Abstract
The occurrence of post-exercise hypotension after resistance exercise is controversial, and its mechanisms are unknown. To evaluate the effect of different resistance exercise intensities on post-exercise blood pressure (BP), and hemodynamic and autonomic mechanisms, 17 normotensives underwent three experimental sessions: control (C—40 min of rest), low- (E40%—40% of 1 repetition maximum, RM), and high-intensity (E80%—80% of 1 RM) resistance exercises. Before and after interventions, BP, heart rate (HR), and cardiac output (CO) were measured. Autonomic regulation was evaluated by normalized low- (LFR–Rnu) and high-frequency (HFR–Rnu) components of the R–R variability. In comparison with pre-exercise, systolic BP decreased similarly in the E40% and E80% (−6 ± 1 and −8 ± 1 mmHg, P < 0.05). Diastolic BP decreased in the E40%, increased in the C, and did not change in the E80%. CO decreased similarly in all the sessions (−0.4 ± 0.2 l/min, P < 0.05), while systemic vascular resistance (SVR) increased in the C, did not change in the E40%, and increased in the E80%. Stroke volume decreased, while HR increased after both exercises, and these changes were greater in the E80% (−11 ± 2 vs. −17 ± 2 ml/beat, and +17 ± 2 vs. +21 ± 2 bpm, P < 0.05). LFR–Rnu increased, while ln HFR–Rnu decreased in both exercise sessions. In conclusion: Low- and high-intensity resistance exercises cause systolic post-exercise hypotension; however, only low-intensity exercise decreases diastolic BP. BP fall is due to CO decrease that is not compensated by SVR increase. BP fall is accompanied by HR increase due to an increase in sympathetic modulation to the heart.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-exercise hypotension has been demonstrated after aerobic exercise (Pescatello et al. 2004). In normotensive subjects, it has been attributed to a decrease in cardiac output (CO) and/or systemic vascular resistance (SVR) (Forjaz et al. 2004; Halliwill et al. 1996). Moreover, it has been accompanied by a decrease in peripheral sympathetic activity (Bisquolo et al. 2005; Halliwill et al. 1996), and an increase in cardiac sympathetic activity (Piepoli et al. 1993).
Nowadays, resistance exercise has also been recommended as part of a comprehensive exercise program to reduce cardiovascular risk in general population (American College of Sports Medicine 2000), and in hypertensives (Pescatello et al. 2004). Nevertheless, the cardiovascular effects of this kind of exercise, especially on blood pressure (BP), are not completely understood.
During resistance exercise BP increases expressively (MacDougall et al. 1985). However, after it, BP has been reported to be higher (Brown et al. 1994; Focht and Koltyn 1999; Koltyn et al. 1995; O’Connor et al. 1993), lower (Bermudes et al. 2004; Brown et al. 1994; DeVan et al. 2005; Fisher 2001; Focht and Koltyn 1999; Hardy and Tucker 1998; MacDonald et al. 1999; O’Connor and Cook 1998), or equal (O’Connor et al. 1993; Raglin et al. 1993; Roltsch et al. 2001) to pre-exercise values. Exercise intensity might be responsible for this controversy, since Focht and Koltyn (1999) observed that systolic BP increased after exercise at 80%, but not after exercise at 50% of one repetition maximum (1 RM).
Moreover, to our knowledge, no study investigated the hemodynamic and neural mechanisms responsible for BP response after resistance exercise. As this exercise is accompanied by an important metabolic production (Bush et al. 1999), these metabolites could promote muscle vasodilation, decreasing SVR and BP. In an alternate way, resistance exercise also promotes a decrease in plasma volume (Bush et al. 1999; Collins et al. 1989), which can result in a decrease in stroke volume (SV), CO, and BP. This hypotensive effect might be accompanied by a reflex increase in sympathetic activity to the heart, increasing heart rate (HR) (Bermudes et al. 2004; DeVan et al. 2005; Focht and Koltyn 1999; MacDonald et al. 1999; O’Connor et al. 1993). These hypotheses need to be tested.
The aim of the present study was to evaluate the effect of a single bout of different resistance exercise intensities on BP, and its hemodynamic and neural mechanisms. Although post-exercise hypotension might have clinical relevance in hypertensives, the study was conducted with healthy subjects in order to understand its physiology without pathological influences.
