Abstract
Older adults have an increase in circulating markers of inflammation. The current study examined whether there is an increase in the expression of inflammatory markers within the vastus lateralis, a major locomotive muscle, of older adults, and if so, whether the reduction in muscle strength and aerobic capacity in older adults is related to increased muscle inflammation. Skeletal muscle biopsies were taken from older adults (n = 17, 67 ± 1.6 years) and young individuals (n = 16, 24 ± 0.6 years) under resting and fasting conditions. Muscle was analyzed for mRNA levels of intracellular inflammatory molecules (MCP1, TNFα and IL-1β) and total cellular protein abundance of cytokines, chemokines and kinases (IL-6, IL-8, MCP1, TNFα, p65 (NF-κB), JNK1/2 and STAT3). MCP1 expression was significantly higher (p < 0.05; 50 %, mRNA and 40 %, protein) in elderly than younger participants, as was IL-8 (4 %). No detectable difference in kinase protein expression was observed for STAT3, JNK or p65 (NF-κB), TNFα or IL-6. Muscle strength was lower in the elderly compared to the young group (1.55 ± 0.17 vs. 2.56 ± 0.13 Nm/kg, p < 0.001). The elderly group also had a significantly lower VO2peak compared to the young group (24.9 ± 1.9 vs. 39.3 ± 1.9, p < 0.001), but muscle strength and VO2peak were not correlated with the examined inflammatory markers. Older adults have increased MCP1 (mRNA and protein abundance) and IL-8 (protein abundance) and also reduced muscle strength and VO2peak. However, the reduction in muscle strength and VO2peak was not related to the increase in muscle inflammatory markers in this cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Inflammation is an essential adaptive response needed for muscular adaptation and repair. The maintenance of muscle mass and strength not only confers significant survival advantage, but also improves the quality of life, with greater mobility and independence. For this, there must be a balance of protein synthesis and degradation as well as pro- and anti-inflammatory molecules. One hallmark feature of aging is the loss of muscle mass, muscle function and muscle strength (sarcopenia) that commences from as early as the fifth decade of life, with loss of muscle accelerating with advancing age and in the presence of additional chronic diseases (Fielding et al. 2011; Hughes et al. 2002). As we age, reduced protein synthesis is apparent and older individuals present with chronic low grade inflammation, characterized by increases in circulating pro-inflammatory mediators; a phenomena known as “inflammaging” (Franceschi et al. 2000, 2007; Toth et al. 2005). Chronically elevated circulating inflammation has been suggested as a contributing feature in the pathogenesis of many age-related diseases, such as dementia, atherosclerosis, type 2 diabetes and Alzheimer’s disease (Bruunsgaard et al. 2003; Bruunsgaard and Pedersen 2003; Ferrucci et al. 2005; Krabbe et al. 2004).
The cellular mechanisms for the loss of regenerative capacity in old age are not well understood. First, age-related loss in the number of myonuclei and satellite cell number per fiber may be one possible limiting factor for muscle regeneration (Fulda and Debatin 2002). However, aging satellite cells and skeletal muscle retain their functionality (Conboy and Rando 2005) and plasticity (Fiatarone et al. 1994; Kosek et al. 2006); therefore there may be systemic factors present to modulate the signaling necessary for the activation of satellite cells for regeneration (Conboy and Rando 2005). Second, there is a complex interplay between tightly regulated signaling pathways which are sensitive to damaging external stimuli, including the mitogen-activated protein kinases (MAPK), nuclear factor kappa-B (NF-κB), c-Jun N-terminal kinases (JNK) and the signal transducer and activator of transcription (STAT) pathway (Peake et al. 2010; Simon et al. 1998). These pathways intersect to transcriptionally regulate the expression of pro-inflammatory mediators, such as tumor necrosis factor (TNFα), interleukin (IL)-8, IL-1β and monocyte chemotactic protein-1 (MCP1). However, to date, it is not clear whether older adults exhibit increases in these pro-inflammatory mediators, particularly in skeletal muscle.
