Abstract
The relative contribution of sympathetic nervous system (SNS)-induced increase in peripheral vascular resistance on central artery blood pressure (BP) and aortic wave reflection (augmentation index; AIx) is not completely understood. Central BP and wave reflection characteristics were measured using radial artery applanation tonometry before, during a 3-min cold pressor test (CPT), and 90 and 180-s post-CPT in 15 young, healthy adults (25 ± 1 years). The CPT resulted in a greater magnitude of change in the estimated aortic systolic (31 vs. 23%, P < 0.05) and pulse (31 vs. 13%, P < 0.05) BP compared with the change in brachial artery BP. Additionally, the CPT resulted in an increased mean arterial pressure (MAP) (P < 0.05) and AIx (10 ± 2 vs. 26 ± 2%, P < 0.05). The change in MAP during the CPT was correlated to the change in AIx (r = 0.73, P < 0.01) and inversely related to roundtrip duration of the reflected wave to the periphery and back (r = –0.57, P < 0.05). The present study suggests that cold pressor testing results in a significant increase in arterial wave reflection intensity, possibly due to an increased MAP. However, the greater increase in systolic and pulse BP in the central compared with the peripheral circulation suggests that increased central artery wave reflection intensity contributes to increased left ventricular myocardial oxygen demand during CPT-induced hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increased sympathetic nervous system (SNS) traffic to resistance arteries/arterioles in skeletal muscle contributes to the onset and sustained increase in blood pressure (BP), and is a plausible mechanism for the development of hypertension (Esler 2000). Increased peripheral vascular tone of peripheral muscular arteries/arterioles has important effects on the central circulation as this leads to increased pulse wave velocity of reflected arterial pressure waves which return early to the central circulation during systole (Nichols 2005; Nichols and Singh 2002). The early return of arterial pressure waves augments the amplitude of central systolic and pulse BPs, resulting in elevated wave reflection intensity (i.e., augmentation index, AIx) which increases left ventricular (LV) afterload and myocardial oxygen demand (Nichols 2005). Additionally, the augmented central BP causes a mismatch in vascular coupling between central and peripheral arteries and thus decreases pulse pressure (PP) amplification (PPA; i.e., the ratio of peripheral PP and central PP). These changes are of clinical importance since central BP more strongly relates to vascular disease and outcome than does brachial BP (Roman et al. 2007).
Acute SNS activation with a cold pressor test (CPT) results in a robust increase in mean arterial pressure (MAP) due to increased peripheral vascular resistance via elevated vascular tone of peripheral muscular arteries/arterioles (Victor et al. 1987). However, the relative contribution of SNS activation on central artery (i.e., aorta) BP and wave reflection characteristics in healthy adults is not completely understood. Therefore, we tested the hypothesis that acute SNS activation would have a greater influence on central artery BP when compared with brachial BP, due to increased arterial wave reflection intensity.
Methods
Subjects
Fifteen young, healthy adults (n = 15; 9 males; age range 21–29) were recruited for participation in the study. All the subjects were either sedentary or recreationally active (≤2 days of activity/exercise per week), and none were participating in a structured exercise program. Additionally, all subjects were normotensive (<140/90 mmHg), non-smokers, non-obese (body mass index, BMI < 30 kg/m2), free from overt cardiovascular disease and were not receiving medication. All measurements were performed in the morning by the same investigator in a quiet, temperature controlled room (21–23°C) following an 8–12 h overnight fast. All measurements for female subjects were completed in the early follicular phase of their menstrual cycle and no subjects were taking birth control medications. Subjects were asked to abstain from caffeine and alcohol for at least 24 h prior to visiting the laboratory. Subjects were also asked to avoid strenuous physical activity at least 24 h prior to the study day. All subjects provided written informed consent prior to participation in the study.
Brachial artery blood pressure and heart rate
Following a 15-min rest period in a supine position, heart rate (HR) and brachial systolic and diastolic BP measurements were performed in triplicate in the right arm using an automated non-invasive BP cuff (Omron, Bannockburn, IL, USA). An average of three HR and BP measurements was used for resting values.
