Abstract
The present study investigated the effect of 21 days of horizontal bed rest on cutaneous cold and warm sensitivity, and on behavioural temperature regulation. Healthy male subjects (N = 10) were accommodated in a hospital ward for the duration of the study and were under 24-h medical care. All activities (eating, drinking, hygiene, etc.) were conducted in the horizontal position. On the 1st and 22nd day of bed rest, cutaneous temperature sensitivity was tested by applying cold and warm stimuli of different magnitudes to the volar region of the forearm via a Peltier element thermode. Behavioural thermoregulation was assessed by having the subjects regulate the temperature of the water within a water-perfused suit (T wps) they were wearing. A control unit established a sinusoidal change in T wps, such that it varied from 27 to 42°C. The subjects could alter the direction of the change of T wps, when they perceived it as thermally uncomfortable. The magnitude of the oscillations towards the end of the trial was assumed to represent the upper and lower boundaries of the thermal comfort zone. The cutaneous threshold for detecting cold stimulus decreased (P < 0.05) from 1.6 (1.0)°C on day 1 to 1.0 (0.3)°C on day 22. No effect was observed on the ability to detect warm stimuli or on the regulated T wps. We conclude that although cold sensitivity increased after bed rest, it was not of sufficient magnitude to cause any alteration in behavioural thermoregulatory responses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies on human thermoregulation conducted under conditions of musculoskeletal and cardiovascular deconditioning such as microgravity or prolonged experimental bed rest indicate that, although maintenance of normothermia is not jeopardised, the core temperature is elevated and some thermoregulatory responses are attenuated.
The most prominent changes were discovered in the autonomic thermoregulatory component, particularly during recovery from exercise. Exercise-induced heat loss (sweating and vasodilatation) and heat production responses (shivering) were shown to be modified after bed rest (Fortney et al. 1996, 1998; Greenleaf 1989; Mekjavic et al. 2005; Pavy-Le Traon et al. 2007). Changes in the efficiency and/or sensitivity of these autonomic responses were suggested to contribute to the elevation in core temperature observed during spaceflights (Rimmer et al. 1999) and in bed rest experiments (Ertl et al. 2000; Fortney et al. 1998; Greenleaf 1997).
However, in addition to autonomic control of body temperature, maintaining normothermia involves also behavioural thermoregulatory responses. Under normal conditions, the temperature of the body is not constant. Rather, a dynamic core-to-skin thermal gradient exists according to the shifts in body temperature at different times of the day, level of activity, etc. Small shifts in core temperature are counteracted initially by changes in peripheral vasomotor tone and behavioural responses; if core temperature is shifted further, then activation of the metabolically more demanding autonomic responses, shivering or sweating, ensues.
Behavioural responses modulate heat flow from the body by adjusting insulation and the effective surface area for heat exchange. In fact, where regulation of ambient temperature is possible, by actively adjusting an environmental control system (i.e. heating and cooling), the action of maintaining a preferred ambient temperature is probably the most efficient means of maintaining thermal balance and in preventing any deleterious displacements of core temperature.
Such thermoregulatory behaviour depends on the normal functioning of the thermal sensory apparatus (thermal information from peripheral and core thermosensors) and is motivated by the perception of thermal discomfort or rather an affective judgement of the thermal environment (Cabanac 1971, 1981; Hensel 1976; Weiss and Laties 1961). Thus, if deconditioning induced by microgravity or bed rest impairs thermal sensation, or the perception of thermal (dis)comfort, initiation of appropriate behavioural responses might be modified. Inappropriate behavioural regulation of body temperature may contribute, at least in part, to the observed thermal imbalance during prolonged bed rest or microgravity. Changes in thermal comfort and thermal sensation have been reported in previous studies during hypokinesia (Panferova 1976, 1989) and experimental bed rest (Fortney et al. 1996; Greenleaf 1989; Mekjavic et al. 2005). However, the effects of bed rest on behavioural thermoregulatory responses have not yet been investigated.
The present study tested the hypothesis that prolonged bed rest alters behavioural thermoregulation in humans. We also evaluated the effects of prolonged bed rest on cutaneous thermal sensitivity, to determine whether changes, if any, in the preferred thermal comfort zone (TCZ) are a consequence of an alteration in cutaneous temperature sensitivity.
