Abstract
The purpose of this study was to track changes in stroke volume during exercise by impedance cardiography in order to validate the method, and to obtain such data in a large number of healthy children for reference purposes. One hundred and fifteen healthy children (aged 7–19 years) performed progressive exercise to voluntary exhaustion with work increments every minute on a cycle ergometer. Oxygen uptake (V̇O2) was measured on a breath-by-breath system. Cardiac output was measured with an ICG-M501 impedance cardiograph. Stroke volume was normalized for body surface area and expressed as stroke volume index. Cardiac output was regressed against V̇O2, and differences between stroke volume index at rest and exercise were assessed by repeated measures analysis of variance. Cardiac output increased linearly with V̇O2 in all subjects: individual slopes and intercepts averaged 5.16 (1.56) l⋅min−1 per l⋅min−1 V̇O2, and 4.25 (1.92) l⋅min−1, respectively [mean (SD)]. Stroke volume index rose by an average of 29% from rest to exercise, reaching a maximum of 52 ml⋅m−2 in boys and girls. Most subjects demonstrated a continuous, gentle rise in stroke volume index with increasing work rate, though a minority demonstrated a falling index as work increased above the anaerobic threshold, despite rising cardiac output. Impedance cardiography accurately tracks cardiac output and can be a useful clinical and research tool in pediatric cardiology and exercise physiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac output in healthy children during exercise has been measured by several different techniques: CO2 rebreathing (Bar-Or et al. 1971; Gadhoke and Jones 1971; Godfrey et al. 1971; Miyamura and Honda 1973; Turley and Wilmore 1997); inert gas uptake (Seely et al. 1974); Doppler echocardiography (Rowland et al. 1997, 2000); or invasive techniques (Cumming 1977; Eriksson et al. 1971). Godfrey et al. (1971) provided reference values for stroke volume during upright exercise in a relatively large sample of children spanning the testable pediatric age range using the indirect Fick [CO2] method. More recently, Rowland et al. (1997) used echocardiography to measure stroke volume in a large sample of healthy children exercising in the semi-recumbent position. Other than these, comprehensive reference data for stroke volume in a large sample of healthy children during incremental exercise are lacking. Impedance cardiography is another non-invasive method for measurement of cardiac output at rest or during exercise (DeMaria and Raisinghani 2000; Raaijmakers et al. 1999). Successful validation studies with one impedance device, ICG M401 (ASK, Budapest), during exercise in children have been reported (Pianosi and Warren 2002; Pianosi 1997; Pianosi and Garros 1996). Yet, impedance cardiography has never gained widespread acceptance because of uncertainty over its theoretical foundations, and because of equivocal findings of previous reports comparing this method with more accepted methods of measuring cardiac output.
Though generally believed that stroke volume reaches a plateau at approximately one-third of maximum aerobic capacity in children, Eriksson et al. (1971) employing an indicator dilution method, noted that six of eight subjects achieved their largest stroke volume at maximal exercise. On the other hand, there is evidence in adults that stroke volume falls slightly during exercise above the ventilatory anaerobic threshold, perhaps because of reduced diastolic filling time (Higginbotham et al. 1986). Clinical experience has shown that during heavy exercise, heart rate in children tends to rise less for a given increment in work rate than it does at moderate exercise. This is usually attributed to the increased utilization of anaerobic metabolism in heavy exercise, while the contribution of aerobic metabolism falls proportionately. An alternative explanation is that stroke volume continues to rise steadily right up to maximal exercise in children. The primary aim of this study was to measure stroke volume repeatedly during progressive exercise in healthy children in order to track its degree of change (or lack thereof) from rest to maximal exercise. Moreover, confirmation that the relationship between oxygen uptake (V̇O2) and cardiac output (product of heart rate and stroke volume) measured by thoracic impedance matched accepted norms in a large number of subjects would demonstrate the value of impedance cardiography in pediatric work physiology.
Methods
One hundred and fifteen subjects were recruited from children of hospital personnel and/or their acquaintances through word of mouth. Inclusion criteria were age 7–19 years, and height minimum of 125 cm to fit on the ergometer, in addition to being healthy with no recent acute illness. This study was approved by the Research Ethics of the IWK Hospital and parents or mature minors signed informed written consent.
