Abstract
We evaluated the effects of regular physical exercise on anemia and iron status in young non-professional female athletes. A total of 191 healthy white Italian women (23.5 ± 4.68 years) were analyzed; 70 were non-professional athletes performing 11.1 ± 2.63 h week−1 exercise and 121 were sedentary controls. Blood markers of anemia and iron status—hemoglobin (Hb), hematocrit (Hct), red blood cells (RBC), serum ferritin, iron, transferrin (Tf), transferrin saturation (TfS), soluble transferrin receptor (sTfR), and the sTfR/log ferritin ratio (sTfR-F index)—were evaluated. Anemia threshold was Hb < 120 g l–1. Ferritin concentrations < 12 μg l–1 were considered as iron deficiency (ID). Frequency of anemia (15.7 versus 10.7%, P = 0.32), ID (27.1 versus 29.8%, P = 0.70), and ID anemia (8.6 versus 5.8%, P = 0.46) was not different in athletes and controls. However, athletes were threefold more likely than controls (17.1 versus 5.8%) to have serum iron < 50 μg dl–1 [odds ratio (OR) 3.37, P = 0.012]. Low-TfS (<15%) was found in 25.7% of athletes and in 13.2% of controls, OR 2.27, P = 0.030. Elevated-sTfR (>1.76 mg l–1) was found in 24.3% of athletes and in 12.4% of controls, OR 2.27, P = 0.034. Regular non-professional sport activity does not cause an increased rate of anemia or of iron deficiency in fertile women. However, physical exercise has an impact on iron status as it reduces serum iron and transferrin saturation, and elevates sTfR. Nearly one fifth of recreational athletes have anemia and a third have iron deficit, these conditions can decrease their physical performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia is particularly detrimental for athletes because impairment of blood gas transport may decrease physical work capacity and may be a reason for fatigue, weakness, and dizziness. Numerous factors may contribute to the development of anemia in athletes: increased iron demand and loss (a consistent iron loss occurs through sweating), intravascular mechanical hemolysis (including foot-strike hemolysis), and dilutional pseudoanemia (Beard and Tobin 2000; Shaskey and Green 2000; Mercer and Densmore 2005). Thus, very frequently anemia in athletes is due to iron deficiency (ID) (Beard and Tobin 2000). ID impairs aerobic exercise, endurance capacity and energetic efficiency, by reducing concentrations and activities of iron-containing oxidative enzymes (Beard and Tobin 2000; Brownlie et al. 2004).
If untreated, ID can ultimately develop into anemia (IDA). In athletes, several studies found a greater prevalence of IDA than in the general population, i.e., 11–14 versus 3–5% in women of childbearing age and 2–3 versus <1% in young men (Looker et al. 1997; Dubnov and Constantini 2004; Sinclair and Hinton 2005).
Fertile female athletes have a disadvantage, with respect to male athletes, of blood loss due to menstruations. Moreover, in female athletes the dietary intake of iron is lower frequently than in male athletes (Dubnov and Constantini 2004). Thus, sportswomen incur more frequently in IDA and in ID than trained men (Dubnov and Constantini 2004; Landahl et al. 2005). Few data are available on the effects of iron status due to recreational physical activity performed by adult young females (Beard and Tobin 2000). One study evaluated the prevalence of ID with (11%) and without (30%) anemia in fertile US women performing recreational aerobic training, total ID was 41% (Sinclair and Hinton 2005). Whereas, a US general population study found 11% ID in women of 20–49 years-old (Looker et al. 1997).
Many biochemical markers are used to evaluate body iron stores, but some of these are subjected to diurnal variations and affected by numerous clinical disorders. Serum ferritin is the most used indicator. However, being an acute phase protein, ferritin levels increase in infections, inflammations, disorders of the liver, and malignancies, and thus several conditions may mask the actual iron deficiency. It has been demonstrated that the physical activity is accompanied by inflammation-like reactions in the joints and muscles, which may induce a rise of ferritin in plasma persisting for few days following strenuous exercise (Malczewska et al. 2000a; Nikolaidis et al. 2003). In contrast to ferritin, the soluble transferrin receptor (sTfR) is not an acute phase protein; it has a low-biological variability and remains quite stable after exercise or a brief training period (Malczewska et al. 2000a; Schumacher et al. 2002). Serum concentrations of sTfR are proportional to TfR present on erythroid precursors in bone marrow and increase in the absence of marrow iron (Brugnara 2003). Furthermore, sTfR is a sensitive marker of stimulated erythropoiesis (Parisotto et al. 2001; Brugnara 2003). In recent years, the sTfR-F index has been widely used as a measure of iron deficit, being more sensitive and specific than sTfR or ferritin itself (Punnonen et al. 1997). A study showed that in athletes, the sTfR-F index remains stable in spite of significant changes in ferritin levels after a physical load (Stupnicki et al. 2003). Malczewska et al. (2001) found that the sTfR-F index had an elevated diagnostic value in detecting iron deficient erythropoiesis in athletes.
