Abstract
During high-intensity dynamic exercise, O2 delivery to active skeletal muscles is enhanced through marked increases in both cardiac output and skeletal muscle blood flow. When the musculature is vigorously engaged in exercise, the human heart lacks the pumping capacity to meet the blood flow demands of both the skeletal muscles and other organs such as the brain. Vasoconstriction must therefore be induced through activation of sympathetic nervous activity to maintain blood flow to the brain and to produce the added driving pressure needed to increase flow to the skeletal muscles. In this review, we first briefly summarize the local vascular and neural control mechanisms operating during high-intensity exercise. This is followed by a review of the major neural mechanisms regulating blood pressure during high-intensity exercise, focusing mainly on the integrated activities of the arterial baroreflex and muscle metaboreflex. In high cardiac output situations, such as during high-intensity dynamic exercise, small changes in total peripheral resistance can induce large changes in blood pressure, which means that rapid and fine regulation is necessary to avoid unacceptable drops in blood pressure. To accomplish this rapid regulation, arterial baroreflex function may be modulated in various ways through activation of the muscle metaboreflex and/or other neural mechanisms. Moreover, this modulation of the arterial baroreflex may change over the time course of an exercise bout, or to accommodate changes in exercise intensity. Within this model, integration of arterial baroreflex modulation with other neural mechanisms plays an important role in cardiovascular control during high-intensity exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most animals live within a limited set of environmental conditions, reflecting Bergmann’s (1847) rule that a species’ body size dictates its living climate. One exception is humans, who now live in most areas of the earth, and so are exposed to a wide range of temperatures and altitudes. Nowadays, in fact, our range is not limited by our terrestrial nature, and we are active both under water and in space. On earth, humans carry out their daily activity mainly in an upright posture, with their heads located above the heart. Consequently, blood pressure (BP) must be well regulated to maintain blood flow in the brain, despite different environments and changing activity levels.
During dynamic exercise, for example, blood flow increases to meet the demands of the skeletal muscles engaged in contractile activity as well as the respiratory and heart muscles. Under these conditions, increased skeletal muscle blood flow is critical to ensure an appropriate supply of O2 to the active skeletal muscles and to remove the metabolic byproducts and generated heat. This exercise-induced skeletal muscle hyperaemia is essentially the product of selective vasodilation of vascular units perfusing the active muscle fibers. But for vasodilation to result in a significant elevation of skeletal muscle blood flow, cardiac output (Q) must increase, and blood flow must also be redistributed from inactive regions (e.g., splanchnic and renal circulations) to support the increase in skeletal muscle blood flow (Calbet and Joyner 2010). In most cases, increases in Q during submaximal dynamic exercise are well matched to increases in skeletal muscle blood flow. In 1977, however, Secher et al. (1977) showed that when arm exercise is added to ongoing leg exercise, lower limb blood flow is reduced despite the unaltered leg power output, reflecting vasoconstriction of the arteries feeding the contracting skeletal muscles in the leg. This led to the idea that the pumping capacity of a healthy human heart is not always sufficient to supply the skeletal muscle with blood, and that vasoconstriction is induced by activation of sympathetic nervous activity (SNA) to maintain BP, even when most of the muscles are vigorously engaged in exercise (Calbet et al. 2004). In 1985, Andersen and Saltin (1985) reported blood flow values of 250 mL (100 g)−1 min−1 for the quadriceps muscle during a leg knee extension exercise, using continuous infusion thermodilution to measure femoral vein outflow and Doppler to measure the arterial inflow (Radegran et al. 1999). Further, in endurance-trained thigh muscles, the maximal blood flow may reach 400 mL (100 g)−1 min−1 (Richardson et al. 1993). Thus, 10 kg of active skeletal muscle (less than the total amount of muscle in the lower legs) may require a maximum of 40 L−1 min−1, which is beyond the heart’s typical pumping capacity of 25–35 L min−1. Notably, BP can be simply expressed using Ohm’s law: blood pressure (BP) = cardiac output (Q) × total peripheral resistance (TPR). This means that to maintain BP within a desired range, bodies must appropriately regulate Q and TPR. So for vasodilation to result in a significant increase in blood flow to the large exercising skeletal muscles TPR can be reduced; however, if the increase in Q does not offset the reduction in TPR, BP will fall. Thus, during whole-body heavy dynamic exercise, the demand for O2 delivery to the active muscles (i.e., the vasodilation to increase skeletal muscle blood flow) strongly competes with BP regulation mediated by neural sympathetic-induced vasoconstriction.
A schematic drawing illustrating systemic BP regulation during exercise is shown in Fig. 1. During high-intensity dynamic exercise, vasodilation within active muscles is mainly influenced by local vascular control mechanisms such as endothelium-mediated dilation, byproduct-induced dilation, erythrocyte-dependent regulation, etc. To maintain BP at an acceptable level during exercise, despite strong vasodilation within the active muscles, sympathetic vasoconstriction must occur within inactive muscles, and even within active muscles, to help redistribute Q to the contracting muscle. It is generally presumed that increased SNA during exercise reflects the activities of both feedforward systems, such as central command, and peripheral feedback systems, such as the arterial baroreceptors, cardiopulmonary baroreceptors, muscle metaboreceptors and mechanoreceptors, and arterial chemoreceptors (Rowell and O’Leary 1990; Rowell et al. 1996; Dempsey 2012; Murphy et al. 2011; Matsukawa 2011; Fadel et al. 2003; Fadel and Raven 2011). During high-intensity exercise, those local and neural control systems are working both independently and synergistically, such that BP control during high-intensity exercise is the product of highly integrated regulation. As shown in Fig. 1, it is hypothesized that efferent sympathetic responses are determined by the integrated input from several neural control systems in the medulla (Integration site ①), while the vascular responses are determined by the integrated effects of sympathetic vasoconstriction and local vasodilation (Integration site ②). Thus, to understand BP control mechanisms during high-intensity exercise, it is necessary to understand not only the characteristics of each control system, but also the interaction among those control systems.
Schematic drawing illustrating systemic cardiovascular regulation during exercise. Within the central nervous system, regulatory signals through central command and peripheral reflexes are integrated in the cardiovascular center (Integration site ①). Vascular responses in/on the vessels (Integration site ②) are also integrated among local regulatory mechanisms and sympathetic vasoconstriction
In this review, we will first briefly summarize local vascular control mechanisms as the main vascular response for O2 delivery during exercise. We will then briefly summarize neural mechanisms as the main control system for maintaining BP during exercise. Among the neural mechanisms operating, the arterial baroreflex and muscle metaboreflex are hypothesized to play particularly important roles during high-intensity exercise. Therefore, the main focus of this review will be on the regulation and possible integration of those reflexes as the major neural-cardiovascular control mechanisms operating during high-intensity exercise.
Local vascular control mechanisms during exercise
Muscle blood flow is determined by perfusion pressure and vasomotor tone in the resistance vessels of the muscles. Local factors that regulate vasomotor tone in active skeletal muscles include substances released from nerves, substances released by or near active muscles, substances carried in the blood, mechanical and myogenic mechanisms, and veno-arterial reflexes (Clifford 2011; González-Alonso 2012; Laughlin 1987; Laughlin et al. 1996) (Fig. 1). Over the years, these factors have been extensively investigated and a number of substances thought to be released from active skeletal muscle have been implicated in exercise hyperaemia or hypothesized to be the “main” or “obligatory” factor that links muscle blood flow to metabolism. The concepts and proposed substances have been well summarized in earlier reviews (Shepherd 1983; Laughlin et al. 1996; Saltin et al. 1998), as has the recent progress in this area (Joyner and Wilkins 2007; González-Alonso 2012; Clifford 2011). The following is a brief discussion of the factors potentially involved in mediating human exercise hyperaemia within active skeletal muscles.
Substances released by the endothelium
It is well recognized that vascular endothelial cells play an important role in the regulation of vascular activity through their production of vasoactive substances, including nitric oxide (NO), a potent vasodilator contributing to the regulation of local vascular tone (Palmer et al. 1987). Plasma NO (measured as the stable end product of NO; i.e., nitrite/nitrate) is reportedly increased in exercising humans (Node et al. 1997), and several observations suggest NO plays an important role in exercise-induced vasodilation and hyperemia in skeletal muscle (Dyke et al. 1995; Gilligan et al. 1994; Hickner et al. 1997; Hirai et al. 1994; Miyauchi et al. 2003). However, recent studies also indicate that NO is not an obligatory regulator of blood flow during exercise-induced hyperemia in human skeletal muscle (Joyner and Wilkins 2007).
