Abstract
The post-exercise period is associated with hypotension, and an increased risk of syncope attributed to decreases in venous return and/or vascular resistance. Increased local and systemic vasodilators, sympatholysis, and attenuated baroreflex sensitivity following exercise are also manifest. Although resting cerebral blood flow is maintained, cerebrovascular regulation to acute decreases in blood pressure has not been characterized following exercise. We therefore aimed to assess cerebrovascular regulation during transient bouts of hypotension, before and after 40 min of aerobic exercise at 60 % of estimated maximum oxygen consumption. Beat to beat blood pressure (Finometer), heart rate (ECG), and blood velocity in the middle cerebral artery (MCAv; transcranial Doppler ultrasound) were assessed in ten healthy young humans. The MCAv-mean arterial pressure relationship during a pharmacologically (i.v. sodium nitroprusside) induced transient hypotension was assessed before and at 10, 30, and 60 min following exercise. Despite a significant reduction in mean arterial pressure at 10 min post-exercise (−10 ± 6.9 mmHg; P < 0.05) and end-tidal PCO2 (10 min post: −2.9 ± 2.6 mmHg; 30 min post: −3.9 ± 3.5 mmHg; 60 min post: −2.7 ± 2.0 mmHg; all P < 0.05), neither resting MCAv nor the cerebrovascular response to hypotension differed between pre- and post-exercise periods (P > 0.05). These data indicate that cerebrovascular regulation remains intact following a moderate bout of aerobic exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The period following aerobic exercise typically exhibits arterial hypotension (Piepoli et al. 1993), orthostatic intolerance (Murrell et al. 2007), and in some cases, loss of consciousness (syncope) (Gratze et al. 2008a, b). Although syncope is fundamentally due to inadequate cerebral perfusion, cerebrovascular regulation during dynamic changes in blood pressure has been subject of limited study. Regardless of the efficacy of cerebrovascular control per se, cardiovascular control is clearly implicated in the aetiology of syncope, as a significant drop in perfusion pressure will produce cerebral hypoperfusion. The numerous changes to cardiovascular function following exercise have been well documented. Both cardiac and vascular baroreflex sensitivities are reduced (Halliwill et al. 1996a, b) with concomitant vascular sympatholysis (Halliwill 2001, Halliwill et al. 1996a); widespread local and systemic release of a diverse array of vasodilators such as nitric oxide, prostaglandins and histamine manifest (Charkoudian et al. 2005b; Green et al. 2010; Halliwill 2001, 2003; Rudas et al. 1999); and, there is likely an attenuated myogenic response to increased arterial shear stress (Dawson et al. 2008). Whether these vascular changes are also manifest in the cerebrovasculature is unknown.
The cerebrovasculature is endowed with intrinsic regulatory mechanisms that serve to maintain adequate brain perfusion in the face of changing perfusion pressure (Lucas et al. 2010; Paulson et al. 1990). Cerebral autoregulation (CA), the term for this apparent regulation, is likely a regulatory amalgamation of metabolic (Ogoh and Ainslie 2009), myogenic (Chan et al. 2011; Tzeng et al. 2011), and neurogenic mechanisms (Ainslie 2009) that produce alterations in cerebrovascular resistance/conductance (Ainslie and Tzeng 2010) and/or compliance (Tzeng et al. 2011). Cerebral autoregulation shows plasticity or impairment under physiological stress [e.g., exposure to high altitude (Subudhi et al. 2009, 2010, 2011), exercise (Ogoh and Ainslie 2009)], or with pathology [e.g., stroke (Aries et al. 2010) and vascular dementia (Claassen and Zhang 2011)].
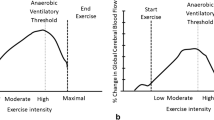
Our understanding of cerebral hemodynamics in the period immediately post-exercise is very limited—three studies have found no change in CA following endurance exercise, and two studies have reported impaired CA following short high-intensity exercise. Following mountain marathons, Murrell et al. (2007, 2009) reported unaltered CA as assessed by transfer function analysis (TFA). Ogoh et al. (2007) found maintained CA using TFA following 10 min of moderate intensity cycling. Conversely, a recent study reported impaired CA following maximal exercise, as assessed by the rate of regulation during suprasystolic thigh-cuff release (Bailey et al. 2011). This is broadly consistent with Ogoh et al. (2005) who reported augmented TFA gain, indicative of impaired CA, following brief (6–8 min) heavy cycling exercise to exhaustion. The disparate findings between these studies could be due to different methods of CA assessment, or the different types of exercise utilized, but regardless, the state of cerebrovascular regulation following exercise remains equivocal.