Few published studies have focused on anemia and iron depletion in young adult non-professional female athletes. The aim of this study was to evaluate the effects of regular physical exercise on iron status in a population of young healthy menstruating women, and to compare the frequency of anemia and ID in athletes and sedentary controls.
Methods
Subjects
Healthy white Italian women (range 18–35 years) were enrolled consecutively at the campus of Udine University, from May 2006 to June 2007. Before entering the study, each woman was interviewed to determine whether she fulfilled the enrollment criteria: non-pregnant or breast-feeding woman, no recent blood donor, no use of supplements containing iron exclusively, no menstrual dysfunction, current infections, chronic inflammatory diseases, or major diseases such as diabetes, and absence of a known thalassemia trait. Furthermore, a detailed record regarding physical exercise activity and lifestyle factors including demographic and medical data was collected for each woman through a questionnaire. Most of the athletes were enrolled at Sport Sciences, Udine School of Medicine. We recruited recreational athletes. They have been performing for at least 3 months, 9 or more h week–1 of regular physical exercise. Controls were women not practicing sport activities and performing <3 h week–1 physical exercise.
The study was conducted with the approval of the Udine School of Medicine Ethics Committee; written informed consent was obtained from all study participants. The methods used in this study were in accordance with the Helsinki Declaration of 1975 as revised in 1983.
Measurements
Venous blood samples were drawn from seated subjects in the morning after overnight fasting, as described (Banfi and Dolci 2003; Casabellata et al. 2007). Women were required to avoid exercise 24 h prior to the blood donation. Full blood counts and hemoglobin (Hb) measurements were performed with Cell-Dyn Sapphire analyzer (Abbott Laboratories, Chicago, IL, USA). Anemia was defined as Hb < 120 g l–1(Looker et al. 1997).
Serum iron (reference interval 50–150 μg dl–1) was analyzed on the Modular analyzer (Roche/Hitachi, Mannheim, Germany) using Roche reagents.
Serum ferritin was determined on the Abbott Architect i2000 analyzer (Abbott Laboratories), using the Abbott Architect Ferritin immunoassay. The analytical sensitivity of the assay was ≤1 μg l–1. The intra- and inter-assay imprecision CVs were 3.6 and 7.3%, respectively. Ferritin values < 12 μg l–1 were considered as ID in females (Looker et al. 1997; Milman et al. 2003). Moreover, the cutoff of <20 μg l–1 was examined because it is frequently chosen in studies comprising both male and female athletes (Malczewska et al. 2000b; Friedmann et al. 2001; Dubnov and Constantini 2004). In addition, ferritin < 30 μg l–1 was examined as this threshold corresponds to absent stainable bone-marrow hemosiderin iron (Milman et al. 2003; Fallon 2007). Iron deficiency anemia (IDA) was defined as ferritin < 12 μg l–1 and Hb < 120 g l–1 (Looker et al. 1997).
The sTfR concentration (reference interval 0.83–1.76 mg l–1) was determined on the nephelometer analyzer BN-II (Dade Behring, Marburg, Germany), using a Dade Behring assay (Thomas and Thomas 2002; Banfi et al. 2006; Casabellata et al. 2007). Analytical sensitivity of the assay was ≤0.15 mg l–1. The intra- and inter-assay CVs% were 1.5 and 3.3%, respectively. We calculated the ratio of sTfR to log ferritin (sTfR-F index) and used the cutoff of 1.5 to assess marrow iron depletion (Punnonen et al. 1997; Thomas and Thomas 2002).
Transferrin (reference interval 200–360 mg dl–1) was measured by nephelometry, using a Dade Behring assay. Additionally, the threshold of 330 mg dl–1 was evaluated (Casabellata et al. 2007).
