Abstract
Objectives
To compare a local cohort of 2488 men occupationally exposed to asbestos and enrolled in a public health surveillance program with the 1995–2009 cancer incidence of the general population of Friuli Venezia Giulia (FVG) region, Northeast Italy, we conducted a historical cohort study.
Methods
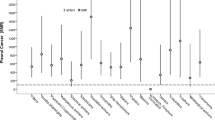
Standardized incidence ratios (SIRs), with 95% confidence interval (95% CI), for specific cancer sites were estimated in the cohort and in subgroups of workers employed in shipbuilding between 1974 and 1994. For internal comparisons, we calculated incidence rate ratios (IRRs) for all cancers, lung cancer and mesothelioma, by level of exposure to asbestos and sector of employment adjusted for smoking habits and age at start of follow-up.
Results
Among cohort members the SIR was 8.82 (95% CI 5.95–12.61) for mesothelioma and 1.61 (95% CI 1.26–2.04) for lung cancer. In subgroup analyses, the SIR for lung cancer in subjects hired in shipbuilding between 1974 and 1984 was 2.09 (95% CI 1.32–3.13). In the overall cohort, a borderline increased incidence was also found for stomach cancer (SIR = 1.53 95% CI 0.96–2.31). Internal comparisons within the cohort show that among men with high asbestos exposure level the relative risk was almost threefold for lung cancer (IRR = 2.94 95% CI 1.01–8.57).
Conclusions
This cohort experienced an excess in the incidence of both mesothelioma and lung cancer, showing increasing incidence rates at higher level of asbestos exposure. For lung cancer, the relative incidence was highest among workers hired in shipbuilding between 1974 and 1984.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Italy has been an important producer and user of asbestos until 1992, with an overall estimated consumption of 3,748,550 tons of raw asbestos, peaking in the period between 1976 and 1980 (Magnani et al. 2015). Several industrial sectors were involved in asbestos exposure in Italy, such as asbestos–cement industry, construction and maintenance of railroad vehicles and ships, chemical industry, steel industry, metal works, building and others (Magnani et al. 2015). In 2011, 1428 new cases of mesothelioma (1035 men and 393 women) were recorded, corresponding to an incidence rate of 3.64 and 1.32 per 100,000 person-years in men and women, respectively (Magnani et al. 2015). The Adriatic coast of Friuli Venezia Giulia (FVG) region (Northeast Italy) near Trieste, its largest coastal city, has been home to shipbuilding industry since the early 1700s and by the end of the nineteenth century the local shipyards had become the most important of the Mediterranean Sea. Worldwide use and presence of asbestos in shipbuilding is well known (Beckett 2007). Accordingly, in the Trieste area, from the early 1900s until the early 1980s the shipbuilding industry has been by far the largest utilizer of asbestos in the area, although also other local industrial activities (e.g., metalworking, shipping, cotton mills, construction) utilized large amounts of asbestos.
The epidemiology of lung cancer in the area has been studied extensively (Barbone et al. 1995a, b, 1997; Biggeri et al. 1996; Bovenzi et al. 1993). In particular, in a case–control study conducted in the general population of Trieste the relative risk (RR) of lung cancer for occupational exposure to asbestos, adjusted for smoking and air pollution, was 1.98 [95% confidence interval (CI) 1.42–2.75], with a corresponding attributable risk (AR) estimate of 20% (95% CI 11.5–28.5) (Bovenzi et al. 1993).
To reduce the risk of asbestos-related disease among asbestos workers, Italian and European regulations were promulgated in the early 1990s (D. Lgs n 277 1991; Italian Law n 257 1992) and occupational health surveillance programs for formerly exposed workers were established in most regions. However, very limited evidence exists on the efficacy of such programs in reducing disease occurrence and mortality (Karjalainen 1997; Pinto et al. 2013).
Timely occupational, public health care services were offered to residents also in FVG region. These health care services have provided technical and health care activities carried out at a dedicated outpatient clinic, as part of an overall “Asbestos Project”. Aims of the project included: (a) control of human contact with asbestos-containing structures, landfills and instruments, and (b) actions limiting the health effects of past exposure, both on workers and on the general population. In particular, a public health surveillance program (PHP) for persons with previous occupational exposure to asbestos was established.
