Abstract
The aim of this study was to determine whether 4 weeks of inspiratory muscle training (IMT) would be accompanied by alteration in cardiopulmonary fitness as assessed through moderate intensity oxygen uptake (V̇O2) kinetics and maximal aerobic power (V̇O2max). Eighteen healthy males agreed to participate in the study [training group (Tra) n=10, control group (Con) n=8]. Measurements of spirometry and maximal static inspiratory mouth pressure (PImax) were taken pre- and post-training in addition to: (1) an incremental test to volitional exhaustion, (2) three square-wave transitions from walking to running at a moderate intensity (80% ventilatory threshold) and (3) a maximal aerobic constant-load running test to volitional fatigue for the determination of time to exhaustion (Tlim). Training was performed using an inspiratory muscle trainer (Powerbreathe). There were no significant differences in spirometry either between the two groups or when comparing the post- to pre-training results within each group. Mean PImax increased significantly in Tra (P<0.01) and showed a trend for improvement (P<0.08) in Con. Post-training Tlim was significantly extended in both Tra [232.4 (22.8) s and 242.8 (20.1) s] (P<0.01) and Con [224.5 (19.6) and 233.5 (12.7) s] (P<0.05). Post-training Tlim was significantly extended in Tra compared to Con (P<0.05). In conclusion, the most plausible explanation for the stability in V̇O2 kinetics and V̇O2max following IMT is that it is due to insufficient whole-body stress to elicit either central or peripheral cardiopulmonary adaptation. The extension of post-training Tlim suggests that IMT might be useful as a stratagem for producing greater volumes of endurance work at high ventilatory loads, which in turn could improve cardiopulmonary fitness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been proposed that inspiratory muscle training (IMT) has a positive effect on cardiopulmonary fitness during prolonged exercise performance in healthy subjects (Spengler et al. 1999; Volianitis et al. 2001). However, this observation appears controversial (Inbar et al. 2000) as the mechanisms by which training of the inspiratory muscles might stimulate exercise performance are unclear, and research indicates that respiratory muscle training is not associated with changes to maximal stroke volume or cardiac output (Markov et al. 2001).
Several studies have reported that decreasing the work of breathing leads to significantly longer exercise tolerance which is associated with a reduced rate of oxygen uptake (V̇O2), ventilation and reduced perceptions of respiratory and limb discomfort (Harms et al. 1998, 2000). This suggests that the work of breathing normally encountered during sustained heavy exercise has a significant influence on exercise performance, possibly due to diaphragmatic fatigue or a higher distribution of blood flow to the working muscles as a consequence of enhanced respiratory efficiency (Harms et al. 1997; Johnson et al. 1993; Mador et al. 1993).
Enhanced cardiopulmonary function is commonly associated with improved performance in appropriately designed tests of cardiopulmonary fitness. Several studies have measured maximal aerobic power (V̇O2max) following IMT, but have not reported significant gains (Fairbarn et al. 1991; Inbar et al. 2000; Markov et al. 2001; Morgan et al. 1987; Spengler et al. 1999).
Both V̇O2 kinetics and V̇O2max have been shown to improve in response to endurance training (Carter et al. 2000; Fukuoka et al. 1997; Phillips et al. 1995) and the two measurements are also known to be enhanced in well-trained endurance athletes (Edwards et al. 2003; Saltin and Astrand 1967). Growing evidence suggests that the two measurements represent different components of cardiopulmonary fitness (Bassett and Howley 1997; Grassi et al. 1996; Rossiter et al. 1999), where the kinetics of V̇O2 at the onset exercise have been shown to closely reflect the kinetics of phosphocreatine hydrolysis (Rossiter et al. 1999) and muscle oxygen consumption (Grassi et al. 1996), while limitations in the transport of oxygen to the working muscles have routinely been proposed as controlling mechanisms for V̇O2max in healthy subjects (Bassett and Howley 1997; Wagner 1996).
V̇O2 kinetics and V̇O2max are known to be interrelated; however, Powers et al. (1985) reported a relatively low coefficient of determination between the two measures (R2=0.64), which further supports the view that they are reflective of different components of cardiopulmonary fitness. As changes in cardiopulmonary fitness are routinely detected through individual responses to appropriately designed fitness tests, the role of IMT has therefore been assessed in terms of whether there is a functional change in V̇O2max and V̇O2 kinetics in healthy subjects undertaking this form of training.
