Abstract
Purpose
The aim of this work is to provide an evidence-based evaluation and overview of causative substances in order to improve disease management.
Methods
We conducted a database search with MEDLINE via PubMed, screened reference lists of relevant reviews and matched our findings with a list of agents denoted as “may cause sensitisation by inhalation” by the phrase H334 (till 2011 R42). After exclusion of inappropriate publications, quality of the selected studies was rated with the Scottish Intercollegiate Guideline Network (SIGN) grading system. The evidence level for each causative agent was graded using the modified Royal College of General Practitioners (RCGP) three-star system.
Results
A total of 865 relevant papers were identified, which covered 372 different causes of allergic work-related asthma. The highest level achieved using the SIGN grading system was 2++ indicating a high-quality study with a very low risk of confounding or bias and a high probability of a causal relationship. According to the modified RCGP three-star grading system, the strongest evidence of association with an individual agent, profession or worksite (“***”) was found to be the co-exposure to various laboratory animals. An association with moderate evidence level (“**”) was obtained for α-amylase from Aspergillus oryzae, various enzymes from Bacillus subtilis, papain, bakery (flour, amylase, storage mites), western red cedar, latex, psyllium, farming (animals, cereal, hay, straw and storage mites), storage mites, rat, carmine, egg proteins, atlantic salmon, fishmeal, norway lobster, prawn, snow crab, seafood, trout and turbot, reactive dyes, toluene diisocyanates and platinum salts.
Conclusion
This work comprises the largest list of occupational agents and worksites causing allergic asthma. For the first time, these agents are assessed in an evidence-based manner. The identified respiratory allergic agents or worksites with at least moderate evidence for causing work-related asthma may help primary care physicians and occupational physicians in diagnostics and management of cases suffering from work-related asthma. Furthermore, this work may possibly provide a major contribution to prevention and may also initiate more detailed investigations for broadening and updating these evidence-based evaluations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As shown in various studies, 9–25 % of adult asthma is due to occupational factors (Blanc and Toren 1999; Balmes et al. 2003; Mapp et al. 2005; Toren and Blanc 2009). This asthma group is also known as work-related asthma. It includes occupational asthma, that is, new onset of asthma due to agents in the workplace, and work-aggravated asthma, that is, worsening of pre-existing or concomitant non-occupational asthma by agents in the workplace.
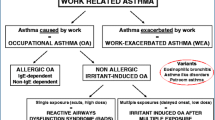
Work-related asthma comprises subtypes of occupational asthma as shown in Fig. 1.
IgE-mediated as well as irritant occupational asthma with not-so-sudden-onset, low-dose-irritant asthma and occupational asthma of unknown pathomechanism all typically showing a latency period from the beginning of causative exposure until appearance of symptoms (Baur et al. 2012b; Burge et al. 2012).
The great majority of occupational asthma cases are based on an IgE-mediated pathomechanism as is the case in adult allergic asthma unrelated to work.
In previous reviews and overviews, up to 300 agents have been reported as causes of occupational asthma (Tarlo and Malo 2009; Tarlo et al. 1998; van Kampen et al. 2000; Sastre et al. 2003; Quirce and Sastre 2011; Malo and Chan-Yeung 2007, 2009; Lombardo and Balmes 2000; Baur 2008; Bernstein et al. 2006).
These causative agents have been classified in two main groups according to their molecular weight: high molecular weight agents and low molecular weight agents. High molecular weight agents typically induce asthma through an IgE-mediated mechanism, while the pathomechanism of many low molecular weight agents is still unknown. Isocyanates and acid anhydrides are examples of the latter group demonstrating allergic as well as irritant effects (Mapp et al. 2005; Bernstein et al. 2006).
New agents are continually being reported as eliciting occupational asthma. Therefore, it is important to constantly keep these lists completed and up-to-date. Furthermore, an evidence-based evaluation of the literature, which does not exist currently, is of particular importance with regard to clinical case management and diagnostics in individual situations. As such, the major aim of this study is to provide an updated evidence-based overview of the present respiratory allergens causing work-related asthma. It should be helpful in clinical practice to identify causes of suspected occupational asthma in the workplace.
In this work, we focused on agents eliciting occupational asthma due to proven IgE-mediated sensitisation. We also included those agents with a likely IgE-mediated pathomechanism, such as platinum salts, that are associated with immediate skin prick test responses but negative results in measurements of specific IgE antibodies. With regard to irritant asthma, a recent publication summarises current knowledge (Baur et al. 2012a).