To measure the relative occurrence of cancer in male subjects enrolled in this PHP on asbestos exposure, an historical cohort study was conducted using as an external comparison the general population of FVG region. In addition, internal comparisons within the cohort were conducted to assess relative cancer incidence by asbestos exposure level, industrial sector of employment and personal risk factors (smoking).
Materials and methods
Setting
FVG region (population: 1.2 million) (ISTAT 2011) offers comparable public health services through its five Public Health Departments (PHD). Since 1991 the largest occupational clinic responsible for the public health surveillance of asbestos-exposed workers has been located in the city of Monfalcone, in the Trieste coastal area, where most of the Italian shipbuilding activities have been concentrated over the past several decades. Monfalcone shipyard is one of the largest in Europe and worldwide, mainly dedicated to the design and production of various types of civil and military ships. This cohort study is based on subjects identified at this clinic between years 1991–2008. During this time-frame former workers from any industrial sectors claiming an occupational exposure to asbestos and their spouses had voluntary and free access to this clinic. The clinic provided both certification of exposure for the purpose of reimbursement and diagnostic and therapeutic prescribing. Since enrollment in the program is voluntary, the actual number of all the exposed workers in the study area or even in the whole region is unknown. As an example of the extent of the regional participation in public health surveillance of asbestos-exposed workers, it has been reported that between 2001 and 2014 over 9100 individuals were enrolled in its five PHDs (Barbiero et al. 2018).
During the initial visit, occupational health personnel collected the work history and any available objective documentation of the subject’s exposure to asbestos. Documentation comprised employment cards, proofs of exposure certified by the National Institute for Insurance against Accidents at Work (INAIL) and/or declarations from colleagues. For each worker, intensity of exposure was classified according to job–exposure matrices available from the literature (Goldberg et al. 1993; Goldberg 2002; Orlowski et al. 1993). Intensity of exposure was considered (a) high when there was evidence that the subject had direct or indirect contact with friable material containing asbestos in confined spaces; (b) moderate, when the subject had occasional contact with friable materials, worked with compact material containing asbestos or used continuously substrates containing asbestos; and (c) low, when the subject had occasional exposure to environmental materials containing asbestos.
Considering that there is not yet an established strategy for the surveillance of asbestos-exposed subjects, that is still empirical rather than evidence-based, types and periodicity of health examinations varied individually according to the physician-expert opinion. Exams may have included physical examination, basal spirometry, alveolar diffusion of CO (DLCO), chest X-ray film and chest computerized tomography (CT) (Acton 2014).
Surveillance registry
For each person enlisted in the surveillance program, the following information was recorded electronically: demographics (name, surname, date of birth, residence and phone number); company name and industrial sector; total years of exposure to asbestos; cigarette smoking habits (never, ex or current smoker); type, date and findings of examination. Since only 96 women enlisted in the surveillance program, their evaluation will not be presented in this report.
A flow-chart describing the process of study cohort identification is shown in Fig. 1. The final cohort included 2488 men with prior occupational exposure to asbestos enrolled in this PHP.
Follow-up
For each member of the cohort, the residential status in FVG and the vital status, including cause of death, between 1 January 1995 and 31 December 2009 were assessed through record linkage with the Regional Health Database. Incident cases of cancer were identified through record linkage with the cancer registry (CR) of the Region Friuli Venezia Giulia, available for the period 1995–2009. The CR of FVG is part of the European Cancer Observatory (ECO), a project developed at the International Agency for Research on Cancer (IARC) in partnership with the European Network of Cancer Registries (ENCR) in the framework of the EUROCOURSE project supported by the European Commission.