The percent of transferrin saturation [TfS (%)] was calculated according to the formula: TfS (%) = serum iron (mg l–1) × 70.9 / Tf (g l–1) (Thomas 1998).
Haptoglobin (reference interval 30–200 mg dl–1) and C-reactive protein (CRP) were measured on the Modular analyzer (Roche/Hitachi, Mannheim, Germany) using Roche Diagnostics reagents. Samples with CRP > 10 mg l–1 were excluded from the study because they were regarded as having suspected current inflammatory processes (Thomas and Thomas 2002).
Statistical analysis
Descriptive data were presented as mean and standard deviation (SD). For skewed markers, median (25th to 75th percentile, interquartile, IQR) values were reported and non-parametric tests used. The Mann–Whitney test was used for comparison of continuous variables. The difference of proportions between athletes and controls was assessed by χ2-test using Pearson test. Odds ratios (ORs) and 95% confidence intervals (CIs) were evaluated for categorical variables. Bivariate relationships were evaluated by Spearman ρ test (r s). All tests were two-sided. P < 0.050 was considered statistically significant. Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL).
Results
Out of 215 participants screened, 191 women met study inclusion and exclusion criteria, 70 of them were recreational athletes and 121 were sedentary controls. Sport activities practiced by athletes are described in Table 1.
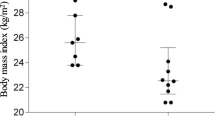
The majority of the 191 study women (91%, 174/191) were in the normal weight range (BMI > 18.0 and < 25.0 kg m–2). They were aged 23.5 ± 4.68 years, BMI was 20.9 ± 2.25 kg m–2, 96.3% were nulliparous, most women were University students or personnel, and all had a middle-class socioeconomic status. The comparison of demographic and life style characteristics of 70 female athletes performing 11.1 ± 2.63 h exercise per week (range 9–20 h week−1) and 121 sedentary control women performing 0.7 ± 0.92 h exercise per week (range from 0 to <3 h week–1) are described in Table 2. Athletes and sedentary women did not differ in alimentary habits with regard to meat, fish, vegetables, carbohydrate, and alcohol consumption (data not shown).
Comparisons of continuous values of the most relevant blood biomarkers measured in athletes and sedentary controls are illustrated in Table 3. Most of blood markers did not differ significantly between athletes and sedentary controls. However, athletes exhibited a lower number of platelets (P = 0.042) and increased mean platelets volume (MPV; P = 0.023) with respect to sedentary women. Notably, athletes showed a significant decrease of serum iron (P = 0.005) and TfS (P = 0.010). However, transferrin and ferritin concentrations did not differ between the two groups. Concentrations of sTfR tended to be increased in athletes (P = 0.072), whereas haptoglobin concentrations tended to be lower (P = 0.060).
The effects of physical exercise on categorical blood markers for anemia and iron status are shown in Table 4. Confirming the findings described in Table 3, physical exercise was not associated with anemia, IDA (Hb < 120 g l–1 and ferritin < 12 μg l−1), low-hematocrit levels, low-ferritin levels, and elevated transferrin or sTfR-F index levels. However, physical exercise was associated with a threefold higher frequency of low-serum iron < 50 μg dl–1 (OR = 3.37, P = 0.012) and with a twofold higher frequency of either TfS < 15% (OR = 2.27, P = 0.030), and TfS < 18% (OR = 2.21, P = 0.014). In addition, elevated sTfR > 1.76 mg l–1 levels were twofold more frequent in athletes than in controls (OR = 2.27, P = 0.034). Notably, athletes were nearly fourfold more likely than controls to show low-haptoglobin levels (<30 mg dl–1) (OR = 3.72, P = 0.020). No other categorical measure was affected by physical exercise.
Among the 12 athletes with serum iron < 50 μg dl–1; two women had anemia; one woman had both RBC < 4.00 × 1012 l–1 and Hct < 36%; and one woman had low-Hct. All these athletes had TfS < 15% and 50% had ferritin < 12 μg l–1.
Among the 17 athletes with elevated sTfR > 1.76 mg l–1; one woman had anemia, low-RBC, and low-Hct; three women had anemia and low-Hct; two had low-Hct; and one had anemia. Furthermore, 53% of these athletes had TfS < 15% and 53% had ferritin < 12 μg l–1. Finally, 41% had serum iron < 50 μg dl–1.