Methodology
For further methodological details of selection criteria, data extraction and synthesis, quality assessment of individual study and the overall list comprising results of each publication, see online resources.
We conducted a systematic literature search in MEDLINE/PubMed on occupational asthma and its causative agents. The search covered the period from MEDLINE/PubMed’s inception until August 2011 and was restricted to publications in English, German or French. The main keywords in the database search were “Bronchial Hyperreactivity”, “Airway Obstruction”, “Occupational Diseases” and “Occupational Exposure”. We also screened the reference lists of already published reviews including their references (van Kampen et al. 2000; Bernstein et al. 2006; Baur 2008; Malo and Chan-Yeung 2009; Tarlo and Malo 2009; Quirce and Sastre 2011). Furthermore, we compared the findings with a list of agents denoted as “may cause sensitisation by inhalation” by the phrase H334 (till 2011 R42) (Baur 2008; ACGIH®; Europäische Gemeinschaft 2001; European Parliament 2008).
Then, we combined results of both the database search and the reviews/summaries. The combination of medical subject headings (MeSH) finally used is the result of an optimised integration of the selection criteria and the comparison with studies found through occupational allergen lists:
(“1”[PDAT]: “2011/08/01”[PDAT]) AND (((((((((((“Signs and Symptoms, Respiratory”[Majr] OR “Occupational Diseases”[Majr]) OR “Allergy and Immunology”[Majr]) OR “Respiratory Function Tests”[Majr]) OR “Bronchial Hyperreactivity”[Majr]) OR “Airway Obstruction”[Majr]) OR “Respiratory Hypersensitivity”[Majr]) OR “Lung Diseases, Obstructive”[Majr]) OR “Asthma”[Majr]) OR “Asthma”[Mesh]) OR “Occupational Exposure”[Majr]) AND “ALLERGEN”[Mesh]) AND (“humans”[MeSH Terms] AND (English[lang] OR French[lang] OR German[lang]) AND “adult”[MeSH Terms]).
Studies with non-occupational asthma causes were excluded.
Publications about occupational agents which do not have an IgE-mediated effect on the respiratory tract or with unrelated issues were excluded. We searched for publications reporting studies performed exclusively with human who had been were occupationally exposed to causative agents (see online resources Table A).
The principal study characteristics and study results were systematically extracted using an extraction sheet (see online resources Table B).
We assessed study quality with the help of a check list (see online resources Table C).
After excluding of irrelevant publications (see Table A and Fig. 2), SIGN (Scottish Intercollegiate Guidelines Network) was used to rate the quality of each study (Harbour and Miller 2001). In order to achieve more differentiation among lower evidence grades, we modified the SIGN grading system and added an additional grade (3+; see Table 1). The modified RCGP (Royal College of General Practitioners) three-star system (Newman Taylor et al. 2005) was used to grade the evidence for each agent on basis of all available publications. The system considers quality and quantity of all studies as well as consistency of reported findings. Some modification was necessary for our study. We introduced additional up- and downgrading: [] indicated downgrading due to lower quality of clinical investigations, that is, due to missing objective parameters such as lung function data; further, (*) indicated upgrading from “−” due to at least five reported asthma cases without contradictory findings (see Table 2).
Results
Overview of reported causative allergenic agents
The database search resulted in 1,890 potentially relevant publications (see selection flow diagram, Fig. 2). An additional 475 potentially relevant publications were retrieved from the reference lists of the identified systematic reviews (van Kampen et al. 2000; Malo and Chan-Yeung 2009; Baur 2008; Bernstein et al. 2006; Quirce and Sastre 2011; Tarlo and Malo 2009).
After the exclusion of non-occupational cases, the different search approaches yield a total of 865 relevant studies. These 865 publications refer to 682 partially overlapping individual agents, to 121 “mixed” agents and to 62 worksites reported to cause allergic work-related/occupational asthma. In 41 cases, only the abstract could be read. They were also included and evaluated.
Table 3 presents an overview of the identified agents grouped according to their worksites and professions and their strength of evidence for causing occupational asthma.
