Abstract
High-intensity interval training (HIT) has been proposed as a time-efficient alternative to traditional cardiorespiratory exercise training, but is very fatiguing. In this study, we investigated the effects of a reduced-exertion HIT (REHIT) exercise intervention on insulin sensitivity and aerobic capacity. Twenty-nine healthy but sedentary young men and women were randomly assigned to the REHIT intervention (men, n = 7; women, n = 8) or a control group (men, n = 6; women, n = 8). Subjects assigned to the control groups maintained their normal sedentary lifestyle, whilst subjects in the training groups completed three exercise sessions per week for 6 weeks. The 10-min exercise sessions consisted of low-intensity cycling (60 W) and one (first session) or two (all other sessions) brief ‘all-out’ sprints (10 s in week 1, 15 s in weeks 2–3 and 20 s in the final 3 weeks). Aerobic capacity (\( \dot{V}{\text{O}}{}_{ 2}{\text{peak}} \)) and the glucose and insulin response to a 75-g glucose load (OGTT) were determined before and 3 days after the exercise program. Despite relatively low ratings of perceived exertion (RPE 13 ± 1), insulin sensitivity significantly increased by 28% in the male training group following the REHIT intervention (P < 0.05). \( \dot{V}{\text{O}}{}_{ 2}{\text{peak}} \) increased in the male training (+15%) and female training (+12%) groups (P < 0.01). In conclusion we show that a novel, feasible exercise intervention can improve metabolic health and aerobic capacity. REHIT may offer a genuinely time-efficient alternative to HIT and conventional cardiorespiratory exercise training for improving risk factors of T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of type 2 diabetes (T2D) is increasing rapidly in the UK (Gonzalez et al. 2009) and throughout the world (Danaei et al. 2011). T2D is associated with substantial human costs in terms of reduced quality of life and life expectancy, and management of the symptoms, and secondary complications of T2D accounts for a considerable proportion of total public health care expenditure (American Diabetes Association 2008). As such, finding effective and inexpensive strategies to prevent and treat T2D should be a key objective, and is indeed essential if affordable health care systems are to remain a viable proposition.
The primary defect underlying the development of T2D is skeletal muscle insulin resistance (DeFronzo and Tripathy 2009). The metabolic causes of insulin resistance are numerous and complex but there is accumulating evidence that physical inactivity may be the major initiating factor (Thyfault and Krogh-Madsen 2011), whereas regular exercise is associated with improved muscle insulin sensitivity and thus represents an effective strategy to prevent T2D (Hawley and Gibala 2009). In fact, it is now recognised that exercise, rather than just being a useful strategy for improving health, is actually essential for good metabolic and cardiovascular function, of which insulin action is a key component (Thyfault and Krogh-Madsen 2011; Booth et al. 2002). With this in mind, the finding that ~6 out of 10 men and ~7 out of 10 women in the UK are currently not achieving the (low) minimum recommended levels of physical activity is a major concern (Allender et al. 2008). Recommendations for levels of physical activity place heavy emphasis on performing moderate and/or vigorous-intensity cardiorespiratory exercise training (Garber et al. 2011), which is associated with a substantial time commitment. ‘Lack of time’ is often cited as a barrier to being physically active (Korkiakangas et al. 2009; Reichert et al. 2007), suggesting that these guidelines may not be the ideal approach to increase physical activity levels to improve public health.
Several recent studies have suggested that high-intensity interval training (HIT), a training model involving a series of 30-s ‘all-out’ cycling sprints (i.e. Wingate sprints) with 4 min of rest/recovery between each bout, may provide a time-efficient strategy for inducing adaptations that are similar to traditional cardiorespiratory training (Gibala et al. 2006; Burgomaster et al. 2005, 2007, 2008; Rakobowchuk et al. 2008; Trilk et al. 2010). Furthermore, we have recently demonstrated the beneficial effects of HIT on insulin sensitivity (Babraj et al. 2009), a finding that has since been confirmed by others (Little et al. 2011; Richards et al. 2010; Whyte et al. 2010). However, whilst these observations are interesting from a human physiological perspective, their translation into physical activity recommendations for the general population is uncertain for two reasons. First, the relatively high exertion associated with ‘classic’ HIT sessions requires strong motivation and may be perceived as too strenuous for many sedentary individuals (Hawley and Gibala 2009). Second, although a typical HIT session requires only 2–3 min of actual sprint exercise, when considered as a feasible exercise session including a warm-up, recovery intervals and cool-down, the total time commitment is more than 20 min, reducing the time efficiency (Garber et al. 2011). Thus, there is scope for further research to determine whether the current HIT protocol can be modified to reduce the levels of exertion and time-commitment while maintaining the associated health benefits.