In athletes and controls, concentrations of sTfR were inversely correlated with TfS (r s = –0.333, P = 0.005; r s = –0.198, P = 0.030, respectively).
Discussion
Physical exercise is widely recommended as a healthy behavior to reduce the risk of several diseases such as cardiovascular diseases, metabolic syndrome, insulin resistance, diabetes, osteoporosis, breast cancer, and other clinical or subclinical disorders including adverse pregnancy outcome (Verloop et al. 2000; Pedersen and Saltin 2006; Siega-Riz et al. 2006). However, intense physical activity has the potential to worsen the hematologic profile, this exercise side-effect is particularly undesirable in fertile age women, who comprise a population per se exposed to a high-frequency of anemia and ID. The effects on women’s iron stores of physical exercise performed even at non-professional levels are important issues. In spite of this, there is, in general, poor attention to the health status of asymptomatic women performing recreational physical activity. In fact, most studies on ID and IDA focused on elite female athletes, or examined non-professional male and female athletes altogether, and/or without exact specification of the ethnic group. To the best of our knowledge, our study was the largest one to assess the prevalence ID and IDA in non-professional young adult white female athletes with respect to matched sedentary women.
Interestingly, trained women exhibited a marked reduction of both serum iron and percent of transferrin saturation with respect to sedentary controls. Specifically, recreational athletes were three times more likely to show low-iron levels (<50 μg dl–1) and two times more likely to show low-transferrin saturation (both <15 and <18%) than sedentary controls. However, transferrin concentrations were not affected by exercise, thus, it is likely that the decrease in serum iron concentrations produced the decrease of transferrin saturation.
Low-transferrin saturation from our findings appears to be associated with the elevation of sTfR, thus with induction of erythropoiesis. Consistently, we found a twofold higher frequency of elevated sTfR (>1.76 mg l–1) in athletes compared to sedentary women. Overall, in our study physical activity appears to impact the iron status of young women. However, physical activity did not cause an increase of severe iron-connected conditions. The rates of ID and IDA were not increased in recreational female athletes in respect to sedentary controls.
Serum ferritin levels below which the athletes are considered “iron deficient” vary considerably in different studies. Thus, we examined three different cutoffs, ferritin concentrations <12, <20, and <30 μg l–1. However, whatever ferritin cutoff was chosen we did not observe a higher frequency of low-ferritin values in athletes compared to sedentary controls. In our study women with signs of inflammation were excluded, thus it is unlikely that inflammation affected ferritin concentrations. Some recent studies adopted the sTfR-F index to assess iron deficient erythropoiesis in athletes (Malczewska et al. 2001; Stupnicki et al. 2003; Sinclair and Hinton 2005). Based on this marker, we found a prevalence of increased iron deficient erythropoiesis in 30% of athletes versus 24% of controls; however, this difference was not significant (P = 0.43). Thus, we were not able to document reduced body iron stores in athletes compared to sedentary women.
We observed a rate of 15.7% anemia, 27.1% ID, and 8.6% IDA, in 70 Italian non-professional athletes performing an average of 11.1 ± 2.63 h week–1 exercise. Our results showed lower rates than those observed by Sinclair and colleagues (Sinclair and Hinton 2005) in 72 US female recreational athletes performing 10.5 ± 6.3 h week–1 exercise, in which the frequency of ID was 39% and that of IDA was 9.7%. However, these authors chose a ferritin threshold (<16 μg l–1) higher than ours, this may in part account for the higher frequency of ID they found.
On the opposite, a very recent study by Fallon (2007) performed in 273 elite female athletes found a three times lower percentage of athletes with ferritin < 30 μg l–1 than that in our study (19 versus 64%). It is likely that the female athletes entering an elite training program are both more frequently screened for iron status and more induced to use iron supplements than non-professional athletes (Fallon 2004). In fact, most of the women we enrolled never assessed their iron status prior to this study.
