Abstract
Purpose
In workers with musculoskeletal injuries, comorbidity is associated with worse return to work (RTW) outcomes. In the context of RTW, it is unclear whether associations between predictors and RTW are similar or different for workers with and without comorbidity. This study aims to investigate differences and similarities between workers with and without comorbidity in 12-month predictors for RTW in workers who are absent from work due to a musculoskeletal injury.
Methods
All workers with lost-time claims who were off work at baseline were selected from the Early Claimant Cohort (Canada) (n = 1,566). Follow-up data on RTW were available of 810 workers after 12 months. Predictors included demographic, health-related, and work-related factors. Differences between coefficients of the groups with and without comorbidity were tested.
Results
Low household income was a predictor for RTW in workers without comorbidity only. Better mental health was a predictor for RTW in workers with comorbidity only. Higher education, less pain intensity, better general health, less bodily pain, better physical health, and a positive supervisor response were predictors for RTW in the total group.
Conclusions
Injured workers with and without comorbidity should be considered as two distinct groups when focusing on mental health or household income.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders (MSDs) are the most prevalent of all chronic disorders in Canada, and musculoskeletal injuries account for the highest disability costs (Mirolla 2004). From all MSDs, low back pain has the highest prevalence, ranging from 58 to 80 % in Western industrialized countries (Koster et al. 2004; Walker 2000). Worldwide, 37 % of low back pain is estimated to be attributable to occupation (Punnett et al. 2005).
Musculoskeletal disorders have a large impact on the workplace and employers. Disability costs resulting from MSDs account for three-quarters of the total costs associated with MSDs, and in Canada, they account for 39 % of the estimated long-term disability costs (Health Canada 1998). Employees suffer from negative consequences due to MSDs, such as perceived limitation at work and sickness absence. In a previous study, we showed that perceived limitation at work enhanced the association between health on sick leave (Boot et al. 2011). Moreover, sickness absence has a further negative impact on psychological health (Kendall and Thompson 1998).
Comorbidity is becoming a problem in the general population, but also in the aging working population. Suffering from comorbidity may have specific implications for functioning at work, as well as the return to work (RTW) process (Buist-Bouwman et al. 2005; Lowe et al. 2004).
Previous research has shown that comorbidity was negatively associated with RTW outcomes within worker populations with musculoskeletal health problems (Lloyd et al. 2008; Nordin et al. 2002; Nyman et al. 2007). Nordin et al. 2002 showed that workers with comorbidity with an episode of low back pain were 1.3 times more likely not to RTW within 6 months compared to workers without comorbidity. Nyman and colleagues concluded that comorbidity of neck–shoulder disorders with low back disorders was associated with a 1.7 times increased risk of sick leave (Nyman et al. 2007). In a review by Lloyd et al. (2008), it was concluded that people of working age with MSDs and depression have worse RTW outcomes. In these studies, comorbidity was included as a predictor for work outcomes. However, it is arguable whether workers with and without comorbidity can be considered as one homogeneous group. Predictors and causal mechanisms might differ between workers with and without comorbidity. It is likely that investigating comorbidity as one predictor, relative to other predictors, or simply correcting for co-morbidity will not appropriately account for the complex process of RTW in workers with comorbidity.
The Canadian workers’ compensation system covers injuries and illnesses that are caused by work and typically only those of physical nature. It does not routinely cover mental health conditions. Because of this, musculoskeletal pain may be a primary driver for seeking care of filing a claim, and it is one of the many symptoms related to musculoskeletal injury. The group of workers with work-related injury therefore offers a great opportunity to study predictors of RTW.
Suffering from limitations from more than one health condition will increase the challenge for workers to overcome problems or RTW in case of injury. It can be hypothesized that comorbidity may lead to specific challenges to RTW in workers with musculoskeletal injury.
Since the prevalence of comorbidity is expected to increase in the future, interventions are needed to enhance RTW in this potentially vulnerable group. Insight into similarities and differences between predictors for RTW in groups of injured workers with and without comorbidity can be used as a starting point to develop interventions targeted to subgroups of workers at risk for not returning to work. To answer questions focused on the interaction of chronic conditions with work-related injuries requires detailed information early in the course of a work-related injury to better distinguish sub-groups before extensive interplay occurs between the chronic condition and the work-related injury in the RTW process. Sometimes, it takes some time for a claim to be accepted, say 2–3 months. The Canadian (Ontario-based) Early Claimant Cohort study employed a unique procedure by interviewing claimants shortly after the injury (maximum 21 days), allowing the exploration of the dynamic interplay between chronic conditions and work-related musculoskeletal injury.