Methods
Subjects
Eighteen healthy male subjects agreed to participate in the study (Table 1.). All participants had normal spirometry and were physically active. All subjects were informed of the procedures in advance of the study and informed consent was provided prior to any data collection in accordance with the Institution’s Research Ethics Committee. The subjects were assigned into two groups one being the training group (Tra n=10) and the other a control group (Con n=8) group.
The tests were performed at similar times of the day and were conducted in the same routine order prior to and following 4 weeks of training. All subjects were required to continue their habitual physical activity patterns over the 4 weeks training period.
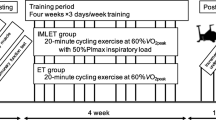
Experimental design
At the beginning of the study, maximal static inspiratory mouth pressure (PImax) was measured using a portable hand held mouth pressure meter (Precision Medical, London, UK) and baseline spirometry measurements were recorded [forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), maximal voluntary ventilation (MVV)] (Vitalograph, Compact, Buckingham, UK). These measures were followed by an incremental test to volitional exhaustion on a treadmill (Woodway PPS 55, Germany) for the combined assessment of maximal aerobic power and ventilatory threshold (Tvent).
On a subsequent occasion, all subjects completed three square-wave exercise transitions from walking at 4 km h−1 for 4 min to running for 6 min at a moderate intensity (80% Tvent) for the assessment of moderate intensity V̇O2 kinetics. Following a rest of 1 h, all subjects completed a constant-load exercise test to examine time to exhaustion (Tlim). The maximal running velocity and incline of the Tlim test utilised the maximal velocity and incline attained by each subject in the initial assessment of V̇O2max. In the Tlim test, the maximal velocity and incline were attained progressively over 30 s as a ramp function and followed a 5 min warm-up at 65% Tvent. Subjects were unaware of test duration and therefore could not make a judgement as to when to conclude the test. Tlim was identified as the time taken (seconds) to reach volitional fatigue. All subjects completed post-test questionnaires for the analysis of perceptual discomfort at maximal exercise intensity using a Borg scale (Borg 1982).
Inspiratory muscle training
Both groups performed 30 inspiratory efforts daily using an inspiratory muscle trainer (POWERbreathe, MT Technologies, Birmingham, UK). Tra were required to complete 30 maximal breaths while Con also inspired 30times, but at a resistance equivalent to 15% of maximum effort using the POWERbreathe device. The use of negligible inspiratory resistance has been used as a control measure in other studies (Volianitis et al. 2001), and is thought to elicit only a minor training effect (Romer and McConnell 2003).
Measurement of gas exchange parameters
For all exercise trials, gas exchange and minute ventilation were continuously measured breath-by-breath at the mouth. Gases were continuously drawn through a capillary line and analysed for oxygen and carbon dioxide concentrations by fast-response analysers utilising principles of electrochemical reactions for the detection of oxygen and absorption by carbon dioxide of appropriate wavelengths of infrared light (Cortex 3B Metalyser, Cortex Biophysik, Germany). The system was calibrated before and verified after each test with standard calibration gases. Expired volume was measured by a volume-measuring turbine, which was calibrated with a 3 l syringe (Hans Rudolph, Kansas City, Mo.). Non-physiological background ‘noise’ was smoothed from the breath-by-breath data by the use of a 5-breath average.
Data analysis of V̇O2 kinetics
Breath-by-breath data for the three repetitions of the square-wave exercise transitions were linearly interpolated at 1-s intervals, time aligned to the start of exercise and ensemble-averaged to yield a single data set per subject.
The kinetic parameters of amplitude, time delay (δ) and time constant (τ) were identified from a mono exponential model of the V̇O2–time relationship in the on-transient (Whipp et al. 1982). A mean response time (MRT) was calculated to represent time constant and delay (δ+τ). The initial 20 s of the response was removed from the data set to eliminate the contribution of the cardiodynamic phase which is not associated with muscle V̇O2 (Hughson and Morrissey 1982; Whipp et al. 1982).
Blood lactate
Arterialised capillary whole-blood samples were taken from the finger tip prior to and at the end of each maximal exercise test. Analysis was performed with an Analox GM7 Multi Assay analyser (Analox, London, UK).
Statistical analysis
The statistical software package SPSS (version 10.0, SPSS, Chicago, Ill.) was used for all statistical analysis. Pre- and post-training results and group interactions were statistically compared using one-way or two-way repeated measures analyses of variance and post-hoc Tukey tests of honest significant difference as appropriate. Other group comparisons were made using paired Student’s t-tests. The relationships between data sets were examined using Pearson product moment correlations. Probability values of less than 0.05 were considered significant. All results are expressed in means (SD) unless otherwise stated.