The aim of the present study was to assess CA during a rapid pharmacologically induced decrease in mean arterial pressure following an exercise bout of intensity and duration consistent with daily physical activity guidelines (Warburton et al. 2010). CA was indexed as the middle cerebral artery velocity (MCAv)–blood pressure relationship (Tzeng et al. 2010c). We sought to evaluate CA before exercise and during the hypotensive phase following aerobic exercise. Given the propensity for syncope (Gratze et al. 2008a, b) and peripheral vascular regulatory changes manifest after exercise, we hypothesized that CA would be impaired following 40 min of moderate intensity cycling.
Methods
Subjects
The study was approved by the New Zealand Central Regional Ethics Committee and conformed to the standards set by the Declaration of Helsinki. 12 healthy subjects [6 male; aged 25.2 ± 6.0 (mean ± SD) range 17–36; body mass index 22.8 ± 3.0 kg m−2] were recruited to the study. All subjects were screened for carotid stenosis, and were excluded for any history of cardiovascular, respiratory or endocrine diseases, medications, or smoking. Based on a self-reported questionnaire, all participants were recreationally active, and typically engaged in low (e.g., walking) to moderate (e.g., jogging, cycling) intensity aerobic activities 2–3 days/week. The possible risks of the experimental procedures were explained to each participant prior to their giving written informed consent. Approximately 2.5 h prior to arriving in the laboratory volunteers ate a light meal. They abstained from any alcohol consumption at least 24 h prior to the experiment, and had no caffeine on the day of testing.
Study design
This study was designed to assess changes in cardiovagal baroreflex sensitivity (BRS) and cerebrovascular regulation following exercise. As part of a larger study, the former BRS data have been previously published (Willie et al. 2011); therefore, while avoiding any overlap of data presentation, the findings presented herein are the cerebral hemodynamic results.
Measurements
Electrocardiogram, respiratory flow (Hans Rudolph Heated Pneumotach, HR 800), PetCO2 sampled from a facemask (gas analyzer model CD-3A, AEI Technologies, Pittsburgh, PA), non-invasive beat-to-beat blood pressure via finger photoplethysmography (Finometer, TNO-TPD Biomedical Instrumentation), and middle cerebral artery blood velocity (MCAv) (Transcranial 2.5 MHz pulsed Doppler ultrasound; Spencer Technologies, Seattle, WA) were acquired continuously at 1 kHz per channel via an analog-to-digital converter (Powerlab/16SP ML795; ADInstruments, Colorado Springs, CO, USA). Beat-to-beat RRI, HR, and values for systolic (SBP), diastolic (DBP), and mean arterial blood pressure (MAP) were, respectively, determined from the recorded ECG and arterial blood pressure waveforms. To account for potential drift, finger blood pressure measures were verified at the brachial artery in the contralateral arm by sphygmomanometry. All off-line data processing was done using custom written software in LabView 10 (National Instruments, Texas, USA) on a Macintosh 2.26 GHz MacBook Pro computer.
Experimental protocol
All measurements were completed in the supine position in a temperature-controlled laboratory (22–23 °C). Subjects rested supine for 15 min following insertion of a venous cannula in the right or left anticubital vein, and placement of measurement apparatus. 5 min of baseline measurements were recorded prior to one or two bolus injections of sodium nitroprusside (SNP; see “Evaluation of cerebral autoregulation”, below). Subjects were moved to an upright stationary bike for 40 min at 60 % predicted VO2max (Swain et al. 1994); this duration and intensity are sufficient to induce a period of post-exercise hypotension (Charkoudian et al. 2003, 2005a; Halliwill et al. 1996a, b; Somers et al. 1985; Willie et al. 2011). Following exercise, subjects promptly resumed the supine position. SNP injections were conducted at 10, 30, and 60 min post-exercise cessation. Changes in blood pressure often induce concomitant ventilatory changes, and therefore subjects breathed to a metronome during the SNP trials; PetCO2 was maintained within 2 mmHg throughout SNP trials in all subjects. In our experience, paced breathing by rate only does not significantly alter heart rate, SBP, MAP, DBP, tidal volume, or PetCO2 compared to spontaneous breathing (Tzeng et al. 2009), and as such no restrictions were imposed on subjects’ tidal volume.