Materials and methods
Subjects
Seventeen young healthy subjects gave written consent to take part in the study, which was approved by the Ethics Committee of the General Hospital of Medical School, University of São Paulo, Brazil.
Subjects who presented any cardiovascular abnormality in resting or exercise ECG, mean resting systolic/diastolic BP ≥140/90 mmHg, and/or body mass index ≥30 kg/m2 were excluded. None of the subjects exercised regularly. The characteristics of the subjects are shown in Table 1.
Experimental protocol
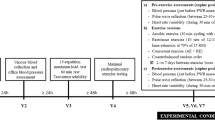
At least 7 days prior to the experiments, subjects underwent a 1 RM test for the bench press, 70° hip angle leg-press, lat pull down, leg curl, biceps curl, and 40° hip angle leg-press, using Kraemer and Fry’s protocol (Kraemer and Fry 1995). Before the test, they underwent four familiarization sessions (3 sets, 20 repetitions of each exercise with the minimum weight allowed by the machines) in non-consecutive days.
All subjects underwent, in a random order, three experimental sessions: control (C), exercise at 40 (E40%), and 80% (E80%) of 1 RM. Sessions were initiated between 1 and 3 p.m., and had an interval of at least 7 days. Subjects were instructed to take a light meal 2 h before the experiments, to avoid physical exercise and alcohol for at least the prior 48 h, and to avoid smoking, caffeine, and medications for 12 h.
In each session, subjects rested in the seated position for 20 min (pre-intervention period). Then they moved to the exercise room, where they remained for about 40 min: resting in the C session, and exercising in the E sessions. Subjects were blinded to which sessions they were going to perform until the exercise or the rest began. In E40%, subjects performed 3 sets of 20 repetitions of the 6 exercises cited above, with a workload corresponding to 40% of 1 RM, and an interval of 45 s between the sets and 90 s between the exercises. In E80%, they performed 3 sets of 10 repetitions with a workload corresponding to 80% of 1 RM, with an interval of 60 s between sets and 90 s between the exercises. Afterwards, subjects returned to the laboratory, where they rested in the sitting position for 90 min (post-intervention period). Air temperature was kept between 20 and 22°C. Hemodynamic data were measured in duplicate pre-intervention, and at 15, 30, 60, and 90 min of the post-intervention period. A mean value was calculated for each moment. Moreover, ECG and respiratory data were collected for autonomic assessment during 10 min pre-interventions and at 20, 40, and 65 min post-interventions.
Measurements
Auscultatory BP was measured immediately before CO determination. The mean differences between duplicated measurements were 3.13 ± 0.18 and 2.91 ± 0.15 mmHg for systolic and diastolic BP, respectively, showing that measurement was accurate (O’Brien et al. 2002). Mean BP was calculated by the sum of DBP and one third of pulse pressure. ECG was continuously monitored (TEB, M-10) and HR was registered immediately after BP measurement.
Cardiac output was estimated by the indirect Fick method of CO2 rebreathing (Jones et al. 1967), using a metabolic cart (MGC, CAD/NET 2001). Briefly, subjects breathed spontaneously until a steady CO2 production was achieved. This procedure was followed by the rebreathing of a mixed gas with a high CO2 concentration (8–10%) and 35% O2 until equilibrium was achieved (maximal of 15 s). At this moment, CO was calculated by the Fick formula. SVR was calculated by the quotient of mean BP and CO, and SV by the quotient of CO and HR.
For autonomic evaluation, ECG (TEB, D10) and respiratory activity (thoracic belt-UFI, Pneumotrace II) were recorded for 10 min with a sample frequency of 500 Hz per channel. A derivated-threshold algorithm provided the series of R–R intervals from ECG, and the signal of respiratory activity was sampled once for every cardiac cycle. An autoregressive spectral analysis of R–R variability was performed, and its theoretical and analytical procedures have been described before (Task Force 1996). Briefly, on stationary segments of the time series, with at least 150 points (Task Force 1996), autoregressive parameters were estimated by the Levinson–Durbin recursion, and the order of the model was chosen according to Akaike’s criterion (Malliani et al. 1991). An autoregressive spectral decomposition was then performed. The components were assigned based on their central frequency as low- (LFR–R—0.04–0.15 Hz) and high-frequency (HFR–R—0.15–0.5 Hz) components, and HF power was considered in dependence to a significant coherence with respiratory spectrum. HFR–R and LFR–R components were reported in normalized units (nu), which represent the relative value of each power component in proportion to the total power minus very low-frequency component (VLF—0–0.04 Hz). Normalized LHR–R and HFR–R components of R–R variability were accepted, respectively, as markers of the cardiac sympathetic and parasympathetic modulations (Task Force 1996).