We (Babraj et al. 2009) and others (Whyte et al. 2010) have suggested that high levels of glycogen depletion observed during repeated 30-s Wingate sprints may play an important role in mediating improvements in insulin sensitivity following HIT. This hypothesis is based on the evidence that muscle glycogen availability is inversely related to muscle cell membrane GLUT4 content during insulin stimulation (Derave et al. 2000), glycogen synthase activity (Jensen et al. 2006), the expression of GLUT4 mRNA (Steinberg et al. 2006), and hence insulin sensitivity (Derave et al. 2000; Jensen et al. 2006; Kawanaka et al. 2000; Laurent et al. 2000; Litherland et al. 2007; Richter et al. 2001). The upregulation of key metabolic genes initiated by the release of glycogen-bound proteins may, at least in part, explain how glycogen depletion affects insulin-dependent muscle glucose uptake (Steinberg et al. 2006; Graham et al. 2010). Regardless of the potential mechanisms, however, if muscle glycogen regulates insulin sensitivity then exercise protocols aiming to reduce glycogen levels should be effective.
It has consistently been shown that a single 30-s Wingate sprint can reduce muscle glycogen stores in the vastus lateralis by 20–30% (Esbjornsson-Liljedahl et al. 1999; Parolin et al. 1999; Esbjornsson-Liljedahl et al. 2002; Gibala et al. 2009). What is intriguing, however, is that glycogenolysis is only activated during the first 15 s of the sprint and is then strongly attenuated during the final 15 s (Parolin et al. 1999). Moreover, activation of glycogenolysis is inhibited in subsequent repeated sprints (Parolin et al. 1999). This suggests that the traditional HIT protocol (4–6 × 30 s) may be unnecessarily strenuous as similar glycogen depletion may be achieved using 1–2 sprints of shorter duration (15–20 s). In turn, this would make the training sessions more time-efficient, less strenuous and more applicable to the largely sedentary general population. Therefore, in the current study we investigated the effects of a reduced-exertion HIT (REHIT) intervention on insulin sensitivity in previously sedentary subjects. We hypothesised that despite reducing sprint time and number, REHIT would still be effective in improving the glucose tolerance.
Methods
Subjects
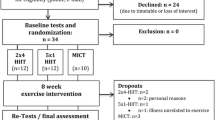
Twenty-nine sedentary but healthy young men (n = 13) and women (n = 16) were recruited to take part in the study and randomly allocated to a training group or a control group. Subjects allocated to the training group completed the full experimental protocol whilst subjects in the control group completed the pre- and post-training assessments without an exercise intervention. Baseline characteristics for each subject group are shown in Table 1. All the participants were classified as sedentary according to the criteria of the International Physical Activity Questionnaire (IPAQ) (Craig et al. 2003) and were only included in the study if they answered ‘no’ to all the questions in the physical activity readiness questionnaire (PAR-Q) (Thomas et al. 1992). Further exclusion criteria included clinically significant hypertension (>140/90 mmHg) and a personal history of metabolic or cardiovascular disease. All the subjects were fully informed of the experimental protocol and any associated risks, both verbally and in writing, before providing written informed consent to participate. In addition, the potentially confounding effect of changes in diet and physical activity patterns was fully explained to all the participants and they were asked to maintain their normal lifestyle patterns throughout the study period. The experimental protocol was approved by the Heriot-Watt University School of Life Sciences Ethics Committee and was conducted in accordance with the Declaration of Helsinki.