CR follows cancer registration rules according to World Health Organization (WHO), IARC and International Association of Cancer Registries (Jensen and Storm 1991). In brief, CR registers all the new, incident cases of malignant neoplasm among residents in the region. CR adopts an ‘automatic’ registration method that starts from a regional epidemiologic data warehouse including the following computerized data sources: Hospital Admissions, Pathology Reports, Death Records and Residential Status Records. After exclusion of prevalent cases and non-residents in the study period, an automatic algorithm, developed using the available data sources in accordance with IARC registration compatibility principles, assigns a new cancer case diagnosis. When automatic assignment is not reached a direct, individual examination is conducted using the sources listed above. Furthermore, the validity of automatic and manual assignments is confirmed by a second manual step on a sample of the available records.
Each member of the cohort was followed from the date of the first surveillance examination or 01/01/1995, whichever last, up to the incidence date, death date, end of residence in FVG or 31/12/2009, whichever first.
Incident cases identified in the CR, were coded according to the WHO International Classification of Diseases, 10th edition (ICD-10). The number of observed cases and incidence rates by calendar year were calculated for all cancers (C00–D48), mesothelioma (C45), lung cancer including trachea and bronchus (C33–C34) and other specific cancers. Prevalent cases of cancer, identified at start of follow-up, were excluded.
Statistical analysis using an external comparison
Age-standardized relative incidence was estimated by comparison with the general population of FVG, from 1995 to 2009. The number of observed cases and calendar year- and age-specific incidence rates from 1995 to 2009 (Supplemental Tables 1–3), were calculated for all cancers, mesothelioma and lung cancer.
Standardized incidence ratios (SIRs), and 95% CI were calculated by the indirect standardization method (Breslow and Day 1987) as the ratio of observed cases by those expected on the basis of calendar year-, age-, and sex-specific rates in the general population of FVG region provided by the Italian Association of Cancer Registries (AIRTUM). Specific rates for the whole Italian population were not used as external standards because of limited historical and geographical availability. However, a sensitivity analysis based on rates from different Italian regions or areas has been conducted and presented elsewhere (Barbiero et al. 2016). Rates of year 2007 were used also for years 2008 and 2009, because the latter were unavailable.
Subgroup analyses restricted to subjects ever employed in the shipbuilding industry were also conducted. Trends in supply and consumption of asbestos in Italy have seen a rapid decrease since 1985 (Virta 2006). On the other hand, we have obtained reliable data about the first year of hire provided by INAIL only since 1974. To account for possible differences in the intensity of exposure over the years, the subgroup of former workers ever employed in the shipbuilding industry was categorized further according to hiring period in the following three groups: (a) subject hired for the first time in the period 1974–1994, (b) those hired for the first time between 1974 and 1984 and (c) those who were hired for the first time between 1985 and 1994.
Statistical analysis using an internal comparison
Within the study cohort the incidence rates, incidence rate ratios (IRRs) and 95% CIs for all cancers, lung cancer and mesothelioma were estimated by study characteristics. Poisson regression modeling was applied, considering as dependent variable the incidence rate, calculated as the ratio between the occurrence of events and a constant represented by the person-time at risk. For each outcome, univariate, bivariate and multivariate analyses were conducted. In our final models, terms were included for the following risk factors: total years of exposure to asbestos, smoking habits, level of exposure to asbestos, industrial sector, age at start of follow-up. Categories were created for these variables, except total years of exposure to asbestos and age.
All analyses were performed using SAS© software, version 9.3 (SAS Institute Inc., Cary, N.C., USA) and Microsoft® Excel 2013 spreadsheet.
Results
External comparison
Since early 1990s to 2008, 7011 physical examinations, 3059 TC, 3081 CXR, 6889 basal spirometry and 4743 DLCO have been provided, with a mean of 9.5 medical tests per person (SD = 6.4, median = 8). 65.9% (N = 1639) of the subjects presenting to the clinic performed two or more visits during the study period, with a mean of 4.1 repeated accesses per person (SD = 1.9; median = 4).