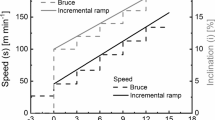
Each subject performed a progressive exercise test with step increments in work rate of 8, 16, or 25 W (depending on the subject’s size and age) on an electrically braked cycle ergometer (Collins, Braintree, Mass., USA). Subjects were verbally encouraged to pedal to symptom-limited exhaustion. Maximal test criteria consisted of any two of the following: visible signs of fatigue (flushing, sweating, panting, and falling pedal rpm); heart rate >190 min−1; and a respiratory exchange ratio greater than unity. Ventilation and gas exchange were measured on a breath-by-breath exercise-testing module (CPX Plus; Collins) that underwent volume and gas calibrations before and after every test. Heart rate was monitored with a tripolar lead system (model 90623A; SpaceLabs, Redmond, Wash., USA) that was connected to the CPX system. Blood pressure was measured by auscultation with the aid of ultrasonic flow detector (Parks Electronics, Aloha, Ore., USA) and anaeroid sphygmomanometer each minute of exercise.
Cardiac output was measured during the final 30 s of each minute of exercise by impedance cardiography (ICG M501; ASK, Budapest). This device is the successor to the device originally used (ICG M401) in the initial validation study (Pianosi and Garros 1996). The present study used one-piece, foam-backed, electrodes (MediTrace Mini; Graphic Controls, Gananoque, Canada) on the neck, and at the level of the xiphoid process. The value for thoracic length, L, used in computation of stroke volume was measured with calipers as the linear distance between the inner pair of neck-thorax electrodes. Each cardiac output determination was done using cardiac cycles over an 8-s interval. In practice, this meant that only eight beats were averaged to compute stroke volume at resting heart rates but as many as 25 beats might be averaged in heavy exercise. After a test, the graphical display of heart rate, stoke volume, and cardiac output (heart rate·stoke volume) over time were examined and the beat-to-beat impedance curves were examined for movement artifact. Significant movement artifact was presumed when the dZ/dt waveform was visibly flattened or heightened compared to adjacent traces, and such beats were deleted from the computation of mean stroke volume for that workload, but no fewer than six to eight beats were used to compute cardiac output. In pilot studies, this “eyeballing” method was more robust than any mathematical manipulations (e.g., exclusion of any dZ/dt value >1.5 or 2 SD beyond the mean for that 8-s measurement interval) that were explored. Cardiac output at rest was determined as the mean of three to four measurements (one per minute) made while the subject was seated on the bicycle but before pedaling commenced. No attempts were made to measure a true “resting” V̇O2. The anaerobic threshold was determined by the V-slope method (Beaver et al. 1986). Peak heart rate and peak V̇O2 were determined as the highest heart rate and V̇O2 achieved during the final workload. The maximum stroke volume observed during exercise was also recorded, regardless of whether it occurred at maximal or submaximal work.
Statistical analysis began with regression of cardiac output (Q̇) against V̇O2 (measured during the final 30 s of each workload) calculated for each subject. Stroke volume index (SVI) was calculated to normalize data from subjects of vastly different body size. Changes from rest to different exercise intensities were tested for statistical significance by repeated measures analysis of variance, which permitted testing of the primary hypothesis. Exercise intensities were divided into mild (≤33% peak V̇O2), moderate (34% of peak V̇O2 to the anaerobic threshold), exercise at the anaerobic threshold, heavy (between V̇O2 at the anaerobic threshold and peak V̇O2), and maximal, all of which constituted the within-subjects variance.
Results
Characteristics of the 115 subjects whose data were analyzed are shown in Table 1. Selected resting and maximal exercise measurements are shown in Table 2. Cardiac output increased linearly with V̇O2 in all subjects and the regression for the entire group plotted collectively is shown in Fig. 1. Individual slopes and intercepts ranged from 5.16 (1.56) l·min−1 per l⋅min−1 V̇O2, and 4.25 (1.92) l·min−1, respectively [mean (SD)], with high coefficients of regression [0.883 (0.09)].