Experimental design
All the subjects underwent pre- and post-intervention testing for insulin sensitivity and aerobic capacity. Insulin sensitivity was assessed using an oral glucose tolerance test (OGTT) and aerobic capacity was assessed using a conventional \( \dot{V}{\text{O}}{}_{ 2}{\text{peak}} \) cycling test. The baseline OGTTs were performed 2 weeks before the training commenced and the post-intervention OGTTs were conducted 3 days after the final training bout at the same time of day as the pre-intervention OGTT. This meant that there were exactly 8 weeks between the pre- and post-training OGTTs which ensured that female subjects were in the same stage of their menstrual cycle. The \( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) tests took place 1–2 days after the OGTTs.
Oral glucose tolerance test
Prior to OGTTs subjects performed no moderate or vigorous intensity physical activities for 3 days, and refrained from drinking alcohol for 1 day. Furthermore, subjects completed a 3-day food diary before each OGTT which was analysed for total energy and macronutrient content using commercially available dietary analysis software (Dietplan6, Forestfield Software, UK). There were no significant differences in total energy, carbohydrate, fat or protein content over the 3 days before the pre- and post-intervention OGTTs in any of the subject groups.
On the day of the OGTT subjects reported to the laboratory between 7:30 and 9:30 am following an overnight fast from 10 pm the previous evening. A fasting blood sample was obtained from a forearm antecubital vein by venepuncture using the vacutainer system. 75 g of anhydrous glucose (Fisher Scientific, Loughborough, UK) dissolved in 100 ml of water was then orally administered and further blood samples were taken at 60 and 120 min after glucose ingestion. The collected blood samples were stored on ice and then centrifuged for 10 min at 1,600g to separate the plasma which was stored at −20°C prior to the determination of plasma glucose and insulin concentrations. Plasma glucose concentration was determined by the glucose oxidase reaction using an automated analyser (YSI Stat 2300, Yellow Spring Instruments, Yellow Spring, OH). Plasma insulin concentration was measured using a commercially available ELISA according to the manufacturer’s instructions (Invitrogen, UK). All the glucose and insulin assays were carried out in duplicate. Area under the curve (AUC) for plasma glucose and insulin was calculated using the trapezoid model. Peripheral insulin sensitivity was determined using the Cederholm index (Cederholm and Wibell 1990) which is calculated using the formula:
where BW is body weight, G 0 and G 120 are plasma glucose concentration at 0 and 120 min (mmol l−1), and I mean and G mean are the mean insulin (mU l−1) and glucose (mmol l−1) concentrations during the OGTT. The Cederholm Index has previously been shown to correlate well with the gold standard insulin clamp method (Piche et al. 2007).
\( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) test
Peak oxygen uptake capacity (\( \dot{V}{\text{O}}{}_{2}{\text{peak}} \)) was determined using a graded cycling test to volitional exhaustion on a mechanically braked cycle ergometer (Ergomedic 874e, Monark, Vansbro, Sweden). Subjects cycled at 60 W for 1 min after which the resistance was increased by 30 W min−1 until the pedal cadence could no longer be maintained at 60 rpm. Participants respired through a rubber mouthpiece which was connected to an online gas analysis system (Sensor-Medics, Bilthoven, the Netherlands). Respiratory volume, flow and levels of expired O2 and CO2 were measured and \( \dot{V}{\text{O}}{}_{2} \) was averaged over 10 s periods. \( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) was taken as the highest 10 s value achieved during the test. In all the tests two or more of the following criteria were met: a plateau in \( \dot{V}{\text{O}}{}_{2} \) despite increasing intensity, RER >1.15, heart rate within 10 beats of age-predicted maximum, and/or volitional exhaustion.
Training protocol
Subjects allocated to the training group completed three exercise sessions per week for 6 weeks, completing 18 sessions overall. All the exercise sessions lasted 10 min in total, including a warm up and cool down, which meant a total training time of 30 min per week. Each training session consisted of low intensity cycling (60 W) and one (1st session) or two (all other sessions) all-out cycling sprints. Just before each sprint, resistance was removed, subjects increased the pedal cadence to their maximal speed, a braking force equivalent to 7.5% of body weight was then applied to the ergometer, and the participants sprinted against the braking force for a designated time period. The duration of the sprints increased from 10 s in week 1, to 15 s in weeks 2 and 3, and 20 s in the final 3 weeks. A full schematic of the training protocol is shown in Fig. 1. Training sessions were fully supervised and verbal encouragement was given during each sprint. A rating of perceived exertion (RPE) was collected using the 15-point Borg scale (Borg 1970) at the end of the first session, and subsequently at the end of each training week, immediately following the completion of the 10-min training session.