Results
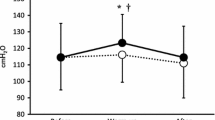
There were no significant differences in FVC, FEV1 or MVV either between the two groups of subjects or within each group pre- to post-training (Table 1). Mean PImax increased significantly in the Tra group (P<0.01) and showed a trend for improvement (P<0.08) in the Con group (Fig. 1). Following statistical analysis, there were no significant relationships between spirometry and PImax.
The results of the post training tests of V̇O2 kinetics and V̇O2max showed there were no significant differences in the two cardiopulmonary fitness measurements for either Tra or Con (Table 2). However, both groups were able to maintain maximal constant-load treadmill running in the Tlim test for a significantly extended duration following the training period (Fig. 1.). The statistical significance of this observation was strongest in Tra (P<0.01), although this effect was also significant in Con, albeit at a lower level (P=0.048, P<0.05) (Table 2). Post-training Tlim was significantly extended in Tra compared with Con (P<0.05). There were no differences between perceptions of maximal effort across the testing conditions.
Maximal blood lactate concentrations following V̇O2max assessment were not significantly different between Tra and Con either before training [8.5 (1.4) and 8.4 (0.9) mmol l−1 respectively] or following 4 weeks of IMT training [8.3 (1.2) and 8.4 (1.1) mmol l−1 respectively]. The maximal blood lactate concentrations following Tlim testing were also unaffected by IMT training and also showed no difference between the two groups (Fig. 2). Mean blood lactate concentrations showed a tendency for lower peak values post training in Tra and higher peak values in Con, but this was not a significant observation.
Significant correlations were observed between V̇O2 kinetics and V̇O2max pre- (r=−0.78) (P<0.01, Fig. 3A) and post-training (r=−0.66) (P<0.01, Fig. 3B). Coefficients of determination show that MRT is significantly dependent on V̇O2max pre- (61%) and post-training (44%). Tlim did not significantly correlate with either the mean response time of V̇O2 kinetics and V̇O2max.
Maximal ventilatory measurements for V̇O2max [expiratory flow (V̇E) and V̇E/V̇O2] were unchanged from pre- [Tra 113.6 (7.7) and 28.5 (1.1) l min−1; Con 117.9 (8.6) and 29.4 (1.8) l min−1] to post-training [Tra 111.4 (8.5) and 27.6 (1.1) l min−1; Con 119.6 (8.3) and 29.9 (1.4) l min−1]. The significant extension of Tlim observed in both groups was not supported by changes in the ventilatory measures V̇E and V̇E/V̇O2 from pre- [Tra 109.9 (7.6) and 27.8 (1) l min−1; Con 114.4 (6.3) and 28.7 (1.4) l min−1] to post-training [Tra 107.6 (8.7) and 26.9 (0.9) l min−1; Con 112.8 (8.1) and 28.3 (1.2) l min−1], although there was a trend for lower maximal V̇E in Tlim compared with V̇O2max in Tra (P=0.09).
Discussion
The results of the present study have shown that Tlim is significantly extended following IMT, but this performance gain is not supported by alteration in either V̇O2 kinetics or V̇O2max as indicators of cardiopulmonary fitness.
V̇O2 in muscle is known to rapidly adjust to short-term training in humans (Berry and Moritani 1985; Cadefau et al. 1994; Green et al. 1995; Phillips et al. 1995) and V̇O2 kinetics have previously been shown to improve after as little as 4 days of whole-body endurance training (2 h per day at 60% pre-training peak V̇O2) (Phillips et al. 1995). However, as a sole stratagem, IMT appears unlikely to be a sufficient stimulus to improve whole-body cardiopulmonary fitness in healthy subjects.
The most plausible cause of the observed stability in V̇O2 kinetics across the training period is the minimal cardiopulmonary stimulation of this form of training. Greater respiratory efficiency might lead to a greater availability of oxygen for the working limb muscles, but oxygen transport limitations have not consistently proved influential in the assessment of V̇O2 kinetics. Speeded V̇O2 kinetics would, more likely, be dependent on direct influence on mitochondrial enzyme activation and/or the concentrations of putative cellular metabolic controllers at the working muscles (Grassi et al. 1996).