Table 1 shows the characteristics of the study cohort. Seventy percent of cohort members were shipyard workers. Measures of frequency and SIRs for all cancers, and for specific cancer sites are presented in Table 2. The number of observed cases (O) for all cancers exceeded those expected (E) (O = 337; E = 297.33), with a statistically significant increase (SIR = 1.13 95% CI 1.02–1.26), based on regional FVG standard rates, but largely explained by respiratory cancers. The SIR for lung cancer in former workers exposed to asbestos was 1.61 (95% CI 1.26–2.04) based on 66 cases observed. There were 30 cases observed of mesothelioma compared with 3.40 expected and a corresponding SIR of 8.82 (95% CI 5.95–12.61). Considering other cancer sites, we did not find an association with cancer of the larynx, whereas an increased, albeit borderline significant incidence was found for stomach cancer. Bladder cancer incidence was significantly lower than expected.
Table 3 shows the results stratified by industrial sector, level of exposure to asbestos and period of hire. Higher level of exposure to asbestos was associated with higher SIRs for all cancers, lung cancer and mesothelioma. Stratification by year of hire shows that the SIRs were particularly high among subjects employed in shipbuilding and hired between 1974 and 1984 for all cancers and lung cancer. For mesothelioma, the observed number of cases among exposed was extremely high in all groups, as compared with the expected, with SIRs varying between 7.72 and 9.56.
Internal comparison
All cancers
We observed a positive association of all cancers risk with high and moderate exposure level to asbestos (Table 4). Current smokers also were at increased risk of all cancers (IRR = 1.38 95% CI 1.09–1.75). There was also an association, albeit not statistically significant, between workers in shipbuilding and incidence of all cancers, compared with workers in other industrial sectors.
Lung cancer
Within the cohort, a high level of exposure to asbestos was associated with an almost threefold risk of lung cancer (IRR = 2.94 95% CI 1.01–8.57), as compared with low exposure. A moderate, albeit imprecise, excess risk of lung cancer, was also shown among men exposed to intermediate level of asbestos. Smoking was strongly associated with risk of lung cancer. The IRR was 4.74 for current smokers and 2.36 for ex-smokers, both compared with never smokers. Among men employed in shipbuilding the IRR of lung cancer was 1.66, compared with workers employed in other industrial sectors (Table 5).
Mesothelioma
After full adjustment for other factors there was no increased risk of mesothelioma among men hired in shipbuilding in comparison with those hired in other industrial sectors (Supplemental Table 4). There was no statistically significant association between smoking and risk of mesothelioma.
Discussion
In the cohort of former workers exposed to asbestos undergoing health surveillance (2488 men), between 1995 and 2009, there was a very strong, specific and statistically significant increase of incidence of mesothelioma, compared with the general population of FVG. In addition, the incidence of lung cancer was 61% higher in comparison with the reference population. Although for all cancers there was also a significant increase (13%), the latter finding is fully explained by the increase in mesothelioma and lung cancer.
Compared with the regional incidence rates of mesothelioma, a large excess was present in all industrial sectors and regardless of date of hire. When external comparison has been performed by level of exposure to asbestos, results showed an incremental trend of incidence of all cancers, lung cancer, and mesothelioma, compared with standard population, at the increase in the level of exposure. Therefore, the result showing that even subjects hired between 1985 and 1994 were at very high risk is puzzling because of the short latency. Given the strength (SIR = 9.56) and the precision (95% CI 5.22–16.05) of this association, it is very unlikely that results are due to chance. As an alternative, it cannot be excluded that a systematic error occurred attributing to a later date the first hire at a job that determined asbestos exposure. Perhaps personnel from the occupational clinic registered first employment in the local area during 1985–1994 decade, but in fact, asbestos exposure was experienced at an earlier time maybe outside of FVG. This would determine a misclassification of categories. Moreover, some evidence suggests that risk of mesothelioma related to asbestos exposure varies by age at exposure and time since last exposure: the effect of duration seems to be weaker for subjects who had their last exposure a long time ago or their first exposure later in life (Lacourt et al. 2012). Therefore maybe those hired in 1985–1994 were younger at first exposure (and thereby at higher risk) than those hired in 1974–1984. This could partially explain the results obtained in the subgroup with the hire date between 1974 and 1984, a longer latency and a greater hypothesized exposure intensity. Nevertheless, although asbestos supply and consumption trend in Italy decreased since 1985 (Virta 2006), it is possible that indeed asbestos in certain local workplaces was used extensively even after 1985, determining such an effect.