Methods
Ten healthy male subjects volunteered for the study. Their average (SD) physical characteristics were: age = 22.2 (3.9) years, height = 182.2 (6.2) cm and mass = 80.3 (11.2) kg.
Protocol
This study was part of a larger study investigating the effects of 35 days of horizontal bed rest on muscle atrophy and osteoporosis. The protocol of the study was approved by the National Ethics Committee of the Republic of Slovenia and conformed with the Declaration of Helsinki. Subjects were accommodated in a ward of the Orthopaedic Hospital Valdoltra (Ankaran, Slovenia). During the bed rest period, subjects were under 24-h health care. Throughout the entire period of bed rest, they were requested to remain in the horizontal position at all times and not to perform any exercises (i.e. undue isometric contractions). All activities were performed in the horizontal position. Subjects could support themselves on their elbows during eating, personal hygiene and transfer between bed and gurney. Subjects received regular physiotherapy, comprising passive movements of all joints and light massage of the neck and lower back regions. Active muscle contractions were avoided. Subjects received physiotherapy also on request.
Cutaneous thermal sensitivity assessment
Minimum detectable temperature (MDT) was assessed on the 1st and 22nd day of bed rest. Testing was conducted in a temperature-controlled room at the same time of the day. Subjects were allowed to equilibrate to the conditions of the room (ambient temperature was 25°C) for 30 min. Following equilibration, two cutaneous temperature (cold and warm) sensitivity tests were performed in random order, to assess the influence of bed rest on MDT. The protocol used for assessing cutaneous thermal sensitivity with a Middlesex Thermal Testing System (Howe Institute, Canvey Island, Essex, UK) has been reported previously (Golja et al. 2004). Briefly, a controlling unit initiated the thermal stimuli, which was presented to the cutaneous region via a thermode (a Peltier element) with a surface area of 24 cm2. The rate of temperature change during heating and cooling of the thermode was 1°C s−1. The thermode was positioned on the volar side of the right forearm between the elbow and the wrist. A thermocouple attached to the copper surface of the thermode determined the magnitude and duration of the stimulus and ensured that the adaptive temperature of the skin (temperature of the skin below the thermode prior to initiation of thermal stimuli) was similar in all trials.
The stimuli were presented to the skin immediately after an audible tone was generated by the computer. Each trial commenced with three stimuli of maximal intensity (either an increase or decrease in temperature of 3°C from the adaptive skin temperature) to familiarise the subjects with the procedure. Subjects were required to detect at least one familiarisation stimulus. Subjects who failed to detect the familiarisation stimuli three times (total of nine stimuli) were excluded from further analysis. Once the trial was initiated, subjects were requested to confirm whether they perceived the stimulus or not. If a stimulus was perceived, the next stimulus was smaller; if the stimulus was not perceived, the next stimulus was greater. Intermittently, the software also initiated a sham stimulus; no thermal stimulus was generated following the audible tone. We considered the ratio of false-positive reports (i.e. number of positive reports to sham stimuli/total number of reports) as a measure of the reliability of the subjects’ assessments.
Behavioural thermoregulation assessment
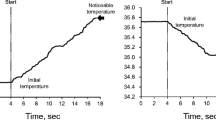
Behavioural thermoregulatory function was assessed after the conclusion of cutaneous thermal sensitivity tests. Subjects remained supine whilst thermocouples were attached to their skin and a water-perfused suit (WPS) donned on them. The WPS was made of five components covering the entire surface of the body with the exception of the hands, feet, neck and face. All five components were fed from a common manifold and consisted of identical length of small-diameter (inner = 4 mm, outer = 5 mm) PVC tubing, which was woven in intervals of 1 cm in the meshed lining of the suit. Velcro strips embedded in the suit ensured a good fit to the surface of the skin. Once fully instrumented, the temperature of the water perfusing the WPS (T wps) was set at 27°C, which was perceived by the subjects as being cool. Thereafter, their behaviour in maintaining thermal comfort was evaluated. The T wps varied in a sinusoidal manner from 27 to 42°C. The rate of change of the water temperature was 2.1°C min−1 and each warming and cooling phase lasted approximately 15 min. Subjects were instructed that by depressing a button on a manual control, they could initiate a change in the direction of the T wps once it became either uncomfortably warm during heating or uncomfortably cool during cooling. Subjects were requested to maintain T wps within a preferred range for a total duration of 1 h. We did not coach the subjects or give them any further instructions during the trials. The resultant magnitude of the sinusoidal T wps pattern defined as the regulated TCZ and its lower (T low) and upper (T high) temperature boundaries were compared between days 1 and 22 of bed rest.