Evaluation of cerebral autoregulation
The relationship between blood pressure and MCAv mean was assessed during bolus SNP injections (Tzeng et al. 2010b) performed on each subject both before and after exercise, as detailed previously (Willie et al. 2011). Briefly, the test consisted of a 50–250 μg i.v. bolus injection of SNP, followed 1-min later by a 150–300 μg bolus of phenylephrine hydrochloride. The regression slope of the MAP–MCAv relationship, where MAP was decreasing linearly, as identified statistically using piecewise linear regression (Taylor et al. 2011), was taken as an index of CA. Because selection of the linear portion of the curve is done automatically, as opposed to visual delineation by the investigator, this method of slope calculation removes investigator bias from analysis of CA gains. To account for respiratory-induced oscillations in MAP, blood pressure was binned over 2 mmHg increments, and the MAP–MCAv relationship plotted in-phase as this yielded the greatest correlation coefficients. This analysis gives gain (G) values, where G = 0 indicates perfect buffering of blood flow, whereas G = 1 indicates a purely pressure passive relationship, and G > 1, where MCAv falls more rapidly than MAP, and therefore a severely reduced CA capacity. We have previously demonstrated that this method of CA quantification produces similar results as CA assessed with a sit to stand maneuver, and is correlated with CA quantified using the rate of regulation (Aaslid et al. 1989) or autoregulatory index (Tiecks et al. 1995) following rapid deflation of suprasystolic thigh-cuffs (Tzeng et al. 2010c). Moreover, this method has the advantage of not inducing pain, as does the thigh-cuff inflation/deflation method.
Statistics
Based on the previous studies of large reductions in BRS following exercise (Charkoudian et al. 2003; Halliwill 2001; Willie et al. 2011) and assuming similar magnitudinal changes in CA, we estimated that a sample of 10 would provide 80 % power to detect a significant difference at an alpha of 0.05.
All data were assessed for parity with a normal distribution using Shapiro–Wilks test. There were no statistical differences in CA values between males and females; therefore, data were pooled for statistical analysis. One way repeated measures ANOVA were used to assess differences across conditions (Greenhouse–Geiser corrected). The Fisher transformation was used on the coefficients of determination (R 2) for MAP–MCAv regression (CA) gains prior to ANOVA. A priori defined comparisons between pre and post-exercise values were made using the Dunnets test. Alpha was set to 0.05. Statistical analyses were completed with SPSS 16.0.2 (SPSS Inc.) and Prism 4.0 (Graphpad Software, Inc., La Jolla CA, USA).
Results
Subjects
In one female subject, a drop of ~15 mmHg MAP was not attainable before exercise even with increased SNP doses; and, one male subject did not respond to SNP at 30 min post-exercise. Both subjects were excluded and the analysis was based on n = 10 (5 females).
Hemodynamics
Mean resting values over the 15 s preceding each SNP bolus are shown in Table 1. Following exercise, HR was increased and remained elevated through 60 min post-exercise. Although DBP did not change following exercise, both SBP (at 10 and 30 min) and MAP were reduced at 10-min post-exercise (P < 0.05).
Cerebrovascular hemodynamics
Figure 1 and Table 2 show baseline and post-exercise CA; coefficients of determination are also shown in Table 2. CA gain was not different from the pre-exercise mean (0.60 ± 0.17 cm s−1 mmHg−1) at any point (P = 0.262). Table 2 also shows the changes in MCAv, PetCO2, and MAP incurred with SNP administration. None were different before or after exercise with the exception of a blunted drop in MAP at 10 min post-exercise (−13.8 ± 5.1 mmHg at 10 min post-exercise, versus −19.3 ± 4.9, −17.6 ± 3.4, and −17.8 ± 5.5 mmHg pre-exercise, 30 and 60 min post-exercise, respectively). Despite hypotension and maintained reductions (P < 0.05) in PetCO2 following exercise, MCAv was not significantly different at any point (Table 1). A linear regression of the percentage change from baseline values at each time point following exercise between MCAv with PetCO2 and between CA and MAP yielded no significant relationships (P > 0.05). The two subjects with the greatest CA (see Fig. 1) at 10 min post-exercise were both young females, with low resting MAP. They were not statistically significant outliers, and their removal from the data set did not change any of the values or relationships described above. Consequently, they were included in the dataset.