Evidence levels in the retrieved literature
Two hundred and thirty-two of the total 865 publications were reviews of cross-sectional studies, case–control studies, cohort studies, longitudinal studies and clinical cross-sectional studies and were rated according to SIGN as 2++ (n = 2), 2+ (n = 18), 2− (n = 120) or 3+ (n = 92). The majority of publications represent questionnaire-based surveys, case series and case reports and were rated according to SIGN as 2− (n = 13), 3 (n = 144) or 3+ (n = 236). There was 1 review of cross-sectional studies, 5 case–control studies, 15 cohort studies, 2 longitudinal studies, 209 clinical cross-sectional studies, 54 questionnaire-based surveys, 115 case series and 467 case reports.
The highest level was 2++, indicating a high-quality analytical study (case–control or cohort studies) with a very low risk of confounding, bias or chance and a high probability that the relationship is causal (n = 2 studies). Eighteen studies were rated 2+ by SIGN grading of indicating well-conducted analytical studies (case–control or cohort studies) with a low risk of confounding, bias or chance and a moderate probability that the relationship is causal (n = 17 studies) and well-conducted systemic reviews of analytical cross-sectional studies (n = 1 review). Most of the other analytical studies were rated with a SIGN grade of 2− or 3+ because their design was limited (cross-sectional or longitudinal study) and/or they comprised a high risk of confounding, bias or chance (n = 212 studies). Some study designs were difficult to classify, notably surveys, which in many cases had very low analytical evidence, rated 3+ or 3 (n = 52 studies). Larger surveys with a lower risk of confounding or bias were graded with 2− (n = 12 studies). No study with a SIGN grade of 4 (expert opinion) was identified in this literature search.
Strength of evidence per agent or worksite
The modified RCGP three-star system enables the classification of strength of evidence for the causative role in allergic occupational asthma of each reviewed agent. The strongest evidence obtained was three stars “***” for one worksite, that is, exposure to various laboratory animals, indicating a strong strength of evidence provided by generally consistent findings in multiple, high-quality scientific studies. For 18 agents or worksites, strength of evidence corresponded to two stars “**” indicating moderate evidence (Table 2). For nine of them, this level was based on high-quality case–control or cohort studies (SIGN 2++) as well as well-conducted studies with a low risk of confounding or bias (SIGN 2+). For nine of these 18 agents, SIGN levels of individual studies were lower (SIGN 2−).
Moderate evidence, provided by generally consistent findings in fewer, smaller or lower quality scientific studies with clinical weakness (“*[*]”), was found for 17 agents.
Limited or contradictory evidence, provided by only one scientific study or inconsistent findings in multiple scientific studies (“*”), was identified for 18 agents. We downgraded (“[*]”) the evidence for 24 agents due to missing objective data.
The majority of agents were reported in non-analytical studies. Therefore, in the case of many agents, no scientific evidence could be obtained. An upgrading [“(*)”] could be realised if at least five cases were identified by case reports or case series proving allergic occupational asthma. Thus, the strength of evidence ranged from very limited or contradictory evidence [“(*)”] for 19 agents to no scientific evidence “−” for 275 agents, worksites or professions (Table 4).
Diagnostic aspects and allergic OA as outcome
In the retrieved publications, different procedures were used for the diagnosis of occupational asthma, with specific inhalation challenge (SIC) and serial lung function tests (sPFT) being considered the most reliable diagnostic tools (Leroyer et al. 1998; Ortega et al. 2002; Banks 2003; Tan and Spector 2003; Moscato et al. 1995).
SIC was used to confirm occupational asthma in 444 of 865 studies (51.3 %). SIC was only applied in non-analytical studies. sPFT were identified in 186 of included studies (21.5 %).
Lung function testing (LFT) was another frequent (n = 438; 50.6 %) diagnostic method for occupational asthma showing an obstructive ventilation pattern.
Exclusively, self-reported asthma symptoms or physician-reported asthma as documented in questionnaires as an alternative diagnostic approach for occupational asthma (Bernstein et al. 2006; Malo et al. 1991) was applied in 291 studies (33.6 %) [no LFT, non-specific bronchial hyperresponsiveness (NSBHR) or sPFT].
Another seven studies (0.8 %) did not have clear diagnosed occupational asthma but reported obstructive ventilation pattern in LFT.
In order to confirm allergic occupational asthma, it is necessary to document immediate-type sensitisation.
In several studies, this was accomplished solely with the skin prick test (SPT; n = 672; 77.7 %). In other studies, specific IgE tests were used in addition (spec. IgE, n = 518; 59.8 %).
Allergic occupational asthma could be diagnosed with these tools in many cases.
