Abstract
Swimming is a popular activity for Australian women with proven cardiovascular benefits yet lacks the features thought necessary to stimulate positive adaptive changes in bone. Given that peak bone mass is attained close to the end of the second decade, we asked whether swimming was negatively associated with bone mineral density in premenopausal women beyond this age. Bone mass and retrospective physical activity data were gathered from 43 female swimmers and 44 controls (mean ages 40.4 and 43.8 years, respectively). Swimmers were recruited from the Australian Union of Senior Swimmers International while controls were healthy community dwellers with similar lean mass, fat mass, height, weight and body mass index. None of the participants had a history of medical complaints nor use of medications known to affect bone. Dual energy X-ray absorptiometry was used to determine areal bone mineral density at total body, lumbar spine, proximal femur, distal radius and tibia while self-administered questionnaires were used to approximate historical and recent physical activity and calcium intake. Swimmers had averaged over 2 hours of swimming per week for the past 5 years and 1.45 h/week over lifetime with no systematic swimming exposure for controls. Lifetime exposure to weight bearing and impact exercise were similar. There were no intergroup differences for bone mass at any site though controls had higher incidence of low bone mass/osteoporosis. No differences in bone mass were detected between swimmers in the upper and lower quartiles for swim participation for any period. Long-term swim participation did not compromise areal bone mineral density.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is said to have a predominately hereditary basis (up to 90% at some sites) with modifiable lifestyle factors like exercise and diet accounting for the remaining variance (Lei et al. 2006). Women are particularly vulnerable given their greater life expectancy, smaller skeletons and loss of the bone preserving action of estrogen which accompanies menopause. Although there are a number of pharmacological (hormone replacement therapy, bisphosphonates, SERMs, cyclic PTH, salmon calcitonin) and dietary (calcium, Vit D) interventions, exercise is considered important for the maintenance and improvement of bone mass and for fall prevention.
Given the primacy of its mechanical functions, it is logical that mechanical loading be the major driver for maintenance and adaptation of bone (Robling et al. 2006). An important result of the work in this area has been the demonstration that it is the combination of strain rate, strain frequency and strain magnitude that is “sensed” by osteocytes and this is central to understanding which modes of physical exercise may promote bone formation or maintenance. In this vein, stress (force per unit area) applied to bones through impact loading or muscle contraction is translated primarily into tensile, compressive and shear strains as bone deforms under the imposed loads (Robling et al. 2006). The resulting pressure gradients force bone fluid through the lacunar/canalicular network deforming the osteocytic membrane with resultant “downstream” responses as described above (Turner and Robling 2004; LaMothe et al. 2005). Hence stress-evoked strains and the resulting shear forces applied to osteocytes appear to be the means by which physical activities evoke positive adaptations in bone structure. The forms of exercise best suited to generating appropriate stresses are considered to feature dynamic forces (not static loading) with rapid rise times and unusual distribution i.e. moderate to high impact loading and/or strong muscle contractions (Turner and Robling 2003; Kohrt et al. 2009; Nikander et al. 2009), though the positive effects of vibration featuring high frequencies but very small strains complicates the picture. The latter have been suggested to perhaps mimic the effects of the continual postural adjustments applied by muscles to the skeleton (Bergmann et al. 2011). In addition, it would seem that high volumes (repetitions) are not necessary to promote a positive response with the mechanotransducing cells (osteocytes) becoming refractory after a relatively small number of stimuli then requiring a recovery period (Robling et al. 2002). Conversely, reduced loading associated with bed rest, spinal cord injury or exposure to microgravity conditions, lead to increased remodeling and bone loss (Pavy-Le Traon et al. 2007). That high muscle forces may not be able to compensate for a lack of impact loading is suggested through studies revealing that competitive cyclists generally have lower bone mass than controls (Nichols et al. 2003; Rector et al. 2008; Smathers et al. 2009). Importantly, the ability to mount an adaptive response to even “appropriate” exercise declines with age (Martyn-St James and Carroll 2009; Nikander et al. 2010) with adults at or beyond the age at which bone mass peaks [peak bone mass (PBM)] most likely to experience bone “sparing” not gains, through exercise (Engelke et al. 2006; Guadalupe-Grau et al. 2009). Given these factors, coupled with the susceptibility of women to bone loss after menopause, it is important that skeletal mass be maximized before this event. In this context, swimming is a popular activity among adult women in Australia, ranking third for participation among all physical activities surveyed by the Australian Bureau of Statistics in 2009 (Australian Bureau of Statistics 2011). However, prior research appears equivocal on the question of whether swimming has positive or negative effects on bone with support for bone maintenance (Emslander et al. 1998; Dalkiranis et al. 2006), bone loss (Risser et al. 1990; Taaffe et al. 1995; Magkos et al. 2007; Ferry et al. 2011) and improved mass or geometric properties (Harumia et al. 2000; Liu et al. 2003; Falk et al. 2004). In light of what has been proposed about the mechanisms of bone adaptation to physical activity, it was hypothesized that a long history of participation in organized swim training, a weight-supported, low-impact activity, with relatively modest demands on muscular strength, would be negatively associated with bone mineral density (BMD) in adult women at or beyond the age of PBM leaving them more susceptible to osteoporosis. This proposition was tested by comparing adult female swimmers and controls on measures of bone mass, calcium intake, historic and recent physical activity participation. The collection of historical physical activity data represents a unique feature of the current investigation given that previous studies investigating the bone mass/swimming association have generally not accounted for long-term physical activity patterns. Furthermore, the subjects were not elite athletes and therefore the findings relate better to the general population of adult women seeking an “exercise prescription” for skeletal health.
