Abstract
Isometric handgrip (IHG) training lowers resting blood pressure (BP) in both hypertensives and normotensives, yet the effect of training dose on the magnitude of reduction and the mechanisms associated with the hypotensive response are elusive. We investigated, in normotensive women, the effects of two different doses of IHG training on resting BP, and explored improved resistance vessel endothelial function and heart rate variability (HRV) as potential mechanisms of BP reduction. Resting BP, HRV, and resistance vessel endothelial function (venous strain-gauge plethysmography with reactive hyperemia) were assessed in 32 women before and after 4 and 8 weeks of 3×/week (n = 12) or 5×/week (n = 11) IHG training (four, 2-min unilateral contractions at 30 % maximal voluntary contraction), or 0×/week control (n = 9). IHG training decreased systolic BP in the 3×/week (94 ± 6 to 91 ± 6 to 88 ± 5 mmHg, pre- to mid- to post-training; P < 0.01) and 5×/week (97 ± 11 to 90 ± 9 to 91 ± 9 mmHg, P < 0.01) groups, concomitant with increased forearm reactive hyperemic blood flow (26 ± 7 to 30 ± 8 to 36 ± 9 mL/min/100 mL tissue, P < 0.01; and 26 ± 7 to 29 ± 7 to 38 ± 13 mL/min/100 mL tissue, P < 0.01, respectively), yet both remained unchanged in the control group. No changes were observed in diastolic BP, mean arterial BP, or any indices of HRV in any group (all P > 0.05). In conclusion, IHG training lowers resting systolic BP and improves resistance vessel endothelial function independent of training dose in normotensive women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of evidence suggests that isometric handgrip (IHG) training, a simple and time-efficient form of exercise, reduces resting systolic and/or diastolic blood pressure (BP) in men and women with and without hypertension (Badrov et al. 2013; McGowan et al. 2007a, b; Millar et al. 2008, 2012; Peters et al. 2006; Ray and Carrasco 2000; Taylor et al. 2003; Wiley et al. 1992). To date, the effect of altered IHG training dose on resting BP has not been investigated, with current studies employing a wide range of IHG training frequencies (3–5 days per week), durations (45-s to 2-min contractions), intensities (30–50 % maximal voluntary contraction; MVC), and intervention lengths (5–10 weeks). The most widely studied IHG training protocol consists of four, 2-min sustained contractions at 30 % of MVC, performed 3 days per week for 8 weeks (McGowan et al. 2007a, b; Millar et al. 2008, 2012; Wiley et al. 1992). In general, training dose is an important determinant of exercise training adaptations. Evidence from aerobic exercise studies demonstrates that higher training frequencies generally elicit greater post-training reductions in resting BP (Jennings et al. 1986; Nelson et al. 1986). Furthermore, work from the isometric leg training literature suggests that training-induced BP reductions are dependent on training intensity (Baross et al. 2012; Wiles et al. 2010). The investigation of IHG training dose-dependent adaptations may be important to formulate the most efficacious training protocol for eliciting BP reductions.
The mechanisms responsible for the hypotensive effects of IHG training remain elusive, but may include augmented autonomic modulation (Millar et al. 2009), improvements in oxidative stress (Peters et al. 2006), and/or improved resistance vessel endothelial function (McGowan et al. 2007a). Augmented resistance vessel endothelial function may be especially important, as the resistance vessels (lumen diameters <400 μm) are primarily responsible for modulating arterial BP, and have been shown to play a significant role in the pathogenesis of chronically elevated BP or hypertension (Schiffrin 2004). Aerobic exercise training improves resistance vessel endothelial function in individuals with and without hypertension (Higashi et al. 1999; Kingwell et al. 1997). To date, the effect of IHG training on resistance vessel endothelial function has not been investigated.
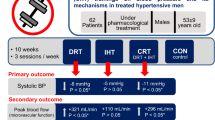
To address these voids in the current IHG literature, we conducted the first randomized controlled trial investigating the effects of two IHG training doses on resting BP, resistance vessel endothelial function, and heart rate variability (HRV, an index of autonomic function). The purpose of the current study was to test the hypotheses that compared to a non-exercising control group: (1) IHG training 5 days per week (IHG5) would elicit greater reductions in resting BP than IHG training 3 days per week (IHG3), and (2) resistance vessel endothelial function and HRV, potential mechanisms for BP reductions, would improve with both IHG3 and IHG5 in normotensive women.