Statistical analysis
All the data are presented as mean ± SEM. Data were analysed using the commercially available SPSS statistics package (PASW Statistics, version 17.0). Three-way mixed-model ANOVAs (gender [male, female] × group [REHIT, control] × time [pre, post]) were performed to test the effects of the REHIT intervention. For variables with significant gender × time interactions, males and females were analysed separately using 2-way mixed model ANOVAs (group × time). Comparisons in RPE data between men and women were made using an independent sample t test. Significance was accepted at P < 0.05.
Results
No significant differences existed between the REHIT and control groups at baseline (Tables 1, 2). There were no changes in weight or BMI following the REHIT training program in any of the groups (Table 2). Ten out of 15 training group participants completed all the 18 training sessions (100% adherence), with a mean adherence to the REHIT training program of 97% for all subjects combined.
\( \dot{V}{\text{O}}{}_{2}{\text{peak}} \)
For \( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) there were significant main effects of gender (P < 0.001) and time (P < 0.01), and a significant interaction effect for group × time (P < 0.01): following REHIT \( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) was increased by 15% in men and by 12% in women with no significant gender difference in this effect (Table 2). These results were the same when \( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) was expressed in l min−1 or ml kg−1min−1.
Glucose and insulin responses to the OGTT
Effects of the REHIT intervention on glucose and insulin responses to an oral glucose load are shown in Fig. 2, with glucose and insulin AUCs shown in Table 2. As we observed a significant interaction effect for gender × time for glucose AUC (P < 0.05), results for male and female subjects were analysed separately using a two-way mixed-model ANOVA (group × time). No significant effects were observed for men. A significant main effect for time for women (P < 0.05) indicated that post-intervention values for glucose AUC were increased, but there was no significant difference between the female REHIT and control groups. No significant changes in insulin AUC were observed (Table 2).
A significant interaction effect for gender × time was also observed for insulin sensitivity (P < 0.01), so male and female subjects were analysed separately. Following REHIT, insulin sensitivity significantly improved by 28% in male subjects (P < 0.05), but not in female subjects (Fig. 3).
Rate of perceived exertion
RPE data over the course of the REHIT training program are shown in Fig. 4. On the whole, despite the incorporation of brief but intense sprints, the training sessions were well tolerated by all of the participants. Mean RPE values peaked at the end of session 12 (week 4; 2 × 20 s), corresponding to ‘somewhat hard’ and between ‘somewhat hard’ and ‘hard’ in men and women, respectively (Fig. 4a). None of the participants gave an RPE score higher than 15. When mean RPE values over the whole training program were calculated, female participants found the training program significantly harder than male participants (Fig. 4b).
Discussion
In the present study, we show that a 6-week novel exercise intervention consisting of very brief, manageable sessions is associated with improved insulin sensitivity in sedentary young men, and improved aerobic capacity in men and women. The beneficial effects occurred independently of changes in body mass and may represent a chronic training adaptation since post-training measurements were taken 3 days after the final exercise bout. Importantly, the improvements were observed despite the low time commitment (totalling 30 min per week) and low required effort; RPE peaked at an average of 14 (‘somewhat hard’) in week 4 which is comparable with RPE scores reported with prolonged cycling at 50–75% \( \dot{V}{\text{O}}_{ 2} {\text{peak}} \) (Borg 1982). This study extends the previous literature showing the beneficial effects of HIT (Burgomaster et al. 2007; Babraj et al. 2009; Richards et al. 2010; Whyte et al. 2010; Rakobowchuk et al. 2008; Trilk et al. 2010) by showing that the sprint number and duration can be substantially reduced whilst still maintaining positive effects.