Methods
Subjects
Subjects were 87 premenopausal adults, 43 swimmers (mean 40.5 years) recruited from the Australian Union of Senior Swimmers International (AUSSI), and 44 healthy community dwelling controls (43.6 years). Recruitment was conducted through the AUSSI members’ database in the case of the former and through advertisements in a community newspaper, local leisure centres and word-of-mouth for the latter. All were premenopausal based upon reports of more than nine normal cycles over the previous year and the absence of current signs of menopause. There was no history of medication use nor condition known to affect bone mass. All participants provided informed consent prior to participation and all procedures were approved by the RMIT University Human Ethics Committee.
Assessment of physical activity
Since the focus of the work was on the effects of swimming on bone, data on all forms of exercise exposure were gathered to isolate any that might be attributable to swimming. Lifetime, recent and current physical activity, in addition to swim participation, were approximated using self-administered questionnaires. Activity over the lifespan was organized by decade (Kriska et al. 1988; Kriska and Caspersen 1997) starting at the second decade (10–19 years) and rated in metabolic equivalents (METS) as: “Moderate” (3–4.9 METS); “Hard” (5–6.9 METS) and “Very Hard” (>7 METS) (Ainsworth et al. 1993, 2000) and subsequently collapsed under the headings: “Moderate Plus” (sum of all categories) and “Hard Plus” (sum of “Hard” and “Very Hard” hours). Given the proposed importance of weight bearing and impact activity, data were also categorized as “Weight Bearing”; “Medium Impact” (running without jumping e.g. tennis), “High Impact” (featuring jumping e.g. gymnastics, basketball), “Medium Plus Impact” (sum of Medium and High categories) with “Upper Body” and “Lower Body” categories included to indicate how exercise loads were distributed. Recent physical activity data (last 5- and 2-year periods) were extracted from the lifetime records and tabulated under the same headings.
Swimming
The nature of swim training over the past 5 years was determined by consulting training diaries and interviewing swimmers and coaches while swimming history for all participants was captured through a questionnaire eliciting age of learning to swim, weeks per year, days per week and hours per day swum over the lifespan (starting 0–9 years). From the records, average weekly hours swum over the lifespan (by decade), past 5 years, past 3 years, past 2 years and last year were calculated to characterize lifelong and recent swimming volumes and to ensure that swimmers and controls were clearly divergent for swimming participation.
Calcium
Calcium intake was determined for the previous 12 months through administration of a Calcium Frequency Questionnaire and recorded in both absolute terms (mg), and percentage of recommended daily intake (RDI) (Sanders et al. 2009).
Bone measurements and body composition
Areal bone mineral density (aBMD) and/or bone mineral content (BMC) were determined by dual energy X-ray absorptiometry (DXA, Lunar DPX-IQ, Madison, WI, USA) for the total body, lumbar spine (L2–L4), femur subregions, ultra distal radius and tibia. Body composition (fat and lean mass) was determined from total body scans. Height and weight were recorded and used in the calculation of body mass index (BMI). Body mass for each individual was compared with the sum of total bone, lean and fat mass determined by DXA as a check on the validity of the X-ray measurements.