Subjects were unaware of the actual temperature of the water perfusing into the suit during the trial. The effects of circadian rhythm were minimised by testing the subjects at the same time of the day.
Ambient conditions
The conditions in the experimental room were monitored by a portable weather station (BAR 938 HG OS, Huger, Germany). The ambient room temperatures were 25–26°C in all testing days and the relative humidity 40–50%.
Skin temperature
Skin temperature (T sk) was measured with T-type (copper-constantan) thermocouples attached to six sites covered by the WPS (calf, thigh, abdomen, chest, forearm and arm) and two sites that were not covered (foot and hand). The distance between the tubes in the WPS was approximately 1 cm, which ensured a uniform stimulation of the skin areas covered by the suit. The thermocouples were attached to the skin at the right side of the body using a thin, breathable transparent film dressing (3 M™, Tegaderm™). Skin temperatures were continuously recorded with a data logger (Almemo 5990-2, Ahlborn, Holzkirchen, Germany). The proximal-to-distal skin temperature gradient was measured in the hand as the difference between T sk at the forearm and the second digit (ΔT forearm-fingertip), and in the foot as the difference between T sk at the calf and toe (ΔT calf-toe). These values were assumed to reflect peripheral blood flow (Rubinstein and Sessler 1990).
Core temperature
The core temperature (T c) was estimated from measurements of tympanic temperature using an infrared thermometer (ThermoScan IRT 3020, Braun, Kronberg, Germany). Three consecutive measurements of T c were performed before and immediately after each trial, and the highest value was considered representative of the core temperature. We did not continuously measure T c during the trial, since we did not expect it to change whilst the subjects were at the vicinity of their TCZ. We previously showed that the tympanic temperature remains unchanged during automatic oscillations of the T wps in the range 27–42°C, and that the preferred T wps for thermal comfort is within this range (Yogev and Mekjavic 2007). Thus, in the current experimental design, changes in T sk, rather than in T c, were the driving force for the behavioural responses involved in maintaining the WPS thermally comfortable.
Data analysis
A paired t test was used to compare differences in ambient room temperature and relative humidity between days 1 and 22 of bed rest. Measurements were taken during the first 10 min (equilibration time) before testing. Mean T sk was calculated as the unweighted mean of the T sk at eight sites (forearm, arm, abdomen, chest, neck, forehead, back, thigh, calf, foot, finger and toe) measured at the right side of the body. A paired t test was used to compare the T wps, T sk, ΔT forearm-fingertip and ΔT calf-toe as measured on the 1st and the 22nd day of bed rest. Data are expressed as means (SD) and the limit of statistical significance was set at 0.05.
Assessment of cutaneous thermal sensitivity
The MDT was calculated as the smallest of the last five positive responses. A paired t test was used to compare differences in the cutaneous thresholds for detecting warm and cold stimuli between days 1 and 22 of bed rest.
Assessment of behavioural thermoregulation
The lower and upper peaks of the oscillation pattern obtained during the last 30 min of each trial were considered to represent the boundaries of the subject’s TCZ (T low and T high, respectively). Pre- and post-BR values were averaged and compared using a paired t test. Changes in the accuracy of the behavioural response (i.e. in the ability to behaviourally maintain thermal comfort) were estimated by calculating the coefficient of variation (%) within the series of T high and T low made by the subject during each half of the 60-min trial.
Results
Effects of bed rest on cutaneous thermal sensitivity
Familiarisation trial
All the subjects (n = 10) could detect the initial 3°C decrease in their adaptive T sk during familiarisation. The warm stimuli, however, were harder to detect and most subjects (seven on day 1 and five on day 22) required more than one familiarisation trial until a 3°C increase in their adaptive T sk was detected.
Adaptive temperature
Testing of cutaneous thermal sensitivity was initiated at similar adaptive T sk before and after bed rest. Due to the familiarisation pre-trial, warm testing was initiated at a slightly higher adaptive T sk compared to cold testing. During the warm trials, the adaptive T sk was 32.9 (0.7)°C on day 1 and 32.1 (1.6)°C on day 22 and, during the cold trials, it was 31.6 (0.7)°C on day 1 and 30.7 (1.4)°C on day 22.