Based on the current knowledge, when considering the health effects of exercise solely from a physiological perspective it is fair to state that more (within reason) is better. In other words, to optimise the metabolic, cardiovascular and psychological benefits that exercise can offer, people should be encouraged to perform a large volume (at least 30 min per day) of both moderate and vigorous intensity cardiorespiratory exercise on most days of the week, as well as sessions focused on strength and flexibility 2–3 times per week (Garber et al. 2011). However, whilst these guidelines may be effective in people who adhere to them, they remain largely ineffective at a societal level (Allender et al. 2008), partly because they fail to sufficiently consider the key barriers which prevent people from performing regular exercise, such as ‘lack of time’. For exercise prescriptions to have a beneficial effect for society, there must be a balance between providing adequate health benefits and helping to generate motivation to perform exercise by overcoming key barriers. One possible alternative strategy could be to define the minimum volume of exercise required to improve health indices with the aim of increasing exercise adherence. To date, the training program utilised in the current study represents the smallest volume of exercise (when considered per session) that has been shown to induce positive effects on health.
Insulin sensitivity was increased by 28% in men following REHIT. The magnitude of this change is comparable with responses to 2 weeks of classic HIT in recreationally active men and women (Babraj et al. 2009; Richards et al. 2010) and in obese men (Whyte et al. 2010). Our results suggest that repeated glycogen depletion might be a key determinant of improved insulin sensitivity following HIT, at least in young lean sedentary male subjects. However, as we did not determine glycogen depletion during the REHIT training sessions this is only speculative, and further studies are required to elucidate the mechanisms by which REHIT improves insulin sensitivity.
The improvements in insulin sensitivity after REHIT appear to be gender-specific as mean insulin sensitivity was not improved in the female subjects after the training program. This is in contrast to a previous study which did not observe gender differences in the improvements in insulin sensitivity in 12 recreationally active subjects after 2 weeks of classic HIT (Richards et al. 2010). No other study has investigated the effects of HIT on insulin sensitivity in women. Following a traditional aerobic exercise intervention in a large cohort, insulin sensitivity improved to a greater degree in men when compared with women but (similar to our study) the female participants had a higher baseline level of insulin sensitivity which may have impacted on the subsequent training response (Boule et al. 2005). The gender differences in the change in insulin sensitivity in response to our REHIT intervention may in part be caused by the low statistical power of our study, with only eight female subjects performing the REHIT intervention. However, it can be speculated that differences in metabolic perturbations during the brief high-intensity cycle sprints may contribute to the observed gender difference, as women have been shown to break down up to 50% less glycogen during a single Wingate sprint (Esbjornsson-Liljedahl et al. 1999, 2002). From this perspective, it would be interesting to determine whether the extent of muscle glycogen breakdown during a REHIT training bout correlates with changes in GLUT4 protein content, insulin-stimulated canonical signalling protein content and activation, glycogen synthase activity, and insulin sensitivity following the training program. Alternatively, it could be that our small sample included several non-responders. Previous studies have comprehensively demonstrated that following a period of exercise training part of the population will not adapt for specific parameters (non-responders), and for insulin sensitivity this has been shown to be the case for up to 40% of the population (Boule et al. 2005; Vollaard et al. 2009; Bouchard and Rankinen 2001). Therefore, further studies with larger sample sizes will be needed to confirm or refute our initial observations. Furthermore, the post-intervention OGTT was scheduled 3 days following the final exercise session, and we cannot rule out that insulin sensitivity was improved in female subjects at an earlier time-point. Finally, although we did not measure power output during the sprints, we observed that some of the female volunteers struggled with the transition from 60 W to the all-out sprints, and were unable to substantially increase their pedal frequency, and thus their power output during the sprints. This may have increased the aerobic contribution to energy supply and reduced glycogen depletion. For sedentary women substituting the 60 W cycling with unloaded pedalling may make the sprints more effective.
Aerobic capacity increased by 15 and 12% in men and women, respectively, after the REHIT intervention, an important observation since a high aerobic capacity is associated with a lower risk of cardiometabolic disease (Church et al. 2005; Wei et al. 1999). Interestingly, since women improved their aerobic capacity but not their insulin sensitivity, it appears that there is a dissociation between changes in aerobic capacity and changes in insulin sensitivity.
