Abstract
This study examined whether a training intervention likely to elicit adaptations in the leg could result in reduced leg pain and increased whole body physical capacity. Twenty-seven peripheral arterial disease (PAD) patients were randomized to either an individual leg plantar flexion training group (TG) training 4 × 4 min intervals at 80% of maximal work rate three times per week for 8 weeks or a control group. The TG significantly increased plantar flexion peak oxygen uptake and power output by 23.5 and 43.9%, respectively. Treadmill peak oxygen uptake (VO2peak) significantly increased 12.3% in the TG and was associated with a significant increased time to exhaustion of 20.0% when treadmill walking. Eleven of 14 patients no longer reported leg pain limitations at VO2peak. No differences in cardiac output measured at VO2peak, or walking economy were observed. Plantar flexion training was effective in increasing VO2peak and walking performance, and may be a useful strategy in treatment of PAD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is an increasing acceptance for the benefits of exercise training as a treatment for peripheral arterial disease (PAD). The effects are observed as increases in physical and functional capacity as well as a decrease in claudication, the primary symptom of the disease (Stewart et al. 2002), contributing to an improved quality of life. However the composition and intensity of the exercise training that gives the best improvement needs further research.
Treadmill walking is most commonly used as a training intervention and is documented to be the most effective type of exercise (Stewart et al. 2002). Physical capacity is most often measured as walking distance. A meta-analysis (Gardner and Poehlman 1995) showed that maximal walking time in a continuous walking protocol on average improved by 120% after a training intervention. A few studies have also included peak oxygen consumption (VO2peak) as a more accurate measure of physical capacity (Hiatt et al. 1990; Slordahl et al. 2005).
The importance of improving VO2peak is well documented. It is shown to be the single most powerful predictor of cardiac and all-cause mortality among patients with cardiovascular disease (Mayers et al. 2002). Although PAD affects the lower extremities, the disease is an expression of systemic atherosclerosis and vascular disease throughout the body (Weitz et al. 1996), and the importance of improving VO2peak is essential.
The intensity of the exercise training in PAD has been a topic of little investigation. However, in a randomized study by Slordahl et al. (2005), a training intensity corresponding to 80% of VO2peak was found to be superior to a moderate training intensity at 60% of VO2peak in improving both VO2peak and walking time to exhaustion. Moderate training intensity is however still the recommended intensity given to PAD patients (Hirsch et al. 2006).
The obstruction of blood flow in the patients’ lower extremities due to atherosclerosis is clearly a supply limitation in terms of Wagner’s (2000) approach to detecting flow limitations. The training responses have however not been linked to increased blood flow, but to peripheral changes in arterio-venous oxygen difference and mainly linked to mitochondrial adaptations (Bauer et al. 2004; Stewart et al. 2002), a response in demand for oxygen. It thus seems that the PAD patients have developed a demand limitation for oxygen utilization that is more pronounced than the supply limitation causing the PAD, most probably due to inactivity. With this background it could be questioned if exercise training using whole body is the optimal intervention?
In PAD patients pulmonary oxygen kinetics were found to be slower in the lower extremities compared to upper extremities (Bauer et al. 2004). This was not due to resting cardiac and pulmonary function. In a study using six healthy subjects Klausen et al. (1982) found that a larger portion of blood flow was directed to the working muscles when exercising with one leg isolated. Also when compared to whole body exercise, one leg knee extension confirms much higher mitochondrial oxygen consumption (Richardson et al. 1999). According to Shephard et al. (1988) the main factor limiting small muscle work (i.e. the calf muscle) is the steady power output that can be developed by the active muscle fibers, rather than oxygen delivery. These studies may indicate a larger adaptation to training in the leg when exercising with a reduced muscle mass. In the study by Shephard et al. (1988) it can also be argued for using a high intensity when training a small muscle mass since power output regulates small muscle work.
In the present study it was hypothesized that individual leg plantar flexion high aerobic intensity interval training will enhance walking performance, but without changing the oxygen supply measured as cardiac output or stroke volume of the heart.
