = 0.516; partial eta2 = 0.06), the lateral (F[1,7] = 3.18; P = 0.118; partial eta2 = 0.31) or the sagittal-by-lateral contrasts (F[1,7] = 0.92; P = 0.371; partial eta2 = 0.12). Thus, dehydration did not accentuate the EEG disturbances observed in these resting hyperthermic individuals, so the third working hypothesis was not accepted.
Discussion
This experiment was designed to evaluate thermal- and dehydration-induced alterations in neurophysiological function. Of particular interest were the potentially independent relationships between those physiologically stressful states and the electrical activity of the brain. The central outcome from this experiment was that the neurophysiological affects of moderate hyperthermia and dehydration were neither ubiquitously observed, nor were they uniformly expressed. Indeed, the current observations show that dehydration resulting in up to a 5% loss in body mass had, on its own (Trial C), minimal electrical impact in these resting individuals. Conversely, elevating the mean body temperature to 38.4 °C (moderate hyperthermia; Trial D) simultaneously elevated alpha power and reduced beta power over the frontal cortex, relative to the electrical activity observed during the normothermic and euhydrated state (Trial A). Readers are directed to other observations from this large experiment, which relate to changes in cognitive performance (van den Heuvel et al. 2017) and to a wide range of other physiological responses during rest and exercise (van den Heuvel et al. 2020).
Reductions in beta power accompanying heat strain have been reported previously (Nielsen et al. 2001; Nybo and Nielsen 2001; Ftaiti et al. 2010). In those studies, however, prolonged exhaustive exercise in the heat resulted in more severe hyperthermia (deep-body temperature > 39 °C), but less stressful dehydration (1–2% body-mass loss) than was induced in the current experiment. Moreover, it remained unclear whether those electrophysiological disturbances resulted from hyperthermia, the exercise stimulus, dehydration or physiological changes accompanying the combination of those non-steady-state conditions. For instance, exercise itself has been reported to modify brain electrical activity (Crabbe and Dishman 2004), though it remains unclear precisely how the exercise mode and intensity influence the EEG, and which cortical areas are affected (Brümmer et al. 2011; Moreas et al. 2011). As a consequence, the mechanistic utility of such observations required elucidation.
With that in mind, several unique design strategies were used to minimise various, potentially confounding influences. Firstly, physiologically normal basal states were established and verified prior to applying the experimental treatments, ensuring that the resulting differences could be wholly attributed to those treatments. Secondly, physiologically significant thermal and hydration states were separately elicited and then clamped throughout experimentation (Trials B–F), allowing for the evaluation of their independent and combined influences. Thirdly, EEG data were obtained with the eyes closed, thereby avoiding visual artefacts within those data. The resulting data support previous observations that the EEG power spectrum was altered during hyperthermia. Nevertheless, neither mild nor moderate dehydration appeared to independently influence either alpha or beta power, nor did their combination with moderate hyperthermia accentuate changes in the electrical activity of the brain.
Previous researchers have used the alpha–beta ratio as an index of fatigue (Nielsen et al. 2001; Nybo and Nielsen 2001; Ftaiti et al. 2010), with the rationale being that a decrease in beta, and an increase in alpha power would reflect reduced arousal. Although alpha activity did not significantly change during those experiments, the reduction in beta power was sufficient for the alpha–beta index to increase, which was interpreted to reflect decreased arousal at higher deep-body temperatures. However, it should be noted that, although the alpha–beta ratio does relate to arousal, it explains only a small portion of the variance in arousal (Barry et al. 2007), thereby complicating any EEG-based inferences regarding arousal state. Thus, although we comment here on the alpha–beta ratio, so that a comparison might be made with the existing literature, we do not believe that it is appropriate to interpret that ratio in terms of arousal without a more appropriate test of arousal (e.g., electrodermal activity). The alpha–beta index computed from the present data did not significantly change during the thermal manipulation (P > 0.05). This implies that moderate hyperthermia affects neither that ratio, nor the functions for which it may be a surrogate. Instead, it induces a more specific change in beta power in resting individuals.
The current experiment further allowed for the exploration of potential changes in the topographical distribution of the EEG power spectrum accompanying moderate hyperthermia and dehydration. Previous experiments of this nature have generally emphasised the frontal cortex within one lateral or one sagittal plane (e.g., Nielsen et al. 2001; Nybo and Nielsen 2001; Ftaiti et al. 2010). Whilst important, that design restricted the resulting electrical observations to those cortical areas only, preventing the attainment of a more comprehensive electrophysiological picture. Thus, it remained unknown whether the power spectral changes were caused by relatively discrete alterations in neural activity at the frontal cortex, within one anatomical plane, or whether they reflected more global neurophysiological effects.