Aggregate plot of individual regression lines (one per subject) of cardiac output versus oxygen uptake, with boys on the left and girls on the right (note range of abscissae). Points represent individual subject values, though symbols had to be used repeatedly due to the large number of subjects tested
Mean resting SVI was slightly higher in girls than in boys [42 (8) versus 39 (6) ml⋅m−2, P=0.02], but the highest exercise SVI was similar in boys and girls [51 (7) and 52 (9) ml⋅m−2]. Overall, SVI rose by a mean of 29% (range 0–77%) from rest to exercise (P<0.0001) although the relative increase was higher in boys than in girls (33% versus 25%, P=0.007). There was a substantial increase in SVI from rest to mild exercise, followed by a more gradual rise above the anaerobic threshold, continuing through to peak exercise (Fig. 2). Individually, 60 children showed a continual rise, 38 showed a leveling off, while 17 showed a fall in SVI during suprathreshold exercise.
Mean stroke volume index (SVI) plotted against exercise intensity (AT anaerobic threshold). Error bars represent 95% confidence intervals. The overall P value for the repeated measures analysis was <0.0001. Scheffe’s post hoc tests demonstrated significant rise in SVI from rest to mild exercise, from moderate to heavy exercise, and from heavy to maximal exercise
Discussion
Previously, impedance cardiography using the ICG-M401 compared very favorably with indirect Fick [CO2] measurements of cardiac output during exercise in healthy children and in children with minimal lung disease due to cystic fibrosis (Pianosi and Garros 1996; Pianosi 1997). Moreover, very similar resting measurements of cardiac output were obtained in a group of children with surgically corrected transposition of the great vessels and Fallot’s tetralogy using Doppler echocardiography and the ICG-M501 (Pianosi and Warren 2002). Another means of validating impedance cardiography is to compare the cardiac output measurements obtained against oxygen uptake (measured independently), since there is a clear physiological coupling between them. In essence, this amounts to a two-point calibration method measuring the “zero” (resting cardiac output) and the “gain” (change in Q̇ with V̇O2) of the impedance device employed. These data extend the initial validation studies of thoracic impedance estimates of cardiac output during exercise to a larger number of healthy children. Validation of the method is axiomatic by virtue of the fact that the measurements obtained did indeed conform to the accepted Q̇-V̇O2 relationship during exercise. Furthermore, resting cardiac output and measurements at light workloads were also made and permitted comparisons of the rest-to-exercise stroke volume recruitment. The indirect Fick [CO2] method employed in the initial validation studies is notoriously unreliable under these circumstances, when the arteriovenous CO2 content differences are small and subject to large errors of estimation. The ability to obtain accurate, repeated measurements during exercise without perturbing the subjects facilitated demonstration that stroke volume rose progressively with increasing exercise intensity in the majority of healthy children studied.
It had long been thought, though with little experimental support, that stroke volume in children reaches a plateau in light-moderate exercise with little or no further rise with increasing exercise intensity (Godfrey 1974; Bar-Or 1983). More recently, Rowland et al. (1997, 2000, 2001) affirmed this notion and corroborated findings previously described in adults, i.e. the initial rise in stroke volume generally terminated in a plateau at mild to moderate work intensity. On the other hand, the present study demonstrated small but significant increments in stroke volume even in heavy exercise, mirroring the pioneering studies of Eriksson et al. (1971). The most likely explanation for these divergent conclusions is differences in sample size and statistical power. The smaller, suprathreshold increments in stroke volume could be drowned out by the larger intersubject variability of the inotropic response to exercise. This variability is interesting in and of itself. Not all the subjects in the present study maintained a level stoke volume with increasing exercise intensity. As Rowland et al. (2000) stated, peripheral vasodilation plays an important role in the early rise in stroke volume, increasing heart rate acts to maintain it at high workloads, and improvements in contractility serve to boost stroke volume as systolic ejection time shortens. It appears that early diastolic filling is crucial to maintaining and even augmenting stroke volume with increasing exercise intensity in children (Rowland et al. 2001) and in the elderly (Peterson et al. 2003). Rowland et al. (2000) further demonstrated improved indices of contractility (shortening fraction, aortic velocity) at moderate to high intensity exercise, but these were not accompanied by further increments in stroke volume because of progressively reduced ejection time. However, it remains conceivable that in healthy children the combination of a compliant left ventricle, brisk diastolic filling, and peripheral vasodilation with improved contractility due to catecholamine release in heavy exercise will result in a further rise in stroke volume. The reasons why a minority of children actually demonstrated a fall in stroke volume with increasing exercise intensity are speculative, but they likely represent the opposite of the spectrum with a combination of stiffer left ventricle, slower early diastolic filling, and/or suboptimal inotropic response to catecholamines.