Methods
Patients
Twenty-seven subjects diagnosed with PAD were recruited among patients from the department of vascular surgery at St. Olavs hospital, Trondheim, Norway and from general practitioners. Inclusion criteria were unilateral or bilateral ankle-brachial index (ABI) ≤0.9 and functional limitations from intermittent claudication. None of the patients had undergone a revascularization operation the last 6 months. Subjects were excluded from the study if exercise tolerance was limited by other factors than claudication and if the exercise pain was not of vascular origin. Patients were also excluded if they were unable to perform the treadmill test procedures. Patients were instructed not to change medications or other received treatment during the period of exercise intervention. Subjects were randomly assigned to an individual leg plantar flexion interval training group (TG) or control group (CG) (Table 1). The CG received advices in accordance with existing exercise guidelines from American Heart Association for PAD patients (Hirsch et al. 2006). Two subjects in the CG withdrew from the study due to personal reasons. The study was performed according to the Helsinki declaration and was approved by the regional medical research ethics committee. Written informed consent was obtained from all patients.
Treadmill testing
After a 10-min warm up period, VO2peak was measured (Metamax II, Cortex, Leipzig, Germany) using a graded treadmill protocol (Hiatt et al. 1990). The treadmill velocity was held constant at 3.2 km h−1, and inclination starting at 0% and increased by 3.5% steps every 3 min until patients were stopped by claudication pain. VO2peak was measured as the mean of the highest 30-s interval as was expiratory exchange ratio and ventilation. Peak heart rate (HRpeak) was measured using a heart rate monitor (Polar Electro, Kempele, Finland). Blood samples were drawn from fingertip for measurement of lactate in blood ([La−]b) using a YSI 1500 Sport Lactate Analyzer (Yellow Springs Instrument Co, Yellow Springs, Ohio, USA) within 1 min after the test. Work economy was determined using oxygen uptake at a standard submaximal workload of 0% inclination at 3.2 km h−1.
Plantar flexion ergometer
Patients performed an exercise test using a plantar flexion ergometer previously used by Haseler et al. (2007). Subjects were placed in a supine position with approximately a 45º angle of flexion between hip and columna and their lower extremities both fully extended. The foot with the lowest ABI was placed in a footplate connected to an electrical adjustable bicycle (Monark 839E, Varberg, Sweden) with a 6 foot metal rod (Fig. 1). Patients performed plantar flexion training working against the footplate, and the bicycle offered adjustments in steps of 1 W. The bicycle flywheel provided constant resistance and returned the pedal to the proper position between plantar flexion pushes. Range of motion was controlled by a fixed distance that the footplate could be moved during flexion and by the distance the metal rod could move during relaxation. Range of motion was 10 cm with the starting position perpendicular to horizontal (Haseler et al. 2007). Patients were given one training session to familiarize with the ergometer before the test. In addition to power, time to exhaustion and pulmonary oxygen consumption were measured continuously during the test protocol. Oxygen consumption was measured with the same method as for the treadmill test. A pilot study was performed prior to the present study to measure coefficients of variation (CoV) for time to exhaustion and pulmonary VO2peak in the plantar flexion ergometer. Ten moderate trained subjects participated in the study (age 27 ± 4.3 years). Each subject were given one familiarization session using the ergometer before the test and retest performed on separate days with a day of rest in between. The method error (ME) and CoV for VO2peak and time to exhaustion were ME = 0.08 l min−1; CoV = 9.0% and 28.5 s; CoV = 5.7% respectively. Bland & Altman plots showed good agreement in the data, and the pilot study showed no significant differences (P < 0.05) in test–retest measurements. Frequency was held constant at 1 Hz, displayed by a monitor. Resistance started at 0 W and was increased by steps of 1 W every minute until exhaustion. As for the treadmill test the VO2peak was measured as the mean of the highest 30-s interval.