Substances released by muscle
ATP, ADP, adenosine and related compounds (e.g., phosphate) have long been known as putative factors controlling exercise hyperaemia (Joyner and Wilkins 2007). However, to the extent that these substances can be manipulated (especially blocked) pharmacologically, their importance as obligatory factors mediating “normal” exercise hyperaemia is unclear. An attractive property of ATP (see below) is that, unlike adenosine, acetylcholine or nitroprusside, its exogenous administration evokes massive dilatation during heavy exercise (Rosenmeier et al. 2004). By contrast, exogenous administration of the other substances typically generates only 50–75 % of the total hyperaemic response.
Erythrocyte-dependent regulation (ATP) during exercise
Recent evidence provides strong support for the notion that circulating erythrocytes play a pivotal role in the regulation of local vascular processes matching O2 supply and demand within active skeletal muscle in humans (Ellsworth et al. 1995; Ellsworth and Sprague 2012; González-Alonso et al. 2002; González-Alonso 2012). It has been proposed that erythrocytes contribute to local regulatory processes, in part, by releasing ATP to act as a vasodilator and sympatholytic in response to several metabolic and mechanical stimuli (González-Alonso 2012; Sprague et al. 1998). The released ATP acts via P2Y purinergic receptors expressed on microvessel endothelial cells to induce profound local and conducted vasodilatation through stimulation of endothelial production of NO, prostaglandin, endothelium-derived hyperpolarizing factor (EDHF), and possibly other endothelial vasoactive signals (Ellsworth et al. 2009; Mortensen et al. 2009). Within human limbs, ATP also appears to act on smooth muscle cells, exerting its local vasodilator and sympatholytic effects (Rosenmeier et al. 2008) directly, without degradation to ADP, AMP or adenosine.
Autonomic control mechanisms during exercise
Central command is thought to be crucial for the rapid cardiovascular regulation operating in parallel with the start of exercise. In addition to central command, peripheral reflexes are feedback systems that detect changes (i.e., error signals) within an organism and act to correct those changes. Among these peripheral reflexes, the arterial baroreflexes and the reflexes arising from exercising skeletal muscles, the so-called “exercise pressor reflex” (i.e., the muscle metaboreflex and mechanoreflex), are thought to be mainly involved in regulating cardiovascular function during high-intensity exercise. Those neural controls have also been well summarized in several recent reviews (Murphy et al. 2011; Dempsey 2012; Fadel et al. 2003; Fadel and Raven 2011). The following is a brief summary of the central command, exercise pressor reflex and arterial baroreflex.
Central command
Central command is a feedforward neural mechanism that transmits excitatory impulses to descending motor neurons for locomotion, and in a parallel fashion to the medulla oblongata for activation of cardiovascular control circuits (Goodwin et al. 1972). In 1913, Krogh and Linhard (1913) quantified the rapid increase in ventilation and pulse rate that occurs within 1 s of the onset of voluntary exercise and concluded that an irradiation of impulses from the motor cortex was the most likely explanation for such a rapid response. Since that time, numerous investigations in both animals and humans have established the importance of central command in the feedforward regulation of the cardiovascular response to exercise (Matsukawa 2011; Matsukawa et al. 2012; Ishii et al. 2012; Ogoh et al. 2002b).
Exercise pressor reflex (muscle metaboreflex and mechanoreflex)
In 1917, Krogh and Linhard (1917) further demonstrated in humans that HR and ventilation were rapidly increased at the onset of involuntary leg contraction induced by electrical stimulation of skeletal muscle under the assumption that the response did not involve voluntary movement and hence eliminated central command. It was concluded that reflex input from the skeletal muscle itself was involved in mediating the cardiorespiratory response to exercise. In support of this concept, Alam and Smirk (1937, 1938a) demonstrated that dynamic calf exercise evoked increases in BP that could be maintained by circulatory arrest after cessation of the exercise. Then upon restoration of blood flow, BP fell precipitously. In a similar protocol, a spinal cord injury patient in whom motor control was preserved, though sensation below one knee was lost, performed a calf exercise with the insensate leg (Alam and Smirk 1938b). The exercise evoked typical increases in HR and BP, but in this patient the sympathoexcitatory responses were not sustained during post-exercise circulatory occlusion. These elegant experiments demonstrated that a reflex originating in skeletal muscle, the exercise pressor reflex, as it is known today (McCloskey and Mitchell 1972; Mitchell et al. 1983), is intimately involved in mediating precise cardiovascular adjustments to exercise. Further, it is now known that the exercise pressor reflex is the product of the so-called muscle metaboreflex and mechanoreflex, whereby group III afferent nerve endings in skeletal muscles function mainly as mechanoreceptors and group IV afferent endings function as metaboreceptors (Adreani and Kaufman 1998; Rowell and O’Leary 1990). These sensory neurons project to the medulla oblongata, and can be stimulated by a variety of metabolites, including lactic acid, adenosine, potassium, diprotonated phosphate, H+ and arachidonic acid products, among others, as well as by mechanical stimuli such as stretch, pressure and contraction (Murphy et al. 2011; Mitchell 1990; Rowell and O’Leary 1990). Activation of the exercise pressor reflex has been shown to evoke increases in SNA, BP, HR, Q and peripheral vasoconstriction, as well as secretion of various vasoactive hormones (Amann et al. 2011; Rowell et al. 1996; Rowell and O’Leary 1990).
Arterial baroreflex
Mechanosensitive nerve endings in the walls of the carotid sinuses and aortic arch are called arterial baroreceptors; they transduce arterial BP changes (distention of the artery in the baroreceptor region) and provide neural information to the central nervous system (Eckberg and Sleight 1992). On the basis of this afferent signaling, efferent autonomic nerve activity is modulated, and the activities of the heart and blood vessels are adjusted on a beat-by-beat basis in an effort to shift systemic BP in the direction opposite to the one giving rise to the input stimulus (Manica and Mark 1983; Sagawa 1983). This reflexive feedback mechanism for control of arterial BP is the so-called arterial baroreflex. The arterial baroreflex function curve, which is constructed by plotting baroreflex output responses (regulated systemic BP, HR, SNA, etc.) against input stimuli to the baroreceptors (BP changes in the baroreceptor regions), is sigmoidal (Fig. 2). Baroreflex-mediated feedback regulation of BP functions continuously within this sigmoidal relationship as changes in input evoke corresponding changes in output to restore the input value to a desired operating point. However, exercise increases both arterial BP and HR, which means the baroreflex-mediated relationship between arterial BP and HR obtained at rest cannot explain the relationship during exercise. This phenomenon led to the hypothesis that the baroreflex function curve and its operating point shift rightward and upward as shown in Fig. 2; that is, the baroreflex input–output relationship is reset during exercise (Rowell et al. 1996; Raven et al. 1997). The increases in HR and SNA, together with the rise in arterial BP, seen during exercise can be explained by this hypothesis if the baroreflex function curve is shifted rightward and upward in accordance with increases in exercise intensity, and autonomic nerve activity is modulated such that arterial BP and HR move to the new operating point on the shifted function curve. In that scenario, arterial BP and HR rise together.
Schematic drawing of the arterial baroreflex function curve and its resetting during exercise. The operating point is the arterial blood pressure that acts as the reference value for the arterial baroreflex. When blood pressure changes from the operating point, the arterial baroreflex works to restore it to the operating point
Integration among peripheral reflexes and qualitative regulation
The mechanisms involved in the upward and rightward shift in the arterial baroreflex function curve are not fully understood, but it is recognized that this curve shift is due to modulation of the arterial baroreflex through activation of central command and/or the exercise pressor reflex during exercise. During steady-state exercise in conscious animals and humans, the baroreflex is reset to function around the higher BPs induced by the physical activity (Fisher et al. 2007; Komine et al. 2003; Potts et al. 1993), enabling it to retain the ability to finely tune the cardiovascular response to exercise. Clearly, all of the described neural inputs (i.e., central command, muscle metaboreflex, muscle mechanoreflex, and the arterial and cardiopulmonary baroreflexes, etc.) contribute significantly to the regulation of the autonomic nervous system during exercise. Each signal is known to transmit information directly to the cardiovascular regulatory centers within the medulla, where the signals are integrated (Integration site ①; Fig. 1), and the autonomic efferent output, and thus the function of the arterial baroreflex, are modulated accordingly. In addition, the transmitted sympathetic efferent signals are further integrated at the local vasculature (Integration site ②; Fig. 1). The sympathetic vasoconstrictor response is attenuated in active skeletal muscles through what is called “sympatholysis” (Remensnyder et al. 1962), but may also be potentiated through interaction with substances circulating in the blood (Yang et al. 1990), so-called “sensitization”. Thus, the BP response during heavy exercise reflects integrated regulation within the central nervous system and at local sites. We will focus on the relationship between the arterial baroreflex and muscle metaboreflex as the typical representation of the integrated regulation during heavy exercise.