MCP1 and IL-8 are pro-inflammatory chemokines involved in the recruitment of monocytes, macrophages and neutrophils and other inflammatory cells (Baggiolini et al. 1997). Through the modulation of these cells, these chemokines are important for tissue degradation, particularly after trauma or injury and yet are important in facilitating a faster rate of regeneration and recovery. Conversely, MCP1 and IL-8 are also potent activators of NF-κB, thus potentially eliciting and maintaining a chronic cycle of maladaptation, impairing muscle regeneration and repair (Handel et al. 1995; Peake et al. 2010). Monocyte and macrophage activation stimulates the release of the majority of circulating TNFα, following damage or inflammation (Figarella-Branger et al. 2003). As a mediator of muscle wasting, TNFα inhibits myoblast differentiation (Langen et al. 2002), resulting in a reduced regenerative capacity following injury. As such, it appears that circulating MCP1, IL-8 and TNFα may contribute to muscle wasting associated with injury (and potentially inactivity); however, it is not clear whether those inflammatory markers are increased in older adults, particularly in skeletal muscle.
Despite the importance of redox-sensitive pathways as regulators of pro-inflammatory cytokine and chemokine production, very few studies have examined these pathways in the skeletal muscle of older individuals (for review see (Peake et al. 2010). To understand the molecular and signaling events present within skeletal muscle prior to the onset of accelerated muscle wasting in the very old, it is important to address whether these intra-muscular regulators are altered during the course of aging, similar to what has already been identified in circulation (plasma/serum) (Bruunsgaard and Pedersen 2003). Furthermore, it is not clear whether the reduction in muscle strength seen in elderly individuals is related to increased muscle inflammation, which was demonstrated in elderly people with severe musculoskeletal disease, such as osteoarthritis (Levinger et al. 2011). Therefore, the main aim of this study was to compare inflammatory gene and protein expression in the vastus lateralis of older adults versus young individuals. A secondary aim was to examine whether the reduction in muscle strength and aerobic power in older adults is related to muscle inflammatory markers. We hypothesized that older participants would have higher levels of inflammatory molecules compared to their younger counterparts, and this would be related to their reduction in muscle strength and peak aerobic capacity.
Methods
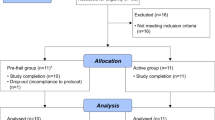
Participants
Seventeen elderly and 16 young people from the general population were recruited for a skeletal muscle biopsy under resting and fasting conditions. As aging is strongly associated with many chronic diseases, we included individuals who suffer from asymptomatic cardiovascular (such as hypertension) or metabolic (obesity and type 2 diabetes) conditions. The two groups reported a similar weekly duration of physical activity, although the young were typically engaged in much higher intensity of exercise (e.g. running rather than walking). Some elderly individuals were on prescribed medications (Table 1). None of the participants were on anti-inflammatory medications. All participants were informed of the nature and risks of the study before their written consent was obtained. The study was approved by the Victoria University Human Research Ethics Committee.
Muscle strength
Muscle strength was measured in a smaller cohort of the elderly (n = 7) and the young (n = 9) participants in the leg from which the muscle biopsy was taken. Strength was measured using a portable purposely built non-extendable strain gauge (load cell) as described previously (Levinger et al. 2011). In brief, the strain gauge was attached to the participant’s leg using a webbing strap with a Velcro fastener. The participant sat in a tall chair with a strap around the lower leg approximately 10 cm above the ankle joint and the hip and knee joint angles positioned at 90°. The distance from the knee joint to the strap around the ankle was measured with a tape measure and was used for the calculation of torque [force (N) × distance (m)]. The participant extracted maximal force against the strap assembly for 3 s. Three trials were recorded and the highest score was used for the analysis. Data were normalized for body mass (Nm/kg).
Aerobic fitness
Aerobic power (VO2peak) was assessed during a symptom-limited graded exercise test on Cybex MET 100 cycle (Cybex Metabolic Systems, Ronkonkoma, NY, USA) as we described previously (Levinger et al. 2007).
Muscle biopsy
The vastus lateralis of either leg was sampled by percutaneous needle biopsy technique as described previously (Trenerry et al. 2007).
RNA extraction and RT-PCR
Samples (10 mg) from each participant were subjected to RNA analysis. First-strand cDNA was generated from 1.0 μg total RNA (Applied Biosystems, Foster City, CA) and RT-PCR was performed in duplicate using Power SYBR Green (Applied Biosystems, Foster City, CA), forward and reverse primers and cDNA template (1.25 ng/μl) (Trenerry et al. 2007). The efficacy of TATA box-binding protein (TBP) as an endogenous control was examined using the equation 2−∆Ct. Primer sequences were designed using Primer Express (Applied Biosystems, Foster City, CA) and validated by BLAST sequence homology (http://blast.ncbi.nlm.nih.gov/Blast.cgi) and melt-curve analysis, as previously described (Trenerry et al. 2007) (see Table 2 for primer details).