Average RPE values reported on immediate completion of the REHIT training sessions were comparable with RPE values obtained during prolonged moderate intensity cardiorespiratory exercise at 50–75% \( \dot{V}{\text{O}}{}_{2}{\text{peak}} \) (Borg 1982). However, there are limitations to the use of the RPE scale in the current study, as the RPE scale is designed for use during (or immediately following) continuous exercise at a constant intensity and may not be a valid measure of exertion during interval based exercises, especially when values are given retrospective of the most intense exercise, as was the case in this study. RPE values obtained in this manner may underestimate exertion during the sprints; indeed, other studies where RPE has been obtained following a 20 s all out sprint have reported higher values of ~16–18 (Baker et al. 2001; Gearhart et al. 2005). However, we were interested in gaining an exertion measure to characterise our entire training intervention and our subjects were asked to consider the whole 10 min exercise session when giving their ratings. Whether the effort required to perform REHIT sessions would deter individuals from performing this type of intervention is a question to be answered in future studies.
In conclusion, in this study we have shown that a very brief and feasible exercise intervention is associated with improvements in metabolic health and aerobic capacity. Our findings suggest that this REHIT protocol may offer a genuinely time-efficient alternative to HIT and conventional cardiorespiratory exercise training for improving risk factors of T2D.
References
Allender S, Peto V, Scarborough P, Kaur A, Rayner M (2008) Coronary heart disease statistics. British Heart Foundation Health Promotion Research Group, Oxford
American Diabetes Association (2008) American Diabetes Association: economic costs of diabetes in the US in 2007. Diabetes Care 31(3):596–615. doi:10.2337/dc08-9017
Babraj JA, Vollaard NB, Keast C, Guppy FM, Cottrell G, Timmons JA (2009) Extremely short duration high intensity interval training substantially improves insulin action in young healthy males. BMC Endocr Disord 9:3. doi:10.1186/1472-6823-9-3
Baker JS, Bailey DM, Davies B (2001) The relationship between total-body mass, fat-free mass and cycle ergometry power components during 20 seconds of maximal exercise. J Sci Med Sport 4(1):1–9
Booth FW, Chakravarthy MV, Spangenburg EE (2002) Exercise and gene expression: physiological regulation of the human genome through physical activity. J Physiol 543(Pt 2):399–411 pii: PHY_019265
Borg G (1970) Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med 2(2–3):92–98
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14(5):377–381
Bouchard C, Rankinen T (2001) Individual differences in response to regular physical activity. Med Sci Sports Exerc 33(6 Suppl):S446–S451 (discussion S452–443)
Boule NG, Weisnagel SJ, Lakka TA, Tremblay A, Bergman RN, Rankinen T, Leon AS, Skinner JS, Wilmore JH, Rao DC, Bouchard C (2005) Effects of exercise training on glucose homeostasis: the HERITAGE family study. Diabetes Care 28(1):108–114 pii:28/1/108
Burgomaster KA, Hughes SC, Heigenhauser GJ, Bradwell SN, Gibala MJ (2005) Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans. J Appl Physiol 98(6):1985–1990. doi:10.1152/japplphysiol.01095.2004
Burgomaster KA, Cermak NM, Phillips SM, Benton CR, Bonen A, Gibala MJ (2007) Divergent response of metabolite transport proteins in human skeletal muscle after sprint interval training and detraining. Am J Physiol Regul Integr Comp Physiol 292(5):R1970–R1976. doi:10.1152/ajpregu.00503.2006
Burgomaster KA, Howarth KR, Phillips SM, Rakobowchuk M, Macdonald MJ, McGee SL, Gibala MJ (2008) Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol 586(1):151–160. doi:10.1113/jphysiol.2007.142109
Cederholm J, Wibell L (1990) Insulin release and peripheral sensitivity at the oral glucose-tolerance test. Diabetes Res Clin Pract 10(2):167–175