Integrated interaction between arterial baroreflex and muscle metaboreflex
It is thought that during heavy exercise, the arterial baroreflex and the muscle metaboreflex are both activated and are interacting in ways that lead to modulation of the primary cardiovascular reflex responses (Sheriff et al. 1990; Nishiyasu et al. 1994a; Rowell et al. 1996; Papelier et al. 1997; Cui et al. 2001; Kamiya et al. 2001; Kim et al. 2005; Ichinose et al. 2002, 2004c, 2006b, 2008; Watanabe et al. 2010). Two types of interaction between the arterial baroreflex and muscle metaboreflex in the control of cardiovascular responses have been demonstrated. The first involves arterial baroreflexes opposing the pressor response elicited via the muscle metaboreflex. The second is a modulation of arterial baroreflex function during muscle metaboreflex activation.
Arterial baroreflex buffers muscle metaboreflex-induced pressor responses
When the muscle metaboreflex is activated and a reflex pressor response occurs, the arterial baroreceptors are loaded, and the resultant baroreflex acts to reduce the rising arterial BP; that is, the arterial baroreflex buffers the muscle metaboreflex pressor response. Sheriff et al. (1990) showed that the muscle metaboreflex pressor response in dogs is increased by about 200 % after arterial baroreceptor denervation, as compared to the same dogs with intact baroreceptors. Their results demonstrated the highly potent buffering effect of the arterial baroreflex on the muscle metaboreflex pressor response. According to Kim et al. (2005) the remarkable increase in the muscle metaboreflex pressor response in baro-denervated dogs is attributable to an increase in peripheral vascular resistance without an increase in Q, which means that in intact animals, the arterial baroreflex buffers the muscle metaboreflex pressor response by inhibiting peripheral vasoconstriction. Similar observations have also been made in humans. For example, Scherrer et al. (1990) showed that increases in HR and muscle sympathetic nerve activity (MSNA) elicited during isometric handgrip exercise at 33 % of maximal voluntary contraction (MVC) are augmented in subjects receiving nitroprusside to suppress the handgrip-induced rise in BP; conversely, HR and MSNA responses were suppressed in subjects receiving phenylephrine to accentuate the handgrip-induced elevation in BP. Because the muscle metaboreflex would be activated and contributing to the rise in HR and MSNA during the handgrip exercise, these findings suggest the loading state of the arterial baroreceptors influences the muscle metaboreflex-mediated cardioacceleration and sympathoexcitation.
During isometric handgrip exercise at 50 % MVC, arterial BP, HR, and MSNA progressively increase over the course of the exercise, as shown in Fig. 3. Then if the exercising forearm is occluded by inflating a cuff fixed at the upper arm to a supersystolic pressure just before the end of the exercise, arterial BP and MSNA remain elevated, even after the end of the exercise. During the period of post-exercise muscle ischemia (PEMI), central command and the muscle mechanoreflex are no longer active because the exercise has been terminated. Therefore, these pressor responses are thought to be evoked via the muscle metaboreflex, which is being activated by metabolic byproducts produced in the forearm skeletal musculature during exercise and now trapped there by the pressure cuff. Induction of PEMI is thus a classic technique to isolate the effect of the muscle metaboreflex from other factors. Because during high-intensity exercise, factors other than the muscle metaboreflex also contribute to cardiovascular regulation, and the observed responses reflect the integration of all the factors involved, it is difficult to selectively assess the effects of the muscle metaboreflex and its interaction during high-intensity exercise. For that reason, PEMI has been widely used as an experimental model to study the interactions between the muscle metaboreflex and other peripheral reflexes, especially in humans.
Representative raw data showing heart rate (HR), arterial blood pressure, and muscle sympathetic nerve activity (MSNA) at rest and during isometric handgrip exercise (IHG) at 50 % MVC, post-exercise muscle ischemia (PEMI) and recovery (Rec). Note that PEMI prevents recovery of BP and MSNA, though HR returns to resting level
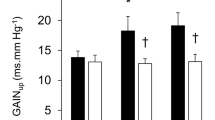
Interestingly, although the increase in SNA seen during PEMI ought to affect both the peripheral vasculature and the heart, HR returns to the resting level (Fig. 3). In that regard, O’Leary (1993) demonstrated that HR remains higher than at rest during PEMI in dogs administered atropine to block parasympathetic nerve activity, and suggested the fall of HR to the resting level during PEMI is due to reactivation of parasympathetic nerve activity after the end of the exercise. In addition, Nishiyasu et al. (1994a) showed that both cardiac sympathetic and parasympathetic tone increase simultaneously during PEMI in humans. They suggested the increase in cardiac parasympathetic tone might be a component of a counteraction by the arterial baroreflex against the elevation in BP induced by the muscle metaboreflex. Other recent studies in humans reported similar observations (Ichinose et al. 2007; Fisher et al. 2010). These findings suggest that maintenance of HR at the resting level during PEMI could reflect the interaction of the effects of sympathetic activation induced via the muscle metaboreflex and parasympathetic activation induced via the arterial baroreflex. Recently, Watanabe et al. (2010) showed that the HR response during PEMI varies considerably from individual to individual. When they investigated the cause of the large individual variation in the HR response, they found that individuals with greater increases in cardiac parasympathetic tone (Fig. 4, left panel) and greater cardiac baroreflex sensitivity (Fig. 4, right panel) during PEMI likely show a greater bradycardic response to PEMI, and vice versa. Their results suggest the interaction between the arterial baroreflex and the muscle metaboreflex may contribute to the individual variation in cardiovascular responses seen during exercise.
Relationships between PEMI-induced changes in the R–R interval and changes in the spectral power of R–R interval variability in the high-frequency range (∆HF power: an index of cardiac parasympathetic tone) and cardiac baroreflex sensitivity (∆Baroreflex sensitivity). Symbols depict data from individual subjects. Lines are the regression lines. Forty subjects’ individual data are plotted in each figure. The mean HR during PEMI did not differ from the resting HR in the forty subjects. However, the HRs of several subjects did increase or decrease from the resting levels during PEMI, indicating there is considerable individual variation in the HR response to PEMI. Likewise, variation in cardiac parasympathetic tone and cardiac baroreflex sensitivity during PEMI are also associated with the large individual differences in the HR response to PEMI. These relationships may have important implications for understanding an individual’s modulation of cardiovascular responses during exercise (reproduced from Watanabe et al. 2010)
Muscle metaboreflex modulates arterial baroreflex function
Arterial baroreflex-mediated cardiovascular regulation is modulated during activation of the muscle metaboreflex. Papelier et al. (1997) reported that during PEMI, the carotid sinus baroreflex shows reduced sensitivity to loading (neck suction) and enhanced sensitivity to unloading (neck pressure) for blood pressure regulation, but the sensitivity for HR regulation is unchanged. In addition, recent studies using microneurographic recordings of MSNA in humans (Cui et al. 2001; Kamiya et al. 2001; Ichinose et al. 2002, 2004b; Ogoh et al. 2009) demonstrated more directly that arterial baroreflex control of SNA is modulated during muscle metaboreflex activation. In our studies (Ichinose et al. 2002; Ichinose and Nishiyasu 2005), we found that during PEMI, unloading the carotid baroreceptor by applying neck pressure evokes greater increases in MSNA, peripheral vasoconstriction and arterial BP than are evoked under control conditions (Fig. 5a). We also found that during PEMI, carotid baroreceptor loading via neck suction produces less suppression of MSNA and less vasodilation, resulting in smaller reductions in arterial BP (Fig. 5b). By contrast, there were no changes in the HR responses to either neck pressure or neck suction. These results suggest that carotid baroreflex-mediated sympathetic vascular regulation is modulated during activation of the muscle metaboreflex, and that the alterations in baroreflex function may contribute to the increase and/or maintenance arterial BP at a higher level than under resting conditions.