Several authors have studied the incidence of anemia, ID, and IDA in female elite athletes, particularly in endurance athletes (Malczewska et al. 2000b; Friedmann et al. 2001; Dubnov and Constantini 2004). For example, a study on female top-level basketball players showed that 38% had anemia (Hb < 120 g l–1), 35% had ID (ferritin < 20 μg l–1), and 14% had IDA (ferritin < 12 μg l–1, TfS < 16%, and anemia) (Dubnov and Constantini 2004). It is likely that in female athletes several factors affect the observed rate of ID and IDA, not only the intensity and duration of training, but also the kind of exercise (aerobic versus anaerobic) and the woman awareness of the importance of her iron status, inducing a higher frequency of iron status testing and supplementation. A limitation of our study was that most of our athletes were performing volleyball (an alternate anaerobic–aerobic activity). However, this is one of the most common recreational team sport activity practiced by young women. Another limitation is the cross-sectional design of the study. A longitudinal study, which is being planned, could better inform about the temporal effects on athletes iron status to assess causal relationships between changes of iron markers levels and physical activity.
Our findings give further support to the assumption made by other authors (Friedmann et al. 2001) that the decrease of serum iron and transferrin saturation in female athletes does not correspond to a real iron deficit condition (Malczewska et al. 2000b). In particular, it has been hypothesized that the decrease of transferrin saturation is a major factor driving increased erythropoiesis and intestinal iron absorption (Roecker et al. 2005; Atanasiu et al. 2007). In fact, about half of our athletes with elevated sTfR levels did not show low-ferritin (<12 μg l–1). In athletes, this mechanism is needed to sustain the exercise induced increased RBC turnover and the loss of RBC by intravascular hemolysis, likely. In fact, we noted that low-haptoglobin levels were almost fourfold more frequent in athletes compared to controls. Low-haptoglobin is considered the most sensitive indicator of intravascular hemolysis. It can be inferred that sport training causes a low-grade hemolysis, that is detected by reduced haptoglobin concentrations even in the absence of serum bilirubin elevation.
Strength of our study is that we examined an ethnically homogenous population of white Italian women, in a rather narrow interval of age (23.5 ± 4.68 years) and BMI (20.9 ± 2.25 kg m–2). On the other hand, as ethnic differences were noted for hematologic indices (Malcovati et al. 2003), our data could not take into account effects of physical training on women belonging to other ethnic groups, and/or of older/younger age, and/or with higher BMI (Ramakrishnan et al. 2002).
Overall, our study documented an altered iron status in recreational athletes, but did not find negative effects of exercise on iron stores and Hb concentrations in young female athletes.
Recreational athletes were not invited to check and take care of their iron status like elite athletes, despite non-elite athletes account for a much larger proportion of the female population than elite athletes. We found that almost a fifth of athletes have anemia and a third have iron deficiency, as these conditions are detrimental to physical activity, our findings support a greater attention to iron status of young women performing recreational physical exercise.
References
Atanasiu V, Manolescu B, Stoian I (2007) Hepcidin-central regulator of iron metabolism. Eur J Haematol 78:1–10
Banfi G, Dolci A (2003) Preanalytical phase of sport biochemistry and haematology. J Sports Med Phys Fitness 43:223–230
Banfi G, Del Fabbro M, Mauris C, Corsi MM, Melegati G (2006) Haematological parameters in elite rugby players during a competitive season. Clin Lab Haematol 28:183–188
Beard J, Tobin B (2000) Iron status and exercise. Am J Clin Nutr 72:594S–597S
Brownlie T 4th, Utermohlen V, Hinton PS, Haas JD (2004) Tissue iron deficiency without anemia impairs adaptation in endurance capacity after aerobic training in previously untrained women. Am J Clin Nutr 79:437–443
Brugnara C (2003) Iron deficiency and erythropoiesis: new diagnostic approaches. Clin Chem 49:1573–1578
Casabellata G, Di Santolo M, Banfi G, Stel G, Gonano F, Cauci S (2007) Evaluation of iron deficiency in young women in relation to oral contraceptive use. Contraception 76:200–207
Dubnov G, Constantini NW (2004) Prevalence of iron depletion and anemia in top-level basketball players. Int J Sport Nutr Exerc Metab 14:30–37