Stroke volume
Cardiac output (Q) and stroke volume (SV) were measured using a Sensormedics Vmax Spectra 229 (Sensormedics, Pennsylvania, USA). The test was performed at the workload representing the subjects VO2peak. The single breath acetylene uptake (SB) procedure started with complete expiration followed by complete inspiration of a gas mixture containing 0.3% carbon monoxide (CO), 0.3% metane (CH4), 0.3% acetylene (C2H2), 21% oxygen (O2), balanced with nitrogen (N2). The inspiration was followed by a continuous complete expiration. Before the test started multiple training bouts were carried out to familiarize subjects to the technique. The SB technique has been validated with the indirect Fick CO2-rebreathing method and compared with open circuit acetylene uptake (Dibski et al. 2005). Both techniques were valid and reliable for measures of Q and SV. CoV was 7.6% at an intensity of 200 W. The test procedure was however concluded to be more difficult to perform at the highest exercise intensities. Although not directly measured, maximal arteriovenous oxygen differences [C(a-v)O2] were calculated from the equation VO2peak = CO × [C(a-v)O2].
Training procedure
The TG received supervised training 3 times a week for 8 weeks. The training was carried out in a laboratory setting. The TG used the same plantar flexion ergometer described in the testing procedure for training (Fig. 1). One training session consisted of 4-min work periods for the individual leg, and 4 intervals were executed on each leg. One leg rested while the other performed work. One session lasted for approximately 40 min involving about 2 min for the changeover from one leg to the other. Initial work load was set at 80% of maximum work rate (Haseler et al. 2007). As work capacity increased the resistance toward movement was increased, by increments of 1 W, to maintain the work intensity.
Allometric scaling
PAD patients are not a homogenous group in terms of bodyweight (56.4–117.1 kg) and comparison of VO2peak between patients with different bodyweight is imprecise when made in absolute terms (l min−1) or relative to bodyweight (ml min−1 kg−1). Allometric scaling raising the bodyweight’s power to 0.75 (ml min−1 kg−0.75) (Bergh et al. 1991; Helgerud 1994) was therefore included in the present study.
Statistical analysis
Data are reported as mean ± SD, with significance level P < 0.05 unless otherwise stated. A T-test was used to compare differences between groups. A paired T-test was used to compare pre- and post test values within groups.
Results
No differences were apparent between TG and CG at baseline. The patients in the TG completed all planned training sessions.
Plantar flexion capacity
After performing plantar flexion interval training during 24 sessions, the TG improved their plantar flexion VO2peak by 23.5% (P < 0.001, Fig. 2) and power output by 43.9% (P = 0.003), as well as time to exhaustion by 41.6% (P = 0.003). All improvements were significantly different from the CG (P < 0.001; P = 0.02; P = 0.02, Table 2).
Plantar flexion test. Changes in peak oxygen consumption (l min−1) and time to exhaustion (s) from pre-test to post-test (CG Control group; TG Plantar flexion training group). Data are presented as mean percentage change and standard error. Significantly different within group from pre- to post-test: * P < 0.05, significantly different between groups from pre- to post-test: § P < 0.01
Treadmill exercise capacity
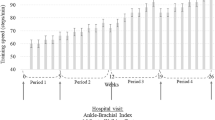
After 8 weeks, VO2peak increased by 12.3% (P = 0.002, Fig. 3) in the TG, whereas the CG remained unchanged. The increase in absolute values was supported by a corresponding increase in relation to bodyweight (P = 0.01) as well as in scaled bodyweight (P = 0.008).
Treadmill test. Changes in peak oxygen consumption (l min−1) and absolute stroke volume of the heart (ml beat−1) from pre-test to post-test (CG Control group; TG Plantar flexion training group). Data are presented as mean percentage change and standard error. Significantly different within group from pre- to post-test: ** P < 0.01, significantly different between groups from pre- to post-test: § P < 0.01
After 8 weeks of training an 8.1% (P = 0.002) increase in HRpeak in TG was observed. There was no change in the CG. Time to exhaustion and [La−]b also showed a significant difference between groups (P = 0.02; P < 0.001, Table 2). The within group increase for the TG was 60.2% (P = 0.003) in [La−]b and 20.0% (P = 0.009) in time to exhaustion, respectively. CG showed a decrease in [La−]b (P = 0.13) from pretest to posttest (Table 2). Maximal ventilation and respiratory exchange ratio also increased in TG (P < 0.001; P = 0.03), and maximal ventilation was significant different from CG (P = 0.002). Eleven out of 14 patients reported that they were no longer limited by leg pain when performing at VO2peak.