MSNA response in one subject to application of +50 mmHg neck pressure (a) and −60 mmHg neck suction (b) under control conditions and during PEMI. NP neck pressure, NS neck suction. During PEMI, the NP-evoked rise in MSNA was enhanced, and the NS-induced period of MSNA suppression was markedly shortened (reproduced from Ichinose et al. 2002)
The arterial baroreflex is known to influence the incidence and strength of MSNA bursts on a beat-to-beat basis, and it is thought to be the major modulator of MSNA in humans (Delius et al. 1972; Wallin et al. 1975; Sundlof and Wallin 1978; Wallin and Eckberg 1982; Fagius et al. 1985; Macefield and Wallin 1999; Kienbaum et al. 2001). During PEMI, both the incidence of MSNA bursting activity and the strength of the bursts are increased, and the bursting activity corresponds well to the fluctuations in arterial BP, which suggests dominant arterial baroreflex modulation on the MSNA. Ichinose et al. (2004c) examined the arterial baroreflex-mediated beat-to-beat MSNA control in three different ways (i.e., control of burst incidence, burst strength and total MSNA) using the linear relationship between spontaneous variations in diastolic arterial pressure (DAP) and MSNA during activation of the muscle metaboreflex. As shown in Fig. 6, the arterial baroreflex regulates the incidence and strength of MSNA bursts at higher BPs and MSNA levels during PEMI, with no change in those gains (slope of the DAP–MSNA lines), as compared to control conditions. In addition, as a consequence of those changes in the control of the incidence and strength of MSNA burst, the arterial baroreflex control of total MSNA is reset to higher BPs and MSNA levels, and the gain of the control is increased. Although the precise mechanisms within the CNS that regulate the sympathetic neurons producing sympathetic bursting activity are unclear, the gate control theory explains well the MSNA bursting that corresponds to arterial BP fluctuations (Kienbaum et al. 2001). Based on this theory, it is thought that arterial baroreflex inputs act as a gate that determines whether MSNA bursts occur, while having little influence on burst strength. Indeed, as seen in Fig. 6, the relationship between burst incidence and BP are quite strong, whereas changes in BP within the range of spontaneous fluctuations have little or no influence on burst strength during either control conditions or PEMI. Taking this into account, the increased occurrence of bursts during activation of the muscle metaboreflex might reflect alteration of the gating function of the arterial baroreflex. On the other hand, the increased burst strength during PEMI may be a result of more direct influence of the increased group III and IV afferent inputs on the sympathetic neurons. Such an integrated regulation of these two reflexes may also serve to maintain BP at a higher level by producing larger sympathetic bursts more frequently when BP starts to fall.
Linear relationships between DAP and burst incidence (a), burst strength (b) and total MSNA (c) under control conditions and during PEMI in a representative subject. PPo prevailing point [the point corresponding to the average diastolic arterial blood pressure (DAP) on the regression line relating burst incidence or total MSNA to DAP, which is taken as an index of the MSNA corresponding to the operating pressure of arterial baroreflex]. Because of the weak relationship between burst strength and DAP, the prevailing point for the regression line relating burst strength to DAP was not calculated. Arterial baroreflex control of the incidence and strength of MSNA bursts was shifted to higher BPs and MSNA levels during PEMI. As a consequence of those alterations, baroreflex control of total MSNA was shifted to higher BPs and MSNA levels, and its gain was increased (reproduced from Ichinose et al. 2004c)
Arterial baroreflex-mediated regulation of MSNA is modulated during both static and dynamic exercise (Scherrer et al. 1990; Fadel et al. 2001; Kamiya et al. 2001; Keller et al. 2004; Ogoh et al. 2007; Ichinose et al. 2006b, 2008). Figure 7 shows alterations in arterial baroreflex control over MSNA over the course of 3 min of isometric handgrip exercise at 30 % MVC. Activation of the muscle metaboreflex is thought to account for the time-dependent upward and rightward shifts in the DAP–MSNA relationship and for increase in the gain of MSNA control observed after the first minutes of handgrip exercise. This idea is supported by the finding that the modulation of the DAP–MSNA relationship that occurred during the handgrip exercise persisted during the PEMI, a time when the muscle metaboreflex would be activated in the absence of both central command and the muscle mechanoreflex. Presumably, the activation of the muscle metaboreflex would be delayed from the onset of exercise by the time needed to accumulate metabolites in the vicinity of the group III and IV afferent endings, which would account for the almost 60-s lag between the onset of isometric handgrip exercise and the onset of sympathetic activation (Seals et al. 1988; Victor et al. 1988; Saito et al. 1989; Pryor et al. 1990; Rowell and O’Leary 1990; Nishiyasu et al. 1994b). For the same reason, the metaboreflex may not be sufficiently activated during the first minute of handgrip exercise to mediate the upward shift in the DAP–MSNA relationship or the increase in the gain. Interestingly, the aforementioned study by Scherrer et al. (1990) showed that MSNA is increased within the first minute of isometric handgrip exercise (33 % MVC) in subjects receiving nitroprusside to suppress the handgrip-induced rise in BP and that, conversely, MSNA is suppressed in subjects receiving phenylephrine to accentuate the handgrip-induced elevation in BP. This suggests the lack of change in MSNA from the resting level during the first minute of handgrip exercise is due, at least in part, to arterial baroreflex control of MSNA. Our finding that the DAP–MSNA relationship is shifted rightward without a significant vertical shift or change in gain suggests that, during the first minute of handgrip exercise, the arterial baroreflex operating pressures are reset, enabling MSNA to be maintained at the resting level, despite an increase in BP. This rapid resetting of the arterial baroreflex operating pressure might be induced by activation of central command and/or the muscle mechanoreflex (Mitchell 1990; Rowell and O’Leary 1990; Rowell et al. 1996; Potts and Mitchell 1998; Gallagher et al. 2001; Iellamo et al. 1997; McIlveen et al. 2001; Ogoh et al. 2002b). In addition, the modulation of arterial baroreflex control of MSNA (i.e., resetting and an increase in gain) was greater during the third minute of handgrip exercise than during PEMI, which indicates that mechanisms other than the muscle metaboreflex (i.e., central command and/or muscle mechanoreflex) were also affecting arterial baroreflex control of MSNA at that time. The time-dependent modulation of the baroreflex function may be one of the mechanisms mediating the progressive increase in both BP and MSNA over the course of isometric exercise.
Group average prevailing points (symbols) with the corresponding mean regression lines relating total MSNA and DAP at the indicated times during the isometric handgrip exercise and PEMI. IHG1, 2 and 3 are the first, second, and third minutes of the isometric handgrip exercise, respectively. The arterial baroreflex control of MSNA was gradually shifted to higher BPs and MSNA levels, and its gain progressively increased over the course of the isometric handgrip exercise. This time-dependent modulation of baroreflex function would be induced through progressive activation of the muscle metaboreflex, central command, etc., during the handgrip exercise. These observations suggest that over the course of an exercise period, BP and MSNA will be increased and regulated at suitable levels through baroreflex modulation (reproduced from Ichinose et al. 2006b)
Figure 8 depicts the arterial baroreflex control over MSNA during dynamic leg cycling using an exercise protocol in which workload was incrementally increased in five steps from very mild to exhausting (Ichinose et al. 2008). Very mild exercise shifted the DAP–MSNA relationship to lower MSNA levels and also reduced arterial baroreflex gain. Thereafter, incremental increases in exercise workload from mild to exhausting caused a gradual upward shift in the DAP–MSNA relationship. During moderate exercise, the sensitivity of the MSNA control recovered to the resting level, and during heavy and exhausting exercise, there was a rightward and upward shift in the DAP–MSNA relation, with a significant increase in the gain. The findings during mild and moderate exercise are consistent with studies showing that arterial baroreflex gain of MSNA control is unchanged during moderate-intensity arm cycling (Fadel et al. 2001; Ogoh et al. 2007) and low-intensity one-legged kicking (Keller et al. 2004). Collectively, these results suggest that the sensitivity of the arterial baroreflex control over MSNA during mild to moderate dynamic exercise remains at the resting level, regardless of exercise mode. In addition, the modulation of the arterial baroreflex function observed during heavy and exhausting exercise is in good agreement with an earlier report showing that in rats, high-intensity treadmill exercise resets the arterial baroreflex control over renal SNA to higher BPs and higher SNA levels, with a significant increase in arterial baroreflex gain (Miki et al. 2003). Bearing those observations in mind, the arterial baroreflex control over SNA would not be uniform during dynamic exercise at different intensities.