Fallon KE (2004) Utility of hematological and iron-related screening in elite athletes. Clin J Sport Med 14:145–152
Fallon KE (2007) Screening for haematological and iron-related abnormalities in elite athletes—analysis of 576 cases. J Sci Med Sport 30 (in press)
Friedmann B, Weller E, Mairbaurl H, Bartsch P (2001) Effects of iron repletion on blood volume and performance capacity in young athletes. Med Sci Sports Exerc 33:741–746
Landahl G, Adolfsson P, Borjesson M, Mannheimer C, Rodjer S (2005) Iron deficiency and anemia: a common problem in female elite soccer players. Int J Sport Nutr Exerc Metab 15:689–694
Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL (1997) Prevalence of iron deficiency in the United States. JAMA 277:973–976
Malcovati L, Pascutto C, Cazzola M (2003) Hematologic passport for athletes competing in endurance sports: a feasibility study. Haematologica 88:570–581
Malczewska J, Blach W, Stupnicki R (2000a) The effects of physical exercise on the concentrations of ferritin and transferrin receptor in plasma of female judoists. Int J Sports Med 21:175–179
Malczewska J, Raczynski G, Stupnicki R (2000b) Iron status in female endurance athletes and in non-athletes. Int J Sport Nutr Exerc Metab 10:260–276
Malczewska J, Szczepanska B, Stupnicki R, Sendecki W (2001) The assessment of frequency of iron deficiency in athletes from the transferrin receptor-ferritin index. Int J Sport Nutr Exerc Metab 11:42–52
Mercer KW, Densmore JJ (2005) Hematologic disorders in the athlete. Clin Sports Med 24:599–621
Milman N, Byg KE, Ovesen L, Kirchhoff M, Jurgensen KS (2003) Iron status in Danish women, 1984–1994: a cohort comparison of changes in iron stores and the prevalence of iron deficiency and iron overload. Eur J Haematol 71:51–61
Nikolaidis MG, Michailidis Y, Mougios V (2003) Variation of soluble transferrin receptor and ferritin concentrations in human serum during recovery from exercise. Eur J Appl Physiol 89:500–502
Parisotto R, Moutian W, Ashenden MJ, Emslie KR, Gore CJ, Howe C, Kazlauskas R, Sharpe K, Trout GJ, Xie M, Hahn AG (2001) Detection of recombinant human erythropoietin abuse in athletes utilizing markers of altered erythropoiesis. Haematologica 86:128–137
Pedersen BK, Saltin B (2006) Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports 16:3–63
Punnonen K, Irjala K, Rajamaki A (1997) Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood 89:1052–1057
Ramakrishnan U, Frith-Terhune A, Cogswell M, Kettel Khan L (2002) Dietary intake does not account for differences in low iron stores among Mexican American and non-Hispanic white women: Third National Health and Nutrition Examination Survey, 1988–1994. J Nutr 132:996–1001
Roecker L, Meier-Buttermilch R, Brechtel L, Nemeth E, Ganz T (2005) Iron-regulatory protein hepcidin is increased in female athletes after a marathon. Eur J Appl Physiol 95:569–571
Schumacher YO, Schmid A, Konig D, Berg A (2002) Effects of exercise on soluble transferrin receptor and other variables of the iron status. Br J Sports Med 36:195–199
Shaskey DJ, Green GA (2000) Sports haematology. Sports Med 29:27–38
Siega-Riz AM, Hartzema AG, Turnbull C, Thorp J, McDonald T, Cogswell ME (2006) The effects of prophylactic iron given in prenatal supplements on iron status and birth outcomes: a randomized controlled trial. Am J Obstet Gynecol 194:512–519
Sinclair LM, Hinton PS (2005) Prevalence of iron deficiency with and without anemia in recreationally active men and women. J Am Diet Assoc 105:975–978
Stupnicki R, Malczewska J, Milde K, Hackney AC (2003) Day to day variability in the transferrin receptor/ferritin index in female athletes. Br J Sports Med 37:267–269
Thomas L (1998) Transferrin saturation. In: Thomas L (ed) Clinical laboratory diagnostics. TH-books, Frankfurt, pp 275–277
Thomas C, Thomas L (2002) Biochemical markers and hematologic indices in the diagnosis of functional iron deficiency. Clin Chem 48:1066–1076
Verloop J, Rookus MA, van der Kooy K, van Leeuwen FE (2000) Physical activity and breast cancer risk in women aged 20–54 years. J Natl Cancer Inst 92:128–135
Acknowledgments
Financial support was provided by the University of Udine, Udine, Italy; research grant years 2006–2007. We thank Prof. Franco Quadrifoglio, Department Biomedical Sciences and Technologies, University of Udine for a critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Santolo, M., Stel, G., Banfi, G. et al. Anemia and iron status in young fertile non-professional female athletes. Eur J Appl Physiol 102, 703–709 (2008). https://doi.org/10.1007/s00421-007-0647-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-007-0647-9