Treadmill work economy
Work economy, measured at 0% inclination and 3.2 km h−1 on the treadmill, did not change after 8 weeks of training, neither within the TG group (P = 0.225, Table 2) nor between the two groups (P = 0.780, Table 2).
Stroke volume
CO and SV were measured at VO2peak on the treadmill. No differences in CO or SV within TG (P = 0.562; P = 0.475) or between (P = 0.762; P = 0.316) groups were detected (Table 3; Fig. 3). Mean SV and CO for both groups were 85.2 ± 25.5 ml beats−1 and 11.6 ± 3.3 l min−1, respectively, at pretest. [C(a-v)O2] showed a significant within group increase of 15.3 ± 19.2% (P = 0.035). The CG showed no within group change (P = 0.386) (Table 3). No differences in resting systolic and diastolic blood pressures were detected in TG or CG from pretest to posttest.
Discussion
The main finding in this randomized controlled study was that 8 weeks and 24 sessions of 4 times 4 min individual leg plantar flexion training effectively increased VO2peak and peak exercise performance during walking and that the improvement was not due to cardiac output of the heart. These findings demonstrate that the small muscle mass in the leg is limiting whole body performance and that training of the small muscle mass in individual legs is highly effective in improving whole body exercise performance. It is thus suggested as an effective treatment of PAD patients.
Aerobic capacity
For the plantar flexion, VO2peak and time to exhaustion showed an increase of 23.5 and 41.6% respectively for the TG. This improvement led to an improvement in treadmill VO2peak and time to exhaustion in a ramp protocol of 12.3 and 20.0%, respectively. It is difficult to interpret how much larger the 20% improvement in time to exhaustion would have been in a continuous walking test, and thus cannot be directly compared with these. Also comparisons between graded protocols are difficult since the steps are progressively getting more difficult, and hence the improvement in time to exhaustion will be dependent on the patients starting point. The improvement in VO2peak on the treadmill in TG is large compared to previous studies (Gardner et al. 2005; Hiatt et al. 1994), especially when considering the duration of the intervention. The size of improvement may be explained by the emphasis on the leg muscles in the plantar flexion training intervention and the use of high aerobic intensity. This leads to a large training adaptation as the adaptation might be dependent on power output of the small muscle mass (Shephard et al. 1988) and not cardiovascular factors like the heart for the PAD patients. It has been shown that the use of high aerobic intensity when treadmill walking was more effective in improving VO2peak than moderate intensity (Slordahl et al. 2005). However, Gardner et al. (2005) found no differences between interventions with low and high intensity. This may be due to the fact that the intensity was not adjusted in the 6 months duration of the latter study. It appears to be a universal finding for increasing oxygen uptake development that high intensity shows greater training responses compared to moderate or low intensity even if the pathological picture is different. Superiority of high aerobic intensity is well documented from studies including healthy subjects (Helgerud et al. 2007), heart failure patients (Wisløff et al. 2007) and coronary artery disease patients (Rognmo et al. 2004). Individual leg plantar flexion training puts emphasis on the limiting factor of claudication, and thus high aerobic work intensity through the interval execution. The high VO2peak values in this study might indicate a better trained selection of patients than regularly shown. However, this appears unlikely as all patients showed an ABI <0.9. Furthermore, low [La−]b concentrations and low respiratory exchange ratios before training together with a large improvement in HRpeak with training indicates that the patients were limited by PAD. No changes were apparent in the CG. Since the CG received advices in accordance with existing exercise guidelines improvements might have been expected. This indicates that instructions following exercise guidelines might not affect physical performance. It could be assumed that the control group did not exercise or that exercise has to be supervised to lead to improvements. The CG indicated in conversations that they had not changed their daily routines. Training with supervised moderate intensity (60% of VO2peak) corresponding to patient guidelines has previously been shown to not affect the VO2peak (Slordahl et al. 2005), and the increase in time to exhaustion observed in many studies, including the Slordahl et al. (2005) study, could be explained by improved walking economy.