This study aims to investigate differences and similarities between workers with and without comorbidity in 12-month predictors for RTW in workers who were absent from work due to a musculoskeletal injury.
Methods
Study design
The original study sample was a cohort of 1,825 injured workers having lost-time claims with the Ontario Workplace Safety and Insurance Board (WSIB) for soft tissue injuries of the upper limb, lower limb, or the back. The Board is the principal provider of workers compensation in Ontario and covers approximately 70 % of labor force participants (Workplace Safety and Insurance Board of Ontario 2002; Smith et al. 2004). Claimants were recruited shortly after they registered their claims.
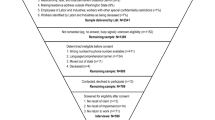
The cohort of 1,566 workers originates from the WSIB claims registration database, where 12,182 claimants were identified from May to November 1993. Of this group, 3,381 could not be contacted within the 21-day time frame from date of time off work, and another 5,866 were determined as ineligible at the screening interview (based on exclusion criteria outlined elsewhere (Hogg-Johnson and Cole 2003) or later because the WSIB claim was eventually denied). An additional 1,102 workers refused to participate at some point during the recruitment/screening interview. Their eligibility was unknown. Finally, eight cases had to be excluded because of damaged or miskeyed data. Information about eligible participants is described in more detail elsewhere (Sinclair et al. 1997). At baseline, 1,566 claimants were still off work, and this group was selected for the present analyses. After 12 months, data were available of 810 workers, which are used for the present analyses.
Measures
Comorbidity
The presence of serious co-existing conditions was measured on the baseline interview by a single question: ‘Do you have or are you currently being treated for any major illnesses or conditions such as bronchitis, arthritis, heart trouble, cancer, balance problems, vision or hearing loss, or any other serious health condition?’ with answering options ‘yes’ and ‘no.’ As the examples mentioned refer to somatic comorbidities, it is unlikely that participants with mental comorbidities have chosen ‘yes.’ Therefore, when we refer to comorbidity in this manuscript, this is likely to be mainly somatic comorbidity.
Pain intensity
Pain intensity was measured using an adaptation of a subscale of the Chronic Pain Grade (Von Korff et al. 1992), a component measure derived from self-reported information on three 0–10 numeric rating scales for the worst and average back pain since the beginning of current episode (at baseline), and back pain severity of this moment. The pain intensity scale was rescaled to range from 0 to 100, with 0 representing worst pain intensity and 100 representing lowest pain intensity (Hogg-Johnson and Cole 2003).
Functional status
Functional status was measured using two injury-specific or body-area-specific measures: the modified American Shoulder and Elbow Surgeons instrument (ASES) for upper extremity injuries (Richards et al. 1994) and the Roland instrument for back problems (Roland and Morris 1983). A more detailed description of these instruments and their properties has been given elsewhere (Sinclair et al. 1997). The body-region-specific functional status measures were all rescaled to range from 0 to 100, with 0 representing poorest functional status and 100 representing best functional status (Hogg-Johnson and Cole 2003). The measures ASES and Roland were used only in the appropriate subgroup, with upper extremity injuries and back injuries, respectively.
For the present study, functional status for lower extremity injuries could not be taken into account as a predictor because the group with comorbidity and a lower extremity injury consisted of 13 participants only who all had returned to work after 12 months.
Health status
All but one dimensions of the SF-36 (Ware et al. 1993), a generic, health-related quality-of-life measure, were used in this study: General health (GH), physical functioning (PF), mental health (MH), bodily pain (BP), role emotional (RE), social functioning (SF), and vitality (V). All SF-36 scores, except for GH, were rescaled to range from 0 to 100, with 0 representing worst health and 100 representing best health. GH was dichotomized into very good or excellent health and good, fair, or poor health. In addition, component scores were calculated for MH (MCS) and physical health (PCS). To calculate the PCS and MCS, test items are scored and transformed in an algorithm to norm-based scores with a mean of 50 and a standard deviation of 10 following Ware and colleagues (Ware et al. 1993). Role Physical could not be taken into analyses, because the majority of respondents (>93 %) had the lowest score (0).