Protein extraction and western blot analysis
Tissue samples from each individual were extracted using cell lysis buffer (Bio-Rad Laboratories, Hercules, CA). Approximately 10 mg of sample was homogenized using a FastPrep tissue disruptor (Thermo-Fisher Scientific) (20 s, setting 5.5) using 15 μl lysis buffer per mg tissue. The homogenate was rotated at 4 °C for 1 h, centrifuged at 13,000 rpm at 4 °C for 10 min and the supernatant collected. Protein concentration was determined using the BCA protein assay kit (Thermo-Fisher Scientific) as per manufacturer’s instructions. Total protein (50 μg) was separated by 10 % SDS-PAGE, transferred onto a nitrocellulose membrane and blocked in either 5 % (w/v) bovine serum albumin, 5 % (w/v) cold fish gelatin or 5 % skim milk powder (w/v) in PBS with 0.1 % Tween 20 (PBST). Primary antibodies, diluted in blocking buffer, were applied and incubated overnight at 4 °C; STAT3, p65 (NF-κB), JNK (Cell Signaling Technology Inc., Danvers, MA) and actin (Sigma-Aldrich, Sydney, Australia). Secondary anti-rabbit HRP-conjugated antibodies were used and visualized by enhanced chemiluminescence (Perkin-Elmer, Boston, MA) with densitometry (Kodak Imaging software, Kodak ID 3.5, Perkin-Elmer, Boston, MA).
Multiplex suspension array system
A Bio-Plex suspension array for IL-6, IL-8, MCP1 and TNFα was conducted in triplicate following the manufacturer’s instructions (Bio-Rad Laboratories, Hercules, CA) and as previously described (Trenerry et al. 2010). Protein samples were prepared as described above, diluted to 1,000 μg/ml, using reagents from the Cytokine reagent kit (Bio-Rad Laboratories). Protein abundances were calculated based on standard curve data with a weighted five-parameter logistic fit analysis using Bio-Plex Manager Software v 5.0 (Bio-Rad Laboratories, Hercules, CA). Standards were between 20 and 10,364 pg/ml for each protein of interest.
Statistical analysis
Unpaired t tests were used to compare BMI, strength, VO2peak, mRNA expression and protein abundance data between groups (elderly and young). Spearman Rho correlation was conducted to assess the correlation between inflammatory markers, age, muscle strength and VO2peak. All data are reported as mean ± standard error of the mean (SEM) and statistical analyses were conducted at the 95 % level of significance.
Results
Aging elevates basal levels of inflammatory molecules in muscle
Skeletal muscle MCP1 and IL-1β mRNA were elevated (20–55 %) in the elderly compared to the younger participants (Fig. 1), although only MCP1 was significant (p < 0.01). Protein abundance of MCP1 was significantly elevated in the elderly participants (40 %, p < 0.01) along with IL-8 (4 %, p < 0.05) (Fig. 2). TNFα mRNA did not reach statistical significance (p > 0.05) (Fig. 1). Both muscle MCP1 mRNA and protein abundance were significantly correlated with age (r = 0.54, p < 0.01; r = 0.42, p < 0.05, respectively). Age was also associated with IL-8 protein abundance (r = 0.37, p < 0.05). There was no difference observed between groups for IL-6 protein abundance (p > 0.05, Fig. 2). In the majority of subjects IL-6 mRNA was below the detection threshold. In the remaining subjects the expression was low and highly variable. Gene expression was not statistically different within groups (i.e. young and older adults) between subjects for which strength measurement and VO2peak were obtained and those from whom those data were not collected.