Statistical analysis
All analyses were carried out using PASW version 18 for Windows. A series of multivariate (MANOVA) and/or univariate analyses were used to compare the swimmers and controls for all variables with age entered as a covariate. Gender and weight-adjusted Z and T scores (Lunar database) were tabulated to identify subjects with low bone mass or osteoporosis. In addition, swimmers were divided into quartiles for swimming involvement (mean h/week) over lifetime and last 5 years and the upper and lower quartiles compared for all bone mass variables also by MANOVA or univariate analysis (radius only). To assess the contribution made by swimming hours to any significant differences in activity patterns identified between groups, MANOVAs were repeated with swimming hours over the various periods entered as covariates. Finally, Chi-square analysis was used to compare the incidences of low bone mass between the groups. All results are expressed as means and standard deviations unless otherwise stated and statistical significance was set at p < 0.05 for all comparisons.
Results
Physical characteristics and calcium intake
Table 1 presents basic physical characteristics of the subjects along with calcium intake and the comparison between DXA and scale-derived body mass. The groups were well matched and there was good agreement for body mass determined by DXA and electronic scales with DXA returning slightly lower values. Calcium intake was low on average in both groups, with swimmers achieving 83% and controls 66% of the RDI with considerable variability revealed by the large standard deviations. The only significant difference detected was for age, (controls older, p < 0.05).
Lifespan and recent physical activity
Swimming
AUSSI swimmers typically performed interval training of varying pace and stroke totaling between 1.5 and 3.5 k per session thrice weekly (past 5 years). They had swimming exposure of over 2 h/week for the past 5 years and 1.45 h per week over lifetime while lifetime mean swimming for the control subjects averaged <5 min/week.
Recent physical activity
Table 2 shows that over the previous 5- and 2-year periods, swimmers were significantly more active than controls in what might be termed the MET-intensive categories (0.06 > p < 0.001) while there were no differences between the groups for Weight Bearing, Impact or Lower Body activities (all p > 0.05).
Lifetime physical activity (Table 3) mirrored recent physical activity patterns with no differences between the groups for any weight bearing or impact category for any decade (all p > 0.05). For the earliest decade recorded, (10–19 years) swimmers were again more active than controls reporting significantly more time in Moderate Plus, Hard Plus and Very Hard activities as well as performing more Upper Body work. By the third decade (20–29 years), the number of significant differences had reduced to a single variable with swimmers only exceeding controls for Very Hard activity. This trend continued for the final two decades with swimmers significantly more active than controls only for Hard Plus and Very Hard activity (30–39 years) and only Very Hard activity for the final decade. It should be noted that there were fewer respondents for these periods, particularly the last decade. That swimmers were consistently more active in Very Hard activities can logically be attributed to swimming given its MET rating ranging between seven and 11 (Ainsworth et al. 2000). To confirm the speculation that swimming hours could account for the differences between the groups for recent and historical physical activity, analyses were repeated with the relevant swimming hours entered as covariates. Tables 2 and 3 (p value adj) reveal that the only comparisons that remained significant were for Hard Plus and Very Hard activity in the 10–19 decade.
Areal bone mineral density
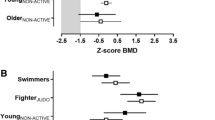
Table 4 provides a summary of the age-adjusted results derived from DXA measurements for all skeletal sites. Swimmers exceeded controls at all sites except for the proximal tibia but only at the ultra distal radius did the difference approach significance (p = 0.062, controls lower). Both groups recorded negative T and Z scores for this site putting them below average even for their own age group. On the other hand, both groups were on average, more than one standard deviation above the mean young adult value (T score) for total body and were also in “positive territory” at the lumbar spine, femoral neck, trochanter and total proximal femur. At Wards, swimmers were slightly above average and controls slightly below.
All individual results were examined to reveal instances of osteoporosis and or low bone mass based upon T scores <−2.5 and <−1.0 for any site, respectively (Table 5). It should be noted that the figures include some subjects with low bone mass at more than one site.
For the control group, osteoporosis was detected in two subjects, one at two sites (Wards and the radius) the other at Wards alone; both individuals demonstrated low bone mass at multiple sites. Of the remaining controls, 20 (46%) had low bone mass, six at two or more sites and the others at a single site, predominantly the radius. Osteoporosis was detected at the radius in two swimmers and in one of them it was accompanied by low bone mass at another site (Wards). Of the remaining swimmers, 15 (36%) had low bone mass, eight at two or more sites and the remainder at a single site, the radius. In absolute terms, there were fewer swimmers with osteoporosis/low bone mass at all sites and the radius was the most common site for low bone mass in both groups. Chi-squared analysis failed to detect any differences between the groups at any individual site (p > 0.05 for all comparisons) but when the total number of cases of low bone mass for swimmers and controls were compared (34 and 56, respectively), swimmers had significantly fewer (p = 0.020).
