Abstract
This study examined the effects of menstrual cycle phase (MCP) upon sprinting and recovery as well as upon metabolic responses to such exercise. Eight females performed a repeated 30-s sprint on a non-motorised treadmill interspersed with a 2-min rest in three phases of the MCP, follicular (low 17β-estradiol and progesterone), just prior to ovulation (midcycle trial, highest 17β-estradiol concentration and low progesterone) and in the luteal phase (high 17β-estradiol and high progesterone). MCP was verified later by radioimmunoassay of 17β-estradiol and progesterone. Peak power output (PPO) and mean power output (MPO) were unaltered (P > 0.05) due to MCP [PPO for sprint 1: 463 (18) W vs. 443 (15) W vs. 449 (18) W; PPO for sprint 2: 395 (17) W vs. 359 (16) W vs. 397 (17) W; MPO for sprint 1: 302 (15) W vs. 298 (13) W vs. 298 (14) W; MPO for sprint 2: 252 (10) W vs. 248 (10) W vs. 259 (12) W for follicular, midcycle and luteal trial, mean (SEM), respectively]. Similarly, percentage recovery of PPO and MPO (the PPO or MPO during sprint 2 expressed as a percentage of the PPO or MPO during sprint 1) was also unchanged (P > 0.05). Blood lactate, blood pH and plasma ammonia after sprinting and estimated plasma volume were also unaltered by MCP (P > 0.05). These findings suggest that hormonal fluctuations due to MCP do not interfere with maximal intensity whole body sprinting and the metabolic responses to such exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increased participation in sport by women has led to enhanced interest in the physiological and metabolic responses of women to sport and exercise (e.g. Constantini et al. 2005). It has been important, therefore, to examine the effects of hormonal fluctuations, due to the female menstrual cycle, upon metabolism and performance. The majority of the studies to date have dealt with the effects of menstrual cycle phase (MCP) on metabolic, ventilatory and cardiovascular responses at rest and during sub-maximal exercise and recovery as well as with sub-maximal intensity exercise performance (Constantini et al. 2005). Few studies have examined the effect of the MCP on sprinting (all out effort of around 30 s or less) and the findings in the literature are equivocal. For example, better performance during the follicular phase has been shown for a single swimming sprint and for repeated sprint cycling (Bale and Nelson 1985; Parish and Jakeman 1987) whereas better performance during the luteal phase has been shown for a single cycle sprint and repeated cycling sprints (Masterson 1999; Middleton and Wenger 2006). Furthermore, two studies examining a single cycle sprint and repeated cycle ergometer sprints have shown no impact of the MCP on performance (Busman et al. 2006; Miskec et al. 1997). Finally, improved performance in the follicular phase during jumping has been shown only where there were premenstrual or menstrual problems (Giacomoni et al. 2000). There have been no studies examining the impact of the MCP on sprint running. These differences in findings across studies may be due to the lack of hormonal documentation of the cycle phase in some studies (Bale and Nelson 1985; Busman et al. 2006; Masterson 1999; Miskec et al. 1997; Parish and Jakeman 1987), and/or due to premenstrual or menstrual problems (Giacomoni et al. 2000) towards the end of the ovarian cycle or during the first days of the bleeding episode in some others (Bale and Nelson 1985; Masterson 1999; Parish and Jakeman 1987).
Strength plays an important role in sprinting (Delecluse 1997) and a relationship has been previously reported between high concentrations of 17β-estradiol and progesterone and strength (Phillips et al. 1993; Reis et al. 1995; Sarwar et al. 1996; Taaffe et al. 2005). Thus, through an influence on strength, ovarian hormones may influence sprinting and/or recovery from sprinting. Such an effect would result in a better performance during the luteal phase of the menstrual cycle (high concentrations of 17β-estradiol and progesterone) or just prior to ovulation (high concentrations of 17β-estradiol) in comparison with the follicular phase. There are no data, however, to date to directly compare the effects of endogenous concentrations of these hormones (follicular, prior to ovulation and luteal phase) upon sprinting, or on recovery from sprinting.