Linear relationships between total MSNA and DAP in a representative subject under the indicated conditions during an incremental dynamic exercise protocol. The symbols indicate the prevailing points. Arterial baroreflex control of MSNA was modulated by changes in exercise intensity. Such alterations in baroreflex function likely involve multiple regulatory factors (e.g., central command, exercise pressor reflex, changes in central blood volume, exercise-induced hyperthermia, etc.) during incremental leg cycling. These findings suggest that sympathetic and cardiovascular responses are continuously regulated to correspond to ongoing workload through integration of the baroreflex and multiple other systems (reproduced from Ichinose et al. 2008)
The mechanisms responsible for the modulation of arterial baroreflex control over MSNA seen during incremental dynamic exercise are uncertain, but they will likely reflect the interactions between the arterial baroreflex and other systems contributing to the regulation of SNA (as seen in Fig. 1). It would be expected that several factors, including central command and peripheral neural inputs that influence the arterial baroreflex function, are gradually activated or modified by the increasing workload during the dynamic exercise (Mitchell 1990; Rowell and O’Leary 1990; Rowell et al. 1996; Gallagher et al. 2001; Iellamo et al. 1997; Potts and Mitchell 1998; McIlveen et al. 2001; Ogoh et al. 2002b; Charkoudian et al. 2004). For example, increasing afferent neural input from active skeletal muscles, reflecting the progressive rise in workload, could be involved in modulating arterial baroreflex control over MSNA. Although the level of dynamic exercise that activates the muscle metaboreflex in humans remains unknown, this reflex is known to be tonically active in dogs at exercise intensities higher than moderate (Wyss et al. 1983; O’Leary and Sheriff 1995). The modulation of arterial baroreflex function during high-intensity and exhausting exercise, which entails resetting MSNA control to higher BPs and MSNA levels and increasing arterial baroreflex gain, are consistent with observations made during isometric exercise and PEMI (Cui et al. 2001; Kamiya et al. 2001; Ichinose et al. 2004c, 2006b; Ogoh et al. 2009). It may be that the muscle metaboreflex is activated at heavy and exhausting leg cycling, which in turn induces the observed modifications in arterial baroreflex function. The modulation of baroreflex function with changes in exercise intensity may play an important role in matching sympathetic and cardiovascular responses to the exercise intensity. As mentioned, peripheral vascular regulation moves to the forefront of maintaining BP when Q approaches its maximum during high-intensity, whole-body dynamic exercise. In that situation, sympathetic baroreflex gain may be enhanced, probably through activation of the muscle metaboreflex, and contribute to preserving fine BP regulation.
Functional importance of the interaction between arterial baroreflex and muscle metaboreflex during high-intensity exercise
As mentioned, in the absence of baroreflex buffering, muscle metaboreflex-induced pressor responses would be up to twice as large as normal, with significant systemic vasoconstriction (Sheriff et al. 1990; Kim et al. 2005). Moreover, important vasoconstriction could even occur in active skeletal muscles and in coronary arteries, which could limit or compromise perfusion and, consequently, O2 delivery to those areas (Mittelstadt et al. 1994; Kim et al. 2005; O’Leary et al. 2007; Ichinose et al. 2010, 2011; Coutsos et al. 2010, 2013). In that case, the muscle metaboreflex would no longer be a flow-raising reflex; instead, activation of this reflex could result in further accumulation of metabolites leading to still more reflexive sympathoexcitation. The resultant vicious cycle could compromise contractile performance of active skeletal muscles as well as the myocardium. Therefore, the baroreflex buffering of the metaboreflex is an important mechanism for preventing such a vicious cycle and regulating the metaboreflex to act as a feedback flow-raising mechanism.
Interestingly, O’Leary and colleagues noted that activation of the muscle metaboreflex during submaximal treadmill exercise in dogs with reduced hindlimb blood flow elicits a pressor response mediated primarily by an increase in Q. However, when the ability to increase Q is limited, such as in heart failure or during maximal exercise, the muscle metaboreflex increases arterial pressure through peripheral vasoconstriction (Hammond et al. 2000; Augustyniak et al. 2001; Ichinose et al. 2012). In addition, muscle metaboreflex function is virtually instantaneously shifted from increasing Q to increasing vasoconstriction when the induced rise in Q is acutely removed (Sheriff et al. 1998; Ichinose et al. 2010). These results indicate that the mechanisms involved in mediating the muscle metaboreflex respond continuously to changes in Q. Although it is not known what causes the shift in the metaboreflex mechanism when the normal rise in Q is impaired, it might be due to a change in the interaction between the metaboreflex and other systems, most likely the baroreflexes. It has been suggested that activation of the muscle metaboreflex resets the arterial baroreflex operating point and function curve to higher BPs and, as a result, autonomic nerve activity is modulated to elevate arterial BP to a new operating pressure (Rowell and O’Leary 1990; Rowell et al. 1996; Raven et al. 1997). As evidenced by the previously mentioned studies of Sheriff et al. (1990) and Kim et al. (2005), muscle metaboreflex activation can increase arterial BP far higher than the operating pressure of the arterial baroreflex. However, the baroreflex buffers the metaboreflex-induced pressor response by inhibiting peripheral vasoconstriction so that arterial BP is maintained at the baroreflex operating pressure. When the ability to increase Q is not limited, activation of the muscle metaboreflex evokes a rise in arterial BP to the new operating pressure by increasing Q, but when the ability to increase Q is impaired, there is no muscle metaboreflex-induced rise in arterial BP via an increase in Q. Consequently, the arterial baroreflex would not act to inhibit peripheral vasoconstriction until the arterial BP exceeded the new operating pressure. In that situation, the muscle metaboreflex could evoke peripheral vasoconstriction.
Because peripheral blood flow capacity within active skeletal muscle can exceed the maximal Q (Andersen and Saltin 1985; Calbet et al. 2004), during maximal whole-body dynamic exercise some system of regulation must be interposed between the heart and the periphery to maintain homeostasis. It has been postulated that the sympathetic nervous system serves to control peripheral vascular conductance and acts to prevent cardiac function from being outstripped by peripheral O2 demands (Calbet et al. 2004; Tschakovsky et al. 2002; Calbet and Joyner 2010): on the one hand, the accumulation of metabolites in exercising muscles causes vasodilation, while on the other hand the metabolites trigger the muscle metaboreflex, thereby increasing sympathetic nerve activity. In that context, the muscle metaboreflex may play a pivotal role as a counterbalance to metabolic vasodilation (Joyner 1991, 1992; Mittelstadt et al. 1994; Daley et al. 2003; Ichinose et al. 2010, 2011). In addition to the direct influence of the muscle metaboreflex on sympathetic activation, this reflex also affects cardiovascular regulation by modulating arterial baroreflex function in a way that helps to maintain the elevated arterial BP. More specifically, enhanced arterial baroreflex-mediated sympathoexcitation and vasoconstriction occurring when metabolites accumulate within muscles (i.e., during activation of the muscle metaboreflex) ought to be an excellent defense against systemic hypotension induced by metabolic vasodilation. Interaction between the arterial baroreflex and muscle metaboreflex would thus provide an important functional link between metabolism within active muscles and BP control, which would contribute to cardiovascular regulation during exercise.
Interestingly, moreover, the changes in arterial baroreflex function that occur with activation of the muscle metaboreflex also occur with unloading of the cardiopulmonary baroreceptors (Bevegård et al. 1977; Ebert 1983; Victor and Mark 1985; Pawelczyk and Raven 1989; Shi et al. 1993, 1997; Ogoh et al. 2002a; Ichinose et al. 2004a, b, 2006a; Ichinose and Nishiyasu 2012), suggesting that in situations such as a posture change and/or hypovolemia during exercise, arterial baroreflex function would change to strengthen the ability to maintain or increase arterial BP through vasoconstriction. During heavy exercise, therefore, the integrated mechanisms governing arterial baroreflex modulation by muscle metaboreflex, perhaps with other neural inputs to the cardiovascular center, would play an important role in mediating the fine and rapid cardiovascular responses that increase the O2 delivery to active muscles and simultaneously maintain systemic BP.
In summary, during high-intensity dynamic exercise, Q and skeletal muscle blood flow increase markedly to meet the need for greater O2 delivery to the active muscles. To maintain blood flow to the brain and to produce the driving pressure necessary to increase blood flow to the skeletal muscles, systemic BP must be appropriately regulated. In this review, we focused on the arterial baroreflex and muscle metaboreflex as the major neural mechanisms regulating BP during high-intensity exercise, and discussed possible integration within and/or across those mechanisms. In the high Q situation that can occur during heavy dynamic exercise, slight changes in TPR can induce large changes in BP, suggesting that rapid and fine regulation are necessary to avoid unacceptable drops in BP. To accomplish this rapid regulation, the function of the arterial baroreflex may be modified in the several ways through activation of the muscle metaboreflex to: (1) speed up the vasoconstrictor response to a BP fall, (2) weaken or abolish the vasodilatory response to a BP rise, (3) increase the likelihood (response incidence) of MSNA burst activity, and (4) augment the gain of the MSNA control. Further, arterial baroreflex modulations through the muscle metaboreflex and/or other neural control mechanisms may also change over the time course of an exercise or with a change in exercise intensity. Thus, the integration of arterial baroreflex modulation with other neural mechanisms would play an important role in cardiovascular control during high-intensity exercise.