Church TS, LaMonte MJ, Barlow CE, Blair SN (2005) Cardiorespiratory fitness and body mass index as predictors of cardiovascular disease mortality among men with diabetes. Arch Intern Med 165(18):2114–2120. doi:10.1001/archinte.165.18.2114
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. doi:10.1249/01.mss.0000078924.61453.fb
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M (2011) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. doi:10.1016/S0140-6736(11)60679-X
DeFronzo RA, Tripathy D (2009) Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 32:S157–S163. doi:10.2337/dc09-S302
Derave W, Hansen BF, Lund S, Kristiansen S, Richter EA (2000) Muscle glycogen content affects insulin-stimulated glucose transport and protein kinase B activity. Am J Physiol Endocrinol Metab 279(5):E947–E955
Esbjornsson-Liljedahl M, Sundberg CJ, Norman B, Jansson E (1999) Metabolic response in type I and type II muscle fibers during a 30-s cycle sprint in men and women. J Appl Physiol 87(4):1326–1332
Esbjornsson-Liljedahl M, Bodin K, Jansson E (2002) Smaller muscle ATP reduction in women than in men by repeated bouts of sprint exercise. J Appl Physiol 93(3):1075–1083. doi:10.1152/japplphysiol.00732.1999
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP (2011) Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43(7):1334–1359. doi:10.1249/MSS.0b013e318213fefb
Gearhart RF Jr, Becque MD, Palm CM, Hutchins MD (2005) Rating perceived exertion during short duration, very high intensity cycle exercise. Percept Mot Skills 100(3 Pt 1):767–773
Gibala MJ, Little JP, van Essen M, Wilkin GP, Burgomaster KA, Safdar A, Raha S, Tarnopolsky MA (2006) Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. J Physiol 575(Pt 3):901–911. doi:10.1113/jphysiol.2006.112094
Gibala MJ, McGee SL, Garnham AP, Howlett KF, Snow RJ, Hargreaves M (2009) Brief intense interval exercise activates AMPK and p38 MAPK signaling and increases the expression of PGC-1 alpha in human skeletal muscle. J Appl Physiol 106(3):929–934. doi:10.1152/japplphysiol.90880.2008
Gonzalez EL, Johansson S, Wallander MA, Rodriguez LA (2009) Trends in the prevalence and incidence of diabetes in the UK: 1996–2005. J Epidemiol Community Health 63(4):332–336. doi:10.1136/jech.2008.080382
Graham TE, Yuan Z, Hill AK, Wilson RJ (2010) The regulation of muscle glycogen: the granule and its proteins. Acta Physiol (Oxf) 199(4):489–498. doi:10.1111/j.1748-1716.2010.02131.x
Hawley JA, Gibala MJ (2009) Exercise intensity and insulin sensitivity: how low can you go? Diabetologia 52(9):1709–1713. doi:10.1007/s00125-009-1425-5
Jensen J, Jebens E, Brennesvik EO, Ruzzin J, Soos MA, Engebretsen EM, O’Rahilly S, Whitehead JP (2006) Muscle glycogen inharmoniously regulates glycogen synthase activity, glucose uptake, and proximal insulin signaling. Am J Physiol Endocrinol Metab 290(1):E154–E162. doi:10.1152/ajpendo.00330.2005
Kawanaka K, Nolte LA, Han DH, Hansen PA, Holloszy JO (2000) Mechanisms underlying impaired GLUT-4 translocation in glycogen-supercompensated muscles of exercised rats. Am J Physiol Endocrinol Metab 279(6):E1311–E1318
Korkiakangas EE, Alahuhta MA, Laitinen JH (2009) Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: a systematic review. Health Promot Int 24(4):416–427. doi:10.1093/heapro/dap031
Laurent D, Hundal RS, Dresner A, Price TB, Vogel SM, Petersen KF, Shulman GI (2000) Mechanism of muscle glycogen autoregulation in humans. Am J Physiol Endocrinol Metab 278(4):E663–E668
Litherland GJ, Morris NJ, Walker M, Yeaman SJ (2007) Role of glycogen content in insulin resistance in human muscle cells. J Cell Physiol 211(2):344–352. doi:10.1002/jcp.20942
Little JP, Gillen JB, Percival M, Safdar A, Tarnopolsky MA, Punthakee Z, Jung ME, Gibala MJ (2011) Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J Appl Physiol. doi:10.1152/japplphysiol.00921.2011