Comparison of stroke volumes obtained in the present study with results obtained in previous studies (Table 3) of upright exercise in children support the accuracy of impedance cardiography. The results of Ericsson et al. (1971) using invasive techniques in a small but well-defined population yielded results for maximal exercise cardiac output and stroke volume strikingly similar to those of the present study. The other two studies yielded higher values for cardiac variables, but also higher V̇O2 at maximum exercise, that, of necessity, would be associated with higher cardiac output. Indeed, Rowland et al. (1997) reported an average increase in stroke volume above resting levels of 42% in boys and 26% in girls, in comparison to the 33% and 25% increase, respectively, found in the present study. The cardiac output, stroke volume, and heart rate values at maximal exercise reported by Miyamura and Honda (1973) in girls were remarkably similar to comparable results in the present study. On the other hand, values obtained in boys differed notably between the two series (Tables 2, 3), which could be due to differences in pubertal status or physical maturity. Cumming (1977) studied 60 children with normal hearts, with a mean age of 12 years, during supine exercise. He reported peak exercise stroke volume index and cardiac index, respectively, of 56 ml⋅m−2 and 10.1 l⋅min−1⋅m−2 in boys, and 46 ml⋅m−2 and 8.6 l⋅min−1⋅m−2 in girls. In the present report, peak exercise stroke index and cardiac index were 51 ml⋅m−2 and 9.2 l⋅min−1⋅m−2 in boys, and 52 ml⋅m−2 and 9.3 l⋅min−1⋅m−2 in girls, respectively. Thus, in general, the results of the present study are more in line with previously published results obtained by invasive techniques, than with other studies that employed non-invasive methods. There have been few previous studies comparing impedance cardiography with other methods of measuring cardiac output in children. Miles and Gotshall (1989) and Braden et al. (1990) found good correlations between impedance and direct Fick measurements of cardiac output in children without intracardiac shunts. The more traditional methods of measuring cardiac output have their own pitfalls, and discrepancies between the results of different methods in validation studies have been automatically and inappropriately presumed due to problems with the impedance method (Raaijmakers et al. 1999).
The theory behind the method and comparisons of impedance-derived cardiac output measurements compared with other methods have been reviewed (Miles and Gotshall 1989; Penney 1985). In short, the thorax is a cylinder or truncated cone whose electrical impedance changes in proportion to the electrical conductivity of the blood within, simultaneously with mechanical systole. Exercise stroke volume in children increases with height in children (Godfrey 1974), and height of the thorax (L) is likewise critical to measurement of stroke volume by impedance cardiography. Precisely how one should measure L has not been specifically addressed in studies, though some authors have used the topographical distance measured along the sternum, anterior chest wall, or posterior chest wall (reviewed in Miles and Gotshall 1989). Introna et al. (1988) went so far as to suggest one choose the value of L that yielded the least difference in cardiac output measurements when compared with thermodilution because it was superior to a fixed L of 0.17×height. Calipers were used as a means of circumventing this unknown (Miles and Gotshall 1989), recognizing that the value for L measured by calipers would fall between the simple vertical distance between coronal planes cut by the electrode pairs (cylindrical model), and the surface topographical distance between them (conical model). Empirically, thoracic length measured as described produced very good results when one compared resting echocardiographic measurements with impedance measurements of cardiac output, and therefore this same value was used throughout exercise.
In summary, thoracic impedance cardiography offers a simple and unobtrusive method, and yields results comparable to other methods, for measuring cardiac output during exercise. This will open the door for additional descriptive and mechanistic studies of cardiac output in children during exercise. Studies to examine the kinetics of the stroke volume and cardiac output response to exercise have already been completed in healthy children as well as children with surgically corrected cyanotic congenital heart disease.