References
Adreani CM, Kaufman MP (1998) Effect of arterial occlusion on responses of group III and IV afferents to dynamic exercise. J Appl Physiol 84:1827–1833
Alam M, Smirk FH (1937) Observations in man upon a blood pressure raising reflex arising from the voluntary muscles. J Physiol 89:372–383
Alam M, Smirk FH (1938a) Observations in man on a pulse-accelerating reflex from the voluntary muscles of the legs. J Physiol 92:167–177
Alam M, Smirk FH (1938b) Unilateral loss of a blood pressure raising, pulse accelerating, reflex from voluntary muscle due to a lesion of the spinal cord. Clin Sci (Lond) 3:247–252
Amann M, Runnels S, Morgan DE, Trinity JD, Fjeldstad AS, Wray DW, Reese VR, Richardson RS (2011) On the contribution of group III and IV muscle afferents to the circulatory response to rhythmic exercise in humans. J Physiol 589:3855–3866
Andersen P, Saltin B (1985) Maximal perfusion of skeletal muscle in man. J Physiol 366:233–249
Augustyniak RA, Collins HL, Ansorge EJ, Rossi NF, O’Leary DS (2001) Severe exercise alters the strength and mechanisms of the muscle metaboreflex. Am J Physiol Heart Circ Physiol 280:H1645–H1652
Bergmann C (1847) Über die Verhältnisse der Wärmeökonomie der Thiere zu ihrer Grösse. Göttinger Studien 3(1):595–708
Bevegård S, Castenfors J, Lindblad E, Tranesjö J (1977) Blood pressure and heart rate regulation capacity of the carotid sinus during changes in blood volume distribution in man. Acta Physiol Scand 99:300–312
Calbet JA, Joyner MJ (2010) Disparity in regional and systemic circulatory capacities: do they affect the regulation of the circulation? Acta Physiol 199:393–406
Calbet JA, Jensen-Urstad M, Van Hall G, Holmberg HC, Rosdahl H, Saltin B (2004) Maximal muscular vascular conductances during whole body upright exercise in humans. J Physiol 558:319–331
Charkoudian N, Martin EA, Dinenno FA, Eisenach JH, Dietz NM, Joyner MJ (2004) Influence of increased central venous pressure on baroreflex control of sympathetic activity in humans. Am J Physiol Heart Circ Physiol 287:H1658–H1662
Clifford PS (2011) Local control of blood flow. Adv Physiol Educ 35:5–15
Coutsos M, Sala-Mercado JA, Ichinose M, Li Z, Dawe EJ, O’Leary DS (2010) Muscle metaboreflex-induced coronary vasoconstriction functionally limits increases in ventricular contractility. J Appl Physiol 109:271–278
Coutsos M, Sala-Mercado JA, Ichinose M, Li Z, Dawe EJ, O’Leary DS (2013) Muscle metaboreflex-induced coronary vasoconstriction limits ventricular contractility during dynamic exercise in heart failure. Am J Physiol Heart Circ Physiol. (Epub ahead of print)
Cui J, Wilson TE, Shibasaki M, Hodges NA, Crandall CG (2001) Baroreflex modulation of muscle sympathetic nerve activity during posthandgrip muscle ischemia in humans. J Appl Physiol 91:1679–1686
Daley JC III, Khan MH, Hogeman CS, Sinoway LI (2003) Autonomic and vascular responses to reduced limb perfusion. J Appl Physiol 95:1493–1498
Delius W, Hagbarth KE, Hongell A, Wallin BG (1972) General characteristics of sympathetic activity in human muscle nerves. Acta Physiol Scand 84:65–81
Dempsey JA (2012) New perspectives concerning feedback influences on cardiorespiratory control during rhythmic exercise and on exercise performance. J Physiol 590(17):4129–4144
Dyke CK, Proctor DN, Dietz NM, Joyner MJ (1995) Role of nitric oxide in exercise hyperemia during prolonged rhythmic handgripping in humans. J Physiol 488:259–265
Ebert TJ (1983) Carotid baroreceptor reflex regulation of forearm vascular resistance in man. J Physiol 337:655–664
Eckberg DL, Sleight P (1992) Human baroreflexes in health and disease. Clarendon, Oxford, pp 19–57
Ellsworth ML, Sprague RS (2012) Regulation of blood flow distribution in skeletal muscle: role of erythrocyte-released ATP. J Physiol 590:4985–4991
Ellsworth ML, Forrester T, Ellis CG, Dietrich HH (1995) The erythrocyte as a regulator of vascular tone. Am J Physiol Heart Circ Physiol 269:H2155–H2161
Ellsworth ML, Ellis CG, Goldman D, Stephenson AH, Dietrich HH, Sprague RS (2009) Erythrocytes: oxygen sensors and modulators of vascular tone. Physiology 24:107–116
Fadel PJ, Raven PB (2011) Human investigations into the arterial and cardiopulmonary baroreflexes during exercise. Exp Physiol 97(1):39–50
Fadel PJ, Ogoh S, Watenpaugh DE, Wasmund W, Olivencia-Yurvati A, Smith ML, Raven PB (2001) Carotid baroreflex regulation of sympathetic nerve activity during dynamic exercise in humans. Am J Physiol Heart Circ Physiol 280:H1383–H1390
Fadel PJ, Ogoh S, Keller DM, Raven PB (2003) Recent insights into carotid baroreflex function in humans using the variable pressure neck chamber. Exp Physiol 88(6):671–680
Fagius J, Wallin BG, Sundlof G, Nerhed L, Englesson S (1985) Sympathetic outflow in man after anaesthesia of the glossopharyngeal and vagus nerves. Brain 108:423–438
Fisher JP, Ogoh S, Young CN, Keller DM, Fadel PJ (2007) Exercise intensity influences cardiac baroreflex function at the onset of isometric exercise in humans. J Appl Physiol 103:941–947
Fisher JP, Seifert T, Hartwich D, Young CN, Secher NH, Fadel PJ (2010) Autonomic control of heart rate by metabolically sensitive skeletal muscle afferents in humans. J Physiol 588:1117–1127
Gallagher KM, Fadel PJ, Strømstand M, Ide K, Smith SA, Querry RG, Raven PB, Secher NH (2001) Effects of partial neuromuscular blockade on carotid baroreflex function during exercise in humans. J Physiol 533:861–870
Gilligan DM, Panza JA, Kilcoyne CM, Waclawiw MA, Casino PR, Quyyumi AA (1994) Contribution of endothelium-derived nitric oxide to exercise-induced vasodilation. Circulation 90:2853–2858
González-Alonso J (2012) ATP as a mediator of erythrocyte-dependent regulation of skeletal muscle blood flow and oxygen delivery in humans. J Physiol 590(20):5001–5013
González-Alonso J, Olsen B, Saltin B (2002) Erythrocyte and the regulation of human skeletal muscle blood flow and oxygen delivery: role of circulating ATP. Circ Res 91:1046–1055
Goodwin GM, McCloskey DI, Mitchell JH (1972) Cardiovascular and respiratory responses to changes in central command during isometric exercise at constant muscle tension. J Physiol 226:173–190
Hammond RL, Augustyniak RA, Rossi NF, Churchill PC, Lapanowski K, O’Leary DS (2000) Heart failure alters the strength and mechanisms of the muscle metaboreflex. Am J Physiol Heart Circ Physiol 278:H818–H828
Hickner RC, Fisher JS, Ehsani AA, Kohrt WM (1997) Role of nitric oxide in skeletal muscle blood flow at rest and during dynamic exercise in humans. Am J Physiol 273:H405–H410
Hirai T, Visneski MD, Kearns KJ, Zelis R, Musch TI (1994) Effects of NO synthase inhibition on the muscular blood flow response to treadmill exercise in rats. J Appl Physiol 77:1288–1293
Ichinose M, Nishiyasu T (2005) Muscle metaboreflex modulates the arterial baroreflex dynamic effects on peripheral vascular conductance in humans. Am J Physiol Heart Circ Physiol 288:H1532–H1538
Ichinose M, Nishiyasu T (2012) Arterial baroreflex control of muscle sympathetic nerve activity under orthostatic stress in humans. Front Physiol 3:314. doi:10.3389/fphys.2012.00314.Epub2012Aug7
Ichinose M, Saito M, Wada H, Kitano A, Kondo N, Nishiyasu T (2002) Modulation of arterial baroreflex dynamic response during muscle metaboreflex activation in humans. J Physiol 544:939–948
Ichinose M, Saito M, Kitano A, Hayashi K, Kondo N, Nishiyasu T (2004a) Modulation of arterial baroreflex dynamic response during mild orthostatic stress in humans. J Physiol 557:321–330
Ichinose M, Saito M, Ogawa T, Hayashi K, Kondo N, Nishiyasu T (2004b) Modulation of control of muscle sympathetic nerve activity during orthostatic stress in humans. Am J Physiol 287:H2147–H2153
Ichinose M, Saito M, Wada H, Kitano A, Kondo N, Nishiyasu T (2004c) Modulation of arterial baroreflex control of muscle sympathetic nerve activity by muscle metaboreflex in humans. Am J Physiol Heart Circ Physiol 286:H701–H707
