Abstract
Purpose
The objective of the present study is to investigate the effects of a worksite health promotion intervention on musculoskeletal symptoms, physical functioning, work ability, work-related vitality, work performance, and sickness absence.
Methods
In a randomized controlled design, 314 construction workers were randomized into an intervention group (n = 162) receiving personal coaching, tailored information, and materials, and a control group (n = 152) receiving usual care. Sickness absence was recorded continuously in company records, and questionnaires were completed before, directly after the 6-month intervention period, and 12 months after baseline measurements. Linear and logistic regression analyses were performed to determine intervention effects.
Results
No significant changes at 6 or 12 months of follow-up were observed in musculoskeletal symptoms, physical functioning, work ability, work-related vitality, work performance, and sickness absence as a result of the intervention.
Conclusions
This study shows that the intervention was not statistically significantly effective on secondary outcomes. Although the intervention improved physical activity, dietary, and weight-related outcomes, it was not successful in decreasing musculoskeletal symptoms and improving other work-related measures. Presumably, more multifaceted interventions are required to establish significant change in these outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Workers in the construction industry are often exposed to physically demanding work tasks. These include, amongst others, the lifting of heavy loads and working in awkward postures. High physical work demands increase the risk of the development of musculoskeletal symptoms (da Costa and Vieira 2010; Holtermann et al. 2010). In blue collar construction workers, musculoskeletal disorders (MSD) are the most prevalent work-related health problem (Boschman et al. 2012; Peterson and Zwerling 1998). In addition, in the Netherlands, the workforce in physically demanding work is ageing and the risk of MDS also increases with age (de Zwart et al. 1997; Hildebrandt 1995). As such, MSD are a major cause for sickness absence, work disability, and early exit from work, are related to lower work performance, and consequently constitute an extensive social, medical, as well as economic problem (van den Heuvel et al. 2010; Arndt et al. 2005).
The prevalence of overweight and obesity in construction workers is higher than in the general adult population (Proper and Hildebrandt 2010; Santos and Barros 2003; Arndt et al. 1996). Both MSD and a high BMI are negatively associated with several work-related outcomes, but are also associated with each other (Claessen et al. 2009; Viester et al. 2013; Roos et al. 2013; Robroek et al. 2013; Alavinia et al. 2009). Since both factors are highly prevalent in blue collar construction workers, these might contribute to the high risk of developing health disorders and associated adverse work-related outcomes compared with workers in other industries and the general population (Snashall 1990; Taimela et al. 2007). This emphasizes the importance to reduce the burden of overweight and obesity in this particular group of workers.
Both diet and physical activity are considered of importance in achieving and maintaining a healthy body weight (Swinburn et al. 2003, WHO 2004). Worksite health promotion programmes aimed at physical activity and diet were found to be effective on weight-related outcomes (Verweij et al. 2011; Groeneveld et al. 2010; Anderson et al. 2009). Moreover, workplace health promotion programmes that improve physical activity levels have been shown to also reduce the risk on MSD (Proper et al. 2003). A lifestyle intervention amongst those with jobs involving moderately heavy or heavy work also showed a reduction in prevalence of low back pain (Mattila et al. 2007). Although intervention studies with MSD as primary outcome have not often been targeted at lifestyle factors, there is evidence from observational studies, suggesting that health promotion should be considered in the prevention of MSD (Hildebrandt et al. 2000; Holth et al. 2008; Morken et al. 2007; Burton et al. 2006). Beneficial effects on work-related outcomes, including sickness absence, productivity, and work ability, have been reported resulting from preventative measures targeted at healthy lifestyle (Cancelliere et al. 2011; Proper et al. 2004; Kuoppala et al. 2008; von Thiele Schwarz and Hasson 2012). Consequently, implementation of worksite programmes targeted at lifestyle factors may be a promising strategy to improve worker health and other outcomes relevant to employers.