We identified 664 studies demonstrating immediate-type sensitisation to occupational agents by means of SPT and/or specific IgE tests. Considering our evaluation criteria, the most frequent occupational asthma causes were wood dust from western red cedar (448 cases), proteases and alcalases from Bacillus subtilis (279 cases), laboratory animals (229 cases), spider mites (174 cases), bakery (174 cases), latex (136 cases), various tea dusts (134 cases), storage mites (130 cases), papain (109 cases) and platinum salts (96 cases).
There were also several agents where these diagnostic methods were not applied or did not confirm the suspicion of allergic work-related asthma even if occupational asthma was highly probable.
Discussion
The aim of this study was to provide an evidence-based and practically relevant overview of the respiratory allergenic agents, worksites and professions causing occupational asthma. In addition to optimised diagnostic tools and adequate management strategies, prevention of occupational asthma is a great challenge for healthcare systems today. An all-embracing list of causative agents as aspired to in this work may be an essential part of respective management strategies. It could help in diagnostics, as well as in the control and reduction of exposures to harmful agents (Allmers et al. 2002; LaMontagne et al. 2006; Tarlo 2007; Quint et al. 2008; Baur et al. 2012b).
To our knowledge, this is the first evidence-based approach to connect occupational asthma with its causes.
The 865 publications retrieved from our Medline/PubMed and additional database search refer to 682 partially overlapping individual agents, 121 “mixed” agents and 62 worksites resulting in 372 different causes of allergic occupational asthma. Following our evaluation criteria, diagnoses of occupational allergic asthma could be confirmed in 664 studies.
Strength and limitations
We identified a large field of occupational agents causing allergic asthma and evaluated the strength of the body of evidence for each agent listed using the RCGP three-star system. This approach is the main strength of this work. Seeing that the concept of evidence-based medicine is omnipresent in contemporary clinical research and practice, we applied this evaluation for grading causes of occupational asthma. We only considered cases to be caused by the investigated agent if there was evidence for both asthma and sensitisation. There are some limitations to such an approach, in particular the underevaluation of certain types of medical reports and the generalisability of the results obtained in this manner. Furthermore, bias in the selection of information, publication content (e.g. exposure to multiple agents) and sample population (healthy hired and healthy worker effects) cannot be excluded. Since the quality and the content of considered studies vary widely, it can sometimes be difficult to combine them and generalise the results. Unfortunately, the source of the agent is not always clearly indicated in publications. In certain confinements (e.g. in swine confinement) or professions, causative agents are not always clear and may comprise different allergens as well as irritants. The same is true for exposure to mixtures of components as is the case in many workplaces (e.g. in the production of plastics or polyurethanes where there may be isocyanates, polyalcohols or solvents as well as irritative gases in the atmosphere).
The evidence levels for causing allergic occupational asthma of many of the listed agents or worksites are moderate to low. Approximately one quarter of the identified studies represent scientific studies. This is due to the fact that randomised controlled trials as claimed in scientific discussion (Tarlo et al. 2008) would have been unethical for studying exposure effects of harmful agents. Therefore, high-quality studies are missing and the available studies sometimes included only a few numbers of cases. The majority of them were surveys, case series or case reports with evidence level rated very low. The common diagnostic procedure for occupational asthma in clinical settings is a stepwise approach including questionnaires with asthma-specific symptoms as well as respiratory and allergological assessment. Objective diagnostic findings such as SPT, specific IgE, lung function parameters and SIC were not frequently applied resulting in limitations in classifying occupational asthma as being due to IgE-mediated sensitisation. Self-reported work-related symptoms are relatively sensitive for a diagnosis of occupational asthma; however, the specificity is low (Tarlo et al. 2008). In 291 of the 865 studies (33.6 %) included in this work, self-reported asthma symptoms or physician-reported asthma were used as a diagnostic approach. Serial spirometric or peak flow measurements (sPFT) which also comprise high sensitivity and specificity (Baur et al. 2012b; Burge et al. 2012) were identified in 186 studies. The SIC or sPFT gold standards were only applied in half of the studies. We included low SIGN grade studies (3/3+) if high level of evidence was missing because they may provide useful information for managing new cases of asthma.
The level of evidence for single agents depends on the number of publication included. Agents for which the research activity is higher obtain higher levels in our rating (Quint et al. 2008). An absence or a low evidence grade of an occupational agent (e.g. in studies without SIC or proven IgE-mediated sensitisation) does not necessarily exclude its potential for causing IgE-mediated asthma. This also comprises the need for modification of grading systems for evidence-based grading of the literature if high-level studies cannot be expected; a Delphi conference including experts world-wide could be an alternative approach.