Elevations of inflammatory molecules are evident with aging. mRNA expression of MCP1, TNFα and IL-1β between young and elderly individuals was examined under resting conditions using RT-PCR. Values are arbitrary units (AU) normalized to the expression of the reference gene TBP. Data reported as mean ± SEM. Significantly different from young participants: *p < 0.05, **p < 0.01
Expression of total protein abundance of inflammatory markers in skeletal muscle. Total protein expression of MCP1, TNFα, IL-6 and IL-8 between young and elderly individuals was examined under resting conditions using a multiplex system. Values are AU. Data reported as mean ± SEM. Significantly different from young participants: *p < 0.05, **p < 0.01
Inflammatory-associated kinases are not altered with age
The total protein abundance of JNK1/2, p65 (NF-κB) and STAT3 were measured to evaluate possible downstream signaling events of the aforementioned inflammatory cytokines. There was no difference in the protein expression of these molecules between young and elderly participants (Fig. 3).
There is no age-associated difference in the expression of inflammatory-associated kinases total protein levels in skeletal muscle. Total protein expression of JNK1/2, p65 (NF-κB) and STAT3 between young and elderly individuals was examined under resting conditions using Western blotting. Values are AU, normalized to the expression of actin. Data reported as mean ± SEM
Muscle strength and aerobic power
Muscle strength was lower in the elderly compared to the young group (1.55 ± 0.17 vs. 2.56 ± 0.13 Nm/kg, p < 0.001). The elderly group had a significantly lower VO2peak compared to the young group (24.9 ± 1.9 vs. 39.3 ± 1.9, p < 0.001). Both muscle strength and VO2peak were negatively correlated with age (r = −0.78, p < 0.001 and r = −0.72, p < 0.01, respectively). Muscle strength and VO2peak did not correlate with any of the examined inflammatory markers. VO2peak, however, tended to be negatively correlated with MCP1 mRNA (r = −0.45, p > 0.05).
Discussion
Skeletal muscle mass, strength and quality are impaired in older individuals compared to that of younger adults (Degens 2007; Janssen et al. 2000) and this may be related to increased inflammation in aging (Peake et al. 2010). The current study examined several inflammatory markers associated with muscle wasting and atrophy within skeletal muscle. We have found that in older adults there was increased muscular MCP1 (mRNA and protein abundance) and IL-8 (protein abundance). However, the reduction in muscle strength in these adults was not associated with the expression of inflammatory markers in muscle.
Under normal conditions, MCP1 is involved in the recruitment of inflammatory cells and is important for muscle repair and regeneration via the regulation of macrophages (Baggiolini et al. 1997; Shireman et al. 2007). Macrophage release is necessary for the stimulation of satellite cell activation for skeletal muscle repair (Tidball 2005). It has been suggested that during aging there is an increase in the susceptibility of satellite cells to cytokines such as MCP1, which may alter regeneration capacity of skeletal muscle that in turn may lead to accumulation of damaged cellular components leading to cellular dysfunction (Shireman et al. 2007). In healthy adults, circulating levels of MCP1 in the blood are elevated in an age-dependent manner (Deo et al. 2004; Gerli et al. 2000; Inadera et al. 1999; Kanda et al. 2006; Mariani et al. 2006; Miles et al. 2008; Seidler et al. 2010). We show here that MCP1 is also increased with age in skeletal muscle. Chronic increase in the levels of circulating MCP1 in the blood has previously been suggested to be associated with developing weight gain and health problems (Inadera et al. 1999; Kanda et al. 2006; Miles et al. 2008; Seidler et al. 2010). However, we saw no such associations in the current study, which is similar to other studies that showed elevated MCP-1 without evidence of atherosclerosis (Deo et al. 2004; Mariani et al. 2006).
Similar to MCP1, IL-8 is also involved in the recruitment of inflammatory cells important for muscle adaptation (Baggiolini et al. 1997). High circulating levels of IL-8 have been observed in healthy elderly (Wieczorowska-Tobis et al. 2006), and it was suggested that the levels of this chemokine may be indicative of healthy aging (Wieczorowska-Tobis et al. 2006), contrary to that described for MCP1. An age-related shift in the immunological network has been proposed to occur in serum/plasma that has not yet been described in skeletal muscle: with an apparent elevation and preferential activation of type 2 cytokines, as well as CC and CXC chemokines, in healthy aging individuals (Antonelli et al. 2006; Deo et al. 2004; Gerli et al. 2000; Inadera et al. 1999; Mariani et al. 2006; Seidler et al. 2010; Wieczorowska-Tobis et al. 2006). Based on the results of the present study, it appears that the same could be said to be occurring for CC (MCP-1) and CXC (IL-8) chemokines within skeletal muscle. To further elucidate an association between circulating and intramuscular cytokine and chemokine levels, future studies should sample both serum and muscle biopsies for comparisons between the two, with the inclusion of investigating expression profiles of their receptors.