References
Bar-Or O (1983) Pediatric sports medicine for the practitioner: from physiologic principles to clinical applications. Springer, Berlin Heidelberg New York, pp 18–22
Bar-Or O, Shephard RJ, Allen CL (1971) Cardiac output of 10- to 13-year-old boys and girls during submaximal exercise. J Appl Physiol 30:219–223
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Braden DS, Leatherbury L, Treiber FA, Strong WB (1990) Noninvasive assessment of cardiac output in children using impedance cardiography. Am Heart J 120:1166–1172
Cumming GR (1977) Hemodynamics of supine bicycle exercise in “normal” children. Am Heart J 93:617–622
DeMaria AN, Raisinghani A (2000) Comparative overview of cardiac output measurement methods: has impedance cardiography come of age? CHF 6:7–18
Eriksson BO, Grimby G, Saltin B (1971) Cardiac output and arterial blood gases during exercise in pubertal boys. J Appl Physiol 31:348–352
Gadhoke S, Jones NL (1971) The response to exercise in boys aged 9–15 years. Clin Sci 41:789–801
Godfrey S (1974) Exercise testing in children: applications in health and disease. Saunders, London, p 98
Godfrey S, Davies CTM, Wozniak E, Barnes CA (1971) Cardiorespiratory responses to exercise in normal children. Clin Sci 40:419–431
Higginbotham MB, Morris KG, Williams RS, McHale PA, Coleman RE, Cobb FR (1986) Regulation of stroke volume during submaximal and maximal upright exercise in normal man. Circ Res 58:281–291
Introna RPS, Pruett JK, Crumrine RC, Cuadrado AR (1988) Use of transthoracic bioimpedance to determine cardiac output in pediatric patients. Crit Care Med 16:1101–1105
Miles DS, Gotshall RW (1989) Impedance cardiography: non-invasive assessment of human central hemodynamics at rest and during exercise. Exerc Sport Sci Rev 17:231–263
Miyamura M, Honda Y (1973) Maximum cardiac output related to sex and age. Jpn J Physiol 23:645–656
Penney BC (1985) Theory and applications of electrical impedance measurements. CRC Crit Rev Biomed Eng 13:227–281
Peterson LR et al (2003) Peak exercise stroke volume: associations with cardiac structure and diastolic function. J Appl Physiol 94:1108–1114
Pianosi P (1997) Impedance cardiography accurately measures cardiac output in children with cystic fibrosis during exercise. Chest 111:333–337
Pianosi P, Garros D (1996) Impedance cardiography in healthy children on exercise: comparison with indirect Fick [CO2] method. Am J Cardiol 77:745–749
Pianosi P, Warren A (2002) Validation of Impedance cardiography in children with repaired congenital heart disease. Can J Cardiol 18 [Suppl B]:36
Raijmakers E, Faes TJ, Scholten R, Goovaerts HG, Heethaar RM (1999) Meta-analysis of three decades of validating thoracic impedance cardiography. Crit Care Med 27:1203–1213
Rowland T, Popowski B, Ferrone L (1997) Cardiac responses to maximal upright cycle exercise in healthy boys and men. Med Sci Sports Exer 29:1146–1151
Rowland T, Potts J, Potts T, Sandor G, Goff D, Ferrone L (2000) Cardiac response to progressive exercise in normal children: a synthesis. Med Sci Sports Exerc 32:253–259
Rowland T, Mannie E, Gawle L (2001) Dynamics of left ventricular diastolic filling during exercise. Chest 120:145–150
Seely JE, Guzman CA, Becklake MR (1974) Heart and lung function at rest and during exercise in adolescence. J Appl Physiol 36:34–40
Turley KR, Wilmore JH (1997) Cardiovascular responses to treadmill and cycle ergometer exercise in children and adults. J Appl Physiol 83:948–957
Acknowledgements
Funded by a grant from the Heart and Stroke Foundation of Nova Scotia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pianosi, P.T. Measurement of exercise cardiac output by thoracic impedance in healthy children. Eur J Appl Physiol 92, 425–430 (2004). https://doi.org/10.1007/s00421-004-1167-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-004-1167-5