Methods
Participants
Thirty-six women with resting BP within the normal range (i.e., <140 mmHg/<90 mmHg) were recruited from Windsor, ON, Canada. Four individuals voluntarily withdrew from the study, three due to time restraints (three in the control group) and one due to illness (one in the IHG5 group). Participants were excluded if they had hypertension, diabetes, a paced rhythm at rest, frequent ventricular premature beats and heart failure, were current smokers, were post-menopausal or amenorrheic, and/or had physical limitations preventing them from performing IHG exercise. Baseline participant characteristics are displayed in Table 1. All protocols in the investigation were submitted to and approved by the University of Windsor Research Ethics Board. All participants provided written informed consent and were familiarized to all testing procedures prior to study participation.
Study design
Participants were randomized to either IHG3 (n = 12), IHG5 (n = 11) or a non-exercising control group (n = 9). Blind randomization of participants was done via GraphPad software (GraphPad Prism 5; GraphPad Software Inc., La Jolla, CA, USA). Participants assigned to either IHG training groups were instructed on proper IHG exercise technique and were habituated to the IHG protocol, whereas participants assigned to the control group were instructed to maintain their regular routine. Following group assignment, all participants underwent baseline testing procedures to assess, in sequential order, resting BP and heart rate (HR), HRV, and resistance vessel endothelial function, which were repeated after 4 and 8 weeks of IHG training for the training groups, or no training for the control group (i.e., weeks 5 and 9).
IHG training protocol
Participants assigned to the IHG training groups trained 3 or 5 days per week, for a total of 8 weeks. IHG exercise consisted of four, 2-min unilateral contractions, using a programmed handgrip dynamometer (IBX H-101, MD Systems, Inc., Westerville, OH, USA), at 30 % of MVC. MVC was determined at the onset of each IHG exercise bout (via imbedded electronic linear load cells contained within each handgrip) from one maximal contraction performed with the non-dominant hand, as previously established (McGowan et al. 2007a, b). All contractions were performed with the non-dominant hand, and each contraction was separated by a 4-min rest period. In the IHG3 group, participants trained every other day (i.e., Monday, Wednesday, Friday) with rest days interspersed, while IHG5 participants trained for five consecutive days (i.e., Monday–Friday) followed by two rest days. In both IHG training groups, two training sessions per week took place under the direct supervision of an exercise trainer in the Physical Activity and Cardiovascular Research Laboratory at the University of Windsor, while the remaining sessions were completed in the participants’ home. Participants were provided detailed written instructions to ensure proper at-home training. Prior to all on-site training sessions, participants had their resting BP measured (Dinamap Carescape v100, Critikon, Tampa, FL, USA); these data were not used for analysis.
To ensure equal face-time with study investigators, participants in the non-exercising control group visited the laboratory twice a week to have their resting BP measured (Dinamap Carescape v100, Critikon, Tampa, FL, USA); as with the IHG training groups, these data were not used for analysis.
All participants in all groups were given a log book to record any symptoms, and/or changes in exercise, diet, and medication. This was discussed with participants at each laboratory visit to ensure that (1) adverse hypotensive events were monitored, and (2) these potentially confounding factors remained unchanged throughout the intervention period. There were no participant reports of adverse symptoms (i.e., light-headedness, dizziness).
Experimental protocol
To minimize the influence of external variables on all cardiovascular measures, participants were required to refrain from vigorous exercise and alcohol for 24 h prior to each testing session, caffeine for 12 h prior and fast for 4 h prior. All testing was conducted in a quiet, temperature-controlled room (20–24 °C), and participants were asked to void their bladder prior to testing to minimize the effects of bladder distension on resting BP (Fagius and Karhuvaara 1989). To control for the potential influence of hormonal variation on our cardiovascular measures, all participants were tested during the early follicular menstrual cycle phase (if not on oral contraceptives) or low hormone phase (if on triphasic oral contraception) at all time points (Chan et al. 2001). All repeat testing was conducted within 2 h of the initial baseline testing time of day.
Resting blood pressure
Resting BP was measured in the seated position in the brachial artery of the dominant arm using automated brachial oscillometry (Dinamap Carescape v100, Critikon, Tampa, FL, USA), following 10 min of seated rest (Pickering et al. 2005). Participants rested with their dominant arm supported at heart level. The BP cuff was placed approximately 2.5 cm proximal to the antecubital fossa (Pickering et al. 2005). Four BP and HR measurements were obtained by the same trained investigator following 10, 12, 14, and 16 min of rest, and the latter three measures were averaged and used in the final analysis.