Inflammatory molecules activate a myriad of signaling pathways to mediate cellular repair. Within skeletal muscle, there is complex crosstalk between several signal transduction cascades, due to the commonality of the ligands which stimulate the activation of these pathways. With age, there may be a dysregulation of this process (Trenerry et al. 2008); therefore, we sought to investigate differences that may be present in the basal levels of important kinases involved in inflammation and skeletal muscle repair. The expression of two common STAT3 activators, IL-6 and TNFα (protein abundance), did not differ between the age groups in the present study, consistent with the lack of difference with age in basal STAT3 levels. However, this is contrary to previously reported age-related differences in total STAT3 protein expression in both humans and rodents muscle (Haddad and Adams 2006; Thalacker-Mercer et al. 2010), where it was suggested that STAT3 increases in older adults were indicative of greater inflammatory signaling at rest (Thalacker-Mercer et al. 2010). As skeletal muscle biopsies contain a mixture of cell types, age-related differences in cell types could be an important factor contributing to the differences observed in inflammatory status between studies. The contrasting findings may also be related to different levels of engagement in physical activity (i.e. sedentary lifestyle vs. recreational active). Some of the elderly individuals in the current study were involved in recreational physical activity which may have a positive (lower) effect on muscle inflammation. A somewhat support for this hypothesis can be found in the trend for negative correlation found between VO2peak and MCP1 mRNA. It is possible that in older adults who live sedentary lifestyle inflammatory markers will be higher than that reported in the current study.
As expected, the elderly group had a significant reduction in muscle strength compared to the young group. Although muscle strength was negatively correlated with age, an important finding was that muscle strength was not associated with any of the measured inflammatory markers in muscle in this older-adult cohort. This is in contrast to the negative correlation observed between muscle strength and inflammatory markers in the very old (Greiwe et al. 2001) and in clinical populations, such as patients with knee osteoarthritis (Levinger et al. 2011). Taking together previous results and those from the current study, it is possible that a correlation exists between muscle strength and inflammatory markers in people aged 75 or older when muscle wasting is evident, and there is a substantial reduction in the capacity to perform activity of daily living that accompanies chronic clinical conditions. It is possible that in a different cohort of elderly people with a more sedentary lifestyle these inflammatory markers may be further elevated, leading to detection of a correlation between reduced muscle strength and increased inflammatory markers. This hypothesis should be explored in future research. In addition, it is possible that a correlation between muscle strength and inflammatory markers may exist in the presence of musculoskeletal disease, where further muscle impairment may be present as was reported previously (Levinger et al. 2011).
JNK and NF-κB are two prominent signaling molecules associated with inflammation, cellular stress and aging. Both kinases are activated by the pro-inflammatory molecule TNFα (Liu 2003). Very few studies have been conducted in older adults measuring the levels of NF-κB proteins or JNK1/2 in skeletal muscle, at rest. We observed no age-related differences in the protein abundance of p65 (NF-κB) and JNK1/2, consistent with unchanged TNFα protein abundance. However, the results for NF-κB contrast with previous research, which have reported increases in phosphorylated IκκB (an NF-κB regulator) and nuclear p65 expression in the older group, but not p50 (Buford et al. 2010), or elevations of p50 in the older adults but no difference in IκκB (Thalacker-Mercer et al. 2010). Differences in the age of the sample populations (67 years in current study vs. 73 years) and physical activity levels (recreationally active vs. sedentary) of the participants may account for some of these discrepancies (Thalacker-Mercer et al. 2010). It was also proposed that in rodents the abundance of NF-κB isoforms might vary between muscle type (e.g. type I vs. type II) in the hindlimb (Phillips and Leeuwenburgh 2005). Additionally, the studies investigating NF-κB within skeletal muscle obtained from aged animals failed to compare the resting levels of p65 prior to immobilization, precluding firm conclusions regarding the effect of age on basal NF-κB levels (Bar-Shai et al. 2005a, b). Similar to NF-κB, there appears to be a difference in JNK expression between muscle types. Age-related changes in JNK protein levels occur in the extensor digitorum longus (EDL) of rats, but not in the soleus (Mylabathula et al. 2006), while in humans, JNK protein expression in the vastus lateralis was not different in a population of young and older men similar to the current study (Williamson et al. 2003). It is possible that the different protein expression in skeletal muscle may occur due to the physical properties of the fibers; however, this requires further investigation.