Comparisons between upper and lower quartiles of swimming participation
The mean hours of participation for each swimming quartile for each period are presented in Table 6 while Table 7 summarizes the results of the “within group” comparisons between upper and lower swimming quartiles for the five periods for all bone mass measures. Addressing Table 6 first, there was considerable variation in mean swimming hours between quartiles for each period with the lowest values for all quartiles, as would be expected, found for the lifetime period. For the more recent swimming periods (previous 1–5 years), the means for each quartile were relatively consistent, all exceeding 40 min, 1, 2 and 4 h, respectively. However, the differences between the means for the upper and lower quartiles for each period, ranged between 2.66 and 4.26 h/week, clearly demonstrating a large disparity in swimming exposure within the group.
As revealed in Table 7, despite substantial differences in swimming participation between quartiles, no significant differences were detected for bone mass at any site for any period (all p > 0.05). The only comparisons that approached significance were for the femur at Wards for the 5-, 3- and 2-year periods (p < 0.067 for all—lower quartile lower). Indeed, there was a trend for higher bone mass for members of the upper quartile at most sites (39 of 50 measurements).
Discussion
The results failed to support the hypothesis that a long-term history of swimming participation is negatively associated with aBMD in women at or beyond PBM, in fact, an opposite trend was revealed. Swimmers had lower though non-significant incidence of low bone mass at each site but significantly fewer in total. In addition, swimmers with the greatest exposure (upper quartile) had the highest bone mass at most sites. These results bear some similarity to those found by Velez et al. (2008) in an older sample (>65 years) of Masters’ athletes including a small number of swimmers (N = 15). For their female swimmers, osteopenia (low bone mass) ranged between 16% at the spine and 61% at the femoral neck with the distal radius being the most common site for osteoporosis. Thirty percent of their controls were osteopenic at the spine and 55% at the femoral neck, with the spine being the most common site for osteoporosis.
Interestingly, the similarities between swimmers and controls for bone mass, occurred in the face of a considerably greater magnitude of past physical activity on the part of the swimmers, differences which could be accounted for logically on the basis of swimming participation (at least over the prior two decades), which is rated as “Hard” or “Very Hard” depending upon pace and distance (Ainsworth et al. 2000). That activities categorized as Weight Bearing and High Impact were practiced to a similar degree by the two groups, lends support to the proposition that swimming (as practiced by these women) did not promote bone acquisition, consistent with previous investigations where bone mass in swimmers has been generally found to be no greater than controls (Emslander et al. 1998; Dalkiranis et al. 2006). By the same token, lack of differences between the groups for bone mass at any site and the positive T and Z scores for two of the three sites and negative results at another for both groups, also indicate that no detrimental effect on bone mass could be attributed to swimming (as practiced here). The results are reminiscent of those found by Harumia et al. (2000), whose 74 female swimmers (40–60 years; 1–2 h/week swimming for past 7 years) had higher bone mass at baseline than controls and that those with the longest swimming history had the highest values. Furthermore, their 2-year observational study found bone loss in both groups but to a lesser degree in the swimmers prompting their conclusion that swimming might be osteogenic before menopause but thereafter is associated with slowing loss rather than preserving bone mass. These conclusions should be tempered, however, given the lack of information provided on “other” physical activities performed by the participants that might have accounted for any advantages that the swimmers enjoyed.
The prevalence of low bone mass at the ultra distal radius for both groups in the current study was an unexpected finding, one for which the data collected could not account, but might reflect a “preferential” loss of bone at this site which is likely to experience a more marked reduction in loading with age than the weight bearing lower limbs and spine. That both swimmers and controls demonstrated this phenomenon indicates that the strains generated by water resistance and forearm muscle activity (used to maintain the position of the hand during the propulsive phase of swimming) are insufficient to maintain forearm bone mass. In addition, there were no differences between swimmers and controls for lean mass (Table 1), supporting the notion that the muscular loads developed by swimming would be unlikely to produce the skeletal strains necessary to stimulate increases in bone mass. In terms of calcium intake, both groups were below the RDI for this nutrient as reported over the previous year with the control group particularly low. However, given the absence of differences between the groups for bone mass and the fact that both groups had positive Z and T scores at most sites, it would appear that low calcium intake, had no effect on the results.