Differently, for lung cancer the results pertaining to the group with hypothesized highest level of exposure to asbestos (first hire before 1985) and longer latency show a particularly high incidence (Table 3). We found a borderline increase in the incidence of stomach cancer (SIR = 1.53; 95% CI 0.96–2.31). Consistently with some epidemiological evidence, our results support the hypothesis of an association between exposure to asbestos and the stomach cancer occurrence (Fortunato and Rushton 2015). However, they should be interpreted with caution considering the likelihood of confounding by other occupational exposures typical of the multifactorial etiology of gastric cancer and of the mixture of agents potentially present in the industrial environment of this study. In fact, in our investigation, we were unable to assess exposure to agents other than asbestos and we are aware that in shipbuilding (prevalent industrial sector), but also in metalworking and in other sectors, work as a painter, welder and carpenter are among the occupations involving exposure to possible carcinogens for the stomach such as inorganic lead and lead compounds (Cogliano et al. 2011). These jobs are listed among those held by workers in the area. In addition to occupational confounders mentioned above, known cause tables of stomach cancer such as genetic susceptibility, dietary habits, interactions between lifestyle, environmental exposure, occupational and genetic factors and other factors not yet recognized may have played a role on this borderline excess in this cohort.
The incidence of cancer for other anatomical sites did not show an increase in comparison with the reference population.
In our cohort, results show an incremental trend of SIRs for all cancer, lung cancer and mesothelioma, with increasing asbestos exposure level. Consistently with other studies (Carel et al. 2007; Clin et al. 2011; Gustavsson et al. 2000; Villeneuve et al. 2012; Yano et al. 2010), we found an association between lung cancer and intensity, but not duration, of asbestos exposure. Indeed, among subjects at high level of asbestos exposure, the risk of lung cancer was significantly increased (almost 3 times) compared with those exposed at low risk (Table 5).
In our final models, sector of employment did not remain associated with all cancers, lung, or mesothelioma since its effect was saturated by level of exposure.
Limitations
The FVG region has the highest incidence rates of mesothelioma in the Italian territory (Barbiero et al. 2016). Therefore, our calculation of the SIR in a population belonging to a geographic area with high underlying disease-specific incidence may have led to an underestimation of the effect introducing a bias toward the null (Barbiero et al. 2016).
In addition, approximately 400 subjects initially admitted in the cohort were excluded from the analyses because linkage with the Regional Health Database was impossible. It is likely that these subjects were actually non-residents in FVG; however, this loss to follow-up may have biased the measure of association in both directions, depending on level of exposure to asbestos in this group compared to those who remained in the final analyses. The non-quantitative assessment of smoking habits and intensity of the exposure to asbestos are additional limitations of this study. In fact, measures of air concentrations of asbestos fibers in workplaces, in Italy, are very limited. For the same reason in our investigation we did not consider: (a) the cumulative exposure dose and (b) the construction of a job–exposure matrix to assess quantitatively the intensity of exposure. Therefore, risk of exposure to asbestos considered in our study may be affected by misclassification.
In addition to these limitations, the number of incident cases of mesothelioma with a non-pleural localization was too small to allow for separate analysis for anatomical site of onset. However, this limitation is mitigated by the fact that mesothelioma of the pleura represents most of the incident cases observed in our cohort (83.0%; N = 25) consistent with the results shown in the IV Italian National Mesothelioma Register Report (Marinaccio et al. 2012). This report indicates that the mesotheliomas of the pleura represent 93.0% of the total number of reported mesothelioma cases in Italy (Marinaccio et al. 2012).
In addition, our estimates of SIRs are limited to the 1995–2009 period according to the data availability of record linkage with the regional CR.
Finally, considering that the latency of lung cancer and mesothelioma may be greater than 40 years (Mott 2012; Robinson 2012), the follow-up period in our study that ended in 2009 may be incomplete for individuals who were exposed since the 1970s or 1980s. The overall impact of the incidence of cancer in our cohort should be evaluated further through 2020 and beyond.