Statistical analysis
Changes in hemodynamic and autonomic parameters in each experimental session were calculated by the difference in values measured in the post- and pre-intervention periods. These changes were compared by a two-way analysis of variance ANOVA for repeated measures (STATISTICA FOR WINDOWS 4.3, Statsoft Inc., 1993, Tulsa, OK, USA), with sessions (C, E40%, and E80%) and stages (pre and 15, 30, 60, and 90 min or pre and 20–30, 40–50, and 65–75 min after exercise) as main factors. The Gaussian distribution of the data was verified by the Shapiro–Wilk test, and a natural logarithmic (ln) transformation was employed when necessary (for HFnu and LF/HF). Post-hoc comparisons were done by Newman–Keuls test. P < 0.05 was accepted as statistically significant. Data are presented as means ± SE.
Results
Six subjects initiated the protocol with the C session, six with E40%, and five with E80%. The workloads corresponding to 40 and 80% of 1 RM were, respectively, 25 ± 3 and 50 ± 6 kg for bench press, 41 ± 3 and 82 ± 6 kg for 70° hip angle leg-press, 22 ± 2 and 42 ± 4 kg for lat pull down, 12 ± 1 and 23 ± 2 kg for leg curl, 8 ± 1 and 16 ± 2 kg for biceps curl, and 29 ± 2 and 57 ± 4 kg for 40° hip angle leg-press. Moreover, in eight subjects, HR was monitored during exercise (Polar, S810), and the maximal values achieved during exercise at 40 and 80% of 1 RM were, respectively, 132 ± 3 and 136 ± 4, 122 ± 3 and 152 ± 6, 132 ± 6 and 161 ± 4, 151 ± 6 and 156 ± 7, 164 ± 5 and 169 ± 5, and 135 ± 4 and 163 ± 4 beat/min for the bench press, 70° hip angle leg-press, lat pull down, leg curl, biceps curl, and 40° hip angle leg-press.
Pre-intervention data
Hemodynamic and autonomic data measured before the interventions in all the experimental sessions are shown in Table 2. Pre-intervention systolic and mean BPs were significantly higher in the E40% than in the C session. Moreover, pre-intervention SVR was also significantly higher in the E40% than in the E80% session. All the other parameters were similar among the experimental sessions.
Hemodynamic data
Systolic, mean, and diastolic BP changes observed in all the experimental sessions are shown in Fig. 1. In comparison with the pre-intervention values, systolic BP did not change in the C session, and decreased similarly during all the recovery periods after exercise in the E40% and E80% sessions (−6 ± 1 and −8 ± 1 mmHg, respectively, P < 0.05). Diastolic BP increased after intervention in the C session (+5 ± 1 mmHg, P < 0.05), did not change in the E80% session, and decreased at 15 and 30 min after exercise in the E40% session (−4 ± 1 mmHg, P < 0.05). Mean BP increased 90 min after intervention in the C session (+3 ± 1 mmHg, P < 0.05), decreased at 60 min (−3 ± 1 mmHg, P < 0.05), and at 30–60 min (−4 ± 1 and −4 ± 1 mmHg, P < 0.05) after intervention in the E80% and E40% sessions, respectively.
Changes in systolic (SBP panel a), diastolic (DBP panel b), and mean (MBP panel c) blood pressures observed in 17 subjects after interventions in the control (C circles), resistance exercise at 40% of 1 RM (E40% squares), and resistance exercise at 80% of 1 RM (E80% triangles) sessions. *Significantly different from pre-intervention (P < 0.05). †Significantly different from the control session (P < 0.05). ‡Significantly different from the E80% session (P < 0.05)
Cardiac output, SVR, SV, and HR changes observed after interventions in the experimental sessions are shown in Fig. 2. In comparison with the pre-intervention values, CO decreased similarly after interventions in all the experimental sessions, while SVR increased after 60 min of the post-intervention period in the C session (+7 ± 2 mmHg min/l, P < 0.05), did not change in the E40% session, and increased at 15 and 30 min after exercise in the E80% session (+5 ± 2 mmHg min/l, P < 0.05).