How might the results be explained? Perhaps the muscular demands of swimming were sufficient to overcome the potential negative effects of the weight-supporting medium, generating bone strains sufficient for bone maintenance with the exception of the forearm. It is also possible and we consider more likely, that the swimmers performed sufficient weight bearing and high impact exercise outside of the pool to maintain bone, a reasonable proposition given the similarities between swimmers and controls for these categories of exercise.
Swimmers and controls were well matched in terms of physical characteristics including lean and fat mass which have been shown to correlate significantly with bone mass in women (r = 0.68 and 0.22, respectively, Kohrt et al. 2009). This finding would suggest that the swimmers were not specifically self-selected for swimming on the basis of lighter frames or better buoyancy and hence makes them better representatives of the general nonathletic population and perhaps allow the results to be more generalizable.
Finally, it is acknowledged that using aBMD, as a surrogate for bone strength ignores the underlying distribution of bone (moments of inertia, cortical thickness, medullary diameter etc.) and that such geometric features may be affected positively by swimming in humans and animals as suggested by others (Liu et al. 2003; Falk et al. 2004; Warner et al. 2006).
Conclusions
Endurance style swimming in premenopausal adult women at or beyond the time when maximum bone mass has been accrued, does not produce any detrimental effects on bone mass when coupled with “normal” weight bearing activities and therefore may be encouraged for its positive effects on cardiovascular fitness and social interaction. However, swimming in mature adult women appears to preserve bone rather than promote gains and would not be suitable as part of an exercise prescription to improve bone mass.
References
Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, Paffenbarger RS Jr (1993) Compendium of physical activities: energy costs of human movement. Med Sci Sports Exerc 25:71–80
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO, Jacobs DR Jr, Leon AS (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32(9 Suppl):S498–S504
Australian Bureau of Statistics (2011) Report 4156.0: Sports and physical recreation: a statistical overview, Australia, 2011. Section 3.4 Participants http://www.abs.gov.au/ausstats/
Bergmann P, Body JJ, Boonen S, Boutsen Y, Boutsen J, Devogelaer JP, Goemaere S, Kaufman J, Reginster JY, Rozenberg S (2011) Loading and skeletal development and maintenance. J Osteoporos. doi:10.4061/2011/786752
Dalkiranis A, Patsanas T, Papadopoulou SK, Gissis I, Denda O, Mylonas A (2006) Bone mineral density in fin swimmers. J Hum Mov Stud 50(1):19–28
Emslander HC, Sinaki M, Muhs JM, Chao EY, Wahner HW, Bryant SC, Riggs BL, Eastell R (1998) Bone mass and muscle strength in female college athletes (runners and swimmers). Mayo Clin Proc 73(12):1151–1160
Engelke K, Kemmler W, Lauber D, Beeskow C, Pintag R, Kalender WA (2006) Exercise maintains bone density at spine and hip EFOPS: a 3-year longitudinal study in early postmenopausal women. Osteoporos Int 17(1):133–142
Falk B, Bronshtein Z, Zigel L, Constantini N, Eliakim A (2004) Higher tibial quantitative ultrasound in young female swimmers. Br J Sports Med 38(4):461–465
Ferry B, Duclos M, Burt L, Therre P, Le Gall F, Jaffré C, Courteix D (2011) Bone geometry and strength adaptations to physical constraints inherent in different sports: comparison between elite female soccer players and swimmers. J Bone Miner Metab 29(3):342–351
Guadalupe-Grau A, Fuentes T, Guerra B, Calbet JA (2009) Exercise and bone mass in adults. Sports Med 39(6):439–468
Harumia Y, Takao S, Satoru Y (2000) The relationship between swimming exercise and bone density. A cohort study among middle-aged women. Dokkyo J Med Sci 27(1):105–111
Kohrt WM, Barry DW, Schwartz RS (2009) Muscle forces or gravity: what predominates mechanical loading on bone? Med Sci Sports Exerc 41(11):2050–2055
Kriska AM, Caspersen CJ (1997) Introduction to a collection of physical activity questionnaires. Med Sci Sports Exerc 29(6):5–9