Conclusions
Our cohort of asbestos-exposed workers undergoing health surveillance experienced a moderate excess of incidence for all cancers. We found a strong excess of incidence of mesothelioma and again a moderate excess for lung cancer. Both mesothelioma and lung cancer incidence increased at higher level of intensity of exposure to asbestos. The relative lung cancer incidence was highest among workers hired in shipbuilding in 1974–1984, corresponding to the period in which the supply and use of asbestos in Italy peaked. Our results confirm that asbestos-related diseases are still a major problem worldwide. For this reason, scientific evidence demonstrating effective prevention in reducing disease occurrence and mortality for former workers exposed to asbestos is urgently needed, especially for lung cancer and mesothelioma.
References
Acton V (2014) Preventing pleural mesothelioma in patients with recognizable asbestos-related pleural plaques. J Thorac Cardiovasc Surg 148(4):1763. https://doi.org/10.1016/j.jtcvs.2014.03.030
AIRTUM Italian Association of Cancer Registers, Italy (2015). http://itacan.ispo.toscana.it/italian/itacan.htm (last access: 13/11/2015)
Barbiero F et al (2016) Standardization of incidence rates of mesothelioma in the absence of national standards: sensitivity analysis in a cohort formerly exposed to asbestos. Med Lav 107(4):307–314
Barbiero F et al. (2018) Mortality in a cohort of asbestos-exposed workers undergoing health surveillance. Med Lav 109(2) (In press)
Barbone F, Bovenzi M, Biggeri A, Lagazio C, Cavallieri F, Stanta G (1995a) [Comparison of epidemiologic methods in a case-control study of lung cancer and air pollution in Trieste, Italy]. Epidemiol e Prev 19(63):193–205
Barbone F, Bovenzi M, Cavallieri F, Stanta G (1995b) Air pollution and lung cancer in Trieste, Italy. Am J Epidemiol 141(12):1161–1169
Barbone F, Bovenzi M, Cavallieri F, Stanta G (1997) Cigarette smoking and histologic type of lung cancer in men. Chest 112(6):1474–1479
Beckett WS (2007) Shipyard workers and asbestos: a persistent and international problem. Occup Environ Med 64(10):639–641. https://doi.org/10.1136/oem.2006.032284
Biggeri A, Barbone F, Lagazio C, Bovenzi M, Stanta G (1996) Air pollution and lung cancer in Trieste, Italy: spatial analysis of risk as a function of distance from sources. Environ Health Perspect 104(7):750–754
Bovenzi M, Stanta G, Antiga G, Peruzzo P, Cavallieri F (1993) Occupational exposure and lung cancer risk in a coastal area of northeastern Italy. Int Arch Occup Environ Health 65(1):35–41
Breslow NE, Day NE (1987) Statistical methods in cancer research. Volume II–The design and analysis of cohort studies. IARC Sci Publ (82):1–406
Carel R et al (2007) Occupational exposure to asbestos and man-made vitreous fibres and risk of lung cancer: a multicentre case-control study in Europe. Occup Environ Med 64(8):502–508. https://doi.org/10.1136/oem.2006.027748
Clin B et al (2011) Cancer incidence within a cohort occupationally exposed to asbestos: a study of dose–response relationships. Occup Environ Med 68(11):832–836. https://doi.org/10.1136/oem.2010.059790
Cogliano VJ et al (2011) Preventable exposures associated with human cancers. J Natl Cancer Inst 103(24):1827–1839. https://doi.org/10.1093/jnci/djr483
D. Lgs n 277 (1991) D. Lgs n. 277 of August 15, 1991. Implementation of directives n. 80/1107 / EEC, n. 82/605 / EEC, n. 83/477 / EEC, n. 86/188 / EEC and n. 88/642 / EEC, concerning the protection of workers against the risks related to exposure to chemical, physical and biological agents during work, a provision of Art. 7 of the Law of 30 July 1990, n. 212
Fortunato L, Rushton L (2015) Stomach cancer and occupational exposure to asbestos: a meta-analysis of occupational cohort studies. Br J Cancer 112(11):1805–1815. https://doi.org/10.1038/bjc.2014.599
