Abstract
Purpose
To assess whether stepping-based weight bearing exercise (WBE) can elicit peak activation of upper leg muscles similar to resistance exercise (RE) at an intensity required to induce strength gains in elderly women.
Methods
Muscular activation of several upper leg muscles was measured during RE and WBE in a cohort of 19 healthy elderly women (69.3 ± 3.4 years). WBE consisted of forward and lateral stepping with step heights of 10, 20 and 30 cm. Muscular activation was compared to 60% of one-repetition maximum (1-RM) of congruent RE.
Results
Peak activation during WBE was higher than RE at 60% 1-RM during forward and lateral stepping in vastus lateralis starting at 20 cm (p = 0.049 and p = 0.001), and biceps femoris at 30 cm step height (p = 0.024 and p = 0.030). Gluteus maximus peak activation matched RE at 60% 1-RM at 20 and 30 cm step height regardless of step direction (p ≥ 0.077). Peak activation of the rectus femoris and gluteus medius matched RE activation at 60% 1-RM during lateral stepping at 30 cm (p = 0.355 and p = 0.243, respectively) but not during forward stepping. WBE did not induce similar activation as RE in the semitendinosus.
Conclusion
In WBE, most upper leg muscles were recruited at an equal or higher intensity than in RE at 60% 1-RM. Lateral stepping at 30 cm step height showed the highest training potential of all WBE’s applied.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia is defined as the age-related loss of muscle mass and strength (Rosenberg 1997) and is one of the leading causes of falls (Pijnappels et al. 2008) and functional impairment in elderly (Liu and Latham 2009; Van Roie et al. 2011). However, engaging in physical activity can ameliorate the debilitating effects of sarcopenia on functional performance and mobility (Montero and Serra 2013). Even though muscle mass and strength will inevitably decline over time, muscle plasticity is rather well preserved (Hakkinen et al. 2000; Liu and Latham 2009; Montero and Serra 2013). This ability has been demonstrated in ages ranging up to 85 (Liu and Latham 2009; Sundell 2011; Montero and Serra 2013). Consequently, over the past decade, a plethora of exercise types have been suggested to preserve functional performance in elderly. Among these, resistance exercise (RE) has generally been indicated as the most effective way to induce gains in muscle mass and strength (Sherrington et al. 2011; Cederholm et al. 2013).
Muscle strength is a strong predictor of functional performance in elderly (Pijnappels et al. 2008; Cawthon et al. 2014) and several studies have shown that strength gains from RE can translate into functional improvements (Bean et al. 2009; Liu and Latham 2009). However, Bean et al. (2009) found that functional improvements were only achieved in a subset of studies with appropriate RE task-specificity, but not in those studies that lacked RE task-specificity, indicating that strength is just one of the determinants of functional ability and balance performance (Cress et al. 1996; Manini et al. 2007; Donath et al. 2015). On a motivational level, RE participation in elderly appears to be limited. For example, data from the 2015 National Health Interview Survey (USA) show that only 15.2% of females between 65 and 74 years old met the federal physical activity guidelines when resistance training was taken into account (Ward et al. 2016). In addition, van Roie et al. (2015) have found that it is difficult to maintain exercise adherence to RE in this population. With limited participation and adherence, it is questionable whether RE is viable as a long-term training method for elderly.
Therefore, several researchers have recently directed their focus at more functional training modalities, stating that exercise protocols aiming to combat functional decline in elderly cannot be based solely on open kinetic chain RE. Alternatively, closed kinetic chain RE’s such as the leg press appear to be more functional since they involve multi-joint movement and are considered to be safer than open kinetic chain RE (Bunton et al. 1993; Begalle et al. 2012). However, training modalities to improve the performance of everyday tasks and to prevent falls should also focus on functional parameters such as balance maintenance and coordination (Donath et al. 2015). A shift towards more functional training is supported by findings that neuromuscular adaptations in elderly appear to be highly task-specific (Manini et al. 2007; Bice et al. 2011). In fact, several studies have demonstrated the efficacy of task-specific training for elderly (Manini et al. 2007; Bean et al. 2009; Pedersen et al. 2015).
One type of exercise that incorporates essential functional components for the performance of everyday tasks, such as balance performance and muscular coordination, is weight bearing exercise (WBE). WBE is characterized by a certain degree of vertical impact relatable to activities of daily life, such as normal gait, stair-navigation, stepping and jumping. Due to its large degree of task-specificity and incorporation of balance maintenance, stepping-based WBE could serve as a useful training modality to improve functional ability and strength. In a systematic review on fall prevention in elderly, Sherrington et al. state that ‘exercise must provide a moderate or high challenge to balance’ by reducing the base of support, involving movement of the center of gravity and reducing the need for upper limb support (Sherrington et al. 2011). Stepping exercise incorporates all three of these balance challenging elements and may, therefore, help when training to prevent falling incidents.