Ichinose M, Saito M, Fujii N, Kondo N, Nishiyasu T (2006a) Modulation of the control of muscle sympathetic nerve activity during severe orthostatic stress. J Physiol 576:947–958
Ichinose M, Saito M, Kondo N, Nishiyasu T (2006b) Time-dependent modulation of arterial baroreflex control of muscle sympathetic nerve activity during isometric exercise in humans. Am J Physiol Heart Circ Physiol 290:1419–1426
Ichinose M, Koga S, Fujii N, Kondo N, Nishiyasu T (2007) Modulation of the spontaneous beat-to-beat fluctuations in peripheral vascular resistance during activation of muscle metaboreflex. Am J Physiol Heart Circ Physiol 293:H416–H424
Ichinose M, Saito M, Fujii N, Ogawa T, Hayashi K, Kondo N, Nishiyasu T (2008) Modulation of the control of muscle sympathetic nerve activity during incremental leg cycling. J Physiol 586:2753–2766
Ichinose M, Sala-Mercado JA, Coutsos M, Li Z, Ichinose TK, Dawe E, O’Leary DS (2010) Modulation of cardiac output alters the mechanisms of the muscle metaboreflex pressor response. Am J Physiol Heart Circ Physio 298:H245–H250
Ichinose M, Delliaux S, Watanabe K, Fujii N, Nishiyasu T (2011) Evaluation of muscle metaboreflex function through graded reduction in forearm blood flow during rhythmic handgrip exercise in humans. Am J Physiol Heart Circ Physiol 301:H609–H616
Ichinose M, Sala-Mercado JA, Coutsos M, Li Z, Ichinose TK, Dawe E, Fano D, O’Leary DS (2012) Dynamic cardiac output regulation at rest, during exercise, and muscle metaboreflex activation: impact of congestive heart failure. Am J Physiol Regul Integr Comp Physiol 303:R757–R768
Iellamo F, Legramante JM, Raimondi G, Peruzzi G (1997) Baroreflex control of sinus node during dynamic exercise in humans: effects of central command and muscle reflexes. Am J Physiol Heart Circ Physiol 272:1157–1164
Ishii K, Liang N, Oue A, Hirasawa A, Sato K, Sadamoto T, Matsukawa K (2012) Central command contributes to increased blood flow in the noncontracting muscle at the start of one-legged dynamic exercise in humans. J Appl Physiol 112(12):1961–1974
Joyner MJ (1991) Does the pressor response to ischemic exercise improve blood flow to contracting muscles in humans? J Appl Physiol 71:1496–1501
Joyner MJ (1992) Muscle chemoreflexes and exercise in humans. Clin Auton Res 2:201–208
Joyner MJ, Wilkins BW (2007) Exercise hyperaemia: is anything obligatory but the hyperaemia? J Physiol 583(3):855–860
Kamiya A, Michikami D, Qi Fu, Niimi Y, Iwase S, Mano T, Suzumura A (2001) Static handgrip exercise modifies arterial baroreflex control of vascular sympathetic outflow in humans. Am J Physiol Regul Integr Comp Physiol 281:R1134–R1139
Keller DM, Fadel PJ, Ogoh S, Brothers RM, Hawkins M, Olivencia-Yurvati A, Raven PB (2004) Carotid baroreflex control of leg vasculature in exercising and non-exercising skeletal muscle in humans. J Physiol 561:283–293
Kienbaum P, Karlsson T, Sverrisdottir YB, Elam M, Wallin BG (2001) Two sites for modulation of human sympathetic activity by arterial baroreceptors? J Physiol 531:861–869
Kim JK, Sala-Mercado JA, Rodriguez J, Scislo TJ, O’Leary DS (2005) Arterial baroreflex alters strength and mechanisms of muscle metaboreflex during dynamic exercise. Am J Physiol Heart Circ Physiol 288:H1374–H1380
Komine H, Matsukawa K, Tsuchimochi H, Murata J (2003) Central command blunts the baroreflex bradycardia to aortic nerve stimulation at the onset of voluntary static exercise in cats. Am J Physiol Heart Circ Physiol 285:H516–H526
Krogh A, Lindhard J (1913) The regulation of respiration and circulation during the initial stages of muscular work. J Physiol 47:112–136
Krogh A, Lindhard J (1917) A comparison between voluntary and electrically induced muscular work in man. J Physiol 51:182–201
Laughlin MH (1987) Skeletal muscle blood flow capacity: role of muscle pump in exercise hyperemia. Am J Physiol Heart Circ Physiol 253:H993–H1004
Laughlin MH, Korthuis RJ, Duncker DJ, Brade RJ (1996) Control of blood flow to cardiac and skeletal muscle during exercise. Handbook of physiology. In: Rowell LB, Shepherd JT (eds). Exercise: regulation and integration of multiple systems (Sect. 12, chap 16). American Physiology Society, Bethesda, pp 705–769
Macefield VG, Wallin BG (1999) Firing properties of single vasoconstrictor neurons in human subjects with high levels of muscle sympathetic activity. J Physiol 516:293–301
Manica G, Mark L (1983) Arterial baroreflexes in humans. In: Handbook of physiology. The cardiovascular system, peripheral circulation and organ blood flow (Sect. 2, vol 3, Pt 2). American Physiological Society, Bethesda, pp 755–793
Matsukawa K (2011) Central command: control of cardiac sympathetic and vagal efferent nerve activity and the arterial baroreflex during spontaneous motor behaviour in animals. Exp Physiol 97(1):20–28
Matsukawa K, Ishii K, Kadowaki A, Liang N, Ishida T (2012) Differential effect of central command on aortic and carotid sinus baroreceptor-heart rate reflexes at the onset of spontaneous, fictive motor activity. Am J Physiol Heart Circ Physiol 303(4):H464–H474
McCloskey DI, Mitchell JH (1972) Reflex cardiovascular and respiratory responses originating in exercising muscle. J Physiol 224:173–186
McIlveen SA, Shawn GH, Kaufman MP (2001) Both central command and exercise pressor reflex rest carotid sinus baroreflex. Am J Physiol Heart Circ Physiol 280:1451–1463
Miki K, Yoshimoto M, Tanimizu M (2003) Acute shifts of baroreflex control of renal sympathetic nerve activity induced by treadmill exercise in rats. J Physiol 548:313–322
Mitchell JH (1990) Neural control of the circulation during exercise. Med Sci Sports Exerc 22:141–154
Mitchell J, Kaufman M, Iwamoto G (1983) The exercise pressor reflex: its cardiovascular effects, afferent mechanisms, and central pathways. Annu Rev Physiol 45:229–242
Mittelstadt SW, Bell LB, O’Hagan KP, Clifford PS (1994) Muscle chemoreflex alters vascular conductance in nonischemic exercising skeletal muscle. J Appl Physiol 77:2761–2766
Miyauchi T, Maeda S, Iemitsu M, Kobayashi T, Kumagai Y, Yamaguchi I, Matsuda M (2003) Exercise causes a tissue-specific change of NO production in the kidney and lung. J Appl Physiol 94:60–68
Mortensen SP, González-Alonso J, Bune LT, Saltin B, Pilegaard H, Hellsten Y (2009) ATP-induced vasodilation and purinergic receptors in the human leg: roles of nitric oxide, prostaglandins, and adenosine. Am J Physiol Regul Integr Comp Physiol 296:R1140–R1148
Murphy MN, Mizuno M, Mitchell JH, Smith SA (2011) Cardiovascular regulation by skeletal muscle reflexes in health and disease. Am J Physiol Heart Circ Physiol 301:H1191–H1204
Nishiyasu T, Tan N, Morimoto K, Nishiyasu M, Yamaguchi Y, Murakami N (1994a) Enhancement of parasympathetic cardiac activity during activation of muscle metaboreflex in humans. J Appl Physiol 77:2778–2783
Nishiyasu T, Ueno H, Nishiyasu M, Tan N, Morimoto K, Morimoto A, Deguchi T, Murakami N (1994b) Relationship between mean arterial pressure and muscle cell pH during forearm ischemia after sustained handgrip. Acta Physiol Scand 151:143–148
Node K, Kitakaze M, Sato H, Koretsune Y, Katsube Y, Karita M, Kosaka H, Hori M (1997) Effect of acute dynamic exercise on circulating plasma nitric oxide level and correlation to norepinephrine release in normal subjects. Am J Cardiol 79:526–528
Ogoh S, Fadel PJ, Wasmund WL, Raven PB (2002a) Haemodynamic changes during neck pressure and suction in seated and supine positions. J Physiol 540:707–716
Ogoh S, Wasmund WL, Keller DM, Yurvati AO, Gallagher KM, Mitchell JH, Raven PB (2002b) Role of central command in carotid baroreflex resetting in humans during static exercise. J Physiol 543:349–364