A potential limitation of the current study is the relatively small sample size. Thus in one sense, this new data should be seen as hypothesis generating. It is possible that with a larger sample size, other correlations, especially between muscle strength and inflammatory markers, will become significant. Another potential limitation is the clinical profile of some elderly participants. We cannot exclude that some of the differences reported are partly related to differences in clinical profile, obesity level, dietary habits (including the possibility of suppressed caloric intake in the elderly) and pharmaceutical use (including NSAIDS), rather than aging per se; however, in current Western societies where 60 % or more of the adult population may be overweight/obese, these clinical profiles are part of aging.
Conclusions
Older adults have increased skeletal muscle MCP1 (mRNA and protein abundance) and IL-8 (protein abundance) and also reduced muscle strength and VO2peak. However, the reduction in muscle strength and VO2peak was not related to the increase in muscle inflammatory markers in this cohort.
Abbreviations
- BMI:
-
Body mass index
- IL:
-
Interleukin
- JNK:
-
c-Jun N-terminal kinases
- MAPK:
-
Mitogen-activated protein kinases
- MCP1:
-
Monocyte chemotactic protein-1
- NF-κB:
-
Nuclear factor kappa-B
- STAT:
-
Signal transducer and activator of transcription
- TNFα:
-
Tumor necrosis factor
- VO2peak :
-
Peak aerobic power
References
Antonelli A, Rotondi M, Fallahi P, Ferrari SM, Paolicchi A, Romagnani P, Serio M, Ferrannini E (2006) Increase of CXC chemokine CXCL10 and CC chemokine CCL2 serum levels in normal ageing. Cytokine 34(1–2):32–38
Baggiolini M, Dewald B, Moser B (1997) Human chemokines: an update. Ann Rev Imm 15:675–705
Bar-Shai M, Carmeli E, Coleman R, Rozen N, Perek S, Fuchs D, Reznick AZ (2005a) The effect of hindlimb immobilization on acid phosphatase, metalloproteinases and nuclear factor-kappaB in muscles of young and old rats. Mech Ageing Dev 126(2):289–297
Bar-Shai M, Carmeli E, Reznick AZ (2005b) The role of NF-kappaB in protein breakdown in immobilization, aging, and exercise: from basic processes to promotion of health. Ann N Y Acad Sci 1057:431–447
Bruunsgaard H, Pedersen BK (2003) Age-related inflammatory cytokines and disease. Immunol Allergy Clin North Am 23(1):15–39
Bruunsgaard H, Andersen-Ranberg K, Hjelmborg JB, Pedersen BK, Jeune B (2003) Elevated levels of tumor necrosis factor alpha and mortality in centenarians. Am J Med 115(4):278–283
Buford TW, Cooke MB, Manini TM, Leeuwenburgh C, Willoughby DS (2010) Effects of age and sedentary lifestyle on skeletal muscle NF-kappaB signaling in men. J Gerontol Series A Bio Sci Med Sci 65(5):532–537
Conboy IM, Rando TA (2005) Aging, stem cells and tissue regeneration: lessons from muscle. Cell Cycle 4(3):407–410
Degens H (2007) Age-related skeletal muscle dysfunction: causes and mechanisms. J Musculoskelet Neuronal Interact 7(3):246–252
Deo R, Khera A, McGuire DK, Murphy SA, Meo Neto Jde P, Morrow DA, de Lemos JA (2004) Association among plasma levels of monocyte chemoattractant protein-1, traditional cardiovascular risk factors, and subclinical atherosclerosis. J Am Coll Cardiol 44(9):1812–1818
Ferrucci L, Corsi A, Lauretani F, Bandinelli S, Bartali B, Taub DD, Guralnik JM, Longo DL (2005) The origins of age-related proinflammatory state. Blood 105(6):2294–2299
Fiatarone MA, O’Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, Roberts SB, Kehayias JJ, Lipsitz LA, Evans WJ (1994) Exercise training and nutritional supplementation for physical frailty in very elderly people. New Engl J Med 330(25):1769–1775