Ideally, exercises that aim to improve functional performance and decrease falling incidents in elderly should incorporate both strengthening and task-specific components to achieve optimal effectiveness (Kraemer et al. 2001). It is conceivable that WBE may also lead to muscle strength gains, but unfortunately it remains unknown whether stepping exercise can provide a sufficient training stimulus, because little research has been done to compare WBE with RE’s known to improve muscle strength. Due to the mechanically complex nature of WBE (Anderson and Behm 2005), the mechanical indeterminacy of muscle-joint-systems and the inability to measure muscle forces without the use of invasive procedures it is hard to compare these exercise types based on muscle output (Staudenmann et al. 2010). Alternatively, muscle activation as measured with surface electromyography (sEMG) can provide some fundamental knowledge on the potential training stimulus that WBE can provide compared to RE.
The current study aimed to compare muscle activation of several major upper leg muscles of elderly women during WBE, and RE at 60% of one-repetition maximum (1-RM). This intensity of 60% of 1-RM for RE was selected as a reference since it is established as the threshold for strength gains in untrained adults by the American College of Sports Medicine (American College of Sports Medicine 2017). By establishing the relative activation during each WBE to activation obtained during a maximal contraction, the strengthening potential for each muscle can be inferred (Boren et al. 2011). The definition of 60% 1-RM as the critical threshold for strength gains is further supported by a review from Macadam et al. (2015) and meta-analysis by Schoenfeld (2013). For elderly this threshold is less clearly defined. According to recent research the relative threshold for muscular gains is likely lower for older adults than young adults (Van Roie et al. 2013; Schoenfeld et al. 2014; Fisher et al. 2016). However, in the absence of a clearly defined threshold for strength gains in elderly we maintained the established peak activation of 60% 1-RM as the reference baseline.
The main goals were (1) to determine whether WBE can elicit peak activation levels sufficient to surpass the threshold for strength gains in this population and (2) how training characteristics, such as step height and step direction, affect peak activation levels. We hypothesized that stepping-based WBE at step heights of 20 and 30 cm could elicit peak muscular activation similar to, or higher than RE at 60% of a 1-RM. Additionally, we assessed the timing of peak activation for each muscle and made additional comparisons with results from closed kinetic chain resistance exercise to support our findings.
Materials and methods
Subjects
Twenty-two healthy, community-dwelling elderly women were recruited through posters at various social activities for elderly in Leuven (Belgium). Exclusion criteria, stated on the recruitment material and confirmed by a questionnaire, were diagnosed osteoarthritis of the lower limbs, hip, knee or ankle prosthetics, a history of mental disorders, balance disorders, brain injuries, and recurring dizziness. Three participants dropped out between the familiarization and testing session. One sustained a sprained ankle in the week following familiarization and two did not wish to disclose their reason for dropping out. The average age of the remaining nineteen subjects was 69.1 years (± 3.1).
This study was approved by the Human Ethics Committee of KU Leuven in accordance with the Declaration of Helsinki. All subjects provided signed informed consent prior to participation.
Familiarization and 1-RM testing
A flowchart of the study protocol is provided in Fig. 1. All subjects attended an individual familiarization session, during which they performed all RE’s at least three times at low intensity. After familiarization, individual 1-RM for each RE was estimated in accordance with methods employed by Brzycki (1993) where five-repetition maximum (86% 1-RM) was the minimum intensity used for estimation. Estimation of 1-RM was chosen since some population groups such as sedentary elderly might experience difficulty to maximally exert themselves during direct 1-RM measurements (Wood et al. 2002). Based on the estimated 1-RM, the external loads corresponding with the predetermined resistance levels (40, 60 and 80%, respectively) for each RE were calculated. Familiarization occurred at least 1 week prior to testing to avoid any effects of fatigue.