Kriska AM, Sandler RB, Cauley JA, LaPorte RE, Hom DL, Pambianco G (1988) The assessment of historical physical activity and its relation to adult bone parameters. Am J Epidemiol 127(5):1053–1063
LaMothe JM, Hamilton NH, Zernicke RF (2005) Strain rate influences periosteal adaptation in mature bone. Med Eng Phys 27(4):277–284
Lei SF, Chen Y, Xiong DH, Li LM, Deng HW (2006) Ethnic difference in osteoporosis-related phenotypes and its potential underlying genetic determination. J Musculoskelet Neuronal Interact 6(1):36–46
Liu L, Maruno R, Mashimo T, Sanka K, Higuchi T, Hayashi K, Shirasaki Y, Mukai N, Saitoh S, Tokuyama K (2003) Effects of physical training on cortical bone at midtibia assessed by peripheral QCT. J Appl Physiol 95(1):219–224
Magkos F, Yannakoulia M, Kavouras SA, Sidossis LS (2007) The type and intensity of exercise have independent and additive effects on bone mineral density. Int J Sports Med 28(9):773–779
Martyn-St James M, Carroll S (2009) Strength training combined with plyometric jumps in adults: sex differences in fat-bone axis adaptations. J Appl Physiol 107(2):636
Nichols JF, Palmer JE, Levy SS (2003) Low mineral density in highly trained male master cyclists. Osteoporos Int 14:644–649
Nikander R, Kannus P, Dastidar P, Hannula M, Harrison L, Cervinka T, Narra NG, Aktour R, Arola T, Eskola H, Soimakallio S, Heinonen A, Hyttinen J, Sievänen H (2009) Targeted exercises against hip fragility. Osteoporos Int 20(8):1321–1328
Nikander K, Sievanen H, Heinonen A, Daly R, Uusi-Rasi K, Kannus P (2010) Targeted exercise against osteoporosis: A systematic review and meta-analysis for optimising bone strength throughout life BMC Medicine 8:47. http://www.biomedcentral.com/1741-7015/8/47
Pavy-Le Traon A, Heer M, Narici MV, Rittweger J, Vernikos J (2007) From space to Earth: advances in human physiology from 20 years of bed rest studies (1986–2006). Eur J Appl Physiol 101:143–194
Rector RS, Rogers R, Ruebel M, Hinton PS (2008) Participation in road cycling vs running is associated with lower bone mineral density in men. Metabolism 57(2):226–232
Risser WL, Lee EJ, LeBlanc A, Poindexter HB, Risser JM, Schneider V (1990) Bone density in eumenorrheic female college athletes. Med Sci Sports Exerc 22(5):570–574
Robling AG, Hinant FM, Burr DB, Turner CH (2002) Improved bone structure and strength after long-term mechanical loading is greatest if loading is separated into short bouts. J Bone Miner Res 17(8):1545–1554
Robling AG, Castillo AB, Turner CH (2006) Biomechanical and molecular regulation of bone. Annu Rev Biomed Eng 8:455–498
Sanders KM, Nowson CA, Kotowicz MA, Briffa K, Devine A, Reid IR (2009) Calcium and bone health: position statement for the Australian and New Zealand Bone and Mineral Society, Osteoporosis Australia and the Endocrine Society of Australia. MJA 190(6):316–320
Smathers AM, Bemben MG, Bemben DA (2009) Bone density comparisons in male competitive road cyclists and untrained controls. Med Sci Sports Exerc 41(2):290–296
Taaffe DR, Snow-Harter C, Connolly DA, Robinson TL, Brown MD, Marcus R (1995) Differential effects of swimming versus weight-bearing activity on bone mineral status of eumenorrheic athletes. J Bone Min Res 10(4):586–593
Turner CH, Robling AG (2003) Designing exercise regimens to increase bone strength. Exerc Sport Sci Rev 31(4):45–50
Turner CH, Robling AG (2004) Exercise as an anabolic stimulus for bone. Curr Pharm Des 10(21):2629–2641
Velez NF, Zhang A, Stone B, Perera S, Miller M, Greenspan SL (2008) The effect of moderate impact exercise on skeletal integrity in master athletes. Osteoporos Int 19(10):1457–1464
Warner SE, Shea JE, Miller SC, Shaw JM (2006) Adaptations in cortical and trabecular bone in response to mechanical loading with and without weight bearing. Calcif Tissue Int 79(6):395–403
Conflict of interest
There are no conflicts of interest for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Susan A. Ward.
Rights and permissions
About this article
Cite this article
Greenway, K.G., Walkley, J.W. & Rich, P.A. Does long-term swimming participation have a deleterious effect on the adult female skeleton?. Eur J Appl Physiol 112, 3217–3225 (2012). https://doi.org/10.1007/s00421-011-2305-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-2305-5