Heart rate variability
Beat-to-beat HR was acquired for 10 min during spontaneous breathing, following 20 min of supine rest using single-lead electrocardiography. ECG signal output was sampled at a frequency of 1,000 Hz and low-pass filtered at 40 Hz. Analogue signals were converted to digital signals using a data acquisition board (PowerLab 8/30; ADInstruments Inc., Colorado Springs, CO, USA) for off-line beat-to-beat analysis. Ensemble averages of 256 beat sequences were taken from a minimum time series of 400–500 beats. Ectopic beats were edited and replaced via linear interpolation from adjacent cardiac cycles (McGowan et al. 2009). Tracings with >5 % ectopy-corrected beats were excluded from the analysis (McGowan et al. 2009). Analysis of HRV was conducted using linear (time and frequency domain) and non-linear methodology (Kubios HRV Analysis Software 2.1, Biosignal Analysis and Medical Imaging Group, Department of Applied Physics, University of Eastern Finland, Kuopio, Finland), as described previously in detail (Millar et al. 2012). Briefly, in the time domain, the standard deviation of normal R–R intervals (SDNN), the root mean square of successive R–R interval differences (RMSSD), and the percentage of consecutive R–R intervals that differ by more than 50 ms (pNN50) are reported. In the frequency domain, R–R intervals were analyzed using fast Fourier transformation to assess total power (TP; total power in the spectrum), low-frequency (LF; sympathetic and vagal activity), and high-frequency (HF; vagal activity) power spectral components (Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology 1996). Furthermore, the ratio between LF and HF power (LF:HF), as an estimate of sympathovagal balance, was calculated (Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology 1996). The LF and HF components are presented in both absolute (ln ms2) and normalized units (nu). Non-linear measures assessed include the short-term fractal scaling exponent (α1) and sample entropy. The reliability (coefficient of variation) for SDNN, RMSSD, pNN50, LF, HF, LFnu, HFnu, TP, LF/HF, α1, and sample entropy in our laboratory is 3.3, 2.5, 4.6, 4.1, 1.6, 10.5, 8.7, 1.1, 10.4, 4.6, and 2.5 %, respectively.
Resistance vessel endothelial function
Venous strain-gauge plethysmography with reactive hyperemia, a validated and reproducible non-invasive technique (Higashi et al. 2001; Tousoulis et al. 2005), was used to assess resistance vessel endothelial function. Specifically, forearm blood flow (FBF) was measured via a mercury-filled strain-gauge plethysmograph (Hokanson EC6 Strain Gauge and Photo Plethysmograph, D.E. Hokanson, Inc., Bellevue, WA, USA). In brief, participants’ non-dominant upper-arm was elevated above heart level and fitted with an inflatable cuff (Hokanson SC12D, D.E. Hokanson, Inc., Bellevue, WA, USA). A second inflatable cuff (Hokanson SC5, D.E. Hokanson, Inc., Bellevue, WA, USA) was fitted on the non-dominant wrist and inflated 60 s prior to resting blood flow measurements to a pressure above systolic BP (~200 mmHg) to eliminate the hand circulation from the subsequent measurements. Venous occlusion was achieved by inflating the upper-arm cuff to a pressure below diastolic BP (~50 mmHg), via a rapid cuff inflator (Hokanson E20 Cuff Inflator, D.E. Hokanson, Inc., Bellevue, WA, USA), for intervals of 10 s, followed by 5 s of deflation. FBF was calculated from the mean of approximately three, 15-s cycles of inflation and deflation applied over 1 min. Following the measurement of resting blood flow, forearm ischemia (occlusion of arterial blood flow to the forearm) was achieved by inflating the upper-arm cuff to ~200 mmHg for 5 min. Following release of the cuff, FBF data were collected for an additional 1-min period. FBF is expressed as mL/min/100 mL tissue and is presented as the change from baseline. The intra-observer reproducibility of resistance vessel endothelial function in our laboratory is: 6.6 % (coefficient of variation), 2.2 % (method error), and 0.92 (correlation coefficient). The inter-observer reproducibility of resistance vessel endothelial function in our laboratory is: 4.3 % (coefficient of variation), 10.4 % (method error), and 0.93 (correlation coefficient).
Statistical analysis
To determine sample size, we used previously published data on the mean reduction and standard deviation (SD) of systolic BP (our primary endpoint) in young, normotensive individuals following IHG training (McGowan et al. 2007a). From this work, we anticipated the smallest meaningful difference and SD in systolic BP following IHG training to be 6 ± 4.6 mmHg. Based on an assigned α of 0.05 and β of 0.2, an estimate of 27 participants (i.e., 9 participants per group) was deemed sufficient.
No baseline differences were observed between groups on any variable. However, as the magnitude of systolic BP reductions following IHG training in the current study was related to pre-training systolic BP values (r = −0.59, P < 0.05), analysis of covariance (ANCOVA) was used to analyze changes in resting BP following IHG training, with baseline BP as the covariate. As no associations were noted between initial HRV and resistance vessel endothelial function indices and changes following IHG training (all P > 0.05), changes in HRV and resistance vessel endothelial function were analyzed via a two-way analysis of variance (ANOVA; group × time) with repeated measures. Shapiro–Wilk tests were used to assess normality of HRV measures, with data undergoing logarithmic transformation as necessary. In all cases, Bonferroni’s post hoc procedures were used to evaluate specific differences between means, where applicable. All data were analyzed using STATISTICA (Version 10.0; StatSoft, Inc., Tulsa, OK, USA) software, and statistical significance was set at P ≤ 0.05. Results are mean ± SD, unless otherwise specified.
Results
All baseline characteristics were similar between the IHG3, IHG5, and non-exercising control groups (all P > 0.05). Adherence to the IHG training prescription was 100 % in both IHG training groups. All participants in the IHG3 and IHG5 groups completed 24 and 40 exercise sessions, respectively, over the 8-week intervention period. MVC remained unchanged with both IHG3 [49 ± 9 to 50 ± 10 to 52 ± 13 lbs (pre- to mid- to post-training); P > 0.05] and IHG5 [51 ± 13 to 50 ± 13 to 50 ± 15 lbs (pre- to mid- to post-training); P > 0.05]. There were no reported changes in exercise, diet, and medication throughout the investigation in both the IHG training and non-exercising control groups.
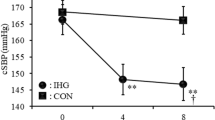
Effects of isometric handgrip training on resting blood pressure
Systolic BP decreased in the IHG3 group [94 ± 6 to 91 ± 6 to 88 ± 5 mmHg (pre- to mid- to post-training)], reaching statistical significance at post-training (P < 0.01), and in the IHG5 group [97 ± 11 to 90 ± 9 to 91 ± 9 mmHg (pre- to mid- to post-training)], reaching statistical significance at mid- (P < 0.01) and post-training (P < 0.01). Systolic BP remained unchanged in the non-exercising control group [94 ± 6 to 94 ± 7 to 96 ± 7 mmHg (pre- to mid- to post-training)] (Fig. 1). In the IHG3 and IHG5 groups, 75 and 78 % of participants, respectively, experienced a clinically relevant reduction (>2 mmHg) in systolic BP (Pescatello et al. 2004).
In contrast, diastolic BP was unchanged in the IHG3 group [57 ± 7 to 56 ± 5 to 54 ± 6 mmHg (pre- to mid- to post-training)], IHG5 group [57 ± 7 to 54 ± 5 to 57 ± 5 mmHg (pre- to mid- to post-training)], and the non-exercising control group [56 ± 3 to 54 ± 6 to 56 ± 4 mmHg (pre- to mid- to post-training)] (all P > 0.05). Mean arterial BP was also unchanged in the IHG3 group [69 ± 6 to 67 ± 4 to 65 ± 4 mmHg (pre- to mid- to post-training)], IHG5 group [70 ± 8 to 66 ± 6 to 68 ± 6 mmHg (pre- to mid- to post-training)], and the non-exercising control group [69 ± 3 to 67 ± 6 to 69 ± 5 mmHg (pre- to mid- to post-training)] (all P > 0.05).
Effects of isometric handgrip training on resting heart rate and heart rate variability
As presented in Table 2, no significant differences were observed in resting HR or any indices of HRV following 4 and 8 weeks of IHG training (IHG3 and IHG5) or non-exercising control (all P > 0.05).
Effects of isometric handgrip training on resistance vessel endothelial function
Forearm reactive hyperemic blood flow increased in the IHG3 group [26 ± 7 to 30 ± 8 to 36 ± 9 mL/min/100 mL tissue (pre- to mid- to post-training)], reaching statistical significance at post-training (P < 0.01), and in the IHG5 group [26 ± 7 to 29 ± 7 to 38 ± 13 mL/min/100 mL tissue (pre- to mid- to post-training)], reaching statistical significance at post-training (P < 0.01). Forearm reactive hyperemic blood flow did not change in the non-exercising control group [28 ± 8 to 29 ± 10 to 27 ± 11 mL/min/100 mL tissue (pre- to mid- to post-training) (P > 0.05)] (Fig. 2).