It is possible that a training effect could be disguised within breath-by-breath variability as this is known to be dependent on the algorithm used for the expression of alveolar gas exchange (Capelli et al. 2001). In this study, oxygen transfer was measured at the mouth and estimation was not made of alveolar gas exchange. The assessment of oxygen transfer at the mouth could lead to greater breath-by-breath variability and artificially long time constants of the V̇O2 on-responses; however, provided sufficient repetitions of the square wave exercise transition are performed and averaged, the noise due to random changes of V̇E is greatly reduced. Therefore, even though the precise time course of the alveolar oxygen transfer at the alveolar level was not estimated, our data suggest that it was not affected by IMT.
The significant relationships between MRT and V̇O2max max pre- (r=0.78) and post-training (r=0.66) (Fig. 3.) support the contention that both measurements reflect cardiopulmonary fitness, while simple linear regression analysis shows that V̇O2 max can only explain 44% of the variation in MRT post-training (R2=0.44). This supports the view that V̇O2 kinetics may be controlled by mechanisms differing to those limiting V̇O2max.
The post-training extension of Tlim in Tra (P<0.01) provides an interesting observation as it is not supported by significant changes in ventilation or other gas exchange parameters. However, this result supports earlier work (Markov et al. 2001) in which cycle endurance performance was extended following 15 weeks of respiratory muscle training without cardiovascular adaptations. Performance studies are typically prone to much variability in Tlim because of day-to-day variations in subject motivation, effort perceptions, learning effects and normal biological variability. It is possible that the cause of this finding is related to one or more of these factors, especially as Con also significantly extended Tlim post training (P<0.05). Sustained motivation or reduced dyspnoea, would clearly prove useful if they were to lead to the maintenance of greater sustained work loads during training, however, the long-term relationship between Tlim and IMT remains to be elucidated.
An alternative explanation for the extension of Tlim may be attributable to respiratory pump fatigue. The occurrence of diaphragmatic fatigue has already been established (Johnson et al. 1993; Mador et al. 1993) and the observations of this study suggest that the respiratory system might prove an exercise-limiting factor in high intensity, constant-load exercise independent of cardiovascular adaptation (Markov et al. 2001).
Post-training blood lactate concentrations in this study were not significantly different in either group. Tra in this study showed a trend for lower peak blood lactate concentrations post IMT (Fig. 2), which could suggest greater respiratory efficiency in the utilisation and turnover of lactate, but this observation would require further investigation. The significant extension of Tlim following IMT may be related to alterations in lactate production and clearance at the respiratory muscles, but the cause remains unclear and could be related to increased exposure to high ventilatory challenges in the V̇O2max and Tlim tests.
In conclusion, the improvement of Pi,max in Tra shows that IMT training enhances inspiratory muscle strength (P<0.01); however, this is not supported by improvement in either V̇O2 kinetics or V̇O2max. It is therefore likely that IMT training alone is not of direct benefit to the cardiopulmonary fitness of healthy subjects. However, diaphragmatic fatigue may have a limiting role in maximal constant-load exercise and consequently, IMT might be a useful stratagem of extracting greater volumes of endurance work at high ventilatory loads, which in turn could improve cardiopulmonary fitness.
References
Bassett DR, Howley ET (1997) Maximal oxygen uptake: “classical” versus “contemporary” viewpoints. Med Sci Sports Exerc 29:591–603
Berry M, Moritani T (1985) The effects of various training intensities on the kinetics of oxygen consumption. J Sports Med Phys Fitness 25(3):77–83
Borg GA (1982) Psychophysical bases of physical exertion. Med Sci Sports Exerc 14:377–381
Cadefau J, Green HJ, Cusso R, Ball-Burnett M, Jamieson G (1994) Coupling of muscle phoshorylation potential to glycolysis during work after short-term training. J Appl Physiol 76:2586–2593