In spite of the importance of repeated sprint ability in many sports (Rechichi and Dawson 2009), recovery from sprinting (the performance during the second sprint expressed as a percentage of the performance during the first sprint) has been little investigated. It has been suggested that ovarian hormones may affect phosphocreatine (PCr) recovery rates induced by the slower rates of PCr recovery after plantar flexion exercises in amenorrheic-endurance athletes in comparison with eumenorrheic (Harber et al. 1998). Higher PCr recovery has also been suggested by Middleton and Wenger (2006) where work over a series of ten 6-s sprints was greater in the luteal phase in comparison with the midfollicular. It has also been suggested that increased concentrations of 17β-estradiol may improve muscle buffering capacity during 10 s of sprint rowing (Redman and Weatherby 2004). Since both PCr recovery (Bogdanis et al. 1996) and muscle buffering capacity (Maughan et al. 1997) are associated with sprinting recovery, it could be postulated that in different phases of a menstrual cycle sprinting recovery might also be different. Rechichi and Dawson (2009) compared the effects of exogenous oral contraception consumption phase (low endogenous 17β-estradiol and progesterone) with early (low endogenous 17β-estradiol and progesterone) and late (low endogenous progesterone only) withdrawal phase (withdrawal from the oral contraceptives) and did not find differences in mean and/or peak power in any of the sprints. Metabolic responses were not examined in this study.
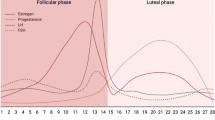
Given the equivocal nature of findings in the literature, the lack of studies examining sprint running per se, the unknown metabolic responses to sprinting in various phases of the menstrual cycle, the sparsity of information on repeated sprints, the perceived methodological limitations of previous studies and the relatively recent identification of oestrogen receptors in human skeletal muscles (Lemoine et al. 2003), the purpose of the present study is to assess whether sprinting, recovery from sprinting and metabolic responses are influenced during three distinct and carefully controlled phases of the menstrual cycle (Fig. 1, see the below section for detail).
Methods
Subjects
Fourteen female sports science students volunteered to participate in the present investigation. They were all highly active and members of the university team in their sports. All but one (recreational athlete but involved in power events) of the subjects were involved in multiple sprints or power events (hockey, soccer, athletics, basketball and rugby). Their mean (SEM) age, body mass and stature were 20.1 (0.3) years (range 18–22), 64.5 (1.7) kg and 1.68 (0.01) m, respectively. Volunteers were informed of the purpose of the study, any known risks, benefits and the right to terminate the participation at will, both orally and in writing, prior to signing a consent form. The experimental protocol had the approval of the Ethical Committee of Loughborough University.
MCP information
All the subjects were eumenorrheic and had not used oral contraceptives for at least 4 months before their participation in experimental procedures. Subjects were non-smokers and were not on any medications that could interfere with the experimental procedures. Their cycle length varied between 25 and 40 days. Subjects were accepted for the study only if their menstrual cycle length was no longer than 40 days (Lenton et al. 1984). Information about cycle length was initially obtained by a menstrual cycle history questionnaire. A cycle was calculated from the first day of menstrual bleeding (included) until the first day of the next bleeding (excluded). Hormonal verification of MCP was determined later by analysis for 17β-estradiol and progesterone and subjects were excluded from the analysis if they did not meet one or more of the pre-established criterion which were a luteal phase length of 11–17 days (Lenton et al. 1984) and a luteal phase serum progesterone concentration >9.54 nmol L−1 (Shepard and Senturia 1977). The length of the follicular phase was calculated from the first day of menstrual cycle (included) until and including the luteinising hormone (LH) surge. The luteal phase was defined as the first day after the LH surge until the last day of the cycle. Evidence of ovulation was obtained using the Clear Plan Home Ovulation Test (Unipath Limited, Bedford, UK), which detected the LH surge using urine samples. The accuracy of these types of kits has been tested experimentally and shown to be satisfactory (Bourne et al. 1996; Miller and Soules 1996). Depending on each participant’s menstrual cycle length, urine testing started 9–17 days after the onset of the menses and continued until the LH surge was detected. For the midcycle trial, the subjects rang the laboratory on the morning of the positive Clear Plan Home Ovulation Test result and reported to the laboratory on that same day.