Discussion
In the present study, we investigated the role of IHG training dose on the magnitude of BP reductions in normotensive women. In contrast to our hypothesis, 8 weeks of IHG3 and IHG5 produced equivalent reductions in resting systolic BP, although increased dose may have a temporal effect, as systolic BP was reduced after 4 weeks of training in the IHG5 group. In an effort to probe the potential mechanisms responsible for the observed reductions in resting BP, we assessed measures of HRV and resistance vessel endothelial function, integral components of BP regulation. Our study demonstrates for the first time that 8 weeks of IHG training potentiates the dilatory capacity of resistance vessels, as evident by a 42 and 57 % increase in the FBF response to reactive hyperemia (IHG3 and IHG5, respectively), providing a biologically plausible mechanism for BP modulation. As in other young normotensive populations, IHG training does not appear to substantially alter autonomic function (Ray and Carrasco 2000; Wiles et al. 2010). Collectively, our findings promote greater understanding of the mechanisms responsible for reductions in BP following IHG training, and will help to develop a training protocol designed to maximize training adaptations.
Effects of isometric handgrip training on resting blood pressure
We primarily sought to determine if a greater dose of IHG training (i.e., IHG5 vs. IHG3) would elicit larger reductions in resting BP. Contrary to our hypothesis, IHG5 did not lead to greater reductions in resting BP vs. IHG3, as both doses of training led to reductions in systolic BP of 6 mmHg. An important novel finding was that the 6 mmHg reduction in systolic BP was achieved after 4 weeks of IHG training in the IHG5 group, with no further reductions following four additional weeks of training, while the 6 mmHg reduction in systolic BP was only noted in the IHG3 group after 8 weeks. This suggests that IHG training-induced reductions in resting BP may be a function of the exposure to the IHG stimulus. Overall, this finding may be critical for the determination of the optimal exercise training dose during initial and maintenance phases.
Our observation of reductions in resting systolic BP after both IHG3 and IHG5 reinforces the concept that this training modality effectively reduces systolic BP in normotensive individuals (McGowan et al. 2007a, Millar et al. 2008, Ray and Carrasco 2000; Wiley et al. 1992). Consistent with these observations, isometric leg training has also demonstrated similar magnitude BP reductions in normotensive samples (Wiles et al. 2010). Of note, this is the lowest initial BP studied to date and the first investigation conducted in normotensive women. This is important, as to date the hypotensive response of IHG training has been primarily studied in predominantly male populations with BP values approximating 120/65 mmHg or greater, and although underrepresented in the current literature, early exploratory evidence suggests that women may be more responsive to the IHG stimulus (Millar et al. 2008).
In contrast to previous research (Taylor et al. 2003; Wiley et al. 1992), reductions in diastolic BP and mean arterial BP were not observed following IHG training. One explanation may be that the participants in these earlier studies had higher initial BP values, and as such, may have had a greater capacity for reduction following IHG training. The high percentage of normotensive participants who experienced clinically relevant modulations in resting BP is confirmatory to the literature (Millar et al. 2008). In contrast, previous studies employing medicated hypertensive patients have reported lower training success rates (McGowan et al. 2007b; Stiller-Moldovan et al. 2012), speculated to be the result of mechanistic interactions with specific anti-hypertensive agents, although these relationships have not yet been explored. Thus, while the most direct application of IHG training is in the hypertensive population, investigations of training protocol specifics may be best carried out in a homogenous normotensive sample.
It is important to note that participants experienced no adverse effects as a result of BP reductions. As such, IHG training may offer a viable tool in the prevention of high BP in normotensive individuals. Strategies aimed at the prevention of high BP applied earlier in life may provide the greatest protection against future hypertension development (Whelton et al. 2002). Our results may also offer clinical implications for individuals with hypertension, as present findings add to the body of literature demonstrating that the magnitude of IHG training-induced BP reductions is related to initial baseline values, whereby patients with higher resting BP experience the largest reductions (Millar et al. 2007).
Effects of isometric handgrip training on heart rate variability
It has been suggested that favorable changes in autonomic modulation may be a potential mechanism by which IHG training reduces resting BP (Millar et al. 2009). HRV represents the oscillation in the interval between consecutive heart beats, and provides insight into cardiac parasympathetic (vagal) and sympathetic modulations (Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology 1996). In the present study, alterations in neither linear nor non-linear measures of HRV were observed following 8 weeks of IHG3 or IHG5, despite significant reductions in systolic BP. These findings are consistent with previous work from our research group in which power spectral analysis of HRV following 8 weeks of IHG training revealed no improvements in older, medicated hypertensives (Millar et al. 2012; Stiller-Moldovan et al. 2012). These findings are also consistent with observations following isometric leg training in normotensive participants (Wiles et al. 2010). In contrast, Taylor et al. (2003) reported improvements in vagal modulation of HR (increased HF power), as well as BP variability (reduced sympathetic vasotone demonstrated by decreased LF power), concomitant with reductions in resting BP following 10 weeks of IHG training in uncontrolled hypertensive patients. Given that hypertension is associated with increased sympathetic activation (Anderson et al. 1989) and dysfunction of vagal HR modulation (Singh et al. 1998), participants in Taylor et al. (2003) may have had greater potential for IHG training-induced improvements in autonomic modulation, in comparison to well-controlled medicated hypertensives in previous work or the normotensive participants used in the current study.
We do acknowledge, however, that HRV is a highly variable measure. As such, future studies, with appropriately powered sample sizes to address changes in autonomic modulation, should further investigate improvements in traditional and non-linear HRV as a potential mechanism of BP change, alongside other indices of autonomic function, including changes in BP variability, direct sympathetic nerve outflow to muscle, organ specific norepinephrine spillover, and/or baroreflex sensitivity.
Effects of isometric handgrip training on resistance vessel endothelial function
Previous work from our research group in hypertensives has demonstrated improved brachial artery flow-mediated dilation (FMD) in both arms following bilateral IHG training, while improvements were confined to the trained limb only following unilateral IHG training (McGowan et al. 2007b). A similar study in normotensives found no changes in brachial artery FMD following unilateral IHG training (McGowan et al. 2007a). As such, a systemic improvement in conduit artery endothelial function is not likely to impact resting BP, which is regulated at the level of the resistance vessels (Schiffrin 2004). Based on increases in peak brachial artery FMD blood flow following 4 weeks of IHG training in normotensive individuals (McGowan et al. 2007a), we hypothesized that reductions in resting BP following IHG training may be associated with improved resistance vessel endothelial function. Our findings support this concept, as forearm reactive hyperemic blood flow increased 42 and 57 % after the 8-week training period in the IHG3 and IHG5 groups, respectively, yet remained unchanged in the non-exercising control group. These findings are consistent and similar in magnitude to those reported following 4–6 weeks of rhythmic handgrip training (Bank et al. 1998), 4 weeks of endurance training (Kingwell et al. 1997), and 12 weeks of whole-body resistance training (Rakobowchuk et al. 2005) in young normotensive participants, and are consistent with the premise that exercise training reduces resting BP through changes in peripheral resistance (Fagard and Cornelissen 2007).
Improvements in resistance vessel endothelial function noted in the present study may be due to increases in the basal production of nitric oxide (Green et al. 2004), and thus, improved nitric oxide-mediated endothelial function of the resistance vessels in the forearm, via an increase in shear stress, as IHG exercise causes repetitive increases in FBF and sympathetic nerve flow. Increases in the basal production of nitric oxide may be the result of improved oxidative stress, which has been noted following IHG training (Peters et al. 2006), as increased oxidative stress plays an important role in the remodeling of resistance vessels (Schiffrin 2004). Reactive oxygen species react vigorously with nitric oxide, reducing subsequent bioavailability. Therefore, reduced oxidative stress following IHG training may lead to an increased bioavailability of basal nitric oxide. Future study is warranted to further investigate the effects of IHG training on resistance vessel endothelial function, simultaneous to the assessment of oxidative stress markers and nitric oxide bioavailability, to determine the mechanisms responsible for post-IHG training increases in forearm reactive hyperemic blood flow.
The improvement in both systolic BP and reactive hyperemic FBF noted in the present study may suggest a role of improved resistance vessel endothelial function as a physiological mechanism of post-IHG training reductions in resting BP. However, as resting BP decreased at 4 weeks with IHG5 without changes in reactive hyperemic FBF, it is likely that improved resistance vessel endothelial function is not a key mechanism of BP change following IHG training. In addition, we did not assess resistance vessel structure, and thus cannot support or refute the influence of structural changes in our observations. Further highlighting the difficulty in probing the mechanisms responsible for the post-IHG training hypotensive response, Wiles et al. (2010) reported a lack of change in both cardiac output and total peripheral resistance following isometric leg training, despite significant reductions in resting BP. As such, it is plausible that the mechanisms of action are multi-factorial, and related to inter-individual genetic and pathological profiles. Further research is needed to conclusively elucidate the exact mechanisms responsible for mediating the change in resting BP following IHG training.