Weight bearing and resistance exercise
On the testing day, the subjects were fitted with electrodes on the dominant leg to record sEMG. Left–right leg dominance was established by asking the participants with which foot they would kick a ball. sEMG was recorded from the vastus lateralis (VL), rectus femoris (RF), biceps femoris (BF), semitendinosus (ST), gluteus maximus (GMAX) and gluteus medius (GMED). Before electrode placement the skin was shaved and thoroughly rubbed with an alcohol swab. Electrodes (Ambu® BlueSensor P Ag/Ag–Cl electrodes, Ballerup, DK) were placed on the belly of the muscles with an inter-electrode distance of 10 mm. Subjects then performed a warm-up of 5 min cycling on a cycle ergometer at 70–80 rpm at a preferred resistance. The subjects were fitted with 50 retro-reflective markers (Giarmatzis et al. 2017) to record kinematics during the dynamic trials with 3D motion capturing (Vicon®, Oxford Metrics, Oxford, UK). Subjects were randomly assigned to perform either WBE or RE first, followed by RE and WBE, respectively. The WBE protocol consisted of forward stepping (Fstep) and lateral stepping (Lstep) onto and off wooden blocks with heights of 10, 20 and 30 cm, respectively. For safety reasons, subjects were allowed to place their hand on a support bar during lateral stepping, without gripping the bar to avoid any force being applied by the hand during ascent. Every trial was performed twice to ensure at least one trial with proper recording of the EMG signals. The RE protocol consisted of five open kinetic chain exercises and one closed kinetic chain exercise. The open kinetic chain exercises included a seated knee extension, knee flexion in prone position, standing hip extension, standing hip flexion and standing hip abduction performed with a cable jungle (Technogym®, Gambettola, IT), adapted to simulate RE in a common gym setting. A seated unilateral leg press was included as a closed kinetic chain exercise. During the RE trials subjects performed three repetitions at each intensity (40, 60 and 80% of 1-RM, respectively) to ensure recording of at least one full cycle from lifting the weight stack to returning the weight stack to starting position. Both RE and WBE were performed at a controlled speed guided by verbal feedback (one second concentric and one second eccentric contraction for RE and one second ascent for WBE).
Data collection
All measurements were performed at the Movement and posture Analysis Laboratory Leuven (MALL). Muscle activation was measured with sEMG through a telemetric system (Aurion®, ZeroWire, Milan, IT) at a sampling frequency of 1000 samples/s. Kinematics were recorded with a 3D motion capturing system (10–15 MX camera system; Vicon®, Oxford Metrics, Oxford, UK) sampled at 100 samples/s to establish start and end of each exercise. The raw sEMG signals were high-pass filtered with a first order Butterworth filter with a cut-off at 20 Hz (De Luca et al. 2010; Staudenmann et al. 2010), full-wave rectified and smoothed with a 0.1-s moving average. The resulting signals were then normalized to the maximal dynamic output obtained during the muscle specific RE (Hodder and Keir 2013) which, due to the difficulties of elderly to perform maximal dynamic contractions (Klass et al. 2007), was recorded at an intensity of 80% 1-RM (Staudenmann et al. 2010), before establishing peak activation per trial. Normalization to a dynamic maximum (1-RM) was chosen over normalization to an isometric maximal voluntary contraction (iMVC) since iMVC-normalized data resulted in higher inter-subject variation, which was in line with findings by Burden (2010). For the WBE trials, the time-normalized sEMG curves were plotted against the vertical displacement of the pelvis (represented by a marker on the sacrum) to detect during which phase of stepping peak activation occurred in each muscle.
Baseline determination
To provide a meaningful assessment of WBE as a training modality we employed a comparison with the American College of Sports Medicine-established threshold for muscle strength gains in RE for untrained adults, which is ≥ 60% of 1-RM (Schoenfeld 2013; American College of Sports Medicine 2017).
Statistical analysis
All processing was performed with MATLAB R2014b (MathWorks®, Natick, USA). Statistical analysis was performed with SPSS (IBM® SPSS v23 Statistics for Windows, Armonk, USA). The data were tested for normality with a Kolmogorov–Smirnov test. Since the assumption of normality was violated, overall significance of differences between each exercise, intensity and the reference exercise at baseline (60% 1-RM) were determined by means of a Friedman test. If an overall significant difference (p < 0.05) was found, a Wilcoxon signed rank test was performed to determine differences in peak sEMG of the individual muscles between each WBE and the baseline. Comparisons were made between each exercise intensity and the relevant baseline RE for that muscle (knee extension for VL and RF, knee flexion for BF and ST, hip extension for GMAX and hip abduction for GMED). Additional comparisons were made between corresponding intensities of each open kinetic chain RE and leg press.
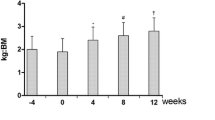
Results
Only data from the ascent phase of stepping was analyzed since none of the recorded sEMG signals during descent were able to match or surpass those obtained during RE at 60% 1-RM. Positive dose–response relationships were found between exercise intensities (step height in WBE and percentage of 1-RM in RE) and peak sEMG amplitude for each muscle (Fig. 2). Below, we report muscular activation during WBE (Fstep and Lstep) and leg press, in comparison to the baseline of the most relevant RE, separately for each muscle group. An overview of the exercises that showed similar or significantly higher peak activation than the baseline can be found in Table 1.
Peak sEMG amplitudes during Fstep, Lstep and Leg Press at 3 different intensities compared to baseline activation (60% 1-RM) of the congruent RE (knee extension for quadriceps, knee flexion for hamstrings, hip abduction for gluteus medius and hip extension for gluteus maximus) indicated by ↓, †significantly lower activation, *significantly higher activation
Quadriceps
For the VL, the baseline RE was knee extension. Fstep at 10 cm elicited a significantly lower maximal activation than the baseline (p = 0.035), while Fstep at 20 and 30 cm elicited significantly higher activation levels (p = 0.049 and p = 0.002, respectively) than the baseline. Lstep at 10 cm step height showed no significant difference with the baseline (p = 0.723) and at 20 and 30 cm heights, significantly higher activation was recorded (p = 0.001 for both). When each intensity of the leg press was compared to the corresponding intensity of knee extension, a significant difference was found between both exercises at 40% 1-RM (p = 0.013) but not at 60 and 80% 1-RM (p > 0.05 for both). For the RF, knee extension was also used as the baseline RE. Forward stepping elicited significantly lower activation of the RF than the baseline at all step heights (p < 0.001 for 10 and 20 cm and p = 0.024 for 30 cm). Lateral stepping elicited higher activation than forward stepping at the same step heights. However, 10 and 20 cm step height elicited lower activation than the baseline (p < 0.001 and p = 0.044, respectively). Only lateral stepping at 30 cm elicited similar activation to the baseline (p = 0.355). Comparisons between the corresponding intensities of leg press and knee extension also showed consistently higher activation of the RF during knee extension (p < 0.01).
Hamstrings
For both hamstrings, the baseline exercise was knee flexion. In the ST, none of the stepping exercises or leg press intensities elicited similar or higher activation than the baseline (p < 0.001). However, in the BF all stepping exercises produced similar or higher activation than the baseline. Both forward and lateral stepping at 10 and 20 cm elicited similar peak activation to knee flexion (p > 0.05 for all). Both stepping directions at 30 cm step height elicited significantly higher activation (p = 0.024 for Fstep and p = 0.030 for Lstep). All leg press exercises resulted in similar activity as their corresponding knee flexion intensity (p > 0.05).
Gluteus maximus
For GMAX the baseline exercise was hip extension. A step height of 10 cm elicited significantly lower activation than the baseline during forward and lateral stepping (p = 0.040 for Fstep and p = 0.004 for Lstep). However, similar activation to the baseline was elicited at step heights of 20 and 30 cm (p > 0.05 for both stepping directions). When compared to their corresponding hip extension intensity, all leg press intensities resulted in significantly lower activation (p < 0.05).
Gluteus medius
The baseline exercise for the GMED was hip abduction. Fstep at 10 cm showed similar activation to the baseline (p = 0.077), however, Fstep at 20 and 30 cm both elicited significantly lower activation (p = 0.004 and p = 0.024 respectively). Lstep at 10 cm and 30 cm showed similar activation to the baseline (p = 0.070 and p = 0.243 respectively), while Lstep at 20 cm showed significantly lower activation (p = 0.044). All leg press intensities produced significantly lower activation than their corresponding hip abduction intensities (p < 0.001 for all intensities).
Timing of peak activation
Figure 3 shows the muscular activation patterns of one representative subject during ascent and descent for Fstep and ascent for Lstep at 30 cm step height. Peak activation occurs during the ascent phase of both stepping directions for all muscles except the ST. The ST shows clear peak activation during the final phase of descent during forward stepping and several peaks over the whole step cycle during lateral stepping with the maximal peak occurring during the final phase of double support. Because lateral stepping is a less common task during activities of daily life, lateral stepping ascent and descent were recorded separately to allow for more standardized trial execution. Peak activation during descent did not surpass activation obtained during ascent and was, therefore, left out of further analyses.
EMG output of VL, RF, ST, BF, GMAX and GMED muscles of one representative subject during ascent and descent of Fstep at 30 cm (a) and ascent of Lstep at 30 cm (b). Group average % of step cycle at which peak activation for each muscle occured in depicted by a dot. Step cycle phases are depicted by vertical displacement of the pelvis (bottom graphs). A low-pass 3rd order butterworth filter was applied at 3 Hz to smooth the EMG signals
Discussion
To the authors’ knowledge, this is the first study to compare peak muscle activation from various stepping exercise modalities with a reference intensity of RE. While several studies have shown that elderly tend to perform daily life activities at a relatively higher effort than young adults (Hortobágyi et al. 2003; Reeves et al. 2008) and that task-specific training is effective for older adults (Manini et al. 2007; Bean et al. 2009; Pedersen et al. 2015), little evidence exists to determine which stepping exercise modalities have the most potential to improve muscle strength in this age group. Therefore, the purpose of this comparison was to determine if, with appropriate step height and direction, stepping could elicit peak muscle activation similar to medium–high intensity RE in elderly subjects and which conditions would yield highest activation. Our findings show that, depending on step height and direction, WBE can indeed elicit peak activation similar to—or higher than—RE at 60% 1-RM for all muscles except the ST.