Ogoh S, Fisher JP, Raven PB, Fadel PJ (2007) Arterial baroreflex control of muscle sympathetic nerve activity in the transition from rest to steady-state dynamic exercise in humans. Am J Physiol Heart Circ Physiol 293:H2202–H2209
Ogoh S, Fisher JP, Young CN, Raven PB, Fadel PJ (2009) Transfer function characteristics of the neural and peripheral arterial baroreflex arcs at rest and during postexercise muscle ischemia in humans. Am J Physiol Heart Circ Physiol 296:H1416–H1424
O’Leary DS (1993) Autonomic mechanisms of muscle metaboreflex control of heart rate. J Appl Physiol 74:1748–1754
O’Leary DS, Sheriff DD (1995) Is the muscle metaboreflex important in control of blood flow to ischemic active skeletal muscle? Am J Physiol Heart Circ Physiol 268:H980–H986
O’Leary DS, Sala-Mercado JA, Hammond RL, Ansorge EJ, Kim JK, Rodriguez J, Fano D, Ichinose M (2007) Muscle metaboreflex-induced increases in cardiac sympathetic activity vasoconstrict the coronary vasculature. J Appl Physiol 103:190–194
Palmer RMJ, Ferrige AG, Moncada S (1987) Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327:524–526
Papelier Y, Escourrou P, Helloco F, Rowell LB (1997) Muscle chemoreflex alters carotid sinus baroreflex response in humans. J Appl Physiol 82:577–583
Pawelczyk JA, Raven PB (1989) Reductions in central venous pressure improve carotid baroreflex responses in conscious men. Am J Physiol 257:H1389–H1395
Potts JT, Mitchell JH (1998) Rapid resetting of carotid baroreflex by afferent input from skeletal muscle receptors. Am J Physiol Heart Circ Physiol 275:H2000–H2008
Potts JT, Shi XR, Raven PB (1993) Carotid baroreflex responsiveness during dynamic exercise in humans. Am J Physiol Heart Circ Physiol 265:H1928–H1938
Pryor SL, Lewis SF, Haller RG, Bertocci LA, Victor RG (1990) Impairment of sympathetic activation during static exercise in patients with muscle phosphorylase deficiency (McArdle’s disease). J Clin Invest 85:1444–1449
Radegran G, Blomstrand E, Saltin B (1999) Peak muscle perfusion and oxygen uptake in humans: importance of precise estimates of muscle mass. J Appl Physiol 87:2375–2380
Raven PB, Potts JT, Shi X (1997) Baroreflex regulation of blood pressure during dynamic exercise. Exerc Sport Sci Rev 25:365–389
Remensnyder JP, Mitchell JH, Sarnoff SJ (1962) Functional sympatholysis during muscular activity. Circ Res 11:370–380
Richardson RS, Poole DC, Knight DR, Kurdak SS, Hogan MC, Grassi B, Johnson EC, Kendrick KF, Erickson BK, Wagner PD (1993) High muscle blood flow in man: is maximal O2 extraction compromised? J Appl Physiol 75:1911–1916
Rosenmeier JB, Hansen J, González-Alonso J (2004) Circulating ATP-induced vasodilatation overrides sympathetic vasoconstrictor activity in human skeletal muscle. J Physiol 558:351–365
Rosenmeier JB, Yegutkin GG, González-Alonso J (2008) Activation of ATP/UTP-selective receptors increases blood flow and blunts sympathetic vasoconstriction in human skeletal muscle. J Physiol 586:4993–5002
Rowell LB, O’Leary DS (1990) Reflex control of the circulation during exercise: chemoreflex and mechanoreflexes. J Appl Physiol 69:407–418
Rowell LB, O’Leary DS, Kellogg DL (1996) Integration of cardiovascular control systems in dynamic exercise. Handbook of physiology. In: Rowell LB, Shepherd JT (eds). Exercise: regulation and integration of multiple systems (Sect. 12, chap 17). American Physiology Society, Bethesda, pp 770–838
Sagawa K (1983) Baroreflex control of systemic arterial pressure and vascular beds. In: Handbook of physiology. The cardiovascular system. peripheral circulation and organ blood flow (Sect. 2, vol 3, Pt 2). American Physiological Society, Bethesda, pp 453–496
Saito M, Mano T, Iwase S (1989) Sympathetic nerve activity related to local fatigue sensation during static contraction. J Appl Physiol 67:980–984
Saltin B, Radegran G, Koskolou MD, Roach RC (1998) Skeletal muscle blood flow in humans and its regulation during exercise. Acta Physiol Scand 162:421–436
Scherrer U, Pryor SL, Bertocci LA, Victor RG (1990) Arterial baroreflex buffering of sympathetic activation during exercise-induced elevations in arterial pressure. J Clin Invest 86:1855–1861
Seals DR, Chase PB, Taylor JA (1988) Autonomic mediation of the pressor responses to isometric exercise in humans. J Appl Physiol 64:2190–2196
Secher NH, Clausen JP, Klausen K, Noer I, Trap-Jensen J (1977) Central and regional circulatory effects of adding arm exercise to leg exercise. Acta Physiol Scand 100:288–297
Shepherd JT (1983) Circulation to skeletal muscle. In: Shepherd JT, Abboud FM (eds). Handbook of physiology. The cardiovascular system, peripheral circulation and organ blood flow (Sect. 2, vol III). American Physiological Society, Bethesda, pp 319–370
Sheriff DD, O’Leary DS, Scher AM, Rowell LB (1990) Baroreflex attenuates pressor response to graded muscle ischemia in exercising dogs. Am J Physiol Heart Circ Physiol 258:H305–H310
Sheriff DD, Augustyniak RA, O’Leary DS (1998) Muscle chemoreflex-induced increases in right atrial pressure. Am J Physiol Heart Circ Physiol 275:H767–H775
Shi X, Potts JT, Foresman BH, Raven PB (1993) Carotid baroreflex responsiveness to lower body positive pressure-induced increase in central venous pressure. Am J Physiol 265:H918–H922
Shi X, Foresman BH, Raven PB (1997) Interaction of central venous pressure, intramuscular pressure, and carotid baroreflex function. Am J Physiol 272:H1359–H1363
Sprague RS, Ellsworth ML, Stephenson AH, Kleinhenz ME, Lonigro AJ (1998) Deformation-induced ATP release from red blood cells requires cystic fibrosis transmembrane conductance regulator activity. Am J Physiol Heart Circ Physiol 275:H1726–H1732
Sundlof G, Wallin BG (1978) Human muscle nerve sympathetic activity at rest. Relationship to blood pressure and age. J Physiol 274:621–637
Tschakovsky ME, Sujirattanawimol K, Ruble SB, Valic Z, Joyner MJ (2002) Is sympathetic neural vasoconstriction blunted in the vascular bed of exercising human muscle? J Physiol 541:623–635
Victor RG, Mark AL (1985) Interaction of cardiopulmonary and carotid baroreflex control of vascular resistance in humans. J Clin Invest 76:1592–1598
Victor RG, Bertocci LA, Pryor SL, Nunnally RL (1988) Sympathetic nerve discharge is coupled to muscle cell pH during exercise in humans. J Clin Invest 82:1301–1305
Wallin BG, Eckberg DL (1982) Sympathetic transients caused by abrupt alterations of carotid baroreceptor activity in humans. Am J Physiol Heart Circ Physiol 242:185–190
Wallin BG, Sundlof G, Delius W (1975) The effect of carotid sinus nerve stimulation on muscle and skin nerve sympathetic activity in man. Pflügers Arch 358:101–110
Watanabe K, Ichinose M, Fujii N, Matsumoto M, Nishiyasu T (2010) Individual differences in the heart rate response to activation of the muscle metaboreflex in humans. Am J Physiol Heart Circ Physiol 299:H1708–H1714
Wyss CR, Ardell JL, Scher AM, Rowell LB (1983) Cardiovascular responses to graded reductions in hindlimb perfusion in exercising dogs. Am J Physiol Heart Circ Physiol 245:H481–H486
Yang Z, Richard V, Segesser L, Bauer E, Stulz P, Turina M, Lüscher TF (1990) Threshold concentrations of endothelin-1 potentiate contractions to norepinephrine and serotonin in human arteries. A new mechanism of vasospasm? Circulation 82:188–195
Acknowledgments
We would like to sincerely thank the many subjects who have participated in our experiments over the years and also our collaborators. This study was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Nigel A.S. Taylor.
Rights and permissions
About this article
Cite this article
Ichinose, M., Maeda, S., Kondo, N. et al. Blood pressure regulation II: what happens when one system must serve two masters—oxygen delivery and pressure regulation?. Eur J Appl Physiol 114, 451–465 (2014). https://doi.org/10.1007/s00421-013-2691-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-013-2691-y