Comparison with previous reviews and overviews of allergenic occupational asthma agents
A continuously updated classification of allergenic occupational asthma agents has been provided by the American Conference of Industrial Hygienists (ACGIH), the European Community and the Health and Safety Executive (ACGIH® http://www.acgih.org; Europäische Gemeinschaft 2001; Deutsche Forschungsgemeinschaft (DFG) 2011; Health and Safety Executive (HSE) 2001; Baur 2008). Allergenic agents are listed in three categories: substances which were considered to meet the EU criteria and labelled with H334 (till 2011 R42), substances which did not meet these criteria and those which were on account of concerns over respiratory sensitisation. Several groups have already published lists of airway sensitising agents (van Kampen et al. 2000; Tarlo and Malo 2009; Quirce and Sastre 2011; Baur 2008; Bernstein et al. 2006; Malo and Chan-Yeung 2009).
Quirce and Sastre recently summarised the new causative agents published between 2009 and 2011. These reviews all lacked an evidence-based evaluation of the clinical literature of identified agents. Therefore, even if the previous reviews already cover approximately 300 allergenic occupational asthma agents, the approach of the present work is more comprehensive, by listing 372 agents and with the advantage of grading each identified agent, worksite or profession in a well-defined evidence-based manner related to causation of occupational asthma.
Concluding remarks
Occupational asthma has a great impact on the socio-economic status of the workers concerned, the healthcare system and the society. In 2008, the costs in Germany for occupational disease “Obstructive respiratory tract diseases caused by allergenic substances”, listed as occupational disease no. 4301, were €52.1 million (Deutsche Gesetzliche Unfallversicherung (DGUV) 2009). This includes compensation for confirmed cases, costs of rehabilitation and preventive interventions. In 2003, Great Britain experienced a total of 631 new occupational asthma cases resulting in costs of about £3.4 to £4.8 million per year over the lifetime of the diseased patient (Boyd et al. 2006).
In 2010, 2,045 claims referring to the occupational disease no. 4301 were officially reported to German accident insurance institutions. Three hundred and twelve cases were acknowledged as new cases of the occupational disease no. 4301, representing only about 15 % of total cases. There were also 119 claims referring to occupational disease no. 1315 (isocyanate-induced diseases) with 30 acknowledged cases, representing about 25 % of total cases. It can be assumed that the official number of allergic occupational asthma cases is significantly higher since in routine diagnostics, objective tests are frequently not available and not applied or a referral to specialised diagnostic centres is not initiated. Primary care physicians are often unaware of the presence of causative agents in the workplace and do not frequently enquire into occupational history using valid questionnaires and a comprehensive diagnostic setup.
To facilitate the identification of occupational asthma agents and to improve preventive measures as well as management in affected cases, causative conditions must be easily available (Heederik et al. 2012). This study summarises the current levels of evidence for individual agents and worksites causing allergic occupational asthma. We found moderate to strong evidence for laboratory animals, several enzymes, isocyanates, farming and bakeries among others. It may help physicians in identifying a suspected allergenic agent as causative and may in such cases initiate a more detailed examination. It also demonstrates that more work is needed to fill in specific gaps, for example, in studying all potential asthma-inducing agents, and that objective diagnostic methods are available but need to be better integrated into clinical practice. Our comprehensive list could be the basis for surveillance programmes of exposed workers in order to identify those at higher risk of developing occupational asthma and to apply appropriate secondary preventive measures (Baur et al. 2012b).
It is hoped that this work provides a relevant contribution to prevention resulting in significant reduction or even elimination of occupational asthma development due to causative exposures, which is the most straightforward approach to reducing the burden of this disease.
Abbreviations
- OA:
-
Occupational asthma
- RADS:
-
Reactive airways dysfunction syndrome
- RCGP:
-
Royal College of General Practitioners
- SIGN:
-
Scottish Intercollegiate Guideline Network
- WRA:
-
Work-related asthma
- LFT:
-
Lung function tests
- sPFT:
-
Serial lung function tests
- SIC:
-
Specific inhalation challenge
- NSBHR:
-
Non-specific bronchial hyperresponsiveness
References
Allmers H, Schmengler J, Skudlik C (2002) Primary prevention of natural rubber latex allergy in the German health care system through education and intervention. J Allergy Clin Immunol 110(2):318–323
Balmes J, