Abstract
Purpose
Occupational e-mental-health (OEMH) may extend existing instruments for preservation or restoration of health and work ability. As a key precondition to efficient implementation, this study examined acceptance and person-centered barriers to potential uptake of OEMH for work-related distress in employees with an elevated risk of early retirement.
Methods
Within the framework of the “Third German Sociomedical Panel of Employees”, 1829 employees with prior sickness absence payments filled out a self-administered questionnaire. Participants had a mean age of 49.93 years (SD = 4.06). 6.2% indicated prior use of eHealth interventions. Potential predictors of acceptance of OEMH were examined based on the “Unified Theory of Acceptance and Use of Technology” (UTAUT) extended by work ability, mental health, eHealth literacy and demographic characteristics.
Results
89.1% (n = 1579) showed low to moderate acceptance (M = 2.20, SD = 1.05, range 1–5). A path analysis revealed significant, positive direct effects of UTAUT predictors on acceptance (performance expectancy: 0.48, SE = 0.02, p < 0.001; effort expectancy: 0.20, SE = 0.02, p < 0.001; social influence: 0.28, SE = 0.02, p < 0.001).Online time and frequency of online health information search were further positive direct predictors of acceptance. Model fit was good [χ 2(7) = 12.91, p = 0.07, RMSEA = 0.02, CFI = 1.00, TLI = 0.99, SRMR = 0.01].
Conclusions
Attitudes towards OEMH are rather disadvantageous in the studied risk group. Implementation of OEMH, therefore, requires a-priori education including promotion of awareness, favorable attitudes regarding efficacy and usability in a collaborative approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An increasing complexity of job demands including work intensification, multi-tasking or constant availability and further dysfunctional psychosocial work environments (e.g. job strain, effort-reward imbalance) have been associated with adverse health effects and reduced work ability (Bethge et al. 2009; Stansfeld and Candy 2006). Consequently, work stress represents a major risk factor for mental disorders (Frese 1999; Stansfeld and Candy 2006) and early retirement (Gjesdal et al. 2004; Mykletun et al. 2006). Correspondingly, inpatients with mental disorders show increased work-related distress compared to the general population, mainly due to interpersonal conflicts and lower coping resources (Zwerenz et al. 2004). In turn, early retirement can be associated with decreased health or higher mortality (Karpansalo et al. 2004).
Following the principle of “rehabilitation before retirement”, improvement or restoration of health and work ability are main objectives of the German system of social security, particularly of the German Pension Insurance Fund (GPIF), with about 200 facilities specialized in mental health care (Deutsche Rentenversicherung 2017). Evidence supports the effectiveness of inpatient psychosomatic rehabilitation (Petermann and Koch 2009). However, rehabilitation services are applied rather late in the course of disease (Deutsche Rentenversicherung Bund 2014) and are preceded by long-term sickness absence (Henderson et al. 2011). Another critical aspect is the reduced adoption of indicated mental health care in those at risk for early retirement: half of early disability pensioners did not use rehabilitation services before the disability pension was approved (Deutsche Rentenversicherung Bund 2014) and two-thirds have not been receiving outpatient psychotherapy (Apfel and Riecher-Rössler 2005). Thus, efforts to increase access to mental health services and to support the development of preventive instruments for occupational mental health are urgently needed.
A promising extension to existing health care instruments may be low-threshold, web- or mobile-delivered interventions, which can be defined as “health-related services and systems, carried out over a distance by means of information and communications technologies, for the purpose of global health promotion, disease control and healthcare” (WHO 1998, p. 1). Since Internet access and use advance constantly (Internet Society 2016), Internet-delivered interventions may be widely accessible and can be administered cost-effectively, with less organizational or local limitations (Hedman et al. 2011; Nordgren et al. 2014). Furthermore, meta-analytic evidence proves the effectiveness of eHealth interventions in mental health promotion (Andersson et al. 2013; Barak et al. 2008) and even suggests a comparative efficacy in comparison with face-to-face interventions (Cuijpers et al. 2010).
However, digital interventions addressing work-related distress and its interactions with mental health problems are underrepresented yet. Summarized as occupational e-mental-health (OEMH), these interventions may comprise preventive or curative interventions, including psychoeducation, health risk assessment, workplace health promotion or return-to-work assistance (Lehr et al. 2016a). Examples of previous studies include a psychodynamic web-based aftercare supporting return-to-work of former inpatients (Zwerenz et al. 2017), self-help for employees with sleep-problems (Thiart et al. 2015), stress management (Ebert et al. 2016) or focus on particular occupational groups (Lehr et al. 2016b). In a recent meta-analysis of 26 studies, Heber et al. (2017) identified a moderate effectiveness of web-based interventions in reducing stress (d = 0.43, 95% CI 0.31–0.54).
However, the implementation of OEMH is still in its early stages. A key precondition to efficient implementation of these technologies is their utilization and adoption by relevant target groups (e.g. help-seekers, health professionals, occupational health management). Studies suggest that individual’s acceptance of new technologies in health care may be critical for their uptake.
Determinants of acceptance of eHealth interventions
Acceptance of eHealth interventions can be considered a highly subjective, internally (e.g. emotional or cognitive perception, self-competence) and externally (e.g. health care or political system, social attitude, technical or institutional resources) driven positive attitude towards their future use. Regarding eHealth interventions for mental health issues, recent surveys demonstrate low acceptance ratings in the general population (Eichenberg et al. 2013; Wallin et al. 2016) or in patient samples (Baumeister et al. 2014, 2015; Ebert et al. 2015). First evidence also suggests low to moderate acceptance of OEMH as an aftercare in inpatients and health professionals of German rehabilitation services (Hennemann et al. 2016, 2017a).
As a well-established theoretical framework, the Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh et al. 2003) operationalizes acceptance as the intention to use technology, which is directly determined by performance expectancy (PE; expected health benefits), effort expectancy (EE; expected usability) and social influence (SI; influence of significant others towards using the technology) and indirectly by facilitating (structural or institutional) conditions. The UTAUT has been adapted to study drivers and barriers to acceptance of eHealth interventions in patients (Ebert et al. 2015; Hennemann et al. 2016) or health professionals (Li et al. 2013; Hennemann et al. 2017a), where studies found positive relations of the postulated predictors with technology acceptance, in particular for performance expectancy.
Furthermore, previous research has established demographic characteristics such as younger age, higher educational or socioeconomic status as predictors of digital health information search or utilization of eHealth interventions (Eichenberg et al. 2013; Kontos et al. 2014). This influence may be mediated through general Internet-orientation, technical competencies (Neter and Brainin 2012) or general treatment motivation. Moreover, knowledge of eHealth interventions has been associated with higher acceptance ratings (Eichenberg et al. 2013; Topooco et al. 2017). Similarly, eHealth literacy, defined as the ability to locate, evaluate, and harness health information in the Internet to cope with health problems (Norman and Skinner 2006), may play a pivotal role in acceptance and adoption of eHealth interventions. In this regard, a survey by Neter and Brainin (2012) points to a ‘digital divide’ of eHealth literacy that reinforces social differences. However, the impact of eHealth literacy on the adoption of eHealth interventions in help-seekers or health professionals has not been studied sufficiently yet.
Regarding the affective determinants of eHealth acceptance, previous studies in patients and health professionals document several reasons for skepticism or rejection of eHealth interventions, including concerns about data security, individuality, therapeutic relationship or limitation of communication (Boonstra and Broekhuis 2010; Hennemann et al. 2017a).
Evidence on the influence of symptom severity on the uptake of eHealth interventions is inconsistent. Ebert et al. (2013) found that work stress was higher in non-participants of a web-based aftercare for psychosomatic inpatients. However, in a transdiagnostic sample of inpatients, Hennemann et al. (2016) could not identify an association of risk for work disability or early retirement or mental health with acceptance of OEMH. Despite the growing body of evidence on implementation strategies of eHealth interventions, no previous study systematically investigated acceptance and barriers to utilization of OEMH in employees.
Objectives
Based on the UTAUT framework, the first aim of the following exploratory cross-sectional study, therefore, was to investigate acceptance defined as behavioral intention to use of OEMH for coping with work-related distress in employees with an elevated risk of early retirement. Second, we were interested in individual barriers and facilitators to acceptance. Based on evidence from previous studies, we postulated positive loadings of UTAUT- and Internet-related predictors (health-related Internet behavior, eHealth literacy) on acceptance. Furthermore, we aimed to explore the influence of mental health, work ability and demographic characteristics on the attitude towards and acceptance of OEMH.
Materials and methods
Study design
Cross-sectional data were collected within the second wave of a large-scale longitudinal cohort survey of employees with health complaints, the “Third German Sociomedical Panel of Employees” (GSPE-III). The GSPE-III was designed to identify environmental and personal risk factors affecting work ability and participation in working life (Bethge et al. 2017). The study population was formed by persons aged 40–54 years with prior sickness absence benefits due to prolonged sick leave (≥ 6 weeks) in 2012 and no utilization of rehabilitation service during the last 4 years. The sample was selected randomly and stratified by gender from the register of the Federal GPIF. Informed consent was obtained from all individual participants. Questionnaires were mailed in July 2015, followed by one reminder within 4 weeks. All procedures involved in the study were approved by the Ethics Committee of the Hannover Medical School (Ref. No. 1730–2013) and by the data protection commissioner of the GPF. The study is registered in the German Clinical Trials Register (DRKS00004824).
Acceptance of OEMH
Based on the UTAUT model, acceptance was operationalized as the intention to use OEMH. Following a short introduction on OEMH interventions and their application to work-related distress, acceptance was measured by two items (see Table 1), which were adapted from previous studies (Baumeister et al. 2014; Ebert et al. 2015; Hennemann et al. 2016). Answers were rated on 5-point scales (1 = “totally disagree” to 5 = “totally agree”), with higher scores indicating elevated acceptance. A mean score was calculated across the items. Reliability was calculated as Cronbach’s alpha (α) or Spearman–Brown (ρ) for two-item scales according to the recommendations by Eisinga et al. (2013). Reliability of the acceptance scale was ρ = 0.83.
Determinants of acceptance
The UTAUT predictors were measured by two items each (see Table 1), based on previous studies in clinical contexts (Baumeister et al. 2014; Ebert et al. 2015; Hennemann et al. 2016). Again, answers were rated on a 5-point scale (1 = “totally disagree” to 5 = “totally agree”) and mean scores were calculated for each predictor. Reliabilities of the scales were satisfactory (PE: ρ = 0.80, SI: ρ = 0.63) except for EE (ρ = 0.44).
eHealth literacy was assessed with two items (see Table 1) from the 8-item German adaption of the eHealth literacy scale (eHEALS) (Soellner et al. 2014). Previous research by Norman and Skinner (2006) showed a high internal consistency of α = 0.88. Answers were rated on a 5-point scale (1 = “strongly disagree” to 5 = “strongly agree”). Items were selected regarding high factor loadings and assignment to the latent factors (information-seeking, information-appraisal) according to Soellner et al. (2014). A mean score across the items was calculated with higher values indicating a higher level of eHealth literacy. Reliability of the composite scale was ρ = 0.79 in this study.
As an indicator of workers’ health, we used the Work Ability Index (WAI) (Tuomi et al. 2001). The WAI assesses work ability on seven dimensions: (1) current work ability compared with the lifetime best, (2) work ability in relation with the demands of the job, (3) number of current diseases diagnosed by a physician, (4) estimated work impairment due to diseases, (5) sick leave during the past year, (6) own prognosis of work ability 2 years from now and (7) mental resources. The WAI score varies from 7 to 49 with higher scores indicating better work ability (7–27 = poor work ability, 28–36 = moderate work ability, 37–43 = good work ability, 44–49 = very good work ability). In a previous study, internal consistency of the WAI proved to be high (α = 0.84) (Bethge and Radoschewski 2010). Cronbach’s alpha was α = 0.69 in this study.
Mental health was operationalized through the mental health index of the German version of the Short Form Health Survey (SF-36; Morfeld et al. 2011). The scale comprises five items on the frequency of positive/negative mental states (e.g. “How much of the time during the past 4 weeks have you felt so down in the dumps that nothing could cheer you up?”) rated on a 6-point scale (1 = “always” to 6 = “never”). Items are recoded into a 0–100 range, with higher values indicating a more favorable mental health state (Hays et al. 1993).Cronbach’s alpha of the index was α = 0.90 in this study.
The frequency of online health information search was assessed in one item, with answers ranging on a 5-point scale from 1 = “never” to 5 = “always”. Participants could specify daily online time in leisure time in minutes. In a nested item, knowledge of (existing vs. non-existing) and prior experience (yes vs. no) with eHealth interventions in general was evaluated, based on a previous survey by Eichenberg et al. (2013) (see Table 1). Sociodemographic characteristics included sex, age, level of education, employment status, type of work, self-reported medical diagnoses and migration background. The latter was identified through foreign place of birth (self or parent), mother tongue, or nationality.
Statistical analyses
The data were analyzed using IBM SPSS Statistics 23 and Mplus 7. Eligible for analyses were participants with current employment and Internet usage. Listwise deletion was performed on missing data in UTAUT variables (0.5–3.6%). Mean scores on aggregated UTAUT and eHEALS items were obtained. Acceptance was further categorized by triparting the mean score into low (1–2.34), moderate (2.35–3.67) and high (3.68–5) values and the frequency of each category was calculated. The acceptance score was differentiated regarding dummy coded demographic variables: sex (male vs. female), level of education (low vs. moderate vs. high), migration background (yes vs. no), employment status (employed vs. unemployed), type of work (mentally vs. physically demanding vs. both), medical diagnoses (mental disorder vs. somatic disease vs. no disease), and experience with eHealth interventions (yes vs. no) using ANOVA or independent t-tests. When the assumption of variance homogeneity was violated, Welch’s F-ratio was calculated.
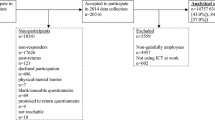
Before entering the predictive model of OEMH acceptance, bivariate correlations between additional variables and UTAUT variables were tested. Since age range was restricted due to sampling criteria and was not significantly correlated with any UTAUT variable, it was excluded from further analyses. We allowed for covariation between additional variables with substantial zero-order correlations (p < 0.001, see online resource 1 and Fig. 1). We conducted separate analyses for the predictive model of acceptance of OEMH. A path analysis was conducted for the subgroup without prior experience with eHealth interventions (n = 1615). Direct effects of UTAUT predictors, as well as direct and indirect effects of additional variables on acceptance (see Fig. 1, left), were analyzed using complete cases and manifest variables (i.e. no latent variables were specified in the presented model). UTAUT predictors served as mediators of additional predictors. Since the data were non-normally distributed, missing cases were observed and the dependent variables were continuous, we used maximum likelihood estimation with robust standard errors (MLR) as a robust and efficient estimator (Yuan and Bentler 2000). Models were analyzed using absolute (χ 2, RMSEA) and incremental (CFI, TLI, SRMR) fit indices that were classified following the interpretation guidelines of Hu and Bentler (1999). Standardized estimates are reported. Employees with self-rated prior experience (n = 111) were analyzed with a separate hierarchical regression model, where predictors were included blockwise: (1) sociodemographic variables, (2) health and work-related variables (work ability, mental health), (3) Internet-related variables, and (4) UTAUT predictors. Listwise deletion was used, leaving n = 94 data sets. The path analytic model is depicted in Fig. 1.
Results
Participants
2233 out of 3294 participants (67.8%) returned completed questionnaires. Non-responders differed from responders in some variables, although effect sizes were marginal: non-responders were more likely to be male (p < 0.001, Cramer’s V = 0.06), less educated (p < 0.001, Cramer’s V = 0.11), non-working (p < 0.001, Cramer’s V = 0.09) and showed poorer mental health (p = 0.03, SMD = 0.08). 229 participants with current unemployment or missing indicator of employment status (n = 20) and non-Internet users (n = 155) were excluded from further analysis. Acceptance of OEMH did not differ between employed (M = 2.15, SD = 1.05) and unemployed individuals (M = 2.07, SD = 1.05), t(2129) = − 1.15, p = 0.25. As expected, non-Internet users (M = 1.59, SD = 0.83) showed lower acceptance ratings than Internet users (M = 2.21, SD = 1.05) t(2087) = − 7.52, p < 0.001. Participant flow is depicted in Fig. 2. The sample thus included 1007 (55.1%) female and 822 (44.9%) male employees with a mean age of 49.93 years (SD = 4.06). Mean daily online time was 45.50 min (SD = 47.50). Out of 1822, 281 (15.4%) participants indicated low, 1103 (60.5%) medium and 438 (24.0%) high education level. Out of 1823 participants, 1229 (67.5%) reported using the internet “sometimes” to “always” for information about health issues. Only 111 (6.2%) out of 1804 participants indicated prior use of eHealth interventions and 766 (42.5%) indicated no prior knowledge of eHealth interventions.
Acceptance of OEMH
Overall observed acceptance of OEMH was low (n = 1772, M = 2.20, SD = 1.05). Only about one in ten participants reported high acceptance, while 89.1% (n = 1579) showed low-to-moderate acceptance (see Fig. 3). The acceptance score was significantly higher in male participants, t(1770) = 4.11, p < 0.001 and followed a quadratic trend in educational status, with highest scores in the high education subgroup (Welch’s F(2,1762) = 5.24, p = 0.005). Furthermore, acceptance scores were significantly higher in participants who indicated prior experience with eHealth interventions (n = 105, t(116.61) = − 11.89, p < 0.001) and lower in participants who indicated a diagnosis of a mental disorder (n = 449, t(1770) = − 1.81, p = 0.07). No differences existed regarding migration background, t(1690) = − 1.64, p = 0.10. Acceptance ratings differed between types of work with higher acceptance in mentally demanding work type (n = 105, Welch’s F(2,279.09) = 18.71, p < 0.001). However, post hoc analysis (Games-Howell) only indicated a significant difference between mentally demanding (n = 984) and both mentally/physically (n = 683) demanding type of work, p < 0.001. No group differences in acceptance ratings were found for type of medical diagnosis, F(2,1769) = 1.67, p = 0.19. Subgroup data and analyses of acceptance ratings can be found in online resource 2.
Barriers and facilitators of OEMH acceptance
Scores on the UTAUT predictors indicated low-to-moderate PE (n = 1758, M = 2.29, SD = 0.95), SI (n = 1759, M = 2.31, SD = 0.89) and EE (n = 1767, M = 2.71, SD = 0.93). eHealth literacy was above average (n = 1802, M = 3.24, SD = 0.84). The WAI total score was ‘moderate’ on average (n = 1767, M = 34.81, SD = 8.20). The mental health index of the SF-36 was in the medium range of the valuation (n = 1808, M = 65.91, SD = 19.98), as was the frequency of online health information search (M = 2.86, SD = 0.96).
As expected, the path model for non-eHealth-experienced employees (n = 1615) yielded significant and positive direct effects on acceptance for all three UTAUT predictors: PE (0.48, SE = 0.02, p < 0.001), EE (0.20, SE = 0.02, p < 0.001), SI (0.28, SE = 0.02, p < 0.001). Explained variance of OEMH acceptance was high, R 2 = 0.73 (SE = 0.01, p < 0.001). Covariation of UTAUT predictors was moderate to high (see online resource 3). Contrary to our hypothesis, eHealth literacy did not predict acceptance directly (− 0.03, SE = 0.01, p = 0.054). Mental health (− 0.01, SE = 0.02, p = 0.57) and work ability (− 0.01, SE = 0.02, p = 0.74) yielded no significant direct effects on acceptance. Online time (0.05, SE = 0.01, p < 0.001) and online health information search (0.05, SE = 0.02, p < 0.001) could be identified as further significant direct predictors of acceptance.
Online health information search, work ability and sex showed significant loadings on all UTAUT predictors. Online time demonstrated significant positive loadings on PE and EE. Mental health scores demonstrated significant negative loadings on PE and SI. Higher education, male sex and migration background were associated with higher ratings in the UTAUT predictors. Significant total indirect effects on acceptance through the UTAUT predictors could be observed for all additional variables except for eHealth literacy, ranging from 0.04 (SE = 0.02, p = 0.03) for migration background to 0.21 (SE = 0.02, p < 0.001) for online health information search. However, educational status and migration background did not yield significant total effects (0.03, SE = 0.03, p = 0.2, resp. 0.03, SE = 0.02, p = 0.17). Table 2 contains the direct and indirect effects of additional variables for non-eHealth-experienced employees (n = 1615). Detailed model estimates can be found in online resource 3.
Overall, model fit was good according to recommendations by Hu and Bentler (1999). χ 2-test was insignificant, χ 2(7) = 12.91, p = 0.07. RMSEA [0.02, 90% CI (0.00; 0.04)] and SRMR (0.01) were below 0.05. CFI (0.99) and TLI (0.99) were above 0.97.
A separate hierarchical linear regression in employees who indicated prior eHealth experience (n = 94) yielded similar results: In the complete model (4), all UTAUT predictors showed significant positive associations with acceptance (PE: β = 0.41, p < 0.001; EE: β = 0.34, p < 0.001; SI: β = 0.21, p < 0.01). However, out of the additional predictors, only online health information search was significantly related to acceptance (β = 0.13, p = 0.05). Consequently, explained variance was highest in the complete model including UTAUT variables (R 2 = 0.79, F(11,82) = 27.18, p < 0.001) in comparison with sociodemographic (R 2 = 0.01, F(3,90) = 0.16, p = 0.92), health-related (R 2 = 0.02, F(5,88) = 0.34, p = 0.89) and internet-related (R 2 = 0.25, F(8,85) = 3.55, p < 0.001) predictor sets.
Discussion
The prevention of work-related mental and somatic health complaints, sick leave and early retirement represents a major challenge in occupational health. Based on the UTAUT (Venkatesh et al. 2003) and further validated constructs, the present study investigated acceptance and person-centered barriers to potential uptake of OEMH as a promising preventive instrument for work-related distress in a large sample of employees with an elevated risk of early retirement.
The behavioral intention to use OEMH in those at risk of early retirement was low. Only about 11% of the participants indicated a substantial acceptance of OEMH interventions in general. Interestingly, this proportion corroborates previous studies based on the UTAUT investigating acceptance of e-mental health in various patient samples, with proportions ranging from 14 to 18% (Baumeister et al. 2014, 2015; Ebert et al. 2015; Hennemann et al. 2016). Further evidence points to an even lower acceptance in representative surveys in the general population, ranging from 9% in an Australian (Gun et al. 2011) to 8% in a German sample (Eichenberg et al. 2013). It thus can be concluded, that around one in ten persons of various target groups demonstrates substantial intention to use eHealth interventions for mental health problems. If the well-known intention–behavior gap is taken into account (Bhattacherjee and Sanford 2009), actual utilization might be limited even more. This becomes relevant when the reach of interventions for occupational health is scaled to a public health level. A follow-up study should thus investigate the actual usage of OEMH longitudinally.
Acceptance of OEMH may have been influenced by attitudes towards mental health resources in general. Since acceptance of the latter may be still limited on a societal level (Corrigan 2004), future research should include a broader perspective on attitudes towards various forms of (occupational) mental health services. However, the flexibility and accessibility of OEMH may also contribute to lowering thresholds towards other mental health resources.
In an effort to identify barriers or facilitators to OEMH acceptance, we used a complex path model including UTAUT predictors as mediators of additional Internet-related, psychological, work-related and demographic variables. Consistent with previous evidence (Hennemann et al. 2016; Liu et al. 2015; Taiwo and Downe 2013), PE was the strongest predictor of acceptance and was significantly associated with all additional predictors. It seems paramount to facilitate positive outcome expectancies and to translate the compelling body of evidence on the efficacy of eHealth interventions in various contexts into public knowledge. In face-to-face psychotherapy, outcome expectancies have even been associated with actual outcome (Constantino et al. 2011). EE and SI exerted a somewhat smaller influence on acceptance, which is consistent with prior research (Hennemann et al. 2017b; Taiwo and Downe 2013). However, present data support the importance of interpersonal attitude formation towards eHealth interventions (Hennemann et al. 2016; Menachemi et al. 2007). In the technology adoption process, PE and SI have been shown to be sustained predictors of technology use, while the influence of EE declines with ongoing utilization (Venkatesh and Davis 2000). Future developers are thus encouraged to take a systemic perspective of technology adoption, including relevant mediators or OEMH champions and to consider practical aspects of technology implementation in every day (work-) lives.
Acceptance ratings were indirectly and positively influenced by work ability, suggesting an association between positive attitudes towards OEMH and a potential need for support in work stress. This finding mirrors evidence from Ebert et al. (2013), who found reduced outcome expectancies in occupationally distressed non-participators of an online-aftercare for psychosomatic inpatients. Furthermore, we found that the level of mental health or mental disorder did not represent direct barriers to the intention to use OEMH and that expectancies regarding usability and social influence were more positive in employees with lower mental health levels. These results encourage implementation of OEMH for various levels of mental distress and in high-risk groups with more severe mental health conditions, in particular, that are still insufficiently targeted by most eHealth interventions.
In line with previous evidence, a set of Internet-related and demographic predictors were positively and directly associated with acceptance. Internet use and online health information search were associated with higher acceptance, underlining previous research on the significance of Internet behavior for the acceptance of eHealth interventions (Eichenberg et al. 2013). Our finding that two-thirds stated regular use of the Internet for health information and the proportion of participants with some form of experience with eHealth interventions corroborates previous evidence of population-based surveys (Eichenberg et al. 2013; Gun et al. 2011). Internet use was lower in the present sample than in representative surveys in comparable age groups (Koch and Frees 2016) and was statistically independent of eHealth literacy. The effect of eHealth literacy was somewhat ambiguous and only indirectly associated with acceptance through PE. However, employees indicated high eHealth literacy, including knowledge and differentiability of eHealth interventions, which is comparable to a recently studied inpatient sample (Hennemann et al. 2016).
The present study found higher acceptance of OEMH in male employees but no direct effect of sex in the predictive models. Evidence on gender effects in technology acceptance and adoption is inconclusive: while some evidence points to a technology friendly orientation in males (Hennemann et al. 2016; Menachemi and Brooks 2006), other studies could not identify gender differences in acceptance of eHealth interventions (Eichenberg et al. 2013). In a representative survey in the United States, Wang et al. (2005) could show that males are more likely to receive adequate mental health care than women. To increase access to effective occupational health instruments, it thus seems important to facilitate positive attitudes towards OEMH in female employees. Baumeister et al. (2014), for example, could demonstrate in this regard, that a short-video-based introductory course on eHealth interventions could increase acceptance in female diabetes patients in particular. Consistent with previous findings (Eichenberg et al. 2013; Hennemann et al. 2016), higher education level was positively associated with acceptance of OEMH. Interestingly, this was only partly mirrored in job demands, where only the mentally demanding type of work significantly differed from a mixture of mentally and physically demanding labor. Together these results underline the need to address less-educated subgroups and efforts to include these in OEMH trials. To our knowledge, this study is one of the first to investigate the role of migration background on acceptance of eHealth interventions. Employees indicated comparable acceptance ratings independent of migration background. However, since migration background is a highly complex construct, more research is advised to further investigate the relationship with the adoption of OEMH. This finding may also reinforce the development of multilingual and culture-sensitive OEMH.
Practical implications and future research
Previous research has demonstrated the efficacy of short video- or text-based introductory courses about application, usability, effectiveness or security of eHealth interventions in increasing acceptance and positive attitudes in patients (Baumeister et al. 2015; Ebert et al. 2015) as well as in health professionals (Donovan et al. 2015). According to Dockweiler (2016), starting points for increasing acceptance and lowering access barriers to OEMH in risk populations may be threefold: First, the intervention itself needs to be addressed, regarding the development of user-friendly and user-oriented eHealth interventions, considering performance and effort expectancies of potential users. Optimally, this process should include users and health professionals (Yardley et al. 2015). Introductory courses to familiarize users with the intervention are also advised when implementing OEMH in institutional settings. However, more research is needed to identify differentiated strategies in the indication for and moderators of efficacy in OEMH. Second, accounting for the person-level requires translating existing evidence of applicability, privacy protection, or risks and potentials of eHealth interventions into the workplace, to enable a comprehensive and informed attitude formation. Education in eHealth interventions could also help establish a realistic perception of OEMH as an extension to, rather than a replacement for existing instruments in occupational health. Third, external drivers to adoption should be incorporated. Beyond the focus of the present study, this may include a conducive organizational culture and further social, cultural, economic or legal aspects of the implementation of OEMH as well as guidelines and orientation for future users, providers and developers (Klein et al. 2016).
Limitations
However, when interpreting the results, several limitations should be considered. First, these concern psychometric properties and construct validity of the UTAUT operationalization. The inclusion of a neutral category in the UTAUT scales, as recommended in the original study by Venkatesh et al. (2003), may have produced a tendency to the mean, resulting in limited variance of values. Also, for economic reasons of this multi-purpose panel, UTAUT predictors were operationalized with only two items, restricting interpretability of reliability (Eisinga et al. 2013). Reliabilities of the UTAUT predictors were satisfactory, except for EE. Here, the inclusion of an inversely coded item may have reduced reliability. Due to the cross-sectional design of this study, caution is advised when interpreting causal direction of the model variables. With cognitive aspects of attitude formation dominating in the UTAUT, affective aspects of attitudes (e.g. concerns, skepticism) may have not been sufficiently covered in the present study. The four-dimensional questionnaire “Attitudes toward psychological online interventions” (Schröder et al. 2015), for example, further substantiates emotional concerns assessing “confidence in effectiveness” or “scepticism and perception of risks” (p. 140). Also, the UTAUT does not differentiate motivational or volitional aspects of attitude formation. Future research may thus include process models, such as the Health Action Process (HAPA) model (Schwarzer 2008), to expand types and levels of acceptance. Furthermore, it could be argued that the rather broad operationalization of UTAUT constructs ensured applicability to various contexts to the disadvantage of a more specific interpretability. For example, social influence could be expanded to the workplace (e.g. colleagues, supervisors, occupational physicians) and specific aspects of work-related distress and applications of OEMH (e.g. preventive, curative, resource-oriented) should be differentiated in future studies on the preconditions of OEMH implementation.
Second, generalization to other welfare and occupational health systems may be limited due to the specific sample characteristics (risk population, age range, employed, Internet users) and possible selection effects as reflected in minor differences between responders and non-responders regarding sex, educational or employment status, corroborating previous evidence on the relevance of demographic characteristics in eHealth acceptance and uptake (Eichenberg et al. 2013; Kontos et al. 2014). However, acceptance of OEMH proved to be low and independent of employment status, type of work (when contrasting predominantly mental vs. physical job demands) or medical diagnoses, indicating the generalizability of the present risk sample.
Third, since the focus of this study was on OEMH for perceived work-related distress, job demands and work stress were not evaluated specifically. Future research should thus include not only the assessment of job demands (e.g. work overload, personal conflicts) but also job resources (e.g. task-oriented, interpersonal, organizational) in an effort to explore further barriers and facilitators to OEMH acceptance. It is worth highlighting, that the response rate of the present study (68%) was high. In contrast to previous surveys in the general or patient populations, the present study is among the first to investigate mechanisms of adoption of OEMH in a large risk group of German employees and was able to prove the applicability and model fit of a complex well-grounded research model.
Conclusions
Employees with an elevated risk of early retirement have reservations towards utilization of OEMH for work-related distress that are similar to other target groups in previous research. Adverse expectancies, reduced health related Internet-orientation and deficient information about eHealth interventions may be important barriers to adoption of OEMH. Although Internet- and mobile technologies are becoming more convenient, attitudes towards their usefulness and usability have shown to be rather independent of technological progress (Gauck 2012) and thus need to be considered in the future development and implementation of OEMH. eHealth interventions may not only save costs in the health care sector (Bernnat et al. 2017), but also in occupational health as they have the potential to extend existing instruments in the prevention of work-related mental and somatic health issues and increase the reach of occupational health in relevant risk groups.
Abbreviations
- ACC OEMH:
-
Acceptance of occupational e-mental-health
- ANOVA:
-
Analysis of variance
- EE:
-
Effort expectancy
- eHEALS:
-
eHealth literacy scale
- CFI:
-
Comparative fit index
- GPIF:
-
German pension insurance fund
- GSPE:
-
German sociomedical panel of employees
- HAPA:
-
Health Action Process Model
- OEMH:
-
Occupational e-mental-health
- PE:
-
Performance expectancy
- MLR:
-
Maximum likelihood estimation with robust standard errors
- RMSEA:
-
Root mean square error of approximation
- SF-36:
-
Short form (36) health survey
- SI:
-
Social influence
- UTAUT:
-
Unified theory of acceptance and use of technology
- WAI:
-
Work ability index
References
Andersson G, Carlbring P, Ljótsson B, Hedman E (2013) Guided internet-based CBT for common mental disorders. J Contemp Psychother 43(4):223–233
Apfel T, Riecher-Rössler A (2005) Do psychiatric patients receive disability pension before adequate diagnostics and treatment? Evaluation of 101 psychiatric expertises done on behalf of the Swiss invalidity insurance at the psychiatric outpatient department basel in 2002. Psychiatr Prax 32(04):172–176
Barak A, Hen L, Boniel-Nissim M, Shapira N (2008) A Comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. J Technol Hum Ser 26(2–4):109–160
Baumeister H, Nowoczin L, Lin J, Seifferth H, Seufert J, Laubner K, Ebert DD (2014) Impact of an acceptance facilitating intervention on diabetes patients’ acceptance of Internet-based interventions for depression: a randomized controlled trial. Diabetes Res Clin Pract 105(1):30–39
Baumeister H, Seifferth H, Lin J, Nowoczin L, Lüking M, Ebert D (2015) Impact of an acceptance facilitating intervention on patients’ acceptance of internet-based pain interventions: a randomized controlled trial. Clin J Pain 31(6):528–535
Bernnat R, Bauer M, Schmidth H, Bieber N, Heusser N, Schönfeld R (2017) Effizienzpotenziale durch eHealth: Studie im Auftrag des Bundesverbands Gesundheits-IT—bvitg. e.V. und der CompuGroup Medical SE. https://www.strategyand.pwc.com/media/file/Effizienzpotentiale-durch-eHealth.pdf. Accessed 03 July 2017
Bethge M, Radoschewski FM (2010) Physical and psychosocial work stressors, health-related control beliefs and work ability: cross-sectional findings from the German Sociomedical Panel of Employees. Int Arch Occup Environ Health 83(3):241–250
Bethge M, Radoschewski FM, Müller-Fahrnow W (2009) Work stress and work ability: cross-sectional findings from the German sociomedical panel of employees. Disabil Rehabil 31(20):1692–1699
Bethge M, Spanier K, Peters E, Michel E, Radoschewski M (2017) Self-reported work ability predicts rehabilitation measures, disability pensions, other welfare benefits, and work participation: longitudinal findings from a sample of german employees. J Occup Rehabil. http://doi.org/10.1007/s10926-017-9733-y
Bhattacherjee A, Sanford C (2009) The intention–behaviour gap in technology usage: the moderating role of attitude strength. Behav Inf Technol 28(4):389–401
Boonstra A, Broekhuis M (2010) Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res 10:231
Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ (2011) Expectations. J Clin Psychol 67(2):184–192
Corrigan P (2004) How stigma interferes with mental health care. Am Psychol 59(7):614
Cuijpers P, Donker T, van Straten A, Li J, Andersson G (2010) Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med 40(12):1943–1957
Deutsche Rentenversicherung (2017) Rehabilitation report. Update 2016. http://bit.ly/2vpmBOI. Accessed 04 July 2017
Deutsche Rentenversicherung Bund (2014) Position paper of the German pension insurance fund on the significance of mental illness in rehabilitation and reduction in earning capacity. http://www.deutsche-rentenversicherung.de/cae/servlet/contentblob/339288/publicationFile/64601/pospap_psych_Erkrankung.pdf. Accessed 24 July 2017
Dockweiler C (2016) Acceptance of telemedicine. In: eHealth in Germany. Springer, Berlin, pp 257–271
Donovan CL, Poole C, Boyes N, Redgate J, March S (2015) Australian mental health worker attitudes towards cCBT: what is the role of knowledge? Are there differences? Can we change them? Internet Interv 2(4):372–381
Ebert D, Tarnowski T, Gollwitzer M, Sieland B, Berking M (2013) A transdiagnostic internet-based maintenance treatment enhances the stability of outcome after inpatient cognitive behavioral therapy: a randomized controlled trial. Psychother Psychosom 82(4):246–256
Ebert DD, Berking M, Cuijpers P, Lehr D, Pörtner M, Baumeister H (2015) Increasing the acceptance of internet-based mental health interventions in primary care patients with depressive symptoms. A randomized controlled trial. J Affect Disord 176:9–17
Ebert DD, Heber E, Berking M, Riper H, Cuijpers P, Funk B, Lehr D (2016) Self-guided internet-based and mobile-based stress management for employees: results of a randomised controlled trial. Occup Environ Med 73(5):315–323
Eichenberg C, Wolters C, Brähler E (2013) The Internet as a mental health advisor in Germany—results of a national survey. PLoS One 8(11):e79206
Eisinga R, Grotenhuis M, Pelzer B (2013) The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? Int J Public Health 58(4):637–642
Frese M (1999) Social support as a moderator of the relationship between work stressors and psychological dysfunctioning: a longitudinal study with objective measures. J Occup Health Psychol 4(3):179–192
Gauck J (2012) DIVSI milieu-study on trust and security in the Internet. https://www.divsi.de/publikationen/studien/divsi-milieu-studie-zu-vertrauen-und-sicherheit-im-internet-aktualisierung-2013/einfuhrung/. Accessed 11 July 17
Gjesdal S, Ringdal PR, Haug K, Mæland JG (2004) Predictors of disability pension in long-term sickness absence: results from a population-based and prospective study in Norway 1994–1999. Eur J Public Health 14(4):398–405
Gun SY, Titov N, Andrews G (2011) Acceptability of Internet treatment of anxiety and depression. Australas Psychiatry 19(3):259–264
Hays RD, Sherbourne CD, Mazel RM (1993) The rand 36-item health survey 1.0. Health Econ 2(3):217–227
Heber E, Ebert DD, Lehr D, Cuijpers P, Berking M, Nobis S, Riper H (2017) The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. J Med Internet Res 19(2):e32
Hedman E, Andersson E, Ljotsson B, Andersson G, Ruck C, Lindefors N (2011) Cost-effectiveness of Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: results from a randomized controlled trial. Behav Res Ther 49(11):729–736
Henderson M, Harvey SB, Øverland S, Mykletun A, Hotopf M (2011) Work and common psychiatric disorders. J R Soc Med 104(5):198–207
Hennemann S, Beutel ME, Zwerenz R (2016) Drivers and barriers to acceptance of web-based aftercare of patients in inpatient routine care: a cross-sectional survey. J Med Internet Res 18(12):e337
Hennemann S, Beutel ME, Zwerenz R (2017a) ‘Morbus Google’ vs. e-Health: a qualitative study of acceptance and implementation of online-aftercare in inpatient rehabilitation. Rehabilitation (Stuttg). http://doi.org/10.1055/s-0043-102150
Hennemann S, Beutel ME, Zwerenz R (2017b) Ready for eHealth? Health professionals’ acceptance and adoption of ehealth interventions in inpatient routine care. J Health Commun 22(3):274–284
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6(1):1–55
Internet Society (2016) Global Internet Report. http://bit.ly/2fQDYzm. Accessed 15 Feb 2017
Karpansalo M, Manninen P, Kauhanen J, Lakka TA, Salonen JT (2004) Perceived health as a predictor of early retirement. Scand J Work Environ Health 30(4):287–292
Klein JP, Gerlinger G, Knaevelsrud C, Bohus M, Meisenzahl E, Kersting A, Röhr S, Riedel-Heller SG, Sprick U, Dirmaier J (2016) Internet-based interventions in the treatment of mental disorders. Overview, quality criteria perspectives. Der Nervenarzt 87(11):1185–1193
Koch W, Frees B (2016) Results of the ARD/ZDF online study 2016: Dynamic developement in mobile Internet use and in audio/video. Media Perspektiven 9(2016):418–437
Kontos E, Blake DK, Chou SW, Prestin A (2014) Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J Med Internet Res 16(7):e172
Lehr D, Geraedts A, Asplund RP, Khadjesari Z, Heber E, Bloom J de, Ebert DD, Angerer P, Funk B (2016a) Occupational e-mental health: current approaches and promising perspectives for promoting mental health in workers. Healthy at work. Springer, Berlin, pp 257–281
Lehr D, Heber E, Sieland B, Hillert A, Funk B, Ebert DD (2016b) Occupational eMental Health and teachers’ health: a meta-analytic review on the efficacy of internet-based intervention for promoting mental health in teachers. Prävention Gesundheitsförderung 11(3):182–192
Li J, Talaei-Khoei A, Seale H, Ray P, MacIntyre CR (2013) Health care provider adoption of eHealth: systematic literature review. Interact J Med Res 2(1):e7
Liu L, Miguel Cruz A, Rios Rincon A, Buttar V, Ranson Q, Goertzen D (2015) What factors determine therapists’ acceptance of new technologies for rehabilitation—a study using the unified theory of acceptance and use of technology (UTAUT). Disabil Rehabil 37(5):447–455
Menachemi N, Brooks RG (2006) EHR and other IT adoption among physicians: results of a large-scale statewide analysis. J Healthc Inf Manag 20(3):79–87
Menachemi N, Langley A, Brooks RG (2007) The use of information technologies among rural and urban physicians in Florida. J Med Syst 31(6):483–488
Morfeld M, Kirchberger I, Bullinger M (2011) SF-36 Questionnaire. German version of the Short Form-36 Health Survey. Hogrefe, Göttingen
Mykletun A, Overland S, Dahl AA, Krokstad S, Bjerkeset O, Glozier N, Aarø LE, Prince M (2006) A population-based cohort study of the effect of common mental disorders on disability pension awards. Am J Psychiatry 163(8):1412–1418
Neter E, Brainin E (2012) eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 14(1):e19
Nordgren LB, Hedman E, Etienne J, Bodin J, Kadowaki Å, Eriksson S, Lindkvist E, Andersson G, Carlbring P (2014) Effectiveness and cost-effectiveness of individually tailored Internet-delivered cognitive behavior therapy for anxiety disorders in a primary care population: a randomized controlled trial. Behav Res Ther 59:1–11
Norman CD, Skinner AH (2006) eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 8(2):e9
Petermann F, Koch U (2009) Psychosomatic rehabilitation: Quo Vadis? Rehabilitation (Stuttg) 48(05):257–262
Schröder J, Sautier L, Kriston L, Berger T, Meyer B, Späth C, Köther U, Nestoriuc Y, Klein JP, Moritz S (2015) Development of a questionnaire measuring Attitudes towards Psychological Online Interventions—the APOI. J Affect Disord 187:136–141
Schwarzer R (2008) Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 57(1):1–29
Soellner R, Huber S, Reder M (2014) The concept of eHealth literacy and its measurement: German translation of the eHEALS. J Media Psychol 26(1):29–38
Stansfeld S, Candy B (2006) Psychosocial work environment and mental health—a meta-analytic review. Scand J Work Environ Health 32(6):443–462
Taiwo AA, Downe AG (2013) The theory of user acceptance and use of technology (UTAUT): a meta-analytic review of empirical findings. J Theor Appl Inf Technol 49(1):48–58
Thiart H, Lehr D, Ebert DD, Berking M, Riper H (2015) Log in and breathe out: internet-based recovery training for sleepless employees with work-related strain—results of a randomized controlled trial. Scand J Work Environ Health 41(2):164–174
Topooco N, Riper H, Araya R, Berking M, Brunn M, Chevreul K, Cieslak R, Ebert DD, Etchmendy E, Herrero R, Kleiboer A, Krieger T, García-Palacios A, Cerga-Pashoja A, Smoktunowicz E, Urech A, Vis C, Andersson G (2017) Attitudes towards digital treatment for depression: a European stakeholder survey. Internet Interv 08:1–9
Tuomi K, Huuhtanen P, Nykyri E, Ilmarinen J (2001) Promotion of work ability, the quality of work and retirement. Occup Med (Lond) 51(5):318–324
Venkatesh V, Davis FD (2000) A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci 46(2):186–204
Venkatesh V, Morris MG, Davis GB, Davis FD (2003) User acceptance of information technology: toward a unified view. MIS Q 27(3):425–478
Wallin EEK, Mattsson S, Olsson EMG, Eysenbach G (2016) the preference for internet-based psychological interventions by individuals without past or current use of mental health treatment delivered online: a survey study with mixed-methods analysis. JMIR Mental Health 3(2):e25
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC (2005) Twelve-month use of mental health services in the united states: results from the national comorbidity survey replication. Arch Gen Psychiatry 62(6):629–640
WHO (1998) A health telematics policy: report of WHO group consultation on health telematics. WHO, Geneva
Yardley L, Morrison L, Bradbury K, Muller I (2015) The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res 17(1):e30
Yuan K, Bentler PM (2000) Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Soc Methodol 30(1):165–200
Zwerenz R, Knickenberg RJ, Schattenburg L, Beutel ME (2004) Work-related stress and resources of psychosomatic patients compared to the general population. Rehabilitation (Stuttg) 43(1):10–16
Zwerenz R, Becker J, Gerzymisch K, Siepmann M, Holme M, Kiwus U, Spörl-Dönch S, Beutel ME (2017) Evaluation of a transdiagnostic psychodynamic online intervention to support return to work: a randomized controlled trial. PLoS One 12(5):e0176513
Acknowledgements
The GSPE-III has been funded by the German Pension Insurance Fund according to § 31 section 1 Nr. 5 SGB VI. The authors would like to thank Julian Thukral for his project assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hennemann, S., Witthöft, M., Bethge, M. et al. Acceptance and barriers to access of occupational e-mental health: cross-sectional findings from a health-risk population of employees. Int Arch Occup Environ Health 91, 305–316 (2018). https://doi.org/10.1007/s00420-017-1280-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-017-1280-5