Cutaneous thermal sensitivity
The 21 days of horizontal bed rest resulted in an increase in cold sensitivity. The MDT during cold stimuli significantly decreased (P < 0.05, power = 0.71) from 1.6 (1.0)°C on day 1 to 1.0 (0.3)°C on day 22. In contrast, the sensitivity to warmth tended to decrease, albeit not significantly, after bed rest; three subjects were unable to detect any of the warm stimuli after bed rest (compared to one subject before bed rest), and the MDT amongst the rest of the subjects did not significantly change after bed rest (P > 0.05, power = 0.20). It was 1.3 (0.5)°C on day 1 and 1.6 (0.9)°C on day 22. Individual differences in the MDT during warming and cooling are presented in Fig. 1.
Reliability
The percentage of false-positive reports was not evenly distributed among the subjects. As demonstrated in Fig. 2, two subjects (S6, S7) had a particularly low reliability score (over 50% false-positive reports). If the results from these subjects are not considered in the analysis of MDT (n = 8), a more homogeneous effect can be observed. Seven subjects experienced a decrease in warmth sensitivity (i.e. increase in MDT/unable to detect stimuli) and six subjects experienced an increase in cold sensitivity (i.e. decrease in MDT) after bed rest.
Effects of bed rest on behavioural thermoregulation
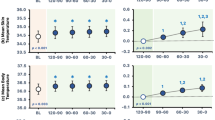
The comfort regulation trials on day 1 and 22 were conducted with minimal experimenter supervision and/or feedback. The subjects received a thorough explanation on the purpose of the trial before it started; however, they were not coached or given any further instructions during the trial. Consequently, three subjects completed the trials without regulating T wps during the entire duration of the trial. The boundaries and width of the TCZ could not be determined for these subjects. The remaining subjects were able to appropriately regulate T wps (Fig. 3) to attain a comfortable level of T sk (Fig. 4).
Characteristics of comfort regulation behaviour
Subjects (n = 7) used different approaches to regulate thermal comfort. Some preferred to regulate T wps within a narrow range (Fig. 5a), whilst others allowed the T wps to fluctuate within a wider range (Fig. 5b). Nevertheless, 21 days of horizontal bed rest did not significantly alter the manner in which subjects controlled the T wps to maintain thermal comfort during a 60-min trial (Figs. 3, 4). A typical learning curve was noted in the T wps pattern with larger oscillations in the first half of the trial followed by smaller oscillations in the second. The mean (SD) frequency of oscillation was similar before and after bed rest. Subjects inverted the direction of the T wps change 21 (9.2) times on day 1 and 24.9 (11.5) times on day 22. The coefficient of variation of T high and T low chosen during the last half of the trial was lower (1.7%) than that observed in the first half (3.5%), indicating a greater accuracy in controlling the temperature towards the end of the trials. Similar accuracy in T wps control was observed after 22 days of bed rest.
Characteristics of the thermal comfort zone
As shown in Tables 1 and 2, the mean (SD) T wps, T high and T low were not significantly different after 22 days of bed rest as compared to the first day. Nevertheless the decrease in the width of the TCZ after bed rest was significant (P < 0.05).
Effects of bed rest on skin and core temperatures
The core temperature of the subjects was slightly increased (P < 0.05) from 36.7 (0.1)°C on day 1 to 37.0 (0.2)°C on day 22. However, after the trial ended, it was not significantly different anymore. Mean skin temperature (T sk) was slightly higher (P < 0.05) after bed rest. It increased from 32.1 (0.7)°C on day 1 to 32.9 (0.9)°C on day 22. In contrast to previous reports (Golja et al. 2002), in the current study, the skin temperature measured at the extremities (the toe and the third digit of the hand) was not significantly different between the 1st and 22nd day of BR. Accordingly, the differences in skin temperature between the forearm and fingertip (ΔT forearm-Fingertip) and between the calf and toe (ΔT calf-toe), indices of blood flow in the extremities, were not significantly different between days 1 and 22.
Discussion
The main finding of the present study is that following 3 weeks of horizontal bed rest, there were no significant changes in thermal comfort or its behavioural control despite small changes in cutaneous temperature sensitivity.