While our results offer many novel and compelling findings, we do recognize certain limitations. First, we acknowledge that the gold standard method for assessing resistance vessel endothelial function is the measurement of FBF using strain-gauge plethysmography in response to the intra-arterial infusion of vasoactive agents (Higashi et al. 2001), and not venous strain-gauge plethysmography with reactive hyperemia, as used in the current investigation. However, we still consider our results valid, as the latter has repeatedly shown to be a valid and reproducible non-invasive tool in the assessment of resistance vessel endothelial function (Higashi et al. 2001; Tousoulis et al. 2005), and is well-correlated with more traditional measures (Higashi et al. 2001). Without the use of agonists to stimulate nitric oxide release, however, we cannot conclude with certainty the role of basal and stimulated nitric oxide release with this technique. Second, measurement of resistance vessel endothelial function was confined to the trained limb only, and therefore, we cannot state with certainty that improvements in resistance vessel endothelial function extend beyond the local vasculature of the IHG trained limb. Finally, the mechanisms responsible for the post-training improvements in resistance vessel endothelial function were not explored in the present study. Future research should aim to investigate the effects of IHG training on systemic resistance vessel endothelial function and explore the mechanisms behind this altered vascular function.
In conclusion, we demonstrate that both IHG3 and IHG5 successfully reduce resting systolic BP in normotensive women, while increased training dose (IHG5) is not associated with a greater magnitude of BP reduction, although it does accelerate the speed of adaptations (i.e., systolic BP reductions at 4 weeks). This finding may be important to determine the most efficacious IHG protocol to maximize BP reductions. Our investigation into potential mechanisms responsible revealed a corresponding improvement in resistance vessel endothelial function, but not HRV, suggesting that improvements in resistance vessel endothelial function may be a contributing factor. It is likely, however, that the mechanistic pathways are multi-factorial and include a combination of both central and peripheral factors. Our results add to the growing body of literature demonstrating the positive effects of IHG training on resting BP and support the need for a large-scale trial designed to further investigate potential mechanisms responsible for IHG training-induced BP adaptations.
References
Anderson E, Sinkey C, Lawton W, Mark A (1989) Elevated sympathetic nerve activity in borderline hypertensive humans. Evidence from direct intraneural recordings. Hypertension 14:177–183
Badrov MB, Millar PJ, Horton S, McGowan CL (2013) Cardiovascular stress reactivity tasks successfully predict the hypotensive response of isometric handgrip training in hypertensives. Psychophysiology 50:407–414
Bank AJ, Shammas RA, Mullen K, Chuang PP (1998) Effects of short-term forearm exercise training on resistance vessel endothelial function in normal subjects and patients with heart failure. J Card Fail 4:193–201
Baross AW, Wiles JD, Swaine IL (2012) Effects of the intensity of leg isometric training on the vasculature of trained and untrained limbs and resting blood pressure in middle-aged men. Int J Vasc Med 2012:964697
Chan NN, MacAllistor RJ, Colhoun HM, Vallance P, Hingorani AD (2001) Changes in endothelium-dependent vasodilation and α-adrenergic responses in resistance vessels during the menstrual cycle in healthy women. J Clin Endorcrinol Metab 86:2499–2504
Fagard RH, Cornelissen G (2007) Effect of exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil 14:12–17
Fagius J, Karhuvaara S (1989) Sympathetic activity and blood pressure increases with bladder distention in humans. Hypertension 14:511–517
Green DJ, Maiorana A, O’driscoll G, Taylor R (2004) Effect of exercise training on endothelium-derived nitric oxide function in humans. J Physiol 561:1–25
Higashi Y, Sasaki S, Sasaki N, Nakagawa K, Ueda T, Yoshimizu A, Kurisu S, Matsuura H, Kajiyama G, Oshima T (1999) Daily aerobic exercise improves reactive hyperemia in patients with essential hypertension. Hypertension 33:591–597
Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Kajiyama G, Oshima T (2001) A noninvasive measurement of reactive hyperemia that can be used to assess resistance artery endothelial function in humans. Am J Cardiol 87:121–125
Jennings G, Nelson L, Nestel P, Esler M, Korner P, Burton D, Bazelmans J (1986) The effects of changes in physical activity on major cardiovascular risk factors, hemodynamics, sympathetic function, and glucose utilization in man: a controlled study of four levels of activity. Circulation 73:30–40
Kingwell B, Sherrard B, Jennings G, Dart A (1997) Four weeks of cycle training increases basal production of nitric oxide from the forearm. Am J Physiol 272:H1070–H1077
McGowan CL, Levy AS, McCartney N, MacDonald MJ (2007a) Isometric handgrip training does not improve flow-mediated dilation in subjects with normal blood pressure. Clin Sci 12:403–409
McGowan CL, Visocchi A, Faulkner M, Verduyn R, Rakobowchuk M, Levy AS, McCartney N, MacDonald MJ (2007b) Isometric handgrip training improves local flow-mediated dilation in medicated hypertensives. Eur J Appl Physiol 99:227–234
McGowan CL, Swiston JS, Notarius S, Mak S, Morris BL, Picton PE, Granton JT, Floras JS (2009) Discordance between microneurographic and heart-rate spectral indices of sympathetic activity in pulmonary arterial hypertension. Heart 95:754–758
Millar PJ, Bray SR, McGowan CL, MacDonald MJ, McCartney N (2007) Effects of isometric handgrip training among people medicated for hypertension: a multilevel analysis. Blood Press Monit 12:307–314
Millar PJ, Bray SR, MacDonald MJ, McCartney N (2008) The hypotensive effects of isometric handgrip training using an inexpensive spring handgrip training device. J Cardiopulm Rehabil Prev 28:203–207
Millar PJ, Bray SR, MacDonald MJ, McCartney N (2009) Isometric handgrip exercise improves acute neurocardiac regulation. Eur J Appl Physiol 107:509–515
Millar PJ, Levy AS, McGowan CL, McCartney N, MacDonald MJ (2012) Isometric handgrip training lowers blood pressure and increases heart rate complexity in medicated hypertensive patients. Scand J Med Sci Sports. doi:10.1111/j.1600-0838.2011.01435.x
Nelson L, Jennings GL, Esler MD, Korner PI (1986) Effect of changing levels of physical activity on blood-pressure and haemodynamics in essential hypertension. Lancet 2:473–476
Pescatello L, Franklin B, Fagard R, Farquhar W, Kelley G, Ray C (2004) Exercise and hypertension. Med Sci Sports Exerc 36:533–553
Peters PG, Alessio HM, Hagerman AE, Ashton T, Nagy S, Wiley RL (2006) Short-term isometric exercise reduces systolic blood pressure in hypertensive adults: possible role of reactive oxygen species. Int J Cardiol 110:199–205
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ (2005) AHA Scientific Statement: recommendations for blood pressure measurement in humans and experimental animals. Hypertension 45:142–161
Rakobowchuk M, McGowan CL, de Groot PC, Hartman JW, Phillips SM, MacDonald MJ (2005) Endothelial function of young, healthy males following whole body resistance training. J Appl Physiol 98:2185–2190
Ray CA, Carrasco DI (2000) Isometric handgrip training reduces arterial pressure at rest without changes in sympathetic nerve activity. Am J Physiol Heart Circ Physiol 279:H245–H249
Schiffrin E (2004) Remodeling of resistance arteries in essential hypertension and effects of antihypertensive treatment. Am J Hypertens 17:1192–1200
Singh JP, Larson MG, Tsuiji H, Evans JC, O’Donnell CJ, Levy D (1998) Reduced heart rate variability and new onset hypertension. Insights into pathogenesis of hypertension: the Framingham Heart Study. Hypertension 32:293–297
Stiller-Moldovan C, Kenno K, McGowan CL (2012) Effects of isometric handgrip training on blood pressure (resting and 24 h ambulatory) and heart rate variability in medicated hypertensive patients. Blood Press Monit 17:55–61
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93:1043–1065
Taylor AC, McCartney N, Kamath MV, Wiley RL (2003) Isometric training lowers resting blood pressure and modulates autonomic control. Med Sci Sports Exerc 35:251–256
Tousoulis D, Antoniades C, Stefanadis C (2005) Evaluating endothelial function in humans: a guide to invasive and non-invasive techniques. Heart 91:553–558
Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC, Karimbakas J (2002) Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA 288:1882–1888
Wiles JD, Coleman DA, Swaine IL (2010) The effects of performing isometric handgrip training at two exercise intensities in healthy young males. Eur J Appl Physiol 108:419–428
Wiley RL, Dunn CL, Cox RH, Hueppchen NA, Scott MS (1992) Isometric exercise training lowers resting blood pressure. Med Sci Sports Exerc 24:749–754
Acknowledgments
The authors would like to thank Don A. Clarke for his technical assistance. The IHG dynamometers used in this study were donated by Zona Health (Boise, Idaho, USA). This work was supported by the University of Windsor (Grant #s 810043; 809264; 808316; CLM), the Canadian Institutes of Health Research (Frederick Banting and Charles Best Canada Graduate Master’s Scholarship; CLB), Heart and Stroke/Richard Lewar Centre of Excellence Postdoctoral Fellowship (PJM), and an Ontario Graduate Scholarship (MBB).
Conflict of interest
Philip J. Millar has received a speaker honorarium from Zona Health (Boise, Idaho, USA).
Ethical standards
The current experiment complies with the current laws of the country in which they were performed (Canada).
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Keith Phillip George.
Rights and permissions
About this article
Cite this article
Badrov, M.B., Bartol, C.L., DiBartolomeo, M.A. et al. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol 113, 2091–2100 (2013). https://doi.org/10.1007/s00421-013-2644-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-013-2644-5