Figure 1 gives the schematic representation of the testing in parallel with the hormonal fluctuations. This design meant that the present study was novel in that subjects were tested just prior to ovulation when only 17β-estradiol concentration was high (World Health Organisation 1980), which practically was a rather short period of time (about a day). The Clear Plan Home Ovulation Test detects not the peak LH concentration, but rather the LH surge (the Clear Plan Home Ovulation Test becomes “positive” when concentration of LH is >40 IU L−1), which is a better predictor of ovulation due to the episodic nature of LH release from the anterior pituitary (Speroff 1999). Peak 17β-estradiol concentrations are attained 24–36 h prior to ovulation (World Health Organisation 1980) and coincide with the onset of the LH surge (Fritz et al. 1992), a period that is in line with the urine detection of LH (Miller and Soules 1996). Thus, theoretically, the method employed in the present study should have facilitated exercise testing at approximately the time of the 17β-estradiol peak. The midcycle trial was included in the analysis only when the urine detection of LH surge was accompanied by higher midcycle 17β-estradiol concentrations than those observed during the luteal phase and concomitant serum progesterone concentrations higher than those observed in the early follicular phase but ≤6.36 nmol L−1 (Speroff 1999). The rationale of testing at the preovulatory point (midcycle trial) was to naturally isolate the 17β-estradiol and to investigate its effects, if any, on metabolism and performance during the repeated 30-s sprint without the concomitant influence of progesterone which has been shown to have antagonistic effects in some metabolic conditions (Bunt 1990; March et al. 1979; Speroff 1999).
Protocol and experimental design
After familiarisation and preliminary trials, subjects undertook the performance test which was a repeated 30-s sprint interspersed with a 2-min passive recovery period on three occasions (follicular phase, just prior to ovulation, luteal phase) in a random order and at the same time of the day on a non-motorised treadmill (Woodway model AB). The sprints were at a maximal self-regulated velocity and participants were instructed to sprint as fast as possible (flat out) from the beginning of each sprint (with the command “go”). This procedure was rehearsed by the participants during the familiarisation sessions. Figure 2 illustrates the schematic representation of the protocol. The treadmill was modified and instrumented as previously described (Lakomy 1987). The performance variables recorded during these sprints were peak power output (PPO), mean power output (MPO), fatigue index for power (FIPO), peak speed (PS), mean speed (MS) and fatigue index for speed (FISP). Also, the recovery of the above variables (the result during sprint 2 expressed as a percentage of the result during sprint 1) was also recorded. Subjects undertook at least five practices on separate days (each of 30 min duration) prior to the main trials in order to be fully familiarised with sprinting on the non-motorised treadmill. Each subject was instructed to refrain (24 h) from alcohol and (12 h) from caffeine prior to the experimental procedures whereas in the same period (24 h) only light exercise was permitted. Prior to each main trial subjects completed, a standard warm-up consisted of 3 min of jogging at 2.0 m s−1 followed by 5-min stretching and two 30-s sub-maximal runs at 3.0 and 3.5 m s−1, respectively, interspersed with 30-s rest.
Preliminary tests
Prior to the performance trials, the endurance fitness of the subjects was established by a \( {\dot{\text{V}}}{\text{O}}_{{2\,{ \max }}} \) test (Taylor et al. 1955) and the determination of blood lactate concentration at sub-maximal running speeds (speed-lactate test) on a level treadmill (Woodway, USA) as the \( \%{\dot{\text{V}}}{\text{O}}_{{2\,{ \max }}} \) at a given blood lactate concentration (%4 mM) has been shown to increase with training (Hurley et al. 1984). The speeds for the speed-lactate test were calculated to represent 60, 70, 80, and 90% (4 min for each stage) of the subject’s \( {\dot{\text{V}}}{\text{O}}_{{2\,{ \max }}} \). These two tests were conducted on separate days. For the speed-lactate test, duplicate capillary blood samples were collected by means of fingertip for later analysis of blood lactate (Maughan 1982). These samples were drawn at rest (upright posture), at the end of each 4-min stage while the subject was running on the treadmill (for the first three stages) and at the end of the fourth stage while the subject was in the upright posture. These tests were conducted to enable comparison of the training status of participants in this and other published studies.