Effects of bed rest on thermoregulation
Previous studies have reported that the physiological adaptation following prolonged periods of inactivity attenuates thermoregulatory responses (Fortney et al. 1998; Greenleaf 1989). Changes in the sensitivity (gain) and threshold of activation of autonomic heat loss and heat gain responses have been suggested as possible mechanisms for these observations. In addition, since activation of behavioural thermoregulatory responses relies on similar thermal afferent neural information as autonomic thermoregulatory responses, it was hypothesised that behavioural responses might also be affected in such conditions.
Mekjavic et al. (2005) reported that subjects perceived similar combinations of skin and the core temperatures as warmer and thermally less uncomfortable after 35 days of horizontal bed rest. Reports from earlier studies indicate that some changes in thermal sensitivity occur (Fortney et al. 1996; Panferova 1976) and that subjects in bed rest studies often complain of cold feet (Fortney et al. 1996; Mekjavic et al. 2005; Taylor et al. 1949). Using weekly infrared thermograms during a 35-day bed rest, Golja et al. (2002) showed a significant decrease in skin temperature at the feet and concluded that cold sensation was due to an actual cooling of extremities rather than alteration in thermal sensory function. In the current study, after a 21-day bed rest, the mean T sk and the core temperature were slightly increased; however, there were no significant changes in extremity T sk. The results from the current study are in agreement with the studies demonstrating that changes in peripheral thermal sensitivity might occur after bed rest (Fortney et al. 1996, 1998; Panferova 1976). In the current study, the changes in cold sensitivity were not due to actual cooling, since the adaptive skin temperature was not significantly different after bed rest and the mean T sk tended to increase. Furthermore, increased sensitivity to cold can also explain why bed rest did not increase, but rather tended to decrease the regulated TCZ. These changes in local thermal sensitivity appear to be too small to significantly affect the preferred temperature or its behavioural regulation.
It therefore seems unlikely that the increase in core temperature observed after bed rest and spaceflights is the result of an inability to activate behavioural thermoregulatory responses near thermal neutrality. This is in agreement with previous bed rest studies where core temperature only occasionally increased in resting subjects (Greenleaf 1997). More consistent are reports of a bed rest-induced “excessive” increase in core temperature during exercise (Golja et al. 2002; Greenleaf 1989, 1997; Mekjavic et al. 2005), or greater decrements in core temperature during immersion in water at 28°C (Mekjavic et al. 2005). The former may be attributed to attenuation of the sweating and/or vasodilatatory responses consequent to a reduced circulating blood volume (Crandall et al. 2003; Wilson et al. 2003), and the latter to attenuation of shivering and/or cold-induced vasoconstriction.
In the present study, there was no change in T c after 60 min of comfort regulation. Furthermore, we have previously demonstrated that oscillations in T wps in the range of 27–42°C lead to fluctuations of 3–4°C in mean T sk, without significantly changing the tympanic temperature (Yogev and Mekjavic 2007). As previously, regulation of the T wps in the current study was limited to the same range. We therefore assumed that the core temperature was unaltered during the entire duration of the trials. Therefore, any change in thermal perception or thermal sensitivity could not reflect changes in the function of either the sweating or the shivering responses.
As there were no significant differences in any of the variables related to vasomotor tone (skin temperature at the extremities, ΔT forearm-finger and ΔT calf-toe), the observed changes in our study most likely resulted from changes in the perception of thermal stimuli. The latter incorporates not only the transduction of thermal energy into neural coded information, but also the central integration of thermal afferent information from the core and the skin that results in a subjective perception of thermal (dis)comfort.
The effects of bed rest on cutaneous thermal sensitivity
An important factor affecting thermal sensitivity is the adaptive temperature of the skin: the steady-state temperature of the skin prior to the application of a thermal stimulus. Alteration in skin blood flow can alter this temperature and consequently affect cutaneous thermosensitivity. Previous bed rest studies show that the naturally occurring central-to-peripheral thermal gradient that enables heat flow from the core to the periphery is altered after lying down (Golja et al. 2002). Such alteration in the thermal gradient may be attributed to redistribution of blood from the peripheral to central regions caused by increased peripheral vasoconstriction (Convertino 2002).
The adaptive temperature in the cutaneous sensitivity tests was not significantly different after bed rest; however, the mean T sk was about 1°C lower on day 1 compared to day 22. Such a change in the skin temperature may have contributed to reduction of the warm- and exaggerated cold sensitivity, since it approaches the temperature corresponding to the maximum activity of the cold thermal sensors (Kenshalo 1976). Thus, we cannot exclude the possibility that the observed increase in cold sensitivity and reduced warm sensitivity were influenced by a small bed rest-induced change in skin temperature.