Changes in cardiac output (CO panel a), systemic vascular resistance (SVR panel b), stroke volume (SV panel c), and heart rate (HR panel d) observed in 17 subjects after interventions in the control (C circles), resistance exercise at 40% of 1 RM (E40% squares), and resistance exercise at 80% of 1 RM (E80% triangles) sessions. *Significantly different from pre-intervention (P < 0.05). †Significantly different from the control session (P < 0.05). ‡Significantly different from the E80% session (P < 0.05)
In comparison with the pre-intervention values, SV did not change in the C session, but decreased after intervention in the E40% and E80% sessions. Moreover, at 15 min of the post-intervention period, SV fall was greater in the E80% than the E40% session (−17 ± 2 vs. −11 ± 2 ml, respectively, P < 0.05).
In comparison with the pre-intervention values, HR decreased throughout the post-intervention period in the C session (−7 ± 2 beat/min, P < 0.05), and increased significantly in the exercise sessions. Moreover, HR increase observed 15 min after exercise was greater in the E80% than E40% session (+21 ± 2 vs. +17 ± 2 beat/min, P < 0.05).
Autonomic data
Indexes of autonomic activity changes observed after intervention in all the experimental sessions are shown in Table 3. Because of technical problems, autonomic data were assessed only in eight subjects. In comparison with the pre-intervention values, R–R interval did not change in the C session, but decreased significantly throughout the recovery period in the E40% session, and until 50 min of recovery in the E80% sessions. LFR–Rnu, ln HFR–Rnu, and ln LF/HF did not change in the C session, but ln HFR–Rnu decreased, while LFR–Rnu and ln LF/HF increased similarly after exercise in the E40% and E80% sessions.
Discussion
The main findings of this study are: (a) a single bout of low- and high-intensity resistance exercise decreased post-exercise systolic BP; however, only low-intensity exercise decreased diastolic BP; (b) independent of the exercise intensity, post-resistance exercise hypotension was due to a decrease in CO which was not completely compensated by an increase in SVR; (c) CO decrease was mediated by a decrease in SV, which was accompanied by an incomplete rise in HR, promoted by cardiac sympathetic activation and parasympathetic deactivation.
In keeping with some previous studies (Bermudes et al. 2004; Brown et al. 1994; DeVan et al. 2005; Fisher 2001; Focht and Koltyn 1999; Hardy and Tucker 1998; MacDonald et al. 1999; O’Connor and Cook 1998), the present investigation showed that resistance exercise promoted post-exercise hypotension in normotensive subjects. The magnitude of systolic BP fall varies extremely among previous studies (from 3 to 20 mmHg). In the present study, systolic BP falls were similar between exercises at low- and high-intensities (−6 ± 1 and −8 ± 1 mmHg, respectively); they were similar to the ones usually reported after aerobic exercise (Pescatello et al. 2004), and lasted for at least 90 min.
In regard to diastolic BP, a significant fall in comparison with pre-exercise values was observed only after low-intensity resistance exercise. However, in the E80% session, diastolic BP did not rise as observed in the C session, showing that high-intensity resistance exercise also had diastolic hypotensive effect. Nevertheless, this effect was lower than the one observed after low-intensity exercise.
To our knowledge, this is the first study to address hemodynamic and neural mechanisms after resistance exercise. It was interesting that CO decreased similarly in all the sessions, including the C session. However, in the C session, CO decrease was due to a slight reduction in HR, and a non-significant decrease in SV. The slight reduction of HR was not observed when R–R interval was evaluated, which might be explained by the different number of subjects applied for the R–R analysis and/or by the different conditions of measurement. The absence of change in the cardiac autonomic indexes of R–R interval variability is in accordance with the R–R interval response. Moreover, in the C session, CO decrease was compensated by an increase in SVR, which explains the increase in diastolic BP and the absence of changing in systolic BP. These hemodynamic responses in resting condition might seem odd at first. Nevertheless, they were also observed by others (Forjaz et al. 2004; Gotshall et al. 1994; Raglin and Morgan 1987), and might be related to the orthostatic stress produced by the sitting position (Gotshall et al. 1994). This position might have decreased venous return, deactivating cardiopulmonary baroreflex and increasing, consequently, SVR and DBP (Mark and Mancia 1996).