Parolin ML, Chesley A, Matsos MP, Spriet LL, Jones NL, Heigenhauser GJ (1999) Regulation of skeletal muscle glycogen phosphorylase and PDH during maximal intermittent exercise. Am J Physiol 277(5 Pt 1):E890–E900
Piche ME, Lemieux S, Corneau L, Nadeau A, Bergeron J, Weisnagel SJ (2007) Measuring insulin sensitivity in postmenopausal women covering a range of glucose tolerance: comparison of indices derived from the oral glucose tolerance test with the euglycemic–hyperinsulinemic clamp. Metabolism 56(9):1159–1166. doi:10.1016/j.metabol.2007.04.002
Rakobowchuk M, Tanguay S, Burgomaster KA, Howarth KR, Gibala MJ, MacDonald MJ (2008) Sprint interval and traditional endurance training induce similar improvements in peripheral arterial stiffness and flow-mediated dilation in healthy humans. Am J Physiol Regul Integr Comp Physiol 295(1):R236–R242. doi:10.1152/ajpregu.00069.2008
Reichert FF, Barros AJ, Domingues MR, Hallal PC (2007) The role of perceived personal barriers to engagement in leisure-time physical activity. Am J Public Health 97(3):515–519. doi:10.2105/AJPH.2005.070144
Richards JC, Johnson TK, Kuzma JN, Lonac MC, Schweder MM, Voyles WF, Bell C (2010) Short-term sprint interval training increases insulin sensitivity in healthy adults but does not affect the thermogenic response to beta-adrenergic stimulation. J Physiol 588(Pt 15):2961–2972. doi:10.1113/jphysiol.2010.189886
Richter EA, Derave W, Wojtaszewski JF (2001) Glucose, exercise and insulin: emerging concepts. J Physiol 535(Pt 2):313–322 pii: PHY_12798
Steinberg GR, Watt MJ, McGee SL, Chan S, Hargreaves M, Febbraio MA, Stapleton D, Kemp BE (2006) Reduced glycogen availability is associated with increased AMPKalpha2 activity, nuclear AMPKalpha2 protein abundance, and GLUT4 mRNA expression in contracting human skeletal muscle. Appl Physiol Nutr Metab 31(3):302–312. doi:10.1139/h06-003
Thomas S, Reading J, Shephard RJ (1992) Revision of the physical-activity readiness questionnaire (PAR-Q). Can J Sport Sci Revue Canadienne Des Sci Du Sport 17(4):338–345
Thyfault JP, Krogh-Madsen R (2011) Metabolic disruptions induced by reduced ambulatory activity in free living humans. J Appl Physiol. doi:10.1152/japplphysiol.00478.2011
Trilk JL, Singhal A, Bigelman KA, Cureton KJ (2010) Effect of sprint interval training on circulatory function during exercise in sedentary, overweight/obese women. Eur J Appl Physiol. doi:10.1007/s00421-010-1777-z
Vollaard NB, Constantin-Teodosiu D, Fredriksson K, Rooyackers O, Jansson E, Greenhaff PL, Timmons JA, Sundberg CJ (2009) Systematic analysis of adaptations in aerobic capacity and submaximal energy metabolism provides a unique insight into determinants of human aerobic performance. J Appl Physiol 106(5):1479–1486. doi:10.1152/japplphysiol.91453.2008
Wei M, Kampert JB, Barlow CE, Nichaman MZ, Gibbons LW, Paffenbarger RS Jr, Blair SN (1999) Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA 282(16):1547–1553 pii: joc90699
Whyte LJ, Gill JM, Cathcart AJ (2010) Effect of 2 weeks of sprint interval training on health-related outcomes in sedentary overweight/obese men. Metabolism 59(10):1421–1428. doi:10.1016/j.metabol.2010.01.002
Acknowledgments
We would like to thank John Fox for technical assistance, and Paul Aikman, Ben Ashcroft, Barnaby Barber, Sarah Dunnett, Mahmoud Gholoum, Liam Harper, Andrew Hebson, Adam Reed, Keith Simpson and Alison Thomson for assistance with testing and the training sessions. The study was funded by Heriot-Watt University.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by David C. Poole.
Rights and permissions
About this article
Cite this article
Metcalfe, R.S., Babraj, J.A., Fawkner, S.G. et al. Towards the minimal amount of exercise for improving metabolic health: beneficial effects of reduced-exertion high-intensity interval training. Eur J Appl Physiol 112, 2767–2775 (2012). https://doi.org/10.1007/s00421-011-2254-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-2254-z