In the vitality in practice (VIP) in construction study, it was hypothesized that a worksite health promotion intervention, aiming at improving physical activity and diet, could positively change body weight-related outcomes, musculoskeletal symptoms, and work-related measures (Viester et al. 2012). The aim of the present study was to evaluate whether the intervention programme for blue collar construction workers reduced musculoskeletal symptoms, limitations in physical functioning and sickness absence, and increased work-related vitality, work performance and work ability.
Methods
Study design and population
The effectiveness of the programme was assessed in a randomized controlled trial (RCT). The research population consisted of consenting blue collar employees of a construction company. All employees who attended a non-compulsory periodic health screening (PHS) and who were not on sick leave for more than 4 weeks prior to the PHS were eligible for inclusion. In total, 314 participants were recruited over a 15-month period (March 2010–June 2011) and randomized to an intervention (n = 162) or control group (n = 152). Participants completed questionnaires at baseline (T0), at 6 months (T1), and at 12 months (T2). Written informed consent was obtained from participants before enrolment in the study.
The study design and procedures were approved by the Medical Ethics Committee of the VU University Medical Center, and the trial has been registered in the Netherlands Trial Register (NTR, www.trialregister.nl): NTR2095.
Randomization, blinding, and sample size
Following baseline measurements, participants were randomly assigned to either the intervention or the control group by a computer-generated list using SPSS 15 (SPSS Inc. Chicago, Illinois, USA). The randomization was prepared and performed by an independent researcher. Whereas participants could have been aware of the allocated arm, data collectors and analyst were kept blinded to the allocation. The sample size was calculated to identify an effect on body weight (Viester et al. 2012). Based on that calculation, in each study group (intervention and control), 130 participants were needed for follow-up.
Intervention
The intervention programme aimed at the prevention and reduction of overweight and musculoskeletal symptoms and was developed and implemented via the Intervention Mapping protocol (Bartholomew et al. 2006; Viester et al. 2012). The full programme has been described previously (Viester et al. 2012). In short, the intervention consisted of an on-site lifestyle coaching programme tailored to the participant’s weight status (BMI and waist circumference), physical activity level, and stage of change. The intervention programme focused on improving (vigorous) physical activity levels and healthy dietary behaviour. The programme consisted of tailored lifestyle information, lifestyle coaching sessions, exercise instructions, and the ‘VIP in construction toolbox’. This toolbox consisted of an overview of the company’s health promoting facilities, a waist circumference measuring tape, a pedometer, a BMI card, a calorie guide, healthy recipes, and a lifestyle knowledge test.
The intervention was delivered face-to-face and via telephone by personal health coaches (PHC) who were trained specifically for the study. Face-to-face coaching sessions took place at the worksite during working hours. An overview of the timing and duration of the contacts is presented in Table 1. Participants additionally received ‘Personal Energy Plan’ (PEP) forms to record their goals and action plans, and to be used during the follow-up health coaching sessions. Intervention providers were not involved in the outcome assessment.
The control group received care as usual and was only contacted for the baseline and follow-up measurements.
Outcome measures
The present study investigated the effectiveness of the intervention on musculoskeletal symptoms, physical functioning, and work-related outcomes (work ability, work performance, work-related vitality, and sickness absence). Sickness absence data were obtained from the company’s registration system after follow-up measurements were completed. All other data were obtained using questionnaires.
Health-related measures
Musculoskeletal symptoms
The prevalence of musculoskeletal symptoms during the past 3 months was assessed using the Dutch musculoskeletal questionnaire (DMQ), which has been validated for different body regions (Hildebrandt et al. 2001). The occurrence of pain or discomfort was rated on a four-point scale (never, sometimes, frequently, and prolonged). For the current analysis, the measure was dichotomized; answer categories ‘frequently’ and ‘prolonged’ were classified as having musculoskeletal symptoms, whereas categories ‘never’ and ‘sometimes’ were classified as having no musculoskeletal symptoms. Body regions were grouped into back (upper and lower back), neck/shoulders, upper extremities (elbows and wrist/hands), and lower extremities (hips/thighs, knees, and ankle/feet).