Peak activation in weight bearing and resistance exercise
Although peak activation of the individual muscles during forward and lateral stepping has shown the potential to match and even surpass peak activation during a congruent RE at the threshold intensity of 60% 1-RM (Fig. 2), step height and, to a certain extent, step direction had different effects on the individual muscle activation. For this reason the comparisons will be discussed separately per muscle group.
For the quadriceps muscles, the minimal required step height to achieve similar peak activation to the baseline was remarkably different. Lateral stepping at 10 cm was sufficient to elicit activation of the VL similar to the baseline. In the RF, however, a minimum step height of 30 cm in lateral direction was required to reach peak activation similar to the baseline. Similar peak activation of the VL during corresponding intensities of leg press and knee extension shows that there is no difference between open and closed kinetic chain RE as a training stimulus for the VL. For the RF, none of the leg press intensities was able to elicit peak activation similar to congruent intensities of knee extension. These differences between VL and RF are all in line with results by Stensdotter et al. (2003) which they related to the nature of the RF as a multi-joint muscle and the fact that the RF has relative later onset activation timing compared to the other quadriceps muscles.
For the hamstrings clear differences were found between individual muscles. As opposed to the ST, which did not show activation up to baseline values for any of the WBE’s or leg press intensities, the BF could be recruited to the baseline starting at a step height of 10 cm and even showed significantly higher activation than the baseline at 30 cm step height for both forward and lateral directions. The difference in relative peak activation between ST and BF could be attributable to differences in neuromuscular coordination of the hamstrings to achieve the most economic force production during different tasks. Previous research has shown that during high load open kinetic chain exercises such as the leg curl, the ST is activated to a much larger extent than the BF (Schuermans et al. 2014). Consequently, the potential for closed kinetic chain exercise to elicit similar peak activation of the ST compared to the baseline is lower than for the BF.
GMAX showed similar recruitment to the baseline from 20 cm step height, regardless of step direction. During stepping the GMAX is mainly responsible for hip extension but also counteracts hip flexion moments induced by the RF when extending the knee during step ascent. This degree of co-activation is not required during isolated hip extension and may, therefore, account for the similarities in peak activation. Leg press peak activation compared to corresponding resistances of hip extension did not show any significant differences, indicating that closed kinetic chain resistance exercise did not provide an additional benefit over open kinetic chain resistance exercise for the GMAX.
GMED peak activation was relatively low in the forward stepping trials, which are functionally similar to stair climbing (Wang et al. 2003; Mair et al. 2014). Forward stepping at 10 cm and lateral stepping at 10 and 30 cm all recruited GMED to a level similar to the baseline. Overall, muscle activation was higher during lateral stepping then forward stepping. This is in line with research by Mercer et al. who found that sEMG activity of the GMED muscles was significantly higher when stepping in lateral direction compared to stepping in a forward direction (Stemmons Mercer et al. 2009). Additionally, this study indicates that a step height of 30 cm is preferable to achieve sufficient recruitment. Low peak activation of the GMED during the leg press indicated that, despite being considered an effective way to promote strength training in elderly, the leg press is likely not ideally suited to induce gains in muscle strength of the GMED.
Overall, stepping-based WBE appears to be a viable way for elderly to simultaneously recruit several important upper leg muscles to a level required to improve muscle strength. Lateral stepping at a height of 30 cm yielded the best results as it simultaneously recruited all muscles measured up to—or beyond—their baseline activation, with the exception of the ST. This makes it an even more effective exercise than a leg press at 80% 1-RM, which could only recruit three out of six muscles to baseline activation.
Timing of peak activation
Our results (Fig. 3) show that peak activation for most muscles (except ST) occurs during the ascent phase of stepping, regardless of stepping direction. Similar activation patterns for VL and BF in forward stepping were found by Reeves et al. (Reeves et al. 2009), indicating concentric work performed by the quadriceps to lift the body while the hamstrings co-contract to extend the hip and simultaneously stabilize the knee joint. Peak activation of the GMED during the ascent phase of lateral stepping was expected since the GMED is the primary muscle responsible for hip abduction. However, during forward stepping peak activation of the GMED also occurred during the ascent phase which could be attributed to its role in controlling lateral weight shift during step ascent (Stemmons Mercer et al. 2009).