Since EEG data in the current experiment were recorded over both hemispheres, and from three cortical regions of each hemisphere, a more detailed localisation of the accompanying electrical changes was made possible. Those data revealed that whole-body heating elevated both alpha and beta power in the frontal relative to the occipital sites, but only elicited changes in alpha power in the lateral dimension (left versus right). Furthermore, topographical alterations in alpha or beta power did not accompany either dehydration on its own, or the combination of those physiologically stressful states.
To our knowledge, this was the first experiment in which both thermal and hydration states were independently manipulated (Trials B–D), clamped and then combined (Trials E and F). That experimental rigour had two important outcomes. In the first instance, it minimised the between-subject variability, thereby elevating the capacity of the experimental design to yield physiologically meaningful data, against which the working hypotheses could be evaluated. Secondly, the time commitment for each participant was considerable (six trials lasting 8–10 h each), and that meant the sample size was necessarily modest. The implication of this is the possibility that the potential effects of these thermal and hydration manipulations, and particularly their interaction, might have been underestimated. That possibility warrants further investigation.
Conclusion
It is concluded that moderate hyperthermia (mean body temperature 38.4 °C), but neither mild (3% sweat-induced mass loss) nor moderate dehydration (5%) on their own, appeared to independently alter the electrical activity of the brain. This was demonstrated in thermally clamped individuals, with whole-body heating eliciting a generalised reduction in beta power, and discrete topographical elevations in alpha power. However, the combination of moderate hyperthermia with even the most dehydrated state, did not accentuate those changes in the EEG power spectrum. That outcome was interpreted to mean that, when both stresses are simultaneously present, changes in neurophysiological function can almost exclusively be attributed to the thermal impact per se, rather than to their combined influences.
Abbreviations
- EEG:
-
Electroencephalographic
- EOG:
-
Electro-oculographic
- E1, E3, E5 and E6:
-
Electrode positions above and below the left eye, and at the outer canthi of the left and right eyes (respectively)
References
Åkersted T, Gillberg M (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52:29–37
Baker LB, Lang JA, Kenney WL (2009) Change in body mass accurately and reliably predicts change in body water after endurance exercise. Eur J Appl Physiol 105:959–967
Barnett A, Maughan RJ (1993) Response of unacclimatized males to repeated weekly bouts of exercise in the heat. Br J Sports Med 27:39–44
Barry RJ, Clarke AR, Johnstone SJ, Magee CA, Rushby JA (2007) EEG differences between eyes-closed and eyes-open resting conditions. Clin Neurophysiol 118:2765–2773
Barry RJ, Rushby JA, Wallace MJ, Clarke AR, Johnstone SJ, Zlojutro I (2005) Caffeine effects on resting-state arousal. Clin Neurophysiol 116:2693–2700
Becerra LR, Breiter HC, Stojanovic M, Fishman S, Edwards A, Comite AR, Gonzalez RG, Borsook D (1999) Human brain activation under controlled thermal stimulation and habituation to noxious heat: an fMRI study. Magn Reson Med 41:1044–1057
Bond A, Lader M (1974) The use of analogue scales in rating subjective ratings. Br J Med Psychol 47:211–218
Brümmer V, Schneider S, Abel T, Vogt T, Strüder HK (2011) Brain cortical activity is influenced by exercise mode and intensity. Med Sci Sports Exerc 43:1863–1872
Cheuvront SN, Carter R, Montain SJ, Sawka MN (2004) Daily body mass variability and stability in active men undergoing exercise-heat stress. Int J Sport Nutr Exerc Metab 14:532–540
Cheuvront SN, Montain SJ (2017) Myths and methodologies: making sense of exercise mass and water balance. Exp Physiol 102:1047–1053
Cooper KE, Cranston WI, Snell ES (1964) Temperature in the external auditory meatus as an index of central temperature changes. J Appl Physiol 19:1032–1035
Cooper NR, Burgess AP, Croft RJ, Gruzelier JH (2006) Investigating evoked and induced electroencephalogram activity in task-related alpha power increases during an internally directed attention task. Neuro Rep 17:205–208
Cotter JD, Patterson MJ, Taylor NAS (1995) A method for clamping human skin and body core temperatures. Proc Aust Physiol Pharmacol Soc 26:204P
Crabbe JB, Dishman RK (2004) Brain electrocortical activity during and after exercise: a quantitative synthesis. Psychophysiology 41:563–574
Croft RJ, Barry RJ (2000) EOG correction of blinks with saccade coefficients: a test and revision of the aligned-artefact average solution. Clin Neurophysiol 111:444–451
Curcio G, Ferrara M, Moroni F, D’Inzeo G, Bertini M, De Gennaro L (2005) Is the brain influenced by a phone call? An EEG study of resting wakefulness. Neurosci Res 53:265–270
Deboer T (1998) Brain temperature dependent changes in the electroencephalogram power spectrum of humans and animals. J Sleep Res 7:254–262
DuBois EF (1941) The temperature of the human body in health and disease. In: American Institute of Physics. Temperature: its measurement and control in science and industry. Reinhold Publishing Corporation, New York, pp 24–40.