Physical functioning
Physical functioning was measured using a subscale of the RAND-36, evaluating functional status (Hays et al. 1993; VanderZee et al. 1996). The RAND-36 cluster on role limitations caused by physical problems consists of 4 items and ranges from 0 to 100 points (higher scores indicating less limitations), with a score of 79.4 considered average (VanderZee et al. 1996). The RAND-36 health survey is a widely adopted, and reliable and valid measurement of health-related quality of life (Brazier et al. 1992). In the present study, the validated Dutch version was used.
Work-related measures
Work ability was assessed with the work ability index (WAI) (Ilmarinen and Tuomi 1993; de Zwart et al. 2002; Nygard et al. 1991). The WAI covers 7 dimensions; current work ability, work ability in relation to job demands, number of current diseases, work impairment due to diseases, sickness absence days during past 12 months, own prognosis of work ability in next 2 years, and mental resources. Total scores over all dimensions range from 7 to 49, with 4 categories: poor (7–27 points), moderate (28–36 points), good (37–43 points), and excellent (44–49 points).
Work-related vitality, defined as vigour, was assessed through a subscale of the Utrecht Engagement Scale (UWES) that refers to high levels of energy and resilience, the willingness to invest effort, not being easily fatigued, and persistence in the face of difficulties (Schaufeli and Bakker 2003). The answers were rated on a seven-point scale from never (0) to daily (6). The mean score of the items resulted in the work-related vitality score, with a higher score indicating a better work-related vitality.
Work performance was measured using a single item from the Health Work Performance Questionnaire (WHO-HPQ)(Kessler et al. 2003, 2004) asking workers to report their overall work performance on a 10-point scale over the past four weeks.
Sickness absence data were collected directly from company records. For the analysis, cumulative sickness absence data over 6-month periods were used (pre-, during-, and post-intervention). Sickness absence has a skewed distribution with a substantial fraction clustered at the value zero. Therefore, sickness absence was dichotomized into no or short-term sickness absence (≤7 days), and long-term sickness absence (>7 days).
Statistical analysis
The analysis was conducted with all available subjects at 6 and 12 months of follow-up. All available data of the participants, regardless of whether or not they actually (fully) received the intervention, were used for analysis. Data on potential confounders and effect modifiers were assessed through the baseline questionnaire and included age, smoking status, education level, and marital status. For all variables, potential baseline differences were checked between intervention and control group.
Linear and logistic regression analyses were performed for the different outcome measures, with both 6- and 12-month follow-up as the dependent variables. Analyses were adjusted for the baseline levels. Analyses were performed using SPSS 20.0 (SPSS Inc. Chicago, Illinois, USA). For all analyses, a two-tailed p value of <0.05 was considered statistically significant.
Results
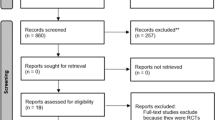
In total, 314 workers responded to the baseline questionnaire. At 12 months of follow-up, 83 % of the participants completed all measurements; 22 workers of the control group (14 %) and 31 workers of the intervention group (19 %) did not complete all follow-up measurements. Figure 1 presents the flow chart of the participants throughout the trial. Baseline characteristics are presented in Table 2. No differences between groups were found for key variables.
Table 3 shows complete case intervention effects on work-related vitality, work performance, work ability, and physical functioning. For all outcome measures, a positive value for B, which represents the estimate (unstandardized coefficient) resulting from the regression analyses, can be interpreted as a positive intervention effect. No statistically significant differences were found for any of the outcome variables after 6 and 12 months of follow-up.
Musculoskeletal symptoms
The intervention did not result in statistically significant effects on musculoskeletal symptoms (Table 4). Although for back symptoms at 6 and 12 months of follow-up (OR 0.69, 95 % CI: 0.36–1.36, and 0.76, 95 % CI: 0.38–1.52, respectively) and lower extremity symptoms at 12 months (OR 0.61, 95 % CI: 0.32–1.16), the odds ratios were in favour of the intervention group, differences reached no statistical significance.