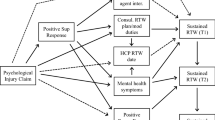
Outcome: RTW
Return to work was measured at the 52-week interview by the question ‘Are you working now?’ with possible responses ‘yes’ or ‘no.’ As our main focus was RTW in general, we included any RTW, including RTW in the same/different job, RTW in modified work, and changes in working hours.
Socio-demographic measures and work-related variables
Participants provided information on age, gender, level of education, household income, and occupational level at the baseline interview. To prevent empty cells, level of education was dichotomised into having an advanced degree yes/no; household income was dichotomised into lower or higher than CAN $40,000, which is little lower than the average household income in Canada in 1993, which was around CAN $45,000 (Hatfield 1996).
Job satisfaction was measured with one single item ‘In general—would you say you were very satisfied, satisfied, dissatisfied or very dissatisfied with your job taking everything into consideration?’ Due to power constraints, this measure was dichotomized into very satisfied and less than very satisfied.
Supervisor response to the disabling injury was examined using the question ‘Please tell me whether any of the following list of reactions that your supervisor may have had to your accident/injury apply to your case: (1) Blames you for the problem; (2) is supportive and helpful; (3) is angry that you are off work; (4) does not believe that anything is wrong with you; (5) is eager for you to RTW; (6) did not want you to file a claim; (7) wanted you to file a claim; (8) has had no reaction; or (9) he/she reacted in another way.’ This question was based on the literature and qualitative studies of injured workers Tarasuk and Eakin 1994, 1995).
The respondents were asked to agree or disagree with each supervisor reaction. Based on this work, the responses were aggregated into a single indicator with values ‘positive,’ ‘mixed,’ or ‘negative.’ To avoid empty cells, we dichotomized this indicator into positive or mixed/negative.
Answers were categorized into the variable ‘positive supervisor response’ if the answers to 2, 5, and 7 were chosen and the answers to items 1, 3, 4, 6, and 8 were not chosen, and otherwise categorized as ‘not positive supervisor response’.
Perceived re-injury risk at work was examined using the question ‘When you return to your usual job, do you think it will put you at no risk, some risk or high risk for an injury again?’ The variable was dichotomized into no perceived risk versus perceived risk.
Analyses
Descriptive analyses were performed to compare baseline characteristics between the groups with and without comorbidity. Because the group with comorbidity without RTW after 12 months was small (n = 17), we carefully checked all categorical variables and dichotomized these when necessary to prevent empty cells.
To assess the homogeneity/non-homogeneity of all predictors over the groups with and without comorbidity, the Dyer approach was followed (Dyer 1986; Noale et al. 2005; Boot et al. 2013):
-
(a)
For each potential predictor, a logistic regression model was fitted with RTW at 12-month follow-up as outcome.
-
(b)
A pooled estimate was constructed by weighting each coefficient with the inverse of its variance, and then summing over the two weighted coefficients, divided by the sum of the weights.
-
(c)
The pooled estimate was used in a chi-square test to test the null hypothesis that both coefficients were equal (i.e., whether the predictor was homogeneously distributed across the groups with and without comorbidity).
-
(d)
If the null hypothesis of homogeneity was not rejected, the pooled estimate from (b) was considered and its significant association with the outcome was tested with a T test (26).
-
(e)
If the null hypothesis of homogeneity was rejected, the coefficients of each group-stratum were examined and compared considering a T test for estimated coefficients (Menotti et al. 1996).
Since in the present study there were only two groups, this last step was not necessary. Logistic regression analyses were performed using SPSS for Windows (version 15.0). All T tests and chi-square tests for coefficients were performed in Microsoft Office Excel 2003 for Windows.
Results
Selection and attrition bias of the cohort
Of the 1,566 baseline cohort members, one had missing data on comorbidity. For 810 participants, information about self-reported RTW after 12 months was available (response 52 %). The group lost to follow-up was more often male (53.0 vs. 48.6 %), more often had a lower level of education (39.5 vs. 35.7 %). Furthermore, they had more often reported lower income (58.5 vs. 41.5 %), lower GH (73.9 vs. 76.9), lower MH (59.6 vs. 62.7), and more pain (lower scores) at baseline (25.2 vs. 28.1) compared to the group with RTW data after 12 months.
Description of the study population
In Table 1, the characteristics of the study population are presented. Comorbidity was reported by 11.7 % of all workers. Equal numbers of males and females participated, which was a direct result of purposeful sampling within the ECC. The average age was 38.9 years. The group with comorbidity was on average 5 years older compared to the group without comorbidity and reported a higher household income. The group without comorbidity reported a better GH status and a more positive physical component scale compared to those with comorbidity (Table 2). At follow-up, 17.8 % of those without comorbidity and 18.5 % of those with comorbidity had not returned to work.
Homogeneous predictors for RTW
All but two predictors tested as homogeneous following the homogeneity analyses. If the chi-square in Table 3 was smaller than 3.84, the homogeneity hypothesis was not rejected, and the predictor was considered homogeneous. This implies that participants with and without comorbidity can be considered as one group and that the pooled estimate should be used for calculation of the odds ratio (OR). Significant predictors of RTW at follow-up were higher education, lower pain intensity, better GH, less BP, better physical health, and a positive supervisor response.
Heterogeneous predictors of RTW
Two predictors were found to be heterogeneous: household income and MH component score (Table 4). Household income of more than CAD $40,000 was a strong predictor for RTW in the group without comorbidity, whereas it was not a significant predictor in the group with comorbidity. In the group without comorbidity, the OR was even lower than 1 (OR 0.43), but not significant. Better MH status was a strong predictor for RTW in the group with comorbidity, but not in the group without comorbidity (OR 1.00).
Discussion
This exploratory study found that most 12-month predictor for RTW in workers with musculoskeletal injuries were similar for groups with and without comorbidity, but two were found to differ. Mental health (MCS) was found to be a predictor for RTW in the group with comorbidity only, suggesting that MH requires special attention in future research. Household income was a predictor for RTW in the group without comorbidity only. As the aim of this study was exploratory, future research is needed to confirm these findings.
Comorbidity and RTW
For most potential predictors of RTW following musculoskeletal injuries investigated here, considering workers with and without comorbidity as distinct groups was not necessary. There were, however, two predictors where workers with and without comorbidity should be considered as distinct groups: MH and household income. Better MH was more important as a RTW predictor to work in the group with comorbidity, but not in the group without comorbidity. Previous research has shown that depression scores were prevalent in workers who had not yet returned to work after 6 months (Franche et al. 2009). In this study, however, the MH dimension of the SF36, a measure for positive affect or depression, was not a predictor for RTW. So this finding shows that even though the prevalence of depression was high in the group without RTW, depression was not a predictor for no RTW. The mental component score is constructed from different scales of the SF36 and represents the broader concept of MH-related quality of life. Since the MH dimension (indicating depression) was not predictive for RTW and only the mental component score (indicating health-related quality of life) was a predictor for RTW in the group with comorbidity, we conclude that MH-related quality of life, rather than depression, caused the differences between the groups.
This implies that impaired MH requires attention in further research, since different mechanisms regarding the RTW process may be present for injured workers with comorbidity.
The importance of MH for the RTW process has been stressed previously. Estimates of depressive symptom prevalence injured worker populations have been between 31 and 55 % (Franche et al. 2009; Dersh et al. 2002; Lerner et al. 2004). The co-occurrence of physical and mental conditions is associated with more work disability than either alone (Dewa and Lin 2000). This is in line with our finding that poor MH predicted RTW, although as our comorbidity measure likely measures mainly somatic comorbidity, it does not explain why MH was a predictor of RTW in the group with comorbidity only. Unfortunately, information about the comorbidity type was not available. The only available information was whether workers experienced other serious health conditions in addition to their musculoskeletal injury.
Another explanation may be that the combination of an injury, comorbidity, and impaired MH was too much to cope with. A recent qualitative study on failed RTW processes of injured workers showed that a ‘toxic dose’ was observed in injured workers who were facing different problems in their RTW process (MacEachen et al. 2010). If the number of problems passes a threshold, having suffered from an injury, having comorbidity, dysfunctions in organizational dynamics across RTW systems, including the workplace, healthcare, vocational rehabilitation, and workers’ compensation, and having poor MH might just have been too much (Baanders et al. 2002). This may interfere with the likelihood of RTW.