Pulse wave analysis
Assessment of arterial wave reflection characteristics was performed non-invasively using the SphygmoCor system (AtCor Medical, Sydney, Australia). High-fidelity radial artery pressure waveforms were recorded by applanation tonometry of the radial pulse in the left wrist using a “pencil type” micromanometer (Millar Instruments, Houston, TX, USA). The aortic pressure waveform is derived non-invasively from the radial pulse using applanation tonometry and application of a generalized transfer function, which corrects for pressure wave amplification in the upper limb (Nichols and O’Rourke 2005). The generalized transfer function has been validated using both intra-arterially (Chen et al. 1997; Pauca et al. 2001) and non-invasively (Gallagher et al. 2004) obtained radial pressure waves. The test–retest reproducibility of this procedure was previously established by others (Wilkinson et al. 1998). In our laboratory reproducibility of AIx was evaluated by triplicate measurement on nonconsecutive days in young, healthy men with a mean coefficient of variation of 6.5% (Casey et al. 2006).
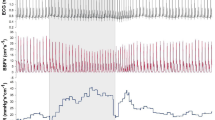
The central aortic pressure wave is composed of a forward traveling wave, generated by LV ejection and a reflected wave that is returning to the ascending aorta from the periphery (Fig. 1) (Nichols and Singh 2002). The AIx is defined as reflected wave amplitude divided by PP and is expressed as a percentage (Murgo et al. 1980). The reflected pressure wave amplitude is referred to as augmented pressure (AP) and is defined as the difference between the first (forward wave) and second systolic shoulders of the central systolic BP. The forward and reflected waves travel in opposite directions along the artery at the same velocity. The round trip travel time (Tr) of the forward traveling wave from the ascending aorta to the major reflection site and back is measured from the foot of the forward traveling pressure wave to the foot of the reflected wave. The Tr is inversely related to arterial pulse wave velocity and arterial stiffness, and directly related to the distance to the reflecting site (Nichols and Singh 2002). AIx is an index of wave reflection intensity, which is influenced by both systemic and peripheral arterial stiffness. Wasted LV pressure energy (ΔE w) is that component of extra myocardial oxygen requirement that is due to early systolic wave reflection, and can be estimated as 2.09 × AP(ED – Tr), where 2.09 is the conversion factor for mmHg s–1 to dynes s–1 cm2 and ED is ejection duration (Murgo et al. 1980; Nichols and Singh 2002). The aortic systolic tension time index (As), a marker of aortic systolic stress and myocardial oxygen demand, was estimated as the integral of aortic pressure and time during ventricular systole. The aortic diastolic tension time index (Ad), an indirect indicator of diastolic perfusion, was estimated as the integral of the diastolic pressure during ventricular diastole (Nichols and O’Rourke 2005). PPA from the aorta to the periphery was estimated as the ratio of brachial PP and central aortic PP (Nichols and O’Rourke 2005). Assessment of central arterial pressure waves is described in detail by Nichols and Singh (2002).
Typical high-fidelity derived ascending aorta pressure waveform with pulse wave analysis components. P s aortic systolic pressure, P d aortic diastolic pressure, P i inflection pressure where incident and reflected waves merge, Tr round trip travel time of reflected pressure wave to peripheral reflecting sites and back to heart, ED ejection duration. Wasted energy is the energy or force (or effort) the left ventricle must generate to overcome the late systolic augmented pressure due to wave reflection
Cold pressor test
Following baseline peripheral and central hemodynamic measurements, a CPT was employed to evoke SNS stimulation (Koch et al. 2003). The subject’s right hand was passively immersed up to the wrist in ice water (4°C) for 3 min and then withdrawn. Tonometric recordings were made during the last 15 s of the CPT (endCPT), 90- and 180-s post-CPT. Brachial BP measurements were taken prior to each tonometric recording. All the measurements were performed with the subject in the supine position.
Statistical analysis
All data are reported as mean ± SEM. One-way ANOVA with repeated measures and pairwise comparisons with Bonferonni correction were used for the analysis of variables compared to baseline. Since Bonferonni correction was used and three pairwise comparisons (baseline vs. endCPT, baseline vs. 90-s post-CPT, and baseline vs. 180-s post-CPT) were used, an alpha level of P < 0.016 (0.05/3) was required for statistical significance for all pairwise comparisons. In addition, the difference in the magnitude of change between brachial and central pressures (from baseline to endCPT) was analyzed using independent t tests and an alpha of P < 0.05 was required for statistical significance. Bivariate Pearson’s correlations between change in MAP at endCPT with indices of arterial stiffness (i.e., AIx and Tr) were performed. An alpha of P < 0.05 was required for significant correlations. All statistical analyses were performed using SPSS 14.0 for Windows (SPSS, Inc., Chicago, IL, USA).