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, De Meynard C, Donini L, Harris T, Kannt A, Keime Guibert F, Onder G, Papanicolaou D, Rolland Y, Rooks D, Sieber C, Souhami E, Verlaan S, Zamboni M (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12(4):249–256
Figarella-Branger D, Civatte M, Bartoli C, Pellissier JF (2003) Cytokines, chemokines, and cell adhesion molecules in inflammatory myopathies. Muscle Nerve 28(6):659–682
Franceschi C, Bonafe M, Valensin S, Olivieri F, De Luca M, Ottaviani E, De Benedictis G (2000) Inflammaging an evolutionary perspective on immunosenescence. Ann N Y Acad Sci 908:244–254
Franceschi C, Capri M, Monti D, Giunta S, Olivieri F, Sevini F, Panourgia MP, Invidia L, Celani L, Scurti M, Cevenini E, Castellani GC, Salvioli S (2007) Inflammaging and anti-inflammaging: a systemic perspective on aging and longevity emerged from studies in humans. Mech Ageing Dev 128(1):92–105
Fulda S, Debatin KM (2002) IFNgamma sensitizes for apoptosis by upregulating caspase-8 expression through the Stat1 pathway. Oncogene 21(15):2295–2308
Gerli R, Monti D, Bistoni O, Mazzone AM, Peri G, Cossarizza A, Di Gioacchino M, Cesarotti ME, Doni A, Mantovani A, Franceschi C, Paganelli R (2000) Chemokines, sTNF-Rs and sCD30 serum levels in healthy aged people and centenarians. Mech Ageing Dev 121(1–3):37–46
Greiwe JS, Cheng B, Rubin DC, Yarasheski KE, Semenkovich CF (2001) Resistance exercise decreases skeletal muscle tumor necrosis factor alpha in frail elderly humans. FASEB J 15(2):475–482
Haddad F, Adams GR (2006) Aging-sensitive cellular and molecular mechanisms associated with skeletal muscle hypertrophy. J Appl Physiol 100(4):1188–1203
Handel ML, McMorrow LB, Gravallese EM (1995) Nuclear factor-kappa B in rheumatoid synovium. Localization of p50 and p65. Arth Rheum 38(12):1762–1770
Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MA (2002) Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nut 76(2):473–481
Inadera H, Egashira K, Takemoto M, Ouchi Y, Matsushima K (1999) Increase in circulating levels of monocyte chemoattractant protein-1 with aging. J Interf Cytokine Res 19(10):1179–1182
Janssen I, Heymsfield SB, Wang ZM, Ross R (2000) Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol 89(1):81–88
Kanda H, Tateya S, Tamori Y, Kotani K, Hiasa K, Kitazawa R, Kitazawa S, Miyachi H, Maeda S, Egashira K, Kasuga M (2006) MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J Clin Inv 116(6):1494–1505
Kosek DJ, Kim JS, Petrella JK, Cross JM, Bamman MM (2006) Efficacy of 3 days/wk resistance training on myofiber hypertrophy and myogenic mechanisms in young vs. older adults. J Appl Physiol 101(2):531–544
Krabbe KS, Pedersen M, Bruunsgaard H (2004) Inflammatory mediators in the elderly. Exp Gerontol 39(5):687–699
Langen RC, Schols AM, Kelders MC, Van Der Velden JL, Wouters EF, Janssen-Heininger YM (2002) Tumor necrosis factor-alpha inhibits myogenesis through redox-dependent and -independent pathways. Am J Physiol Cell Physiol 283(3):C714–C721
Levinger I, Goodman C, Hare DL, Jerums G, Selig S (2007) The effect of resistance training on functional capacity and quality of life in individuals with high and low numbers of metabolic risk factors. Diabetes Care 30(9):2205–2210
Levinger I, Levinger P, Trenerry MK, Feller JA, Bartlett JR, Bergman N, McKenna MJ, Cameron-Smith D (2011) Increased inflammatory cytokine expression in the vastus lateralis of patients with knee osteoarthritis. Arthr Rheum 63(5):1343–1348
Liu ZG (2003) Adding facets to TNF signaling. The JNK angle. Mol Cell 12(4):795–796
Mariani E, Cattini L, Neri S, Malavolta M, Mocchegiani E, Ravaglia G, Facchini A (2006) Simultaneous evaluation of circulating chemokine and cytokine profiles in elderly subjects by multiplex technology: relationship with zinc status. Biogerontol 7(5–6):449–459