A third explanation could be that MH is important for both groups, but that the presence of this factor is phase-specific. It can be hypothesized that MH problems may be an important contributing factor at baseline for those with other important health problems, whereas for those without comorbidity, MH problems may develop later and play a role also for this group before the 12-month follow-up. However, more research is needed to confirm this hypothesis.
Household income was a predictor for RTW in the group without comorbidity only. An explanation for this may be that when individuals suffer from serious health conditions, this may change their drivers to RTW. Examples of such drivers are motivation to RTW, or the meaning of work and involvement in work. The group with comorbidity probably has bigger problems than their low household income, such as their health problems. This may explain why household income was not related to RTW. Interestingly, household income was a little higher in the group with comorbidity. This contrasts with previous studies where reduced income was associated with serious health conditions (Hogg-Johnson et al. 2010). Age might have played a role in this. Being older might imply that workers are having more years of work experience, and thus a higher salary. The higher salary in the group with comorbidity may thus be a consequence of the higher age rather than the presence of comorbidity. However, it should be noted that the relevance of this finding may be limited as the percentage of explained variance of the predictor household income was only 4 %, much lower than the explained variance by the MH component score (10 %).
Methodological considerations
The loss to follow-up after 12 months was 48 %. Although no major differences were observed at baseline between the groups with and without comorbidity, attrition bias may have occurred. The study aim was to gain insight into similarities and differences between predictors of RTW in injured workers with and without comorbidity rather than to generalize about the prevalence of RTW in the population. Our sample included a distribution of cases with and without comorbidity, with and without RTW, and a range of values across the predictors of interest. Although it is reasonable to believe that the RTW rates will differ between the respondents and those lost to follow-up, we do not have any indications to expect differences in the associations between predictors for RTW between the respondents and non-respondents.
The definition of comorbidity was based on self-reported information about other serious health conditions at baseline. No information was available about the specific diagnosis or severity of the health conditions, or the duration of the health problems. However, the study aim was to look into conditions that were present before the injury.
To reject the hypothesis of homogeneity, a statistically significant difference between the coefficients and the pooled estimate needed to be found. If the power is (too) low, the conclusion of homogeneity might be drawn incorrectly. For the present analyses, power was maximized by dichotomizing categorical variables. Our significant findings in the smallest group (comorbidity and no RTW) support our conclusion that the statistical power was sufficient.
The data used for the present analyses were collected in 1993 (Sinclair et al. 1997). This has implications for interpretation. In 1998, there were changes enacted in the workers’ compensation system in Ontario. Ongoing research has shown that the largest differences in outcomes were observed in individuals who had not returned to work 12 months following injury (Hogg-Johnson et al. 2010). Because of this, it is expected that the present findings still apply to the present situation.
It is likely that the prevalence of comorbidity within this population is an underestimation. In the present study, the prevalence of comorbidity was rather low, 11.7 %. Underreport may partially explain the low prevalence of comorbidity in this study, compared to other studies where a higher prevalence of comorbidity was reported in populations with workers with chronic musculoskeletal pain (Dersh et al. 2002).
The study outcome RTW after 12 months was based on self-reported data, obtained from the follow-up interview. This information was used rather than information on benefits received for two reasons: (1) having or not having returned to work at the time of the interview was considered a question that can clearly and easily be answered and (2) receiving full time benefits is considered a proxy for not being at work. In theory, however, there are situations where a person has returned to work, but is still receiving benefits and situations where a person may not have returned to work, but is no longer receiving benefits. In addition, it is unclear whether injured workers who are on part-time benefits are working or not. Because of these biases in the use of administrative data, we decided to rely on self-reported data only.
A final remark concerns study generalizability. All injured workers who had returned to work at the time of recruitment were excluded. This implies the study predictors cannot be generalized to workers who RTW within the first 21 days after injury. Since the RTW process becomes increasingly complex the more days that have passed following injury, the cohort is considered to be comprised of the most important target population to investigate predictors for RTW.
Implications for research and practice
Due to expectations that as the population ages, the prevalence of comorbidity among workers is likely to increase in the future. Because of this, we have formulated implications for RTW research, as well as for RTW practice. For research, the study findings imply that, when analyzing predictors for RTW in injured workers, attention should be paid to comorbidity with regard to MH-related quality of life. However, in general, predictors for RTW in injured workers with and without comorbidity appear to be similar. Future research should focus on further exploring the role of comorbidity and how this interferes with RTW, in particular the role of MH. Interventions focusing on improving MH-related quality of life may have different effect in injured workers with and without comorbidity. For practice, the study findings are an indication that in general, workers with comorbidity can be considered as one group when it involves RTW, although differences are present between workers with and without comorbidity. The main implication for practice is that predictors can be used to identify subgroups at risk for not returning to work. Following musculoskeletal injury, workers with comorbidity and poor MH need special attention. Health professionals and rehabilitation specialists are in the best position to monitor both comorbid conditions and MH. In the RTW process, this vulnerable group with both comorbidity and poor MH deserves special attention. Moreover, insight into predictors for RTW in vulnerable subgroups also has implications for how the RTW process is managed. The results show that there is a need for more communication between different provider groups and an expanded role of the case manager. This could be accomplished by sharing electronic medical records. This has large privacy issues, but it would allow the primary provider to see the range of chronic conditions being managed. Alternatively, the process of RTW could be improved by initiating a more collaborative consultation process.
Another implication of this study for occupational rehabilitation professionals and researchers is that the predictors may be the basis to develop interventions for RTW targeted to these subgroups at risk. This will enable employers to give additional support to employee subgroups with a higher risk of not returning to work, and not to give additional support to workers who will RTW without additional support as well.
This may have implications for policy makers and decision makers regarding disability benefits since existing criteria may not be applicable to injured workers with comorbidity in all cases.
Conclusion
The study conclusion is that few indications were found of differences in RTW predictors following musculoskeletal injury in workers with and without comorbidity. However, when investigating MH and household income as RTW predictors, workers with and without comorbidity should be considered as distinct groups.
References
Baanders AN, Rijken PM, Peters L (2002) Labour participation of the chronically ill: a profile sketch. Eur J Public Health 12:124–130
Boot CR, Koppes LL, van den Bossche SN, Anema JR, van der Beek AJ (2011) Relation between perceived health and sick leave in employees with a chronic illness. J Occup Rehabil 21:211–219
Boot CR, Deeg DJ, Abma TA, Rijs KJ, Van der Pas S, Van Tilburg TG, Van der Beek AJ (2013) Predictors of having paid work in older workers with and without chronic disease: a 3-year prospective cohort study. J Occup Rehabil. doi:10.1007/s10926-013-9489-y
Buist-Bouwman MA, De Graaf R, Vollebergh WA, Ormel J (2005) Comorbidity of physical and mental disorders and the effect on work-loss days. Acta Psychiatr Scand 111:436–443
Dersh J, Gatchel RJ, Polatin P, Mayer T (2002) Prevalence of psychiatric disorders in patients with chronic work-related musculoskeletal pain disability. J Occup Environ Med 44:459–468
Dewa CS, Lin E (2000) Chronic physical illness, psychiatric disorder and disability in the workplace. Soc Sci Med 51:41–50
Dyer AR (1986) A method for combining results from several prospective epidemiologic studies. Stat Med 5:303–317
Franche RL, Carnide N, Hogg-Johnson S et al (2009) Course, diagnosis, and treatment of depressive symptomatology in workers following a workplace injury: a prospective cohort study. Can J Psychiatry 54:534–546
Hatfield M (1996) Family incomes in Canada: 1984–1993. The role of markets, governments and demographics. Report No.: W-96-E. Applied Research Branch Strategic Policy Human Resources Development Canada, Quebec, Canada