Results
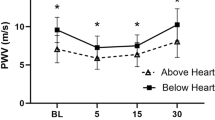
All 15 subjects (mean age of 25 ± 1 years; BMI = 22.7 ± 0.6) completed the study. There was no change in HR in response to the CPT (Table 1). At endCPT, there was an increase in all components of brachial and central blood pressures (P < 0.05). The change in systolic BP (31 ± 3 vs. 27 ± 3 mmHg) and pulse BP (9 ± 1 vs. 5 ± 1) was greater in the aorta when compared with the brachial (P < 0.05, Fig. 2). The greater change in central PP compared to brachial pulse BP resulted in a reduction in PPA (P < 0.05). AIx increased and Tr decreased at endCPT (P < 0.05). Changes in aortic pressure wave intensity (AIx) and Tr resulted in elevated levels of As and ΔE w at endCPT (P < 0.05).
Brachial pressures did not differ from baseline values at 90-s post-CPT. Central systolic BP, AP, and MAP continued to be elevated 90-s post-CPT (P < 0.05). This resulted in higher AIx, As, and ΔE w at 90 s post when compared to baseline values (P < 0.05; Table 1). All hemodynamic variables at 180-s post-CPT were not different than baseline values.
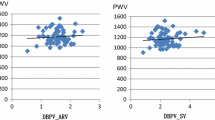
Bivariate Pearson’s correlation analysis demonstrated a relation between the change in MAP and the change in AIx (r = 0.73, P < 0.01; Fig. 3a). There was also a relation between the change in MAP and the change in Tr (r = −0.57, P < 0.05; Fig. 3b).
Discussion
The primary finding of the present study was that the magnitude of change in central systolic and pulse BP is greater than the magnitude of change in brachial artery BP following an acute elevation in SNS activity via CPT. Additionally, we found that the change in MAP during the CPT was related to the changes in wave reflection characteristics (AIx and Tr). Together, these findings suggest that an increased amplitude and/or early return of the arterial reflected pressure wave from the periphery during acute SNS elevation contributes to the increased AIx in young healthy adults.
Mean arterial pressure is a key determinant of arterial stiffness and wave reflection intensity (Laurent et al. 1993). Accordingly, the change in MAP during CPT showed a strong correlation with the change in AIx (r = 0.73) and was inversely related with the change in Tr (r = −0.57). The increase in MAP observed in the present study is likely due to increased total peripheral vascular resistance due to α-adrenergic vasoconstriction of muscular arteries and arterioles elicited by the acute cold and/or pain stress (Dinenno et al. 2001). Vasoconstriction of peripheral muscular arteries and arterioles also leads to an increase in pulse wave velocity (PWV) (Geleris et al. 2004) and possibly a decrease in the distance of peripheral reflecting sites (i.e., more proximal reflecting sites). Although PWV was not directly assessed in the present study, Tr was decreased. A decrease in Tr indicates that the reflected wave returns early to the ascending aorta and merges with the incident wave during systole and augments the aortic pressure. The early return of the reflected wave leads to greater LV myocardial oxygen demand (systolic tension time index, As) and thus requires a greater LV energy (i.e., wasted energy, ΔE w) to overcome this added augmentation of pressure (Nichols 2005). The results indicate that the augmentation of the central pressure wave during the CPT resulted in a 33% increase in As and a threefold increase in LV ΔE w.
The results are in agreement with two previous studies that demonstrated CPT causes an increase in AIx. Geleris et al. (2004) demonstrated that the magnitude of change in AIx during CPT is comparable to the AIx changes observed during isometric handgrip exercise, another test of sympathetic activation. Edwards et al. (2006) showed that acute whole body exposure to cold (via an environmental chamber) for 30 min resulted in increases in AIx and central pressures. However, the results differ from these studies in several ways. First, Geleris et al. (2004) reported only brachial artery BP before and after CPT, whereas we derived at both central and peripheral BP and demonstrated that central BP increases more than peripheral BP upon acute SNS activation. Second, the CPT in this study was used experimentally to increase MAP via SNS activation, not to examine the effects of whole body cooling. This allowed us to manipulate SNS activity without the confound of a decreased core body temperature, thus isolating the acute changes in vascular resistance and MAP on central artery BP and wave reflection characteristics. Although SNS activity was not measured, the CPT evokes acute increases in SNS activity, as measured by microneurography (Dishman et al. 2003; Lambert and Schlaich 2004; Schobel et al. 1998) and plasma catecholamine levels (Pascualy et al. 1999; Schobel et al. 1998).