Clinical implications
These findings indicate the importance of acquiring fundamental knowledge regarding different exercise modalities prior to designing more effective exercise programs for elderly. For example, most studies on the effects of stepping exercise only applied a limited range of step heights, based on commonly encountered step heights (Wang et al. 2003; Mair et al. 2014). The results of this study, however, show that this may not provide enough training stimulus for the RF and GMED. For the VL, WBE appears to be an excellent exercise method since a step height of 20 cm is more than sufficient to achieve threshold level activation regardless of stepping direction. For the GMED, however, proper step direction and height (lateral at 30 cm) are essential to achieve threshold activation.
Future considerations
There are some limitations to this study that need to be taken into consideration. First, some major leg muscles such as the vastus medialis, tibialis anterior and gastrocnemius were not included in the analyses. Previous research by Stensdotter et al. (2003) has shown that activation of the vastus medialis obliquus is higher during closed kinetic chain exercises compared to open kinetic chain exercises, indicating that stepping exercise also has a higher training potential for the vastus medialis obliquus. And while the plantar- and dorsiflexors also play an important role during functional tasks and balance recovery (Pijnappels et al. 2008), no congruent RE was performed to serve as a reference for comparison.
Second, no assumptions can be made with regard to repetitions required to improve muscle strength. Since fatigue affects the EMG power spectrum (Dimitrova and Dimitrov 2003) and fatigue onset is different in every subject, all exercises were performed with minimal repetitions to minimize possible signal changes which could affect a reliable comparison between each exercise type and intensity. Further research is needed to explore the optimal training volume and further improve the fundamental basis for stepping based WBE in elderly.
Third, during lateral stepping a safety bar was essential to provide subjects with the confidence to perform an unfamiliar movement normally, without fear of falling. Subjects were clearly instructed to only use the bar for tactile feedback and any force applied was visible since the bar could shift slightly. When a shift of the bar was detected or task execution was not adequate, subjects were asked to perform the task again. Only adequately performed tasks were included in the analyses. However, the use of this safety bar may still have influenced muscular activation of the GMED in particular, resulting in a higher variability at step height of 20 cm where not all subjects utilized this safety feature. However, even with the use of a safety bar, lateral stepping at 30 cm could still incite muscular activation to the baseline reference for muscular gains.
Finally, this study was conducted exclusively with elderly females because they are at higher risk for developing functional limitations and falling incidents compared to men due to accelerated muscle loss after menopause (Cederholm et al. 2013; Montero and Serra 2013). In addition, the cohort was quite homogenous due to strict exclusion criteria. For this reason no additional baseline measurements of functional status were recorded to further characterize the cohort. Therefore, caution is advised when extrapolating the results of this study to male or young populations and elderly with physical disability.
Conclusion
Stepping-based WBE appears to be a viable alternative to RE for improving muscle strength, since it shows the capacity to produce peak muscular activation similar to RE at an intensity required to induce hypertrophy and strength gains, while also incorporating relevant task-specific challenges to balance and coordination. However, exercise characteristics such as step height and step direction affect recruitment of individual muscles differentially and need to be taken into account when designing training programs. Lateral stepping at 30 cm step height appears to provide the best training potential for all muscles except the ST. The findings from this study can be used to comprise more evidence-based WBE-based training programs to improve both strength and functional performance in elderly.
Abbreviations
- BF:
-
Biceps femoris
- Fstep:
-
Forward stepping
- GMAX:
-
Gluteus maximus
- GMED:
-
Gluteus medius
- iMVC:
-
Isometric maximal voluntary contraction
- Lstep:
-
Lateral stepping
- 1-RM:
-
One-repetition maximum
- RF:
-
Rectus femoris
- RE:
-
Resistance exercise
- ST:
-
Semitendinosus
- sEMG:
-
Surface electromyography
- VL:
-
Vastus lateralis
- WBE:
-
Weight bearing exercise
References