Miles EA, Rees D, Banerjee T, Cazzola R, Lewis S, Wood R, Oates R, Tallant A, Cestaro B, Yaqoob P, Wahle KW, Calder PC (2008) Age-related increases in circulating inflammatory markers in men are independent of BMI, blood pressure and blood lipid concentrations. Atheroscl 196(1):298–305
Mylabathula DB, Rice KM, Wang Z, Uddemarri S, Kinnard RS, Blough ER (2006) Age-associated changes in MAPK activation in fast- and slow-twitch skeletal muscle of the F344/NNiaHSD X Brown Norway/BiNia rat model. Exp Gerontol 41(2):205–214
Peake J, Della Gatta P, Cameron-Smith D (2010) Aging and its effects on inflammation in skeletal muscle at rest and following exercise-induced muscle injury. Am J Physiol Reg Int Comp Physiol 298(6):R1485–R1495
Phillips T, Leeuwenburgh C (2005) Muscle fiber specific apoptosis and TNF-alpha signaling in sarcopenia are attenuated by life-long calorie restriction. FASEB J 19(6):668–670
Seidler S, Zimmermann HW, Bartneck M, Trautwein C, Tacke F (2010) Age-dependent alterations of monocyte subsets and monocyte-related chemokine pathways in healthy adults. BMC Immunol 11:30
Shireman PK, Contreras-Shannon V, Ochoa O, Karia BP, Michalek JE, McManus LM (2007) MCP-1 deficiency causes altered inflammation with impaired skeletal muscle regeneration. J Leukoc Biol 81(3):775–785
Simon AR, Rai U, Fanburg BL, Cochran BH (1998) Activation of the JAK-STAT pathway by reactive oxygen species. Am J Physiol 275(6 Pt 1):C1640–C1652
Thalacker-Mercer AE, Dell’Italia LJ, Cui X, Cross JM, Bamman MM (2010) Differential genomic responses in old vs. young humans despite similar levels of modest muscle damage after resistance loading. Physiol Genomics 40(3):141–149
Tidball JG (2005) Inflammatory processes in muscle injury and repair. Am J Physiol Reg Int Comp Physiol 288(2):R345–R353
Toth MJ, Matthews DE, Tracy RP, Previs MJ (2005) Age-related differences in skeletal muscle protein synthesis: relation to markers of immune activation. Am J Physiol Endocrinol Metabol 288(5):E883–E891
Trenerry MK, Carey KA, Ward AC, Cameron-Smith D (2007) STAT3 signaling is activated in human skeletal muscle following acute resistance exercise. J Appl Physiol 102(4):1483–1489
Trenerry MK, Carey KA, Ward AC, Farnfield MM, Cameron-Smith D (2008) Exercise-induced activation of STAT3 signaling is increased with age. Rejuvenation Res 11(4):717–724
Trenerry MK, Della Gatta PA, Larsen AE, Garnham AP, Cameron-Smith D (2010) Impact of resistance exercise training on interleukin-6 and JAK/STAT in young men. Muscle Nerve 43(3):385–392
Wieczorowska-Tobis K, Niemir ZI, Podkowka R, Korybalska K, Mossakowska M, Breborowicz A (2006) Can an increased level of circulating IL-8 be a predictor of human longevity? Med Sci Monit 12(3):CR118–CR121
Williamson D, Gallagher P, Harber M, Hollon C, Trappe S (2003) Mitogen-activated protein kinase (MAPK) pathway activation: effects of age and acute exercise on human skeletal muscle. J Physiol 547(Pt 3):977–987
Acknowledgments
This study was partly funded by the L.E.W Carty Charitable Fund. The authors wish to thank Dr Andrew Garnham (Deakin University) and Dr Mitchell Anderson for performing the muscle biopsies, Dr Paul Della Gatta and Dr Jessica Mathers (Deakin University) for helping with participant recruitment, and all participants for volunteering for this study. Dr Itamar Levinger is a Heart Foundation Postdoctoral Research Fellow (PR 11M 6086).
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Fabio Fischetti.
Rights and permissions
About this article
Cite this article
Caldow, M.K., Cameron-Smith, D., Levinger, P. et al. Inflammatory markers in skeletal muscle of older adults. Eur J Appl Physiol 113, 509–517 (2013). https://doi.org/10.1007/s00421-012-2458-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-012-2458-x