Systemic hemodynamics after resistance exercise were different from the C session, and were influenced by the exercise intensity. After low-intensity exercise, CO decrease was not accompanied by an increase in SVR, which explains the fall in both systolic and diastolic BPs. However, after exercise at 80% of 1 RM, SVR presented an increase at the beginning of the recovery and maintenance afterwards, which explains the decrease in systolic, but not in diastolic BP.
After both exercise sessions, CO decrease was mediated by a reduction in SV, which could be explained by a decrease in cardiac contractility, an increase in afterload and/or a reduction in pre-load. Nevertheless, a decrease in cardiac contractility is not likely, since it has only been reported after extremely extenuating dynamic exercises, such as a 24-h run (Niemela et al. 1984) or exercise bout to exhaustion (Seals et al. 1988), which was not the case of the present exercise sessions. The increase in afterload might explain, in part, the SV fall at 15 min after exercise at 80% of 1 RM because, at this moment, SVR was increased. However, it could not explain SV decrease in the E40% session. Thus, a decrease in pre-load is the most plausible mechanism to explain the reduction in SV after resistance exercise because plasma volume is reduced by a shift of plasma liquid from blood to the interstitial space (Bush et al. 1999; Collins et al. 1989). As the magnitude of this plasma reduction is greater after more intense exercise (Collins et al. 1989), this mechanism is also in accordance with the greater SV fall observed after exercise at 80% than 40% of 1 RM.
The decrease in plasma volume and consequently, in venous return, may also be involved in SVR responses observed after resistance exercises. This decrease might deactivate cardiopulmonary receptors, increasing peripheral sympathetic activity and SVR (Rowell et al. 1996). This effect was especially evident at the beginning of the recovery period in the E80% of 1 RM session, when plasma volume decrease was probably maximized. However, other vasoconstrictor mechanisms activated by plasma volume decreases, such as renin–angiotensin–aldosterone system (Convertino 1987), might also be involved. These mechanisms were not addressed in the present study.
After both exercise sessions, SV decreases were accompanied by HR increases, which were not big enough to compensate SV decreases, resulting in CO reductions. It is important to state, however, that post-exercise increase of HR was reported in comparison with pre-exercise levels, and it really represents the delay of HR to return to pre-exercise values after being elevated during exercise. This increase in HR after resistance exercise has already been reported by others (Bermudes et al. 2004; DeVan et al. 2005; Focht and Koltyn 1999; MacDonald et al. 1999; O’Connor et al. 1993). Nevertheless, this is the first time that it is shown that HR increase after resistance exercise was mediated by an increase in sympathetic and a decrease in parasympathetic modulation of the heart, as set by the increase in LFR–Rnu and ln LF/HFR–R, and decrease in ln HFR–Rnu components. These autonomic responses might be mediated by baroreflex control evoked by BP decrease observed after exercise (Halliwill et al. 1996).
It is important to note that post-exercise measurements were taken after subjects walked back from the exercise to the laboratory room, and this procedure might have influenced post-exercise hemodynamic results at 15 min of recovery. Nevertheless, as this procedure took less than 30 s, and it was also followed in the C session, any possible influence was minimized.
Based on previous comments, it is possible to point out that exercise intensity is an important factor determining the hemodynamic responses after resistance exercise. Low-intensity exercise promoted greater hypotensive effect than the higher intensity one, especially on diastolic BP, because it did not increase SVR to compensate CO decrease. Nevertheless, CO decreases were similar between different exercise intensities, although SV reductions were greater after the high-intensity exercise. These responses might be attributed to the lower deactivation of cardiopulmonary reflex produced by low-intensity exercise, which resulted in a lower increase in SVR.
Study limitations
This study included men and women. It is known that gender might influence hemodynamic and neural responses in certain situations. However, a complementary statistical analysis, including gender as a between-group main factor, found no difference between men and women.