The effect of bed rest on behavioural regulation of thermal comfort
It was previously reported that thermal perception changes after bed rest (Mekjavic et al. 2005). Since thermal perception is the basis for behavioural thermoregulation, it was suggested that these changes might lead to inappropriate behavioural thermoregulatory responses. Assuming that similar changes would occur in microgravity, this might be of practical importance to astronauts during space exploration missions. Namely, during extravehicular activity (EVA), the liquid cooling garment (LCG) worn next to the skin, and designed to maintain a thermoneutral microenvironment, is controlled manually. In this study, rather than asking the subjects to passively evaluate the degree of thermal (dis)comfort using a rating scale (a non-parametric variable), we assessed the manner by which they actively regulate the temperature of the WPS according to their comfort. We have previously shown that the T wps at which a discomfort perception appears and the T wps at which subjects initiate a behavioural response to counteract it, are highly correlated (Yogev and Mekjavic 2007).
The facts that no significant differences were observed in the preferred skin temperature, the upper and lower boundaries of the TCZ and in the characteristics of the control of T wps suggest that the changes that occur after 3 weeks of bed rest do not significantly attenuate the ability to behaviourally maintain thermal comfort in the WPS.
A limitation to the current study is that we did not estimate the contribution of local discomfort. Thus, we cannot determine the relative contribution of certain skin regions to the resultant thermoregulatory behaviour. Previous studies have demonstrated that different skin regions do not equally contribute to thermal sensation and comfort (Burke and Mekjavic 1991; Cotter and Taylor 2005; Zhang et al. 2004). It would be interesting to examine how subjects, given control over their skin temperature, would regulate the different regions of the skin to maintain an overall thermal comfort.
Our results are in line with previous observations indicating that prolonged inactivity may lead to changes in thermal sensation (Mekjavic et al. 2005), and suggest that it is primarily the peripheral sensation of cold. Future studies on thermal sensitivity after bed rest will have to eliminate any change in adaptive temperature of the skin, a consequence of the bed rest-induced increase in peripheral vasoconstriction. The ability to behaviourally maintain thermal comfort was not compromised under the prevailing, relatively mild conditions of this study (vicinity of thermal neutrality, rest, no additional tasks). However, the results of this study indicate that small changes in thermal perception after bed rest may occur not only as a result of alteration in core temperature (induced by exercise or immersion in cold water), but also at rest, within the boundaries of TCZ. Although these changes seem to be too small to result in significant changes in the behavioural thermoregulatory response, it would be premature to dismiss the role of behavioural thermoregulatory responses when thermal balance in actual microgravity is considered. In such conditions, an astronaut might have to perform accurate tasks after strenuous activity over long periods. Even a small shift from thermal comfort might increase the metabolic demand and exhaust an astronaut, thus jeopardising his safety. Future studies will have to widen the scope of conditions under which behavioural thermoregulation is examined.
References
Burke WE, Mekjavic IB (1991) Estimation of regional cutaneous cold sensitivity by analysis of the gasping response. J Appl Physiol 71:1933–1940
Cabanac M (1971) Physiological role of pleasure. Science 173:1103–1107
Cabanac M (1981) Physiological signals for thermal comfort. In: Cena K, Clark J (eds) Bioengineering, thermal physiology, and comfort. Elsevier, Amsterdam, pp 181–192
Convertino VA (2002) Mechanisms of microgravity-induced orthostatic intolerance: implications for effective countermeasures. J Gravit Physiol 9:1–13
Cotter JD, Taylor NA (2005) The distribution of cutaneous sudomotor and alliesthesial thermosensitivity in mildly heat-stressed humans: an open-loop approach. J Physiol 565:335–345