Sickness absence
Table 5 shows mean days of sickness absence in the past 6 months, and Table 3 presents the course of sickness absence for the study group, dichotomized into no or short-term, and long-term sickness absence. Directly following the intervention, the 6-month prevalence of long-term sickness absence was lower in the intervention group than in the control group. At 12 months, sickness absence was slightly higher in the intervention group compared with the control group. However, at both 6 and 12 months, the between-group differences were not statistically significant.
Discussion
The aim of this study was to evaluate the effectiveness on secondary outcomes of a health promotion intervention aiming at increasing physical activity and improving dietary behaviour in construction workers. No significant short- or long-term intervention effects were found on musculoskeletal symptoms, physical functioning, work-related vitality, work performance, work ability, or sickness absence. These findings will be discussed for the different outcome measures.
Musculoskeletal symptoms
The lack of observed statistically significant intervention effects on musculoskeletal symptoms is in line with other intervention studies in the construction sector (Gram et al. 2012a, 2012b; Oude Hengel et al. 2013). Overall in the present study, the prevalence of workers reporting musculoskeletal symptoms declined. For back and lower extremity symptoms, odds ratios were in favour of the intervention group, although not statistically significant. Since sample size calculations were performed to determine effects on the study’s primary outcome measure (body weight), for other outcome measures, the study could have been underpowered.
In the current study, it was hypothesized that an improvement in physical capacity through increased physical activity, and a decrease in workload through a reduction of overweight, would be effective in preventing or reducing musculoskeletal symptoms.
Although it is still not clear what type of exercise should be recommended, several reviews support the use of exercise as an effective strategy for the prevention or treatment of musculoskeletal conditions, including a wide range of interventions, such as increasing general physical activity levels, general exercise, and specific body-region exercises for strength and flexibility (Roddy et al. 2005; Hayden et al. 2005). The current intervention consisted of a combination of exercise prescription and coaching on improving physical activity levels, which implied that participants self-selected their physical activity goals. Although an increase in vigorous physical activity in the intervention group was found, this may not have been exercise or physical activity selected for the purpose to prevent or reduce musculoskeletal symptoms, and might as a result not have been the most appropriate type of activity or exercise to reduce or prevent specific symptoms. Additionally, the increase in physical activity levels may not have led to sufficient physical capacity improvements to be effective on musculoskeletal symptoms.
Presumably, the effects on outcomes related to body weight, as found in this study, were not substantial enough to have a direct effect on MSD. Another explanation could be that the intervention period was not long enough for effects on MSD to occur. However, prevention of body weight gain or reducing excess body weight could have future effects by lowering both systemic and metabolic risk factors. Systemic risk factors include a combination of mechanical load on weight-bearing joints and work postures. Obesity is one of the components of the metabolic syndrome, and metabolic risk factors are increasingly being recognized as a possible cause of MSD (Berenbaum 2013; Sellam and Berenbaum 2013).
To reduce or prevent musculoskeletal symptoms, it has been suggested that multi-component interventions are potentially more effective (Kennedy et al. 2010). In these programmes, exercise or training interventions are combined with components addressing environmental and/or organizational issues. For example, the physical and psycho-social work environment has been recognized as risk factors for MSD in the construction sector. This is supported by findings from interviews with employees during the development of the present study as well as in the study of Oude Hengel et al. (2010), Viester et al. (2012). Combining health and lifestyle promotion with efforts to decrease workload and/or change working conditions is probably necessary for programmes to be effective.
Work-related vitality, physical functioning, work performance, and work ability
In addition to the explanation of the lack of effect as described in the section on musculoskeletal symptoms, the initially high scores for work-related vitality, physical functioning and WAI could explain the lack of further detectable increase in these outcomes, i.e. a ceiling effect. For work-related vitality, this was also found in previous studies (Strijk et al. 2013). The lack of effect on the WAI in the current study is in accordance with previous studies on work ability (Oude Hengel et al. 2013; Nurminen et al. 2002; Pohjonen and Ranta 2001). The average baseline WAI score of 40.7 was only slightly higher compared with the average score of Finnish men in the same age group and engaged in physical work (Ilmarinen et al. 1997), and scores ranging from 37 to 43 are regarded as good work ability. For the physical functioning dimension of the SF-36, baseline values of the study population largely exceeded norm values of a reference population.