Discussion
In this study, we aimed to characterize the cerebrovascular response to pharmacologically induced transient hypotensive episodes before and within 1 h after aerobic exercise. In contrast to our hypothesis, we found that CA was not impaired following exercise. Interestingly, we observed that resting MCAv was well maintained during the post-exercise period despite two factors that are known to reduce CBF: hypotension and hypocapnia.
Cerebral perfusion following exercise
Few studies have explicitly assessed brain perfusion or CA following exercise (Smith et al. 2010). Murrell et al. (2007, 2009) studied cardiovascular control and orthostatic tolerance following a mountain marathon using TFA to assess CA. Although time to syncope was reduced post-exercise, there was no difference in transfer function gain or phase following the marathon. A critical consideration, however, is that end-tidal CO2 was not measured, and was likely decreased with hyperventilation during upright tilt (Immink et al. 2006). Hypocapnia has two important implications, a direct reduction in cerebral blood flow (Ainslie and Duffin 2009) and a potentially enhanced CA (Aaslid et al. 1989). Both of these factors will influence the time to syncope, making interpretation of these data in the context of post-exercise cerebrovascular regulation difficult. Considering that cerebral blood flow changes 3–5 % for each 1 mmHg change in PaCO2 (Ainslie and Duffin 2009) and that PetCO2 was reduced by ~4 mmHg at 30 min post-exercise, CBF was well maintained following exercise. Our data are broadly supported by Scott et al. (2008) who observed that PEH did not contribute to orthostatic challenge-associate changes in cerebral tissue oxygenation. Collectively, these data support the notion that CA is unaltered into the post-exercise hypotensive phase.
Cardiovascular control following exercise
Following exercise, there are numerous cardiac and vascular alterations that affect the control of blood pressure, particularly in response to an orthostatic challenge. Following 30–60 min of aerobic exercise, normotensive individuals exhibit a drop in MAP of 5–10 mmHg lasting almost 2 h; these reductions may be more marked and last for longer in hypertensive individuals (Halliwill 2001). This period is associated with attenuated sympathetic vascular BRS (Halliwill et al. 1996a), decreased total sympathetic outflow (Kulics et al. 1999; Piepoli et al. 1993), and blunted transduction of efferent vascular sympathetic nerve activity into peripheral vasoconstriction (Halliwill et al. 1996a). This sympatholysis (and consequent drop in total peripheral resistance) is not fully compensated for by increased heart rate and cardiac output, and also yields a reduced ability to maintain CVP with an orthostatic challenge. Indeed, Murrell et al. (2007) found that stroke volume was significantly reduced following a mountain marathon, yielding a 5 ± 21 % transient decrease in cardiac output upon initial standing versus the 20 ± 19 % increase observed before exercise. The resultant decreased time to syncope during a tilt-test was also found to be unrelated to the magnitude of post-exercise hypotension (Murrell et al. 2010), suggesting the post-exercise disposition to syncope is related to the post-exercise period, not the hypotensive state per se. A number of investigators have reported an independent relationship between cardiac output and stroke volume with CBF, which may be of particular relevance to the cerebrovasculature in the context of transient hypotension. Whereas increased cerebral perfusion pressure can be attenuated through increased resistance/reduced conductance, if perfusion pressure falls too much, no amount of cerebrovascular dilation will maintain brain perfusion. Nonetheless, in the present study, where SNP was utilized to drive acute decreases in blood pressure, the cerebrovasculature itself retains its regulatory capabilities.