Goldberg MI, E (2002) The use of job exposure matrices for cancer epidemiology research and surveillance. Arch Pub Health 60:173–185
Goldberg M et al (1993) Job exposure matrices in industry. Int J Epidemiol 22(Suppl 2):S10-5
Gustavsson P, Jakobsson R, Nyberg F, Pershagen G, Jarup L, Scheele P (2000) Occupational exposure and lung cancer risk: a population-based case-referent study in Sweden. Am J Epidemiol 152(1):32–40
ISTAT (2011) Italian National Institute of Statistics, 15th Census of Population and Housing, 2011. Available at: http://dati-censimentopopolazione.istat.it/. Accesses 03 Nov 2014
Italian Law n 257 (1992) Italian Law n. 257 of March 27. Rules relating to the cessation of asbestos
Jensen OM, Storm HH (1991) Cancer registration: principles and methods. Reporting of results. IARC Sci Publ 95:108–125. https://www.ncbi.nlm.nih.gov/pubmed/1894317
Karjalainen A (1997) Asbestos–a continuing concern. Scand J Work Environ Health 23(2):81–82
Lacourt A et al (2012) Temporal patterns of occupational asbestos exposure and risk of pleural mesothelioma. Eur Respir J 39(6):1304–1312
Magnani C et al (2015) III Italian Consensus Conference on Malignant Mesothelioma of the Pleura. Epidemiology, Public Health and Occupational Medicine related issues. Med Lav 106(5):325–332
Marinaccio A et al (2012) Italian National Mesothelioma Register, IV Report. http://www.inail.it/internet_web/wcm/idc/groups/internet/documents/document/ucm_085815.pdf. Accessed 15 Sept 2015
Mott FE (2012) Mesothelioma: a review. Ochsner J 12(1):70–79
Orlowski E et al (1993) Retrospective assessment of asbestos exposure–II. At the job level: complementarity of job-specific questionnaire and job exposure matrices. Int J Epidemiol 22(Suppl 2):S96-105
Pinto C et al. (2013) Second Italian consensus conference on malignant pleural mesothelioma: state of the art and recommendations. Cancer Treatm Rev 39(4):328–339 https://doi.org/10.1016/j.ctrv.2012.11.004
Robinson BM (2012) Malignant pleural mesothelioma: an epidemiological perspective. Ann Cardiothorac Surg 1(4):491–496. https://doi.org/10.3978/j.issn.2225-319X.2012.11.04
Villeneuve PJ, Parent ME, Harris SA, Johnson KC (2012) Occupational exposure to asbestos and lung cancer in men: evidence from a population-based case-control study in eight Canadian provinces. BMC Cancer 12:595. https://doi.org/10.1186/1471-2407-12-595
Virta RL (2006) Worldwide asbestos supply and consumption trends from 1900 through 2003: U.S. Geological Survey Circular 1298, p 80. Available at: http://pubs.usgs.gov/circ/2006/1298/c1298.pdf (last access: 03/11/2014)
Ware RE et al (2016) Hydroxycarbamide versus chronic transfusion for maintenance of transcranial doppler flow velocities in children with sickle cell anaemia-TCD With Transfusions Changing to Hydroxyurea (TWiTCH): a multicentre, open-label, phase 3, non-inferiority trial. Lancet 387(10019):661–670. https://doi.org/10.1016/S0140-6736(15)01041-7
Yano E, Wang X, Wang M, Qiu H, Wang Z (2010) Lung cancer mortality from exposure to chrysotile asbestos and smoking: a case-control study within a cohort in China. Occup Environ Med 67(12):867–871. https://doi.org/10.1136/oem.2009.051615
Funding
This study has been carried out with no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. Fabio Barbone, Massimo Bovenzi, and Federica E. Pisa acted as expert witnesses for the public prosecutor in criminal trials on asbestos-related cancers.
Ethical approval
For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Barbiero, F., Zanin, T., Pisa, F.E. et al. Cancer incidence in a cohort of asbestos-exposed workers undergoing health surveillance. Int Arch Occup Environ Health 91, 831–841 (2018). https://doi.org/10.1007/s00420-018-1326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-018-1326-3