Since the patients did not perform any training on the treadmill during the 8-week training program the work economy remained unchanged as was expected. The increased capacity from plantar flexion training also led to an increase in HRpeak and [La−]b with training. This might be explained by the reduction of clauducation pain, giving rise to a higher work load on the heart during the test, but not affecting the stroke volume since this load was not represented during the training intervention. The higher load on whole body work also led to an increased [La−]b during the maximal test. The increased treadmill walking capacity from plantar flexion training brought the PAD patients closer to the criteria for reaching their VO2max, and not being limited by claudication when walking. This assumption is also supported by respiratory exchange ratio values that increased from pretest to posttest in TG. Previous studies using the longest training intervention periods also tend to be the ones that document a change in blood flow (Tan et al. 2000). When performing the treadmill posttest in the present study 11 out of 14 patients reported that they were limited by heavy breathing and not by intermittent claudication, the primary symptom of PAD. Measured at the same time, 7 of the patients displayed respiratory exchange ratios above 1.07 and [La−]b values above 5 mmol l−1. This indicate that a reduction in claudication symptoms as in this experiment might put more emphasis on central factors and might in a next step including whole body training lead to changes in stroke volume of the heart and thus blood flow as the patients becomes more fit and the whole body work limitation might shift from small leg muscles to cardiac output.
Cardiac output
Previous studies including PAD patients have rarely found changes in blood flow (Stewart et al. 2002), and for the few who have, the change is far too little to account for the adaptation to training. The present study clearly demonstrated that large improvements in VO2peak are not related to the heart, measured by its cardiac output and stroke volume. This is expected from the training intervention where it is unlikely that the low VO2peak attained in individual leg plantar flexion work should have any effect on the pumping capacity of the heart. It also demonstrated that large increases in VO2peak from training are closely related to PAD patients’ peripheral factors, and that these factors contribute to large functional benefits. The stroke volume in TG was approximately 80 ml beat−1. In comparison values for untrained university students is measured to be 128 ml beat−1 (Zhou et al. 2001). The SB technique of acetylene uptake normally includes a difficult practical breathing procedure where the subjects’ ability to perform the test becomes worse as the intensity increases. In the PAD patients, however, it is somewhat less complicated since the patients often do not hyperventilate as much, because they are limited by their leg muscles and not by central factors.
Study limitations
In addition to the measurements of cardiac output and stroke volume it would have been preferable to include direct measures of which factors that caused the change in C(a-v)O2. A more detailed insight into these mechanisms might have shown if changes in the ischemia threshold and/or peripheral perfusion could have contributed to the observed effects. It would also have been of interest to compare the TG with a treadmill training intervention. A continuous walking test could also have been advantageous as a measure of functional walking capacity. The method for measuring stroke volume is not easy, and is dependent of the patient’s ability to perform the correct breathing procedure. This was overcome by multiple training bouts.
Conclusion
This study demonstrated that plantar flexion training can be used as an effective treatment in patients with PAD. The emphasis on high aerobic intensity, reflected by the individual leg exercise and by the high relative workload during training, may explain the large improvement in VO2peak. The present study also showed that training adaptations were not related to the cardiac output of the heart and hence did not change central cardiac hemodynamics. These findings should have important consequences for training as a treatment and rehabilitation of PAD patients.