Health Canada (1998) Economic burden of illness in Canada. Health Canada, Ottawa
Hogg-Johnson S, Cole DC (2003) Early prognostic factors for duration on temporary total benefits in the first year among workers with compensated occupational soft tissue injuries. Occup Environ Med 60:244–253
Hogg-Johnson S, Tompa E, Amick BA, Tolusso D, Chen C, Davilmar A (2010) The problem of long duration claims: examining markers of claim management and course. Workers’ Compensation Research Group, Hopkinton, MA
Kendall NAS, Thompson BF (1998) A pilot program for dealing with the comorbidity of chronic pain and long-term unemployment. J Occup Rehabil 8:26
Koster A, Bosma H, Kempen GI, van Lenthe FJ, van Eijk JT, Mackenbach JP (2004) Socioeconomic inequalities in mobility decline in chronic disease groups (asthma/COPD, heart disease, diabetes mellitus, low back pain): only a minor role for disease severity and comorbidity. J Epidemiol Community Health 58:862–869
Lerner D, Adler DA, Chang H et al (2004) The clinical and occupational correlates of work productivity loss among employed patients with depression. J Occup Environ Med 46:S46–S55
Lloyd C, Waghorn G, McHugh C (2008) Musculoskeletal disorders and comorbid depression: implications for practice. Aust Occup Ther J 55:23–29
Lowe B, Willand L, Eich W et al (2004) Psychiatric comorbidity and work disability in patients with inflammatory rheumatic diseases. Psychosom Med 66:395–402
MacEachen E, Kosny A, Ferrier S, Chambers L (2010) The, “toxic dose” of system problems: why some injured workers don’t return to work as expected. J Occup Rehabil 20:349–366
Menotti A, Keys A, Blackburn H et al (1996) Comparison of multivariate predictive power of major risk factors for coronary heart diseases in different countries: results from eight nations of the Seven Countries Study, 25-year follow-up. J Cardiovasc Risk 3:69–75
Mirolla M (2004) The cost of chronic disease in Canada. The Chronic Disease Prevention Alliance of Canada, Ottawa
Noale M, Minicuci N, Bardage C et al (2005) Predictors of mortality: an international comparison of socio-demographic and health characteristics from six longitudinal studies on aging: the CLESA project. Exp Gerontol 40:89–99
Nordin M, Hiebert R, Pietrek M, Alexander M, Crane M, Lewis S (2002) Association of comorbidity and outcome in episodes of nonspecific low back pain in occupational populations. J Occup Environ Med 44:677–684
Nyman T, Grooten WJ, Wiktorin C, Liwing J, Norrman L (2007) Sickness absence and concurrent low back and neck-shoulder pain: results from the MUSIC-Norrtalje study. Eur Spine J 16:631–638
Punnett L, Pruss-Utun A, Nelson DI et al (2005) Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med 48:459–469
Richards RR, An KN, Bigliani LU, Friedman R, Gartsman JM, Gristina AG (1994) A standardized method for the assessment of shoulder function. J Shoulder Elb Surg 3:347–352
Roland M, Morris R (1983) A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 8:141–144
Sinclair SJ, Hogg-Johnson SH, Mondloch MV, Shields SA (1997) The effectiveness of an early active intervention program for workers with soft-tissue injuries: the Early Claimant Cohort Study. Spine 22:2919–2931
Smith PM, Mustard CA, Payne JL (2004) A methodology for estimating the labour force insured by the Ontario Workplace Safety and Insurance Board: 1990–2000. Chronic Dis Can 25(127):137
Tarasuk V, Eakin JM (1994) Back problems are for life: perceived vulnerability and its implications for chronic disability. J Occup Rehabil 4:55–64
Tarasuk V, Eakin JM (1995) The problem of legitimacy in the experience of work-related back injury. Qual Health Res 5:204–221
Von Korff M, Ormel J, Keefe FJ, Dworkin SF (1992) Grading the severity of chronic pain. Pain 50:133–149
Walker BF (2000) The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 13:205–217
Ware JE, Snow KK, Kosinski M, Gandek B (1993) SF-36 Health survey manual and interpretation guide. New England Medical Center, The Health Institute, Boston, MA
Workplace Safety and Insurance Board of Ontario (2002) Coverage under the Ontario workplace safety and insurance act: technical report. Workplace Safety and Insurance Board of Ontario, Toronto, Ontario
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boot, C.R.L., Hogg-Johnson, S., Bültmann, U. et al. Differences in predictors for return to work following musculoskeletal injury between workers with and without somatic comorbidities. Int Arch Occup Environ Health 87, 871–879 (2014). https://doi.org/10.1007/s00420-014-0928-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-014-0928-7