Sickness absence
With regard to sickness absence, the lack of effects is in line with other studies amongst blue collar worker (Oude Hengel et al. 2013; Jorgensen et al. 2011). During the trial period, several factors in addition to illness, which are related to sickness absence, may have influenced the results. Not all absence can be attributed to sickness; sickness absence has been associated with, for example, socio-economic factors, organizational features, job content, and attitudes to work (Briner 1996). This is especially of concern when using total sickness absence data, compared with the absence related to a specific condition, such as MSD. The current economic recession that strongly affected the construction sector during the trial period may have distorted effects on total sickness absence or patterns of sickness absence. Stress, increased (perceived) workload, and fear of job loss are factors that might have played a larger role under these circumstances during the study period.
For all outcome measures, the lack of intervention effects can in part be attributed to the level of implementation of the programme. In a process evaluation of the programme, it was concluded that the extent to which the programme was implemented as intended was modest (Viester et al. 2014). Although participants’ satisfaction with the programme and dose delivered by the health coaches was high, exposure and fidelity were not optimal. The compliance to the coaching sessions was acceptable, but the implementation of the exercise component was not successful. Although approximately two thirds of the participants indicated to have done the exercises, only a small percentage exercised regularly as prescribed by the programme.
The trial findings could be applicable to a larger population of manual labour workers. The intervention was implemented in a diverse group of blue collar workers with comparable participation rates for the subunits of the construction company. However, when generalizing the results from the specific setting of the RCT to a larger worker population, it should be taken into account that compared to the original population, older workers were slightly overrepresented in the study population (Viester et al. 2014).
Strengths and limitations
Strengths of the study include the randomized controlled trial design, and obtaining sickness absence data from company records. The use of sickness absence data from company records is preferred since it is more accurate than data gathered via self-report (Ferrie et al. 2005).
Some limitations have to be addressed as well. First, power calculation was performed on the primary outcome measure of the study, i.e. body weight. As a result, group sizes might have been below the required number to establish inter-group differences for other study outcomes. Further, missing data on items of the work ability index resulted in a reduced number of complete cases. For participants who did not complete all 7 items, the index could not be determined. With exception of sickness absence, all outcome measures were obtained using self-report which may lead to overestimation or underestimation of the outcomes. Finally, although contamination of the control group participants was expected to be minimal, since only intervention participants had access to coaching and the toolbox, it could not be completely ruled out. Behaviour change in colleagues working at the same worksites could have influenced control participants.
Implications for practice and future research
Maintaining a healthy and productive workforce depends on a wide variety of factors. It is recommended that future interventions aiming to improve work-related outcomes also include organizational and/or environmental components to more effectively target factors related to work ability and performance.
Theoretically, improving physical capacity (i.e. improving muscle function or increasing oxidative capacity) by increasing physical activity and exercise might prevent or reduce musculoskeletal symptoms. In the present study, we did not include measures to monitor possible effects of increased physical activity levels on physical capacity. To increase knowledge on the relevance of increasing physical capacity in this group of workers and to contribute to insight into optimal type, duration, and intensity of exercise, future studies should include such measures related to physical capacity.
Conclusions
The results of this RCT did not show effects of the programme on musculoskeletal symptoms, physical functioning, work-related vitality, work performance, work ability, or sickness absence. Although the intervention programme improved physical activity levels, dietary outcomes, and weight-related outcomes at 6 months, it was not successful in improving other health-related and work-related outcomes. In conclusion, for all outcome measures in the present paper, it could be argued that they are affected by additional factors to those included in the current conceptual model of the study (Viester et al. 2012). Based on the results of the present study, organizations attempting to improve worker health- and work-related outcomes should provide additional programme components. Although a non-significant decline in musculoskeletal symptoms was observed, without co-intervening on (psycho-social) organizational aspects in a more multifaceted intervention, the potential of improving these outcomes by health promotion is probably limited.