Dubois M, Coppola R, Buchsbaum MS, Lees DE (1981) Somatosensory evoked potentials during whole body hyperthermia in humans. Electroencephalogr Clin Neurophysiol 52:157–162
Dubois M, Sato S, Lees DE, Bull JM, Smith R, White BG, Moore H, Macnamara TE (1980) Electroencephalographic changes during whole body hyperthermia in humans. Electroencephalogr Clin Neurophysiol 50:486–495
Duning T, Kloska S, Steinsträter O, Kugel H, Heindel W, Knecht S (2005) Dehydration confounds the assessment of brain atrophy. Neurology 64:548–550
Engell DB, Maller O, Sawka MN, Francesconi RN, Drolet L, Young AJ (1987) Thirst and fluid intake following graded hypohydration levels in humans. Physiol Behav 40:229–236
Farrell MJ (2016) Regional brain responses in humans during body heating and cooling. Temperature 3:220–231
Ftaiti F, Kacem A, Jaidane N, Tabka Z, Dogui M (2010) Changes in EEG activity before and after exhaustive exercise in sedentary women in neutral and hot environments. Appl Ergon 41:806–811
Gagge AP, Stolwijk JAJ, Hardy JD (1967) Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res 1:1–20
Hales JRS, Rowell LB, King RB (1979) Regional distribution of blood flow in awake heat-stressed baboons. Am J Physiol 273:H705–H712
Hardy JD, DuBois EF (1938) Basal metabolism, radiation, convection, and vaporization at temperatures of 22 to 35 °C. J Nutr 15:477–497
Hayward JS, Eckerson JD, Kemna D (1984) Thermal and cardiovascular changes during three methods of resuscitation from mild hypothermia. Resuscitation 11:21–33
Jasper HH (1958) The ten-twenty electrode system of the International Federation. Electroencephalogr Clin Neurophysiol 10:371–375
Kalevo L, Miettinen T, Leino A, Kainulainen S, Korkalainen H, Myllymaa K, Töyräs J, Leppänen T, Laitinen T, Myllymaa S (2020) Effect of sweating on electrode-skin contact impedances and artifacts in EEG recordings with various screen-printed Ag/Agcl electrodes. IEEE Access 8:50934–50943
Kempton MJ, Ettinger U, Schmechtig A, Winter EM, Smith L, McMorris T, Wilkinson ID, Williams SCR, Smith MS (2009) Effects of acute dehydration on brain morphology in healthy humans. Hum Brain Mapp 30:291–298
Kempton MJ, Ettinger U, Foster R, Williams SCR, Calvert GA, Hampshire A, Zelaya FO, O’Gorman RL, McMorris T, Owen AM, Smith MS (2011) Dehydration affects brain structure and function in healthy adolescents. Hum Brain Mapp 32:71–79
Kiyatkin EA (2005) Brain hyperthermia as physiological and pathological phenomena. Brain Res Rev 50:27–56
Lee JY, Wakabayashi H, Wijayanto T, Tochihara Y (2010) Differences in rectal temperatures measured at depths of 4–19 cm from the anal sphincter during exercise and rest. Eur J Appl Physiol 109:73–80
Matthews WB, Read DJ, Pountney E (1979) Effect of raising body temperature on visual and somatosensory evoked potentials in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry 42:250–255
Maughan RJ, Shirreffs SM, Watson P (2007) Exercise, heat, hydration and the brain. J Am Coll Nutr 26:604S–612S
Maw GJ, Mackenzie IL, Taylor NAS (2000) Can skin temperature manipulation, with minimal core temperature change, influence plasma volume in resting humans? Eur J Appl Physiol 81:159–162
Mekjavić IB, Remple ME (1990) Determination of oesophageal probe insertion length based on standing and sitting height. J Appl Physiol 69:376–379
Merson SJ, Maughan RJ, Shirreffs SM (2008) Rehydration with drinks differing in sodium concentration and recovery from moderate exercise-induced hypohydration in man. Eur J Appl Physiol 103:585–594
Montain SJ, Cheuvront SN (2008) Fluid, electrolyte and carbohydrate requirements for exercise. In: Taylor NAS, Groeller H (eds) Physiological bases of human performance during work and exercise. Churchill Livingstone, Philadelphia, pp 563–573
Moreas H, Deslandes A, Silveira H, Ribeiro P, Cagy M, Piedade R, Pompeu F, Laks J (2011) The effect of acute effort on EEG in healthy young and elderly subjects. Eur J Appl Physiol 111:67–75
Nakata H, Oshiro M, Namba M, Shibasaki M (2015) Effects of passive heat stress on human somatosensory processing. Am J Physiol 309:R1387–R1396
Nielsen B, Hyldig T, Bidstrup F, González-Alonso J, Christoffersen GRJ (2001) Brain activity and fatigue during prolonged exercise in the heat. Plügers Arch 442:41–48
Nunneley SA, Martin CC, Slauson JW, Hearon CM, Nickerson LDH, Mason PA (2002) Changes in regional cerebral metabolism during systemic hyperthermia in humans. J Appl Physiol 92:846–851
Nybo L, Nielsen B (2001) Perceived exertion is associated with an altered brain activity during exercise with progressive hyperthermia. J Appl Physiol 91:2017–2023
Patterson MJ, Stocks JM, Taylor NAS (2014) Whole-body fluid distribution in humans during dehydration and recovery, before and after humid-heat acclimation induced using controlled hyperthermia. Acta Physiol 210:899–912
Sawka MN, Cheuvront SN, Kenefick RW (2015) Hypohydration and human performance: impact of environment and physiological mechanisms. Sports Medicine 45:S51–S60
Segrave RA, Thomson RH, Cooper NR, Croft RJ, Sheppard DM, Fitzgerald PB (2012) Emotive interference during cognitive processing in major depression: and investigation of lower alpha 1 activity. J Affect Disord 141:185–193
Stocks JM, Patterson MJ, Hyde DE, Jenkins AB, Mittleman KD, Taylor NAS (2004) Effects of immersion water temperature on whole-body fluid distribution in humans. Acta Physiol Scand 182:3–10
Szinnai G, Schachinger H, Arnaud MJ, Linder L, Keller U (2005) Effect of water deprivation on cognitive-motor performance in healthy men and women. Am J Physiol 289:R275–R280
Taylor NAS, Tipton MJ, Kenny GP (2014) Considerations for the measurement of core, skin and mean body temperatures. J Therm Biol 46:72–101
Todd G, Gordon CJ, Groeller H, Taylor NAS (2014) Does intramuscular thermal feedback modulate eccrine sweating in exercising humans? Acta Physiol 212:86–96
Trangmar SJ, Chiesa ST, Llodio I, Garcia B, Kalsi KK, Secher NH, González-Alonso J (2015) Dehydration accelerates reductions in cerebral blood flow during prolonged exercise in the heat without compromising brain metabolism. Am J Physiol 309:H1598–H1607
Vallerand AL, Savourey G, Hanniquet A, Bittel JHM (1992) How should body heat storage be determined in humans: by thermometry or calorimetry? Eur J Appl Physiol 65:286–294
van den Heuvel AMJ, Haberley BJ, Hoyle DJR, Taylor NAS, Croft RJ (2017) The independent influences of heat strain and dehydration upon cognition. Eur J Appl Physiol 117:1025–1037
van den Heuvel AMJ, Haberley BJ, Hoyle DJR, Croft RJ, Peoples GE, Taylor NAS (2020) Hyperthermia and dehydration: their independent and combined influences on physiological function during rest and exercise. Eur J Appl Physiol. https://doi.org/10.1007/s00421-020-04493-4
Watson P, Head K, Pitiot A, Morris P, Maughan RJ (2010) Effects of exercise and heat-induced hypohydration on brain volume. Med Sci Sports Exerc 42:2197–2204
Wilson MM, Morley JE (2003) Impaired cognitive function and mental performance in mild dehydration. Eur J Clin Nutr 57:S24–S29
Wittbrodt MT, Sawka MN, Mizelle JC, Wheaton LA, Millard-Stafford ML (2018) Exercise-heat stress with and without water replacement alters brain structures and impairs visuomotor performance. Physiol Rep 6:e13805
Acknowledgements
AMJvdH held an Australian Post-Graduate Award from the University of Wollongong (Australia) throughout this investigation. NAST was supported during the writing of this manuscript by the Brain Pool Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science and Information, Communication and Technology (Grant number: 2019H1D3A2A01061171). No other funding was provided by agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AMJvdH, NAST and RJC designed and planned this research, and were involved in data analysis and all phases of manuscript preparation. AMJvdH ran the experiments, and was also responsible for data collection. BJH and DJRH were essential participants in subject preparation, data collection, laboratory operations and manuscript preparation. NAST supervised the thermal physiological aspects of this project, whilst RJC was responsible for the neurophysiological methods. All authors read and approved the final version of the manuscript and its submission for publication, and agree to be accountable for this work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All persons designated as authors qualify for authorship, and all those who qualify for authorship have been listed as authors.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Additional information
Communicated by George Havenith.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van den Heuvel, A.M.J., Haberley, B.J., Hoyle, D.J.R. et al. Hyperthermia, but not dehydration, alters the electrical activity of the brain. Eur J Appl Physiol 120, 2797–2811 (2020). https://doi.org/10.1007/s00421-020-04492-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-020-04492-5