American College of Sports Medicine (2017) ACSM’s Guidelines for exercise testing and prescription, 10th edn. Lippincott Williams & Wilkins, Philadelphia
Anderson K, Behm DG (2005) The impact of instability resistance training on balance and stability. Sport Med 35:43–53. https://doi.org/10.2165/00007256-200535010-00004
Bean JF, Kiely DK, LaRose S et al (2009) Increased velocity exercise specific to task training versus the national institute on aging’s strength training program: Changes in limb power and mobility. J Gerontol Ser A Biol Sci Med Sci 64:983–991. https://doi.org/10.1093/gerona/glp056
Begalle RL, DiStefano LJ, Blackburn T, Padua DA (2012) Quadriceps and hamstrings coactivation during common therapeutic exercises. J Athl Train 47:396–405. https://doi.org/10.4085/1062-6050-47.4.01
Bice MR, Hanson N, Eldridge J et al (2011) Neuromuscular adaptations in elderly adults are task-specific during stepping and obstacle clearance tasks. Int J Exerc Sci 4:77–85
Boren K, Conrey C, Le Coguic J et al (2011) Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther 6:206–223
Brzycki M (1993) Strength testing-predicting a one-rep max from reps-to-fatigue. J Phys Educ Recreat Danc 64:88–90. https://doi.org/10.1080/07303084.1993.10606684
Bunton EE, Pitney WA, Cappaert TA, Kane AW (1993) The role of limb torque, muscle action and proprioception during closed kinetic chain rehabilitation of the lower extremity. J Athl Train 28:10–20
Burden A (2010) How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. J Electromyogr Kinesiol 20:1023–1035. https://doi.org/10.1016/j.jelekin.2010.07.004
Cawthon PM, Peters KW, Shardell MD et al (2014) Cutpoints for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol Ser A Biol Sci Med Sci 69 A:567–575. https://doi.org/10.1093/gerona/glu023
Cederholm T, Cruz-Jentoft AJ, Maggi S (2013) Sarcopenia and fragility fractures. Eur J Phys Rehabil Med 49:111–117
Cress ME, Conley KE, Balding SL et al (1996) Functional training: muscle structure, function, and performance in older women. J Orthop Sports Phys Ther 24:4–10
De Luca CJ, Donald Gilmore L, Kuznetsov M, Roy SH (2010) Filtering the surface EMG signal: Movement artifact and baseline noise contamination. J Biomech 43:1573–1579. https://doi.org/10.1016/j.jbiomech.2010.01.027
Dimitrova N, Dimitrov GV (2003) Interpretation of EMG changes with fatigue: facts, pitfalls, and fallacies. J Electromyogr Kinesiol 13:13–36. https://doi.org/10.1016/S1050-6411(02)00083-4
Donath L, van Dieën JH, Faude O (2015) Exercise-based fall prevention in the elderly: what about agility? Sport Med 46:143–149. https://doi.org/10.1007/s40279-015-0389-5
Fisher J, Steele J, Smith D (2016) High- and low-Load resistance training: interpretation and practical application of current research findings. Sport Med 1–8. https://doi.org/10.1007/s40279-016-0602-1
Giarmatzis G, Jonkers I, Baggen RJ, Verschueren SM (2017) Less hip joint loading only during running rather than walking in elderly compared to young adults. Gait Posture 53:155–161. https://doi.org/10.1016/j.gaitpost.2017.01.020
Hakkinen K, Alen M, Kallinen M et al (2000) Neuromuscular adaptation during prolonged strength training, detraining and re-strength training in middle-aged and elderly people. Eur J Appl Physiol 83:51–62. https://doi.org/10.1007/s004210000248
Hodder JN, Keir PJ (2013) Obtaining maximum muscle excitation for normalizing shoulder electromyography in dynamic contractions. J Electromyogr Kinesiol 23:1166–1173. https://doi.org/10.1016/j.jelekin.2013.06.012
Hortobágyi T, Mizelle C, Beam S, DeVita P (2003) Old adults perform activities of daily living near their maximal capabilities. J Gerontol A Biol Sci Med Sci 58:M453–M460. https://doi.org/10.1093/gerona/58.5.M453
Klass M, Baudry S, Duchateau J (2007) Voluntary activation during maximal contraction with advancing age: a brief review. Eur J Appl Physiol 100:543–551. https://doi.org/10.1007/s00421-006-0205-x
Kraemer WJ, Keuning M, Ratamess N et al (2001) Resistance training combined with bench-step aerobics enhances women’s health profile. Med Sci Sports Exerc 33:259–269. https://doi.org/10.1097/00005768-200102000-00015
Liu C, Latham NK (2009) Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev (3):CD002759
Macadam P, Cronin J, Contreras B (2015) An examination of the gluteal muscle activity associated with dynamic hip abduction and hip external rotation exercise: a systematic review. Int J Sports Phys Ther 10:573–591
Mair JL, Laudani L, Vannozzi G et al (2014) Neuromechanics of repeated stepping with external loading in young and older women. Eur J Appl Physiol 114:983–994. https://doi.org/10.1007/s00421-014-2826-9
Manini T, Marko M, VanArnam T et al (2007) Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life. J Gerontol A Biol Sci Med Sci 62:616–623 pii]
Montero N, Serra JA (2013) Role of sarcopenia in elderly. Eur J Phys Rehabil Med 49:131–143
Pedersen MM, Petersen J, Bean JF et al (2015) Feasibility of progressive sit-to-stand training among older hospitalized patients. PeerJ 3:e1500. https://doi.org/10.7717/peerj.1500
Pijnappels M, van der Burg PJCE., Reeves ND, van Dieën JH (2008) Identification of elderly fallers by muscle strength measures. Eur J Appl Physiol 102:585–592. https://doi.org/10.1007/s00421-007-0613-6
Reeves ND, Spanjaard M, Mohagheghi AA et al (2008) The demands of stair descent relative to maximum capacities in elderly and young adults. J Electromyogr Kinesiol 18:218–227. https://doi.org/10.1016/j.jelekin.2007.06.003
Reeves ND, Spanjaard M, Mohagheghi AA et al (2009) Older adults employ alternative strategies to operate within their maximum capabilities when ascending stairs. J Electromyogr Kinesiol 19:e57–e68. https://doi.org/10.1016/j.jelekin.2007.09.009
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127:990s–991s
Schoenfeld BJ (2013) Is there a minimum intensity threshold for resistance training-induced hypertrophic adaptations? Sports Med 43:1279–1288. https://doi.org/10.1007/s40279-013-0088-z
Schoenfeld BJ, Wilson JM, Lowery RP, Krieger JW (2014) Muscular adaptations in low- versus high-load resistance training: a meta-analysis. Eur J Sport Sci 1391:1–10. https://doi.org/10.1080/17461391.2014.989922
Schuermans J, Van Tiggelen D, Danneels L, Witvrouw E (2014) Biceps femoris and semitendinosus—teammates or competitors? New insights into hamstring injury mechanisms in male football players: a muscle functional MRI study. Br J Sports Med 48:1599–1606. https://doi.org/10.1136/bjsports-2014-094017
Sherrington C, Tiedemann A, Fairhall N et al (2011) Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. N S W Public Health Bull 22:78–83. https://doi.org/10.1071/NB10056
Staudenmann D, Roeleveld K, Stegeman DF, van Dieen JH (2010) Methodological aspects of SEMG recordings for force estimation—a tutorial and review. J Electromyogr Kinesiol 20:375–387. https://doi.org/10.1016/j.jelekin.2009.08.005
Stemmons Mercer V, Gross MT, Sharma S, Weeks E (2009) Comparison of gluteus medius muscle electromyographic activity during forward and lateral step-up exercises in older adults. Phys Ther 89:1205–1214
Stensdotter AK, Hodges PW, Mellor R et al (2003) Quadriceps activation in closed and in open kinetic chain exercise. Med Sci Sports Exerc 35:2043–2047. https://doi.org/10.1249/01.MSS.0000099107.03704.AE
Sundell J (2011) Resistance training is an effective tool against metabolic and frailty syndromes. Adv Prev Med 2011:984683. https://doi.org/10.4061/2011/984683
Van Roie E, Verschueren SM, Boonen S et al (2011) Force-velocity characteristics of the knee extensors: an indication of the risk for physical frailty in elderly women. Arch Phys Med Rehabil 92:1827–1832. https://doi.org/10.1016/j.apmr.2011.05.022
Van Roie E, Delecluse C, Coudyzer W et al (2013) Strength training at high versus low external resistance in older adults: effects on muscle volume, muscle strength, and force–velocity characteristics. Exp Gerontol 48:1351–1361. https://doi.org/10.1016/j.exger.2013.08.010
Van Roie E, Bautmans I, Coudyzer W et al (2015) Low- and high-resistance exercise: long-term adherence and motivation among older adults. Gerontology 61:551–560. https://doi.org/10.1159/000381473
Wang M-Y, Flanagan S, Song J-E et al (2003) Lower-extremity biomechanics during forward and lateral stepping activities in older adults. Clin Biomech 18:214–221. https://doi.org/10.1016/S0268-0033(02)00204-8
Ward BW, Clarke TC, Nugent CN, Schiller JS (2016) Early release of selected estimates based on data from the 2015 National Health Interview Survey (05/2016). Natl Heal Interview Surv Early Release Progr, pp 1–120
Wood TM, Maddalozzo GF, Harter RA (2002) Accuracy of seven equations for predicting 1-RM performance of apparently healthy, sedentary older adults. Meas Phys Educ Exerc Sci 6:67–94. https://doi.org/10.1207/S15327841MPEE0602_1
Acknowledgements
This study was funded by the European Commission through MOVE-AGE, an Erasmus Mundus Joint Doctorate programme (Grant number 2014-0691) and by the Fund for Scientific Research Flanders (FWO-Vlaanderen, Grant number G0521-05). We would like to thank Dr. Georgios Giarmatzis and MSc. Aijse de Vries for their assistance during data collection and programming.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest. The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Additional information
Communicated by Toshio Moritani.
Rights and permissions
About this article
Cite this article
Baggen, R.J., Van Roie, E., van Dieën, J.H. et al. Weight bearing exercise can elicit similar peak muscle activation as medium–high intensity resistance exercise in elderly women. Eur J Appl Physiol 118, 531–541 (2018). https://doi.org/10.1007/s00421-017-3793-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-017-3793-8