References
Alavinia SM, van den Berg TIJ, van Duivenbooden C, Elders LAM, Burdorf A (2009) Impact of work-related factors, lifestyle, and work ability on sickness absence among Dutch construction workers. Scand J Work Environ Health 35:325–333
Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, Johnson DB, Buchanan LR, Archer WR, Chattopadhyay S, Kalra GP, Katz DL (2009) The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med 37:340–357
Arndt V, Rothenbacher D, Brenner H, Fraisse E, Zschenderlein B, Daniel U, Schuberth S, Fliedner TM (1996) Older workers in the construction industry: results of a routine health examination and a five year follow up. Occup Environ Med 53:686–691
Arndt V, Rothenbacher D, Daniel U, Zschenderlein B, Schuberth S, Brenner H (2005) Construction work and risk of occupational disability: a ten year follow up of 14,474 male workers. Occup Environ Med 62:559–566
Bartholomew LK, Parcel GS, Kok G, Gottlieb NH (2006) Planning health promotion programs: intervention mapping. Jossey-Bass, San Francisco
Berenbaum F (2013) Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr Cartil 21:16–21
Boschman JS, van der Molen HF, Sluiter JK, Frings-Dresen MH (2012) Musculoskeletal disorders among construction workers: a one-year follow-up study. BMC Musculoskelet Disord 13:196
Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Briner RB (1996) ABC of work related disorders. Absence from work. BMJ 313:874–877
Burton AK, Balague F, Cardon G, Eriksen HR, Henrotin Y, Lahad A, Leclerc A, Muller G, van der Beek AJ (2006) Chapter 2. European guidelines for prevention in low back pain. Eur Spine J 15(Suppl 2):S136–S168 November 2004
Cancelliere C, Cassidy JD, Ammendolia C, Cote P (2011) Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 11:395
Claessen H, Arndt V, Drath C, Brenner H (2009) Overweight, obesity and risk of work disability: a cohort study of construction workers in Germany. Occup Environ Med 66:402–409
da Costa BR, Vieira ER (2010) Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med 53:285–323
de Zwart BC, Broersen JP, Frings-Dresen MH, van Dijk FJ (1997) Musculoskeletal complaints in The Netherlands in relation to age, gender and physically demanding work. Int Arch Occup Environ Health 70:352–360
de Zwart BCH, Frings-Dresen MHW, van Duivenbooden JC (2002) Test-retest reliability of the work ability index questionnaire. Occup Med 52:177–181
Ferrie JE, Kivimaki M, Head J, Shipley MJ, Vahtera J, Marmot MG (2005) A comparison of self-reported sickness absence with absences recorded in employers’ registers: evidence from the Whitehall II study. Occup Environ Med 62:74–79
Gram B, Holtermann A, Sogaard K, Sjogaard G (2012a) Effect of individualized worksite exercise training on aerobic capacity and muscle strength among construction workers—a randomized controlled intervention study. Scand J Work Environ Health 38:467–475
Gram B, Holtermann A, Bultmann U, Sjogaard G, Sogaard K (2012b) Does an exercise intervention improving aerobic capacity among construction workers also improve musculoskeletal pain, work ability, productivity, perceived physical exertion, and sick leave? A randomized controlled trial. J Occup Environ Med 54:1520–1526
Groeneveld IF, Proper KI, van der Beek AJ, van Mechelen W (2010) Sustained body weight reduction by an individual-based lifestyle intervention for workers in the construction industry at risk for cardiovascular disease: results of a randomized controlled trial. Prev Med 51:240–246
Hayden JA, van Tulder MW, Malmivaara AV, Koes BW (2005) Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med 142:765–775
Hays RD, Sherbourne CD, Mazel RM (1993) The RAND 36-Item Health Survey 1.0. Health Econ 2:217–227
Hildebrandt VH (1995) Back pain in the working population: prevalence rates in Dutch trades and professions. Ergonomics 38:1283–1298
Hildebrandt VH, Bongers PM, Dul J, van Dijk FJ, Kemper HC (2000) The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health 73:507–518
Hildebrandt VH, Bongers PM, van Dijk FJ, Kemper HC, Dul J (2001) Dutch musculoskeletal questionnaire: description and basic qualities. Ergonomics 44:1038–1055
Holtermann A, Jorgensen MB, Gram B, Christensen JR, Faber A, Overgaard K, Ektor-Andersen J, Mortensen OS, Sjogaard G, Sogaard K (2010) Worksite interventions for preventing physical deterioration among employees in job-groups with high physical work demands: background, design and conceptual model of FINALE. BMC Public Health 10:120
Holth HS, Werpen HKB, Zwart JA, Hagen K (2008) Physical inactivity is associated with chronic musculoskeletal complaints 11 years later: results from the Nord-Trondelag Health Study. BMC Musculoskelet Disord 9:159
Ilmarinen J, Tuomi K (1993) Work ability index for aging workers. Finnish Institute of Occupational Health, Helsinki
Ilmarinen J, Tuomi K, Klockars M (1997) Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health 23(Suppl 1):49–57
Jorgensen MB, Faber A, Hansen JV, Holtermann A, Sogaard K (2011) Effects on musculoskeletal pain, work ability and sickness absence in a 1-year randomised controlled trial among cleaners. BMC Public Health 11:840
Kennedy CA, Amick BC, Dennerlein JT, Brewer S, Catli S, Williams R, Serra C, Gerr F, Irvin E, Mahood Q, Franzblau A, Van Eerd D, Evanoff B, Rempel D (2010) Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J Occup Rehabil 20:127–162
Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, Pronk N, Simon G, Stang P, Ustun TB, Wang P (2003) The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med 45:156–174
Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, Stang PE, Ustun TB (2004) Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med 46:S23–S37
Kuoppala J, Lamminpaa A, Husman P (2008) Work health promotion, job well-being, and sickness absences—a systematic review and meta-analysis. J Occup Environ Med 50:1216–1227
Mattila R, Malmivaara A, Kastarinen M, Kivela SL, Nissinen A (2007) The effects of lifestyle intervention for hypertension on low back pain: a randomized controlled trial. Spine (Phila Pa 1976.) 32:2943–2947
Morken T, Mageroy N, Moen BE (2007) Physical activity is associated with a low prevalence of musculoskeletal disorders in the Royal Norwegian Navy: a cross sectional study. BMC Musculoskelet Disord 8:56
Nurminen E, Malmivaara A, Ilmarinen J, Ylostalo P, Mutanen P, Ahonen G, Aro T (2002) Effectiveness of a worksite exercise program with respect to perceived work ability and sick leaves among women with physical work. Scand J Work Environ Health 28:85–93
Nygard CH, Eskelinen L, Suvanto S, Tuomi K, Ilmarinen J (1991) Associations between functional capacity and work ability among elderly municipal employees. Scand J Work Environ Health 17(Suppl 1):122–127
Oude Hengel KM, Joling CI, Proper KI, Blatter BM, Bongers PM (2010) A worksite prevention program for construction workers: design of a randomized controlled trial. BMC. Public Health 10:336
Oude Hengel KM, Blatter BM, van der Molen HF, Bongers PM, van der Beek AJ (2013) The effectiveness of a construction worksite prevention program on work ability, health, and sick leave: results from a cluster randomized controlled trial. Scand J Work Environ Health 39:456–467
Peterson JS, Zwerling C (1998) Comparison of health outcomes among older construction and blue-collar employees in the United States. Am J Ind Med 34:280–287
Pohjonen T, Ranta R (2001) Effects of worksite physical exercise intervention on physical fitness, perceived health status, and work ability among home care workers: five-year follow-up. Prev Med 32:465–475
Proper KI, Hildebrandt VH (2010) Overweight and obesity among Dutch workers: differences between occupational groups and sectors. Int Arch Occup Environ Health 83:61–68
Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W (2003) The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med 13:106–117
Proper KI, van der Beek AJ, Hildebrandt VH, Twisk JWR, van Mechelen W (2004) Worksite health promotion using individual counselling and the effectiveness on sick leave; results of a randomised controlled trial. Occup Environ Med 61:275–279
Robroek SJ, Reeuwijk KG, Hillier FC, Bambra CL, van Rijn RM, Burdorf A (2013) The contribution of overweight, obesity, and lack of physical activity to exit from paid employment: a meta-analysis. Scand J Work Environ Health 39:233–240
Roddy E, Zhang W, Doherty M (2005) Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis 64:544–548
Roos E, Laaksonen M, Rahkonen O, Lahelma E, Lallukka T (2013) Relative weight and disability retirement: a prospective cohort study. Scand J Work Environ Health 39:259–267
Santos AC, Barros H (2003) Prevalence and determinants of obesity in an urban sample of Portuguese adults. Public Health 117:430–437
Schaufeli WB, Bakker AB (2003) Utrecht work engagement scale. Utrecht University, Utrecht, Occupational Health Psychology Unit
Sellam J, Berenbaum F (2013) Is osteoarthritis a metabolic disease? Joint Bone Spine 80:568–573
Snashall D (1990) Safety and health in the construction industry. BMJ 301:563–564
Strijk JE, Proper KI, van Mechelen W, van der Beek AJ (2013) Effectiveness of a worksite lifestyle intervention on vitality, work engagement, productivity, and sick leave: results of a randomized controlled trial. Scand J Work Environ Health 39:66–75
Swinburn BA, Caterson I, Seidell JC, James WPT (2003) Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr 7:123–146
Taimela S, Laara E, Malmivaara A, Tiekso J, Sintonen H, Justen S, Aro T (2007) Self-reported health problems and sickness absence in different age groups predominantly engaged in physical work. Occup Environ Med 64:739–746
van den Heuvel SG, Geuskens GA, Hooftman WE, Koppes LLJ, van den Bossche SNJ (2010) Productivity loss at work; health-related and work-related factors. J Occup Rehabil 20:331–339
VanderZee KI, Sanderman R, Heyink JW, de Haes H (1996) Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health statusv. Int J Behav Med 3:104–122
Verweij LM, Coffeng J, van MW, Proper KI (2011) Meta-analyses of workplace physical activity and dietary behaviour interventions on weight outcomes. Obes Rev 12:406–429
Viester L, Verhagen EALM, Proper KI, van Dongen JM, Bongers PM, van der Beek AJ (2012) VIP in construction: systematic development and evaluation of a multifaceted health programme aiming to improve physical activity levels and dietary patterns among construction workers. BMC Public Health 12:89
Viester L, Verhagen EALM, Oude Hengel KM, Koppes LLJ, van der Beek AJ, Bongers PM (2013) The relation between body mass index and musculoskeletal symptoms in the working population. BMC Musculoskelet Disord 14:238
Viester L, Verhagen EALM, Bongers PM, van der Beek AJ (2014) Process evaluation of a multifaceted health program aiming to improve physical activity levels and dietary patterns among construction workers. J Occup Environ Med 56:1210–1217
von Thiele Schwarz U, Hasson H (2012) Effects of worksite health interventions involving reduced work hours and physical exercise on sickness absence costs. J Occup Environ Med 54:538–544
World Health Organization (WHO) (2004) Diet, nutrition, and prevention of chronic diseases. WHO, Geneva
Acknowledgments
This project is part of the research programme ‘Vitality in Practice’, which is financed by Fonds Nuts Ohra (Nuts Ohra Foundation).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Viester, L., Verhagen, E.A.L.M., Bongers, P.M. et al. The effect of a health promotion intervention for construction workers on work-related outcomes: results from a randomized controlled trial. Int Arch Occup Environ Health 88, 789–798 (2015). https://doi.org/10.1007/s00420-014-1007-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-014-1007-9