Blood collection and analysis
Venous blood samples were drawn at rest, post-warm-up, immediately after the first sprint, immediately after the second sprint and at 5, 10, 15, 20 and 30 min during the recovery from the second sprint (Fig. 2), via an indwelling cannula inserted into an antecubital or forearm vein. The resting sample was taken after the volunteers had rested in a semi-supine position on the experimental couch for at least 20 min in order to standardise initial plasma volume and thus minimise any confounding effect of posture. For the same reasons, great care was also taken to keep the sampling arm in the same position. Posture was also standardised for the post-exercise samples. Blood pH was determined immediately (ABL™ Blood Gas System, Copenhagen, Denmark). Duplicate 20 μL blood samples were dispensed into pre-treated tubes with 200 μL of 0.4 mol L−1 perchloric acid to ensure deproteinisation and blood lactate concentration was determined at a later date (Maughan 1982). Another aliquot of blood (1.5 mL) was dispensed immediately into a calcium heparinized tube, centrifuged, and the plasma supernatant was stored at −70°C. The ammonia assay was performed enzymatically within 48 h after the collection of the blood (MPR 1Ammonia, Boehringer Mannheim UK, Ltd, Lewes, UK). Haematocrit (Hct) was assessed in triplicate (Hawksley and Sons Ltd, Lancing, UK). Haemoglobin (Hb) concentration was determined using the cyanmethaemoglobin method (Boehringer Mannheim, Gmbh Test-combination, Mannheim, Germany). Plasma volume relative changes were then estimated from the Hb and Hct values using the method described by Dill and Costill (1974). The 17β-estradiol and progesterone assays were performed with the Coat-A-Count 17β-estradiol and progesterone method, respectively, which is a no-extraction, solid-phase 125I radioimmunoassay designed for the quantitative measurement of 17β-estradiol and progesterone in serum (Coat-A-Count 17β-estradiol/progesterone, Diagnostics Products Corporation, Los Angeles, USA). Both assays were performed with the aid of an automated gamma counter (Cobra II, Packard Instrument Company Inc, USA). Intra-assay coefficient of variations for 17β-estradiol and progesterone was 7.0 and 4.6%, respectively.
Statistical analysis
Prior to the statistical analysis tests, data were checked for normality (using SPSS for windows version 15). A two-way analysis of variance for within-subjects design was used to assess whether there were any differences in performance variables among MCPs (main effect: cycle phase) and between the first and second sprints in each phase (main effect: sprint). One-way analysis of variance for a within-subjects design was used to examine if any differences existed in recovery of performance variables among MCPs (main effect: cycle phase). Two-way analysis of variance for a within-subjects design was used to ascertain any differences in metabolic responses between MCPs (main effect: cycle phase) and the response to each subject with respect to time, including in the analysis the resting, post-warm-up, post-sprint and recovery responses (main effect: time). When significant interactions (phase by sprint or phase by time) were revealed, the Bonferroni method was used for multiple comparisons. Relationships between the variables were evaluated by means of Pearson moment correlation coefficients. Results are expressed as mean (SEM), unless otherwise stated. Significance was set at P < 0.05.
Results
Hormonal documentation of MCP
Resting serum 17β-estradiol and progesterone concentrations confirmed the MCPs for 8 of the 14 subjects (Table 1). For these eight subjects, there were 4.3- and 3-fold increase in 17β-estradiol (P < 0.01 in both cases) and 2.3- and 13.2-fold increase in progesterone (P < 0.01 in both cases) at the midcycle and luteal phases, respectively. The remainder of the subjects (n = 6) was excluded from the study due to their failure to meet one or more from the pre-established criterion of hormonal concentrations. No premenstrual or menstrual cycle discomfort was reported from the subjects (from menstrual cycle history questionnaire, data not shown).
Performance data
Body mass was not altered significantly due to MCP [62.9 (2.2) kg, 63.1 (2.1) kg and 62.8 (2.0) kg for follicular, midcycle and luteal phases, respectively, P > 0.05] and, therefore, data are not normalised for body mass (e.g. divided by body mass). Performance variables (i.e. MPO, PPO, PS) are presented in Table 2. None of these variables were altered due to MCP (P > 0.05). However, the performance profile in sprint 1 was always higher than in sprint 2 (P < 0.05), apart from the FIPO and FISP which were not different (P > 0.05). Percentage recovery of power output and speed was also unaffected by MCP (P > 0.05; Table 3). There was a significant correlation between recovery of MPO in the midcycle trial and 17β-estradiol (r = 0.75, P < 0.05). On the other hand, no such relationships were found between 17β-estradiol and performance variables for the luteal phase trial. Mean maximum oxygen uptake was 50.1 (2.1) mL kg−1 min−1 while mean %4 mM was 81 (3)%.