Subjects presented higher systolic BP, and consequently higher mean BP and SVR in the pre-intervention period of the E40% session. Nevertheless, these differences were small and within the measurement error (O’Brien et al. 2002). Thus, they should not have interfered with results. Besides that, as the objective was to compare the responses after exercise, the calculation of the differences between post- and pre-intervention values decreases any possible influence.
The interpretation of LFR–R as the sympathetic modulation of the heart has some controversy. However, when normalized units are employed, it is assumed that this band is predominantly representative of sympathetic modulation (Task Force 1996). Moreover, as we observed a decrease in ln HFR–Rnu, and an increase in LFR–Rnu and ln LF/HF, this pattern of response undoubtedly indicates sympathetic predominance.
Conclusion
Low- and high-intensity resistance exercises promote systolic post-exercise hypotension in normotensive subjects, while only low-intensity exercise decreases diastolic BP. After both exercise intensities, BP decrease was due to a reduction in CO that is not completely compensated by an increase in SVR. CO reduction is due to a decrease in SV besides the increase in HR promoted by the activation of sympathetic and deactivation of parasympathetic modulation of the heart.
References
American College of Sports Medicine (2000) ACSM’s guidelines for exercise testing and prescription. Lippincott Williams and Wilkins, Philadelphia
Bermudes AM, Vassallo DV, Vasquez EC, Lima EG (2004) Ambulatory blood pressure monitoring in normotensive individuals undergoing two single exercise sessions: resistive exercise training and aerobic exercise training. Arq Bras Cardiol 82:65–71, 57–64
Bisquolo VA, Cardoso CG Jr, Ortega KC, Gusmao JL, Tinucci T, Negrao CE, Wajchenberg BL, Mion D Jr, Forjaz CL (2005) Previous exercise attenuates muscle sympathetic activity and increases blood flow during acute euglycemic hyperinsulinemia. J Appl Physiol 98:866–871
Brown SP, Clemons JM, He Q, Liu S (1994) Effects of resistance exercise and cycling on recovery blood pressure. J Sports Sci 12:463–468
Bush JA, Kraemer WJ, Mastro AM, Triplett-McBride NT, Volek JS, Putukian M, Sebastianelli WJ, Knuttgen HG (1999) Exercise and recovery responses of adrenal medullary neurohormones to heavy resistance exercise. Med Sci Sports Exerc 31:554–559
Collins MA, Cureton KJ, Hill DW, Ray CA (1989) Relation of plasma volume change to intensity of weight lifting. Med Sci Sports Exerc 21:178–185
Convertino VA (1987) Fluid shifts and hydration state: effects of long-term exercise. Can J Sport Sci 12:136S–139S
DeVan AE, Anton MM, Cook JN, Neidre DB, Cortez-Cooper MY, Tanaka H (2005) Acute effects of resistance exercise on arterial compliance. J Appl Physiol 98:2287–2291
Fisher MM (2001) The effect of resistance exercise on recovery blood pressure in normotensive and borderline hypertensive women. J Strength Cond Res 15:210–216
Focht BC, Koltyn KF (1999) Influence of resistance exercise of different intensities on state anxiety and blood pressure. Med Sci Sports Exerc 31:456–463
Forjaz CL, Cardoso CG Jr, Rezk CC, Santaella DF, Tinucci T (2004) Postexercise hypotension and hemodynamics: the role of exercise intensity. J Sports Med Phys Fitness 44:54–62
Gotshall RW, Aten LA, Yumikura S (1994) Difference in the cardiovascular response to prolonged sitting in men and women. Can J Appl Physiol 19:215–225
Halliwill JR, Taylor JA, Eckberg DL (1996) Impaired sympathetic vascular regulation in humans after acute dynamic exercise. J Physiol 495(Pt 1):279–288
Hardy DO, Tucker LA (1998) The effects of a single bout of strength training on ambulatory blood pressure levels in 24 mildly hypertensive men. Am J Health Promot 13:69–72
Jones NL, Campbell EJ, McHardy GJ, Higgs BE, Clode M (1967) The estimation of carbon dioxide pressure of mixed venous blood during exercise. Clin Sci 32:311–327
Koltyn KF, Raglin JS, O’Connor PJ, Morgan WP (1995) Influence of weight training on state anxiety, body awareness and blood pressure. Int J Sports Med 16:266–269