References
Andersen P, Saltin B (1985) Maximal perfusion of skeletal muscle in man. J Physiol 366:233–249
Bauer TA, Brass EP, Nehler M, Barstow TJ, Hiatt WR (2004) Pulmonary Vo2 dynamics during treadmill and arm exercise in peripheral arterial disease. J Appl Physiol 97:627–634. doi:10.1152/japplphysiol.00612.2003
Bergh U, Sjodin B, Forsberg A, Svedenhag J (1991) The relationship between body mass and oxygen uptake during running in humans. Med Sci Sports Exerc 23:205–211. doi:10.1249/00005768-199102000-00010
Dibski DW, Smith DJ, Jensen R, Norris SR, Ford GT (2005) Comparison and reliability of two non-invasive acetylene uptake techniques for the measurement of cardiac output. Eur J Appl Physiol 94:670–680. doi:10.1007/s00421-005-1343-2
Gardner AW, Poehlman ET (1995) Exercise rehabilitation programs for the treatment of claudication pain: a meta analysis. JAMA 274:975–980. doi:10.1001/jama.274.12.975
Gardner AW, Montgomery PS, Flinn WR, Katzel LI (2005) The effect of exercise intensity on the response to exercise rehabilitation in patients with intermittent claudication. J Vasc Surg 42:702–709. doi:10.1016/j.jvs.2005.05.049
Haseler LJ, Lin A, Hoff J, Richardson RS (2007) Oxygen availability and PCr recovery rate in untrained human calf muscle: evidence of metabolic limitation in normoxia. Am J Physiol Regul Integr Comp Physiol 293:2046–2051. doi:10.1152/ajpregu.00039.2007
Helgerud J (1994) Maximal oxygen uptake, anaerobic threshold and running economy in women and men with similar performances level in marathons. Eur J Appl Physiol 68:155–161. doi:10.1007/BF00244029
Helgerud J, Høydal KL, Wang E, Karlsen T, Berg PR, Bjerkaas M et al (2007) Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc 39:665–671. doi:10.1249/mss.0b013e3180304570
Hiatt WR, Regensteiner JG, Hargarten ME, Wolfel EE, Brass EP (1990) Benefit of exercise conditioning for patients with peripheral arterial disease. Circulation 81:602–609
Hiatt WR, Wolfel EE, Meier RH, Regensteiner JG (1994) Superiority of treadmill walking exercise versus strength training for patients with peripheral arterial disease. Circulation 90:1866–1874
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. (2006) ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 113:463–454. doi:10.1161/CIRCULATIONAHA.106.174526
Klausen K, Secher NH, Clausen JP, Hartling O, Jensen JT (1982) Central and regional circulatory adaptations to one- leg training. J Appl Physiol 52:976–983
Mayers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE (2002) Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346:793–801. doi:10.1056/NEJMoa011858
Richardson RS, Grassi B, Gavin TP, Haseler LJ, Tagore K, Roca J et al (1999) Evidence of O2 supply- dependent VO2max in the exercise- trained human quadriceps. J Appl Physiol 86:1048–1053
Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slørdahl SA (2004) High intensity aerobic interval training is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary arterial disease. Eur J Cardiovasc Prev Rehabil 11:216–222. doi:10.1097/01.hjr.0000131677.96762.0c
Shephard RJ, Bouhlel E, Vandevalle H, Monod H (1988) Muscle mass as a factor limiting physical work. J Appl Physiol 64:1472–1479. doi:10.1063/1.341820
Slordahl SA, Wang E, Hoff J, Kemi OJ, Amundsen BH, Helgerud J (2005) Effective training for patients with intermittent claudication. Scand Cardiovasc J 39:244–249. doi:10.1080/14017430510035844
Stewart KJ, Hiatt WR, Regensteiner JG, Hirsch AT (2002) Exercise training for claudication. N Engl J Med 347:1941–1951. doi:10.1056/NEJMra021135
Tan KH, Cossart L, Edwards PR (2000) Exercise training and peripheral vascular disease. Br J Surg 87:553–562. doi:10.1046/j.1365-2168.2000.01445.x
Wagner PD (2000) New ideas on limitations to VO2max. Exerc Sport Sci Rev 28:10–14
Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, Sackett DL et al (1996) Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: a critical review. Circulation 94:3026–3049
Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM et al (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients. Circulation 115:3086–3094. doi:10.1161/CIRCULATIONAHA.106.675041
Zhou B, Conlee RK, Jensen R, Fellingham GW, George JD, Fisher AG (2001) Stroke volume does not plateau during exercise in elite male distance runners. Med Sci Sports Exerc 33:1849–1854. doi:10.1097/00005768-200111000-00008
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, E., Hoff, J., Loe, H. et al. Plantar flexion: an effective training for peripheral arterial disease. Eur J Appl Physiol 104, 749–756 (2008). https://doi.org/10.1007/s00421-008-0826-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-008-0826-3