Change in plasma volume
Estimated percentage changes in mean plasma volume for post-sprint 1 and post-sprint 2 (greatest changes) were: post-sprint 1: −18.5 (1.3)%, −16.1 (1.6)% and −16.3 (1.1)% for follicular, midcycle and luteal phase trials, respectively; post-sprint 2: −20.8 (1.3)%, −19.5 (2.2)% and −18.1 (1.8)% for follicular, midcycle and luteal phase trials, respectively. Statistical analysis revealed no significant changes due to MCP (P > 0.05). Subsequently, none of the metabolic responses were corrected for plasma volume changes.
Metabolic responses
All the blood metabolites changed over time during each cycle phase (P < 0.01), but MCP did not affect the metabolic responses (Figs. 3, 4).
Venous whole blood lactate and pH concentrations at rest, post-warm-up (PWP), post-sprint 1 (PS1), post-sprint 2 (PS2) and at 5 (5) min, 10 (10) min, 15 (15) min, 20 (20) min and 30 (30) min of recovery after the second sprint at follicular, midcycle and luteal phases of the menstrual cycle [mean (SEM), n = 8]. Venous whole blood lactate and pH responses were increased over time (P < 0.01); however, no menstrual cycle effect was found (P > 0.05)
Venous plasma ammonia concentrations at rest, post-warm-up (PWP), post-sprint 1 (PS1), post-sprint 2 (PS2) and at 5 (5) min, 10 (10) min, 15 (15) min, 20 (20) min and 30 (30) min of recovery after the second sprint at follicular, midcycle and luteal phases of the menstrual cycle [mean (SEM), n = 8]. Venous plasma ammonia responses were increased over time (P < 0.01); however, no menstrual cycle effect was found (P > 0.05)
Discussion
The principal finding of the present study was that the performance profile during a repeated 30-s sprint with 2-min passive recovery was not altered by the hormonal fluctuations of 17β-estradiol and progesterone. In addition, the metabolic responses to a repeated sprint were also unaffected by MCP.
The present study included the novel methodological approach of studying the subjects exactly prior to ovulation where the highest 17β-estradiol concentration exists while progesterone concentration remains low. This period prior to ovulation was verified by radioimmunoassay of resting serum 17β-estradiol and progesterone, in 8 of the 14 individuals who participated in the study. Indeed, resting serum concentrations of 17β-estradiol and progesterone were within the reference range for eumenorrheic women in the respective phases according to the criteria presented in “Methods”. The rigorous design, i.e., the combination of indirect methods (Clear Plan Home Ovulation Test kit and cycle history questionnaire) and hormonal documentation of cycle phase, is of crucial importance when the precise timing of experimental procedures in the context of MCP is to be performed. The need for a well-controlled methodology is even greater when the subjects are young (≈20-year old) as in the present study because of high incidence of anovulatory cycles that occur about that age (Speroff 1999).
The lack of impact of MCP on sprint running is in agreement with earlier studies using maximal intensity cycling exercise (Busman et al. 2006; Miskec et al. 1997). In addition, the current investigation is in line with the findings of Giacomoni et al. (2000) who reported that, as long as the subjects did not suffer with premenstrual and menstrual symptoms (as was the case in this investigation), no alterations in exercise performance that involves eccentric muscle actions will occur. The present study involved sprint running during which eccentric muscle actions play an important role but trials were not undertaken during the first days of the menstrual cycle, when menstrual discomfort usually takes place (Giacomoni et al. 2000), while in the luteal phase trial of the menstrual cycle no such symptoms were reported from the volunteers (from the questionnaire that was given to the subjects, data not shown). The impairment of physical performance due to premenstrual and menstrual pain in the late luteal phase and first days of the menstrual cycle, respectively, could also explain some of the previously reported studies where findings conflict with the present research. In the Bale and Nelson (1985) study, the best 50-m sprint swimming was achieved in days 8–15 in comparison with day 21 to the first day of the next menstrual cycle (their subjects complained of perimenstrual symptoms) defined as the premenstrual period. Menstrual discomfort may also explain the differences in sprinting in Masterson’s (1999) experiment where participants were tested at day 2 from the onset of the menstrual cycle bleeding and during the luteal phase.