Kraemer WJ, Fry AC (1995) Strength testing: development and evaluation of methodology. In: Maud PJ, Foster C (eds) Physiological assessment of human fitness. Human Kinetics, Champaign, pp. 115–138
MacDonald JR, MacDougall JD, Interisano SA, Smith KM, McCartney N, Moroz JS, Younglai EV, Tarnopolsky MA (1999) Hypotension following mild bouts of resistance exercise and submaximal dynamic exercise. Eur J Appl Physiol Occup Physiol 79:148–154
MacDougall JD, Tuxen D, Sale DG, Moroz JR, Sutton JR (1985) Arterial blood pressure response to heavy resistance exercise. J Appl Physiol 58:785–790
Malliani A, Pagani M, Lombardi F, Cerutti S (1991) Cardiovascular neural regulation explored in the frequency domain. Circulation 84:482–492
Mark AL, Mancia G (1996) Cardiopulmonary baroreflex in humans. In: Rowell LB, Shepherd JT (eds) Handbook of physiology: a critical, comprehensive presentation of physiological knowledge and concepts. Oxford University Press, New York, pp 795–813
Niemela KO, Palatsi IJ, Ikaheimo MJ, Takkunen JT, Vuori JJ (1984) Evidence of impaired left ventricular performance after an uninterrupted competitive 24 hour run. Circulation 70:350–356
O’Brien E, Pickering T, Asmar R, Myers M, Parati G, Staessen J, Mengden T, Imai Y, Waeber B, Palatini P, Gerin W (2002) Working Group on Blood Pressure Monitoring of the European Society of Hypertension International Protocol for validation of blood pressure measuring devices in adults. Blood Press Monit 7:3–17
O’Connor PJ, Cook DB (1998) Anxiolytic and blood pressure effects of acute static compared to dynamic exercise. Int J Sports Med 19:188–192
O’Connor PJ, Bryant CX, Veltri JP, Gebhardt SM (1993) State anxiety and ambulatory blood pressure following resistance exercise in females. Med Sci Sports Exerc 25:516–521
Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA (2004) American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc 36:533–553
Piepoli M, Coats AJ, Adamopoulos S, Bernardi L, Feng YH, Conway J, Sleight P (1993) Persistent peripheral vasodilation and sympathetic activity in hypotension after maximal exercise. J Appl Physiol 75:1807–1814
Raglin JS, Morgan WP (1987) Influence of exercise and quiet rest on state anxiety and blood pressure. Med Sci Sports Exerc 19:456–463
Raglin JS, Turner PE, Eksten F (1993) State anxiety and blood pressure following 30 min of leg ergometry or weight training. Med Sci Sports Exerc 25:1044–1048
Roltsch MH, Mendez T, Wilund KR, Hagberg JM (2001) Acute resistive exercise does not affect ambulatory blood pressure in young men and women. Med Sci Sports Exerc 33:881–886
Rowell LB, O’Leary D, Kellogg DL Jr (1996) Integration of cardiovascular control systems in dynamic exercise. In: Rowell LB, Shepherd JT (eds) Handbook of physiology: a critical, comprehensive presentation of physiological knowledge and concepts. Oxford University Press, New York, pp 770–838
Seals DR, Rogers MA, Hagberg JM, Yamamoto C, Cryer PE, Ehsani AA (1988) Left ventricular dysfunction after prolonged strenuous exercise in healthy subjects. Am J Cardiol 61:875–879
Task Force of the European Society of Cardiology, the North American Society of Pacing Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93:1043–1065
Acknowledgments
We gratefully acknowledge the volunteers involved in this study. We also thank Alberto Porta for providing the software for spectral analysis, and Mariana Curi for statistical support. Cláudio C. Rezk works at Centro Universitário FIEO and Universidade Santo Amaro. Regina C.B. Marrache works at Instituto de Cardiologia Dante Pazzanese. This study was supported by FAPESP (01/01952-8) and CAPES (Demanda Social).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rezk, C.C., Marrache, R.C.B., Tinucci, T. et al. Post-resistance exercise hypotension, hemodynamics, and heart rate variability: influence of exercise intensity. Eur J Appl Physiol 98, 105–112 (2006). https://doi.org/10.1007/s00421-006-0257-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-006-0257-y