Crandall CG, Shibasaki M, Wilson TE, Cui J, Levine BD (2003) Prolonged head-down tilt exposure reduces maximal cutaneous vasodilator and sweating capacity in humans. J Appl Physiol 94:2330–2336
Ertl AC, Dearborn AS, Weidhofer AR, Bernauer EM, Greenleaf JE (2000) Exercise thermoregulation in men after 1 and 24 hours of 6 degrees head-down tilt. Aviat Space Environ Med 71:150–155
Fortney SM, Schneider VS, Greenleaf JE (1996) The physiology of bed rest. In: Fregly MJ, Blatteis CM (eds) Handbook of physiology. Oxford University Press, Oxford, pp 889–939
Fortney SM, Mikhaylov V, Lee SM, Kobzev Y, Gonzalez RR, Greenleaf JE (1998) Body temperature and thermoregulation during submaximal exercise after 115-day spaceflight. Aviat Space Environ Med 69:137–141
Golja P, Eiken O, Rodman S, Sirok B, Mekjavic IB (2002) Core temperature circadian rhythm during 35 days of horizontal bed rest. J Gravit Physiol 9:P187–P188
Golja P, Kacin A, Tipton MJ, Eiken O, Mekjavic IB (2004) Hypoxia increases the cutaneous threshold for the sensation of cold. Eur J Appl Physiol 92:62–68
Greenleaf JE (1989) Energy and thermal regulation during bed rest and spaceflight. J Appl Physiol 67:507–516
Greenleaf JE (1997) Exercise thermoregulation with bed rest, confinement, and immersion deconditioning. Ann N Y Acad Sci 813:741–750
Hensel H (1976) Correlations of neural activity and thermal sensation in man. In: Zotterman Y (ed) Sensory functions of the skin in primates with special reference to man. Pergamon Press, Oxford, pp 331–353
Kenshalo DR (1976) Correlation of temperature sensitivity in man and monkey, a first approximation. In: Zotterman Y (ed) Sensory functions of the skin in primates with special reference to man. Pergamon Press, Oxford, pp 205–330
Mekjavic IB, Golja P, Tipton MJ, Eiken O (2005) Human thermoregulatory function during exercise and immersion after 35 days of horizontal bed rest and recovery. Eur J Appl Physiol 95:163–171
Panferova NE (1976) Cardiovascular system during hypokinesia of varying duration and intensity. Kosm Biol Aviakosm Med 10:15–20
Panferova NE, Anisimova IV, Pavlova LS, Poliakov VM (1989) Measurement of the temperature of deep-seated tissues in healthy men during hypokinesia. Kosm Biol Aviakosm Med 23:42–46
Pavy-Le Traon A, Heer M, Narici MV, Rittweger J, Vernikos J (2007) From space to Earth: advances in human physiology from 20 years of bed rest studies (1986–2006). Eur J Appl Physiol 101:143–194
Rimmer DW, Dijk D-J, Ronda JM, Hoyt R, Pawelczyk JA (1999) Efficacy of liquid cooling garments to minimize heat strain during space shuttle deorbit and landing. Med Sci Sports Exerc 31:S305
Rubinstein EH, Sessler DI (1990) Skin-surface temperature gradients correlate with fingertip blood flow in humans. Anesthesiology 73:541–545
Taylor HL, Henschel A, Brozek J, Keys A (1949) Effects of bed rest on cardiovascular function and work performance. J Appl Physiol Behav 2:223–229
Weiss B, Laties VG (1961) Behavioral thermoregulation. Science 133:1338–1344
Wilson TE, Shibasaki M, Cui J, Levine BD, Crandall CG (2003) Effects of 14 days of head-down tilt bed rest on cutaneous vasoconstrictor responses in humans. J Appl Physiol 94:2113–2118
Yogev D, Mekjavic IB (2007) A new method for evaluation of behavioural thermoregulation in humans. In: Mekjavic IB, Kounalakis SN, Taylor NAS (eds) Proceedings of the 12th international conference on environmental ergonomics (ICEE XII), Piran, Slovenia. Biomed, Ljubljana pp 359–360
Zhang H, Huizenga C, Arens E, Wang D (2004) Thermal sensation and comfort in transient non-uniform thermal environments. Eur J Appl Physiol 92:728–733
Acknowledgments
This work was supported, in part, by a Knowledge for Security and Peace Grant to I.B.M. from the Ministry of Defence (Republic of Slovenia), the Italian Space Agency (Osteoporosis and Muscle Atrophy, OSMA Project) and the Regione Firuli Venezia Giulia (LR11).
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by George Havenith, Susan A. Ward.
Rights and permissions
About this article
Cite this article
Yogev, D., Eiken, O., Pisot, R. et al. Effect of 21 days of horizontal bed rest on behavioural thermoregulation. Eur J Appl Physiol 108, 281–288 (2010). https://doi.org/10.1007/s00421-009-1202-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-009-1202-7