The findings of the present investigation do not support the hypothesis that 17β-estradiol has muscle-strengthening effects and that force will be increased, at least, just prior to ovulation (midcycle trial in the present experiment) where 17β-estradiol will be at the highest concentrations while progesterone will be still low. Sarwar et al. (1996), using an isometric contraction experimental model, proposed that 17β-estradiol can alter the negative feedback of inorganic phosphate (Pi) upon cross-bridge kinetics (McLester 1997). Indeed, all studies to date that have shown improvements in force or performance when high concentrations of 17β-estradiol were present have used an isometric exercise model (Phillips et al. 1993; Sarwar et al. 1996; Taaffe et al. 2005). However, in dynamic exercise, as in the present study, type II fibres produce more force than type I fibres (Fitts and Widrick 1996) and it is known, from animal research, that muscle type II fibres are considerably less sensitive to inorganic phosphate both in isometric (Altringham and Johnston 1985) and in dynamic muscle contraction (Widrick 2002) which may explain the lack of influence of 17β-estradiol on sprinting in the present study. Alternatively, based on findings from animal research, this lack of influence could be due to the noticeably lower oestrogen receptors in type II fibres (Saartok 1984).
There was a significant positive correlation between mean resting 17β-estradiol concentrations at the midcycle phase and recovery of MPO (r = 0.75, P < 0.05). One possible explanation for this relationship is that ovarian hormones may affect PCr recovery rates as suggested by the slower rates of PCr recovery after plantar flexion exercises in amenorrheic-endurance athletes in comparison with eumenorrheic (Harber et al. 1998). However, Harber et al. (1998) reported that amenorrheic subjects had a different hypothalamic–pituitary thyroid axis profile compared with eumenorrheic-endurance athletes as indicated by lower thyroxine and triiodothyronine concentrations complicating any clear influences of reproductive hormones on recovery of PCr and thus on the recovery of sprinting (Bogdanis et al. 1996). However, Middleton and Wenger (2006) did find higher work performed over a series of sprints during the luteal phase of the cycle and associated this improvement with the positive influence of 17β-estradiol on PCr restoration. However, peak power or recovery of power was unaltered due to MCP as it was in the present study.
MCP did not alter the metabolic responses to a repeated 30-s sprint. Mean peak whole blood lactate concentration did not change due to MCP, a finding which is consistent with previous investigations (Lynch and Nimmo 1998; Middleton and Wenger 2006). In addition, blood pH values were similar across MCPs. It has been previously suggested that variations in 17β-estradiol due to MCP are only likely to influence metabolism by glycogen sparing in favour of fat oxidation at relatively low exercise intensities below 75% of \( \%{\dot{\text{V}}}{\text{O}}_{{2\,{ \max }}} \) (Hackney et al. 1994). Thus, the findings of the present study, with no impact of MCP on metabolism during sprinting, are in agreement with these earlier suggestions.
It has been suggested that bioavailability (free and not specifically bound) of hormones, rather than total concentrations, may reflect more accurately the clinical situation (Vermeulen et al. 1999). To date, bioavailability of progesterone has not been determined. Bioavailability of 17β-estradiol has been determined, but the studies are equivocal as to whether or not free and/or not specifically bound 17β-estradiol concentration differs across MCPs (Elliott et al. 2003). Thus, it is possible that while the total concentration of 17β-estradiol was higher during the midcycle trial its bioavailability, and thereby its influence, was similar across the MCPs. When methodology allows it, future studies should measure both total and bioavailable concentrations of the hormones in question.
One limitation of the present study is that the small sample size and resultant low power could have masked real differences in performance and metabolism as a result of MCPs. However, the observed variations in performance and metabolism across phases were very small and probably not of importance in a performance context.