Capelli C, Cautero M, di Prampero PE (2001) New perspectives in breath-by-breath determination of alveolar gas exchange in humans. Pflugers Arch, 441:566–577
Carter H, Jones AM, Barstow TJ, Burnley M, Williams C, Doust J. (2000). Effect of endurance training on oxygen uptake kinetics during treadmill running. J Appl Physiol 89:1744–1752
Edwards AM, Claxton DB, Fysh ML (2003) A comparison of two time domain analysis procedures in the determination of V̇O2 kinetics by PRBS exercise testing. Eur J Appl Physiol 88:411–416
Fairbarn MS, Coutts KC, Pardy RL, McKenzie DC (1991) Improved respiratory muscle endurance on highly trained cyclists and the effects on maximal exercise performance. Int J Sports Med 12:66–70
Fukuoka Y, Shigematsu M, Itoh M, Fujii N, Homma S, Ikegami H (1997) Effects of football training on ventilatory and gas exchange kinetics to sinusoidal work load. J Sports Med Phys Fitness 37:161–167
Grassi B, Poole DC, Richardson RS, Knight DR, Erickson BK, Wagner PD (1996) Muscle O2 uptake kinetics in humans: implications for metabolic control. J Appl Physiol 80:988–998
Green HJ, Cadefau J, Cusso R, Ball-Burnett M, Jamieson G (1995) Metabolic adaptations are expressed early in submaximal exercise. Can J Physiol Pharmacol 73:474–482
Harms CA, Babcock MA, McClaran SR, Pegelow DF, Nickele GA, Nelson WB, Dempsey JA (1997) Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol 82:1573–1583
Harms CA, Wetter T, McClaran SR, Pegelow DF, Nickele GA, Nelson WB, Dempsey JA (1998) Effect of respiratory muscle work on cardiac output and its distribution during maximal exercise. J Appl Physiol 85:609–618
Harms CA, Wetter TJ, St Croix CM, Pegelow DF, Dempsey JA (2000) Effects of respiratory muscle work on exercise performance. J Appl Physiol 89:131–138
Hughson RL, Morrissey M (1982) Delayed kinetics of respiratory gas exchange in the transition from prior exercise. J Appl Physiol 52:921–929
Inbar O, Weiner P, Azgad Y, Rotstein A, Weinstein Y (2000) Specific inspiratory muscle training in well-trained endurance athletes. Med Sci Sports Exerc 32:1233–1237
Johnson BD, Babcock MA, Suman OE, Dempsey JA (1993) Exercise-induced diaphragmatic fatigue in healthy humans. J Physiol (Lond) 460:385–405
Mador MJ, Magalang UJ, Rodis A, Kufel TJ (1993) Diaphragm fatigue after exercise in healthy human subjects. Am Rev Respir Dis 148:1571–1578
Markov G, Spengler CM, Knopfli-Lenzin C, Stuessi C, Boutellier U (2001) Respiratory muscle training increases cycling endurance without affecting cardiovascular responses to exercise Eur J Appl Physiol 85:233–239
Morgan DW, Kohrt WM, Bates BJ, Skinner JS (1987) Effects of respiratory muscle endurance training on ventilatory and endurance performance of moderately trained cyclists. Int J Sports Med 8:88–93
Phillips SM, Green HG, MacDonald MJ, Hughson RL (1995) Progressive effect of endurance training on V̇O2 kinetics at the onset of submaximal exercise. J Appl Physiol 79:1914–1920
Powers SK, Dodd S, Beadle RE (1985) Oxygen uptake kinetics in trained athletes differing in V̇O2max. Eur J Appl Physiol 54:306–308
Romer LM, McConnell AK (2003) Specificity and reversibility of inspiratory muscle training. Med Sci Sports Exerc 35:237–244
Rossiter HB, Ward SA, Doyle VL, Howe FA, Griffiths JR, Whipp BJ (1999) Inferences from pulmonary O2 uptake with respect to intramuscular [phosphocreatine] kinetics during moderate exercise in humans. J Physiol (Lond) 518:921–932
Saltin B, Astrand PO (1967) Maximal oxygen consumption in athletes. J Appl Physiol 23:353–358
Spengler CM, Roos M, Laube SM, Boutellier U (1999) Decreased exercise blood lactate concentrations after respiratory endurance training in humans. Eur J Appl Physiol 79:299–305
Volianitis S, McConnell AK, Koutedakis Y, McNaughton L, Backx K, Jones DA (2001) Inspiratory muscle training improves rowing performance. Med Sci Sports Exerc 33:803–809
Wagner PD (1996) A theoretical analysis of factors determining V̇O2 max at sea level and altitude. Respir Physiol 106:329–343
Whipp BJ, Ward SA, Lamarra N, Davis JA, Wassermann K (1982) Parameters of ventilatory and gas exchange dynamics during exercise. J Appl Physiol 52:1506–1513
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Edwards, A.M., Cooke, C.B. Oxygen uptake kinetics and maximal aerobic power are unaffected by inspiratory muscle training in healthy subjects where time to exhaustion is extended. Eur J Appl Physiol 93, 139–144 (2004). https://doi.org/10.1007/s00421-004-1188-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-004-1188-0