In conclusion, acute SNS activation via CPT results in greater increases in systolic and pulse BP in the central circulation when compared to the peripheral circulation. Additionally, CPT in young healthy adults results in an increase in AIx, possibly due to an increased MAP. Increased central artery wave reflection intensity also contributes to increased LV myocardial oxygen demand during acute SNS activation-induced hypertension.
References
Casey DP, Pierce GL, Nichols WW, Braith RW (2006) Measurement of pulse wave velocity and augmentation index is reproducible in young, healthy men (abstract). Med Sci Sport Exer 38:S185–S186
Chen CH, Nevo E, Fetics B, Pak PH, Yin FC, Maughan WL, Kass DA (1997) Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure: validation of generalized transfer function. Circulation 95:1827–1836
Dinenno FA, Tanaka H, Stauffer BL, Seals DR (2001) Reductions in basal limb blood flow and vascular conductance with human ageing: role for augmented alpha-adrenergic vasoconstriction. J Physiol 536:977–983
Dishman RK, Nakamura Y, Jackson EM, Ray CA (2003) Blood pressure and muscle sympathetic nerve activity during cold pressor stress: fitness and gender. Psychophysiology 40:370–380
Edwards DG, Gauthier AL, Hayman MA, Lang JT, Kenefick RW (2006) Acute effects of cold exposure on central aortic wave reflection. J Appl Physiol 100:1210–1214
Esler M (2000) The sympathetic system and hypertension. Am J Hypertens 13:99S–105S
Gallagher D, Adji A, O’Rourke MF (2004) Validation of the transfer function technique for generating central from peripheral upper limb pressure waveform. Am J Hypertens 17:1059–1067
Geleris P, Stavrati A, Boudoulas H (2004) Effect of cold, isometric exercise, and combination of both on aortic pulse in healthy subjects. Am J Cardiol 93:265–267
Koch DW, Leuenberger UA, Proctor DN (2003) Augmented leg vasoconstriction in dynamically exercising older men during acute sympathetic stimulation. J Physiol 551:337–344
Lambert EA, Schlaich MP (2004) Reduced sympathoneural responses to the cold pressor test in individuals with essential hypertension and in those genetically predisposed to hypertension: no support for the “pressor reactor” hypothesis of hypertension development. Am J Hypertens 17:863–868
Laurent S, Hayoz D, Trazzi S, Boutouyrie P, Waeber B, Omboni S, Brunner HR, Mancia G, Safar M (1993) Isobaric compliance of the radial artery is increased in patients with essential hypertension. J Hypertens 11:89–98
Murgo JP, Westerhof N, Giolma JP, Altobelli SA (1980) Aortic input impedance in normal man: relationship to pressure wave forms. Circulation 62:105–116
Nichols WW (2005) Clinical measurement of arterial stiffness obtained from noninvasive pressure waveforms. Am J Hypertens 18:3S–10S
Nichols WW, O’Rourke MF (2005) McDonald’s blood flow in arteries: theoretical, experimental and clinical principles, 5th edn. Hodder Arnold Publishing, London
Nichols WW, Singh BM (2002) Augmentation index as a measure of peripheral vascular disease state. Curr Opin Cardiol 17:543–551
Pascualy M, Petrie EC, Brodkin K, Peskind ER, Veith RC, Raskind MA (1999) Effects of advanced aging on plasma catecholamine responses to the cold pressor test. Neurobiol Aging 20:637–642
Pauca AL, O’Rourke MF, Kon ND (2001) Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension 38:932–937
Roman MJ, Devereux RB, Kizer JR, Lee ET, Galloway JM, Ali T, Umans JG, Howard BV (2007) Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the strong heart study. Hypertension 50:197–203
Schobel HP, Heusser K, Schmieder RE, Veelken R, Fischer T, Luft FC (1998) Evidence against elevated sympathetic vasoconstrictor activity in borderline hypertension. J Am Soc Nephrol 9:1581–1587
Victor RG, Leimbach WN Jr, Seals DR, Wallin BG, Mark AL (1987) Effects of the cold pressor test on muscle sympathetic nerve activity in humans. Hypertension 9:429–436
Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, Cockcroft JR, Webb DJ (1998) Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens 16:2079–2084
Conflict of interest
There are no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Casey, D.P., Braith, R.W. & Pierce, G.L. Changes in central artery blood pressure and wave reflection during a cold pressor test in young adults. Eur J Appl Physiol 103, 539–543 (2008). https://doi.org/10.1007/s00421-008-0746-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-008-0746-2