In conclusion, this study has shown that sprinting and recovery from sprinting are unaffected during three distinct and carefully controlled phases of the menstrual cycle. Furthermore, blood metabolites following such a repeated sprint were also unaffected by MCP. In addition, the study has shown that naturally isolated higher 17β-estradiol concentrations with low progesterone do not have any significant effect on sprinting and recovery or on the metabolic responses to such exercise. These findings suggest that in future studies it may not be necessary to control the timing of testing due to MCP, as long as pre- and/or perimenstrual problems do not exist.
References
Altringham JD, Johnston IA (1985) Effects of phosphate on the contractile properties of fast and slow muscle fibres from an Antarctic fish. J Physiol 368:491–500
Bale P, Nelson G (1985) The effects of menstruation on performance of swimmers. Aust J Sci Med Sport 17:19–22
Bogdanis GC, Nevill ME, Boobis LH et al (1996) Contribution of phosphocreatine and aerobic metabolism to energy supply during repeated sprint exercise. J Appl Physiol 80:876–884
Bourne TH, Hagstrom H, Hahlin M et al (1996) Ultrasound studies of vascular and morphological changes in the human corpus luteum during the menstrual cycle. Fertil Steril 65:753–758
Bunt JC (1990) Metabolic actions of estradiol: significance for acute and chronic exercise responses. Med Sci Sports Exerc 22:286–290
Busman B, Masterson G, Nelsen J (2006) Anaerobic performance and the menstrual cycle: eumenorrheic and oral contraceptive users. J Sport Med Phys Fitness 46:132–137
Constantini NW, Dubnow G, Lebrun CM (2005) The menstrual cycle and sport performance. Clin Sports Med 24:e51–e82. Available via PubMed. http://www.sportsmed.theclinics.com/title of the article
Delecluse C (1997) Influence of strength training on sprint running performance. Current findings and implications for training. Sports Med 24:147–156
Dill DB, Costill DL (1974) Calculation of percentages changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol 37:247–248
Elliott KJ, Cable NT, Reilly T et al (2003) Effect of menstrual cycle phase on the concentration of bioavailable 17β-oestradiol and testosterone and muscle strength. Clin Sci 105:663–669
Fitts RH, Widrick JJ (1996) Muscle mechanics: adaptations with exercise-training. Exerc Sports Sci Rev 24:427–473
Fritz MA, McLachlan RI, Cohen NL et al (1992) Onset and characteristics of the midcycle surge in bioactive and immunoactive luteinizing hormone secretion in normal women: influence of physiological variations in periovulatory ovarian steroid hormone secretion. J Clin Endocrinol Metab 75:489–493
Giacomoni M, Bernard T, Gavarry O et al (2000) Influence of menstrual cycle phase and menstrual symptoms on maximal anaerobic performance. Med Sci Sports Exerc 32:486–492
Hackney AC, McCracken-Compton MA, Aisworth B (1994) Substrate responses to submaximal exercise in the midfollicular and midluteal phases of the menstrual cycle. Int J Sport Nutr 4:299–308
Harber VJ, Petersen SR, Chilibeck PD (1998) Thyroid hormone concentrations and muscle metabolism in amenorrheic and eumenorrheic athletes. Can J Appl Physiol 23:293–306
Hurley BF, Hagberg JM, Allen WK et al (1984) Effect of training on blood lactate levels during submaximal exercise. J Appl Physiol 56:1260–1264
Lakomy HKA (1987) The use of a non-motorised treadmill for analysing sprint performance. Ergonomics 30:627–637
Lemoine S, Granier P, Tiffoche C et al (2003) Estrogen receptor Alpha mRNA in human skeletal muscles. Med Sci Sports Exerc 35:439–443
Lenton EA, Landgren BM, Sexton L (1984) Normal variation in the length of the luteal phase of the menstrual cycle: identification of the short luteal phase. Br J Obstet Gynaecol 91:685–689
Lynch NJ, Nimmo MA (1998) Effects of menstrual cycle phase and oral contraceptive use on intermittent exercise. Eur J Appl Physiol 78:565–572
March CM, Goebelsmann U, Nakamura RM, Mishell DR Jr (1979) Roles of estradiol and progesterone in eliciting the midcycle luteinizing hormone and follicle-stimulating hormone surges. J Clin Endocrinol Metab 49:507–513
Masterson G (1999) The impact of menstrual cycle phases on anaerobic power performance in collegiate women. J Strength Cond Res 13:325–329
Maughan R (1982) A simple, rapid method for the determination of glucose, lactate pyruvate, alanine, 3-hydroxyburate and acetoacetate on a single 20-μl blood sample. Clin Chim Acta 122:231–240
Maughan R, Gleeson M, Greenhaff PL (1997) Biochemistry of exercise and training. Oxford University Press, Oxford
McLester JR (1997) Muscle contraction and fatigue. The role of adenosine 5′-diphosphate and inorganic phosphate. Sports Med 23:287–305
Middleton LE, Wenger HA (2006) Effects of menstrual cycle phase on performance and recovery in intense intermittent activity. Eur J Appl Physiol 96:53–58. doi:10.1007/s00421-005-0073-9
Miller PB, Soules MR (1996) The usefulness of a urinary LH kit for ovulation prediction during menstrual cycles of normal women. Obstet Gynecol 87:13–17
Miskec CM, Potteiger JA, Nau KL et al (1997) Do varying environment and menstrual cycle conditions affect anaerobic power output in female athletes. J Strength Cond Res 11:219–223
Parish HC, Jakeman PM (1987) The effects of menstruation upon repeated maximal sprint performance (abstract). J Sports Sci 5:78
Phillips SK, Rook LM, Siddle NC et al (1993) Muscle weakness in women occurs at an earlier age than in men, but strength is preserved by hormone replacement therapy. Clin Sci 84:95–98
Rechichi C, Dawson B (2009) Effect of oral contraceptive cycle phase on performance in team sport players. J Sci Med Sport 12:190–195
Redman LM, Weatherby RP (2004) Measuring performance during the menstrual cycle: a model using oral contraceptives. Med Sci Sports Exerc 36:130–136
Reis E, Frick U, Schmdtbleicher D (1995) Frequency variations of strength training sessions triggered by the phases of the menstrual cycle. Int J Sports Med 16:545–550
Saartok T (1984) Steroid receptors in two types of rabbit skeletal muscle. Int J Sports Med 5:130–136
Sarwar R, Niclos BB, Rutherford OM (1996) Changes in muscle strength, relaxation rate and fatiguability during the human menstrual cycle. J Physiol 493:267–272
Shepard MK, Senturia YD (1977) Comparison of serum progesterone and endometrial biopsy for confirmation of ovulation and evaluation of luteal function. Fertil Steril 28:541–548
Speroff L (1999) Clinical gynecologic endocrinology and infertility, 6th edn. Lippincott Williams and Wilkins, Philadelphia
Taaffe DR, Newman AB, Haggerty CL et al (2005) Estrogen replacement, muscle composition, and physical function: the health ABC study. Med Sci Sports Exerc 37:1741–1747
Taylor HL, Buskirk E, Henschel A (1955) Maximal oxygen uptake as an objective measure of cardiorespiratory performance. J Appl Physiol 8:73–80
Vermeulen A, Verdonck L, Kaufman JM (1999) A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 84:3666–3672
Widrick JJ (2002) Effect of Pi on unloaded shortening velocity of slow and fast mammalian muscle fibers. Am J Physiol Cell Physiol 282:C647–C653
World Health Organisation, Task Force for Methods for the Determination of the Fertile Period, Special Programme of Research, Development and Research Training in Human Reproduction (1980) Temporal relationships between ovulation and defined changes in the concentration of plasma estradiol-17β, luteinizing hormone, follicle-stimulating hormone, and progesterone. Am J Obstet Gynecol 138:383–390
Acknowledgments
This study and Antonios Tsampoukos were supported by funding from the Greek State Scholarships Foundation. The authors would like to thank Dr Henryk K.A. Lakomy for his advice with respect to the non-motorised treadmill. The authors declare that the experiments comply with the current laws of the country in which they were performed.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Susan Ward.
Rights and permissions
About this article
Cite this article
Tsampoukos, A., Peckham, E.A., James, R. et al. Effect of menstrual cycle phase on sprinting performance. Eur J Appl Physiol 109, 659–667 (2010). https://doi.org/10.1007/s00421-010-1384-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-010-1384-z