Technological considerations
Assessment of CA
We aimed to assess the cerebral hemodynamic response during falling blood pressure. Previous studies have observed both altered (Ogoh et al. 2005) and unaltered (Ogoh et al. 2007) post-exercise CA assessed using TFA. However, the physiological meaning of TFA parameters is equivocal—they provide metrics that describe the temporal and amplitudinal relationship between cerebral perfusion pressure and flow; to what extent transfer function coherence, gain, and phase reflect CA (Zhang et al. 2009; Tzeng et al. 2011) or alter the risk of syncope is unclear. Furthermore, these TFA measures cannot dissociate the cerebrovascular response to rising and falling blood pressure—this is problematic because data indicate CA may be more sensitive to rising than falling arterial blood pressure (Aaslid et al. 2007; Tzeng et al. 2010a); reduced CA efficacy during falling blood pressure is likely of particular relevance to the study of syncope. The present study was designed to investigate CA to falling blood pressure per se, and is the only study that has done so. As such, our findings of no post-exercise change in CA are likely more robust than other studies utilizing spontaneous methods of CA quantification (e.g. Murrell et al. 2007; Ogoh et al. 2005).
The physiological processes that comprise CA are incompletely understood, and subject to constant debate amongst researchers. Cerebral autoregulation is conventionally held to refer to changes in resistance at the level of the pial arterioles; however, there are likely other processes that serve to maintain cerebral perfusion. Because we measured the linear segment of the MAP–MCAv relationship, this value does not necessarily reflect the ability of the cerebrovasculature to actively dilate in response to hypotension, but is rather an index of resistive flow gain. This value does not give a complete description of cerebral autoregulation, but, indeed, there is no “gold-standard” metric of CA; the present method correlates well with other methods of dynamic CA quantification. However, it is nonetheless difficult to interpret any metric of CA because of this mechanistic ambiguity with respect to the physiology of CA. The meaning of the high dispersion of CA at 10 min post-exercise is similarly equivocal. That the magnitude of the post-exercise change in CA gain was not related to the change in MCAv, PetCO2 or MAP suggests a high-degree of inter-subject variability of cerebrovascular regulation following exercise. Thus, future studies attempting to identify the mechanisms of post-exercise syncope need to take this variation into consideration, and must have the means to directly assess the cerebral vessels; neck vascular ultrasound and high-resolution magnetic resonance imaging are likely methodological candidates to address these questions in humans.
Experimental considerations
TCD only gives a reliable index of flow if the MCA diameter does not change; a direct effect of SNP on the cerebrovasculature is a possible confounder. It has been reported, however, that sodium nitroprusside administered during craniotomy did not directly produce changes in MCA diameter (Paulson et al. 1990; Rapela et al. 1967; Robinson et al. 2003). Two studies have found regulation of resistance vessels within the cerebrovasculature to be nitric oxide independent (Joshi et al. 1997; Lavi 2003), indicating there is likely no direct effect of SNP on downstream cerebrovascular resistance. Moreover, BP manipulation with drugs avoids other confounders. Other studies have utilized release of suprasystolic thigh cuffs to elicit a transient hypotension. Thigh-cuff release is likely confounded by pain and associated sympathetic activation, which has been implicated in the cerebrovascular response to hypotension (Ogoh et al. 2008). In our experience, thigh-cuff release does not produce a reliably consistent BP drop. The design of the present study required that the transient hypotension be of a similar magnitude, and at the same time point following exercise in each subject; in this respect we have had previous success with the technique (Tzeng et al. 2010a).
We chose an exercise paradigm sufficient to induce post-exercise hypotension, which is consistent with numerous studies assessing BRS during the post-exercise hypotensive phase, and also with current recommendations for physical activity (Warburton et al. 2010). While these data are consequently difficult to compare with the two studies assessing post-exercise CA, they are perhaps more germane to post-exercise cerebrovascular function in the normal population. Indeed, we cannot extend these findings to aging subjects or those with cardiovascular disease, as stiffer arteries and reduced cardiac function could yield a different CBF response to transient hypotension.
Finally, this study did not actually test CA during post-exercise syncope. MAP was reduced ~15 mmHg and no subject lost consciousness during any of the SNP injections. Thus, while these data elucidate CBF regulation during hypotension following exercise, it is possible that CBF control is differentially altered during syncope per se. Future study of the BP–CBF relationship during actual syncope would address this question.
Conclusion/perspectives
Given its high metabolic demand, reliance on aerobic metabolism and inability to store significant energy substrate, efficacious mechanisms of brain perfusion regulation are quite necessary. Indeed, this regulation is certainly not isolated to mechanisms above the neck: peripheral vascular control serves to maintain blood pressure, cardiac filling and output, each necessary for maintained perfusion pressure to the head. And, while these peripheral regulatory mechanisms have received ample attention during and after exercise, few studies have focused on cerebrovascular regulation post-exercise. The present data indicate that unlike the peripheral vasculature, cerebrovascular function is maintained following exercise.
References
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H (1989) Cerebral autoregulation dynamics in humans. Stroke 20:45–52
Aaslid R, Blaha M, Sviri G, Douville CM, Newell DW (2007) Asymmetric dynamic cerebral autoregulatory response to cyclic stimuli. Stroke 38:1465–1469
Ainslie P (2009) Have a safe night: intimate protection against cerebral hyperperfusion during REM sleep. J Appl Physiol 106:1031–1033
Ainslie P, Duffin J (2009) Integration of cerebrovascular CO2 reactivity and chemoreflex control of breathing: mechanisms of regulation, measurement, and interpretation. AJP: regulatory. Integr Comp Physiol 296:R1473–R1495
Ainslie P, Tzeng Y (2010) On the regulation of the blood supply to the brain: old age concepts and new age ideas. J Appl Physiol 108:1447–1449
Aries MJH, Elting JW, De Keyser J, Kremer BPH, Vroomen PCAJ (2010) Cerebral autoregulation in stroke: a review of transcranial Doppler studies. Stroke 41:2697–2704
Bailey DM, Evans KA, McEneny J, Young IS, Hullin DA, James PE, Ogoh S, Ainslie PN, Lucchesi C, Rockenbauer A, Culcasi M, Pietri S (2011) Exercise-induced oxidative–nitrosative stress is associated with impaired dynamic cerebral autoregulation and blood–brain barrier leakage. Exp Physiol 96(11):1196–1207
Chan GSH, Ainslie PN, Willie CK, Taylor CE, Atkinson G, Jones H, Lovell NH, Tzeng YC (2011) Contribution of arterial Windkessel in low-frequency cerebral hemodynamics during transient changes in blood pressure. J Appl Physiol 110:917–925
Charkoudian N, Halliwill JR, Morgan BJ, Eisenach JH, Joyner MJ (2003) Influences of hydration on post-exercise cardiovascular control in humans. J Physiol (Lond) 552:635–644
Charkoudian N, Eisenach JH, Joyner MJ, Roberts SK, Wick DE (2005a) Interactions of plasma osmolality with arterial and central venous pressures in control of sympathetic activity and heart rate in humans. Am J Physiol Heart Circ Physiol 289:H2456–H2460
Charkoudian N, Joyner MJ, Johnson CP, Eisenach JH, Dietz NM, Wallin BG (2005b) Balance between cardiac output and sympathetic nerve activity in resting humans: role in arterial pressure regulation. J Physiol (Lond) 568:315–321
Claassen JAHR, Zhang R (2011) Cerebral autoregulation in Alzheimer’s disease. J Cerebr Blood Flow Met 31:1572–1577
Dawson EA, Whyte GP, Black MA, Jones H, Hopkins N, Oxborough D, Gaze D, Shave RE, Wilson M, George KP, Green DJ (2008) Changes in vascular and cardiac function after prolonged strenuous exercise in humans. J Appl Physiol (Bethesda, Md: 1985) 105:1562–1568
Gratze G, Mayer H, Luft FC, Skrabal F (2008a) Determinants of fast marathon performance: low basal sympathetic drive, enhanced postcompetition vasodilatation and preserved cardiac performance after competition. Br J Sports Med 42:882–888
Gratze G, Mayer H, Skrabal F (2008b) Sympathetic reserve, serum potassium, and orthostatic intolerance after endurance exercise and implications for neurocardiogenic syncope. Eur Heart J 29:1531–1541
Green DJ, Spence A, Halliwill JR, Cable T, Thijssen D (2010) Exercise and vascular adaptation in asymptomatic humans. Exp Physiol
Halliwill JR (2001) Mechanisms and clinical implications of post-exercise hypotension in humans. Exerc Sport Sci Rev 29:65–70
Halliwill JR, Taylor JA, Eckberg DL (1996a) Impaired sympathetic vascular regulation in humans after acute dynamic exercise. J Physiol (Lond) 495:279–288
Halliwill JR, Taylor JA, Hartwig TD, Eckberg DL (1996b) Augmented baroreflex heart rate gain after moderate-intensity, dynamic exercise. Am J Physiol 270:R420–R426
Halliwill JR, Dinenno FA, Dietz NM (2003) Alpha-adrenergic vascular responsiveness during postexercise hypotension in humans. J Physiol 550:279–286
Immink RV, Secher NH, Roos CM, Pott F, Madsen PL, Van Lieshout JJ (2006) The postural reduction in middle cerebral artery blood velocity is not explained by PaCO2. Eur J Appl Physiol 96:609–614
Joshi S, Young WL, Pile-Spellman J, Fogarty-Mack P, Sciacca RR, Hacein-Bey L, Duong H, Vulliemoz Y, Ostapkovich N, Jackson T (1997) Intra-arterial nitrovasodilators do not increase cerebral blood flow in angiographically normal territories of arteriovenous malformation patients. Stroke 28:1115–1122
Kulics JM, Collins HL, DiCarlo SE (1999) Postexercise hypotension is mediated by reductions in sympathetic nerve activity. Am j physiol 276:H27–H32
Lavi S (2003) Role of nitric oxide in the regulation of cerebral blood flow in humans: chemoregulation versus mechanoregulation. Circulation 107:1901–1905
Lucas SJ, Tzeng YC, Galvin SD, Thomas KN, Ogoh S, Ainslie PN (2010) Influence of changes in blood pressure on cerebral perfusion and oxygenation. Hypertension 55:698–705
Murrell C, Wilson L, Cotter JD, Lucas S, Ogoh S, George K, Ainslie PN (2007) Alterations in autonomic function and cerebral hemodynamics to orthostatic challenge following a mountain marathon. J Appl Physiol 103:88–96
Murrell C, Cotter J, George K, Shave R, Wilson L, Thomas K, Williams M, Lowe T, Ainslie P (2009) Influence of age on syncope following prolonged exercise; differential responses but similar orthostatic intolerance. J Physiol (Lond) 1–11
Murrell CJ, Cotter JD, George K, Shave R, Wilson L, Thomas K, Williams MJA, Ainslie PN (2010) Syncope is unrelated to supine and postural hypotension following prolonged exercise. Eur J Appl Physiol 111:469–476
Ogoh S, Ainslie PN (2009) Cerebral blood flow during exercise: mechanisms of regulation. J Appl Physiol 107:1370–1380
Ogoh S, Dalsgaard MK, Yoshiga CC, Dawson EA, Keller DM, Raven PB, Secher NH (2005) Dynamic cerebral autoregulation during exhaustive exercise in humans. Am J Physiol Heart Circ Physiol 288:H1461–H1467
Ogoh S, Fisher JP, Purkayastha S, Dawson EA, Fadel PJ, White MJ, Zhang R, Secher NH, Raven PB (2007) Increases in central blood volume modulate carotid baroreflex resetting during dynamic exercise in humans. J Appl Physiol (Bethesda, Md : 1985) 102:713–721
Ogoh S, Brothers R, Eubank W, Raven P (2008) Autonomic neural control of the cerebral vasculature: acute hypotension. Stroke 39:1979–1987
Paulson OB, Strandgaard S, Edvinsson L (1990) Cerebral autoregulation. Cerebrovasc Brain Metab Rev 2:161–192
Piepoli M, Coats AJ, Adamopoulos S, Bernardi L, Feng YH, Conway J, Sleight P (1993) Persistent peripheral vasodilation and sympathetic activity in hypotension after maximal exercise. J Appl Physiol 75:1807–1814
Rapela CE, Green HD, Denison ABJ (1967) Baroreceptor reflexes and autorregulation of cerebral blood flow in the dog. Circ Res 21:559–568
Robinson TG, Dawson SL, Eames PJ, Panerai RB, Potter JF (2003) Cardiac baroreceptor sensitivity predicts long-term outcome after acute ischemic stroke. Stroke 34:705–712
Rudas L, Crossman AA, Morillo CA, Halliwill JR, Tahvanainen KU, Kuusela TA, Eckberg DL (1999) Human sympathetic and vagal baroreflex responses to sequential nitroprusside and phenylephrine. Am J Physiol 276:H1691–H1698
Scott JM, Esch BTA, Lusina S-JC, McKenzie DC, Koehle MS, Sheel AW, Warburton DER (2008). Post-exercise hypotension and cardiovascular responses to moderate orthostatic stress in endurance-trained males. Applied physiology, nutrition, and metabolism = Physiologie appliquée, nutrition et métabolisme 33:246–253
Smith JC, Paulson ES, Cook DB, Verber MD, Tian Q (2010) Detecting changes in human cerebral blood flow after acute exercise using arterial spin labeling: implications for fMRI. J Neurosci Methods 191:258–262
Somers VK, Conway J, LeWinter M, Sleight P (1985) The role of baroreflex sensitivity in post-exercise hypotension. J Hypertens Suppl 3:S129–S130
Subudhi AW, Panerai RB, Roach RC (2009). Acute hypoxia impairs dynamic cerebral autoregulation: results from two independent techniques. J Appl Physiol (Bethesda, Md: 1985) 107:1165–1171
Subudhi AW, Panerai RB, Roach RC (2010) Effects of hypobaric hypoxia on cerebral autoregulation. Stroke 41:641–646
Subudhi AW, Dimmen AC, Julian CG, Wilson MJ, Panerai RB, Roach RC (2011) Effects of acetazolamide and dexamethasone on cerebral hemodynamics in hypoxia. J Appl Physiol (Bethesda, Md: 1985) 110(5):1219–1225
Swain DP, Abernathy KS, Smith CS, Lee SJ, Bunn SA (1994) Target heart rates for the development of cardiorespiratory fitness. Med Sci Sports Exerc 26:112–116
Taylor CE, Atkinson G, Willie CK, Jones H, Ainslie PN, Tzeng YC (2011) Diurnal variation in the mechanical and neural components of the baroreflex. Hypertension 58:51–56
Tiecks FP, Lam AM, Aaslid R, Newell DW (1995) Comparison of static and dynamic cerebral autoregulation measurements. Stroke 26:1014–1019
Tzeng YC, Sin PYW, Lucas SJE, Ainslie PN (2009) Respiratory modulation of cardiovagal baroreflex sensitivity. J Appl Physiol 107:718–724
Tzeng Y-C, Willie CK, Atkinson G, Lucas SJE, Wong A, Ainslie PN (2010a) Cerebrovascular regulation during transient hypotension and hypertension in humans. Hypertension 1–7
Tzeng YC, Lucas SJ, Atkinson G, Willie CK, Ainslie PN (2010b) Fundamental relationships between arterial baroreflex sensitivity and dynamic cerebral autoregulation in humans. J Appl Physiol 108:1162–1168
Tzeng YC, Willie CK, Atkinson G, Lucas SJ, Wong A, Ainslie PN (2010c) Cerebrovascular regulation during transient hypotension and hypertension in humans. Hypertension 56:268–273
Tzeng YC, Chan GS, Willie CK, Ainslie PN (2011) Determinants of human cerebral pressure-flow velocity relationships: new insights from vascular modeling and Ca2 + blockade. J Physiol 589:3263–3274
Warburton DER, Charlesworth S, Ivey A, Nettlefold L, Bredin SSD (2010) A systematic review of the evidence for Canada's Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act 7:39
Willie CK, Ainslie PN, Taylor CE, Jones H, Sin PYW, Tzeng YC (2011) Neuromechanical features of the cardiac baroreflex after exercise. Hypertension 57:927–933
Zhang R, Behbehani K, Levine BD (2009) Dynamic pressure–flow relationship of the cerebral circulation during acute increase in arterial pressure. J Physiol (Lond) 587:2567–2577
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Dag Linnarsson.
Rights and permissions
About this article
Cite this article
Willie, C.K., Ainslie, P.N., Taylor, C.E. et al. Maintained cerebrovascular function during post-exercise hypotension. Eur J Appl Physiol 113, 1597–1604 (2013). https://doi.org/10.1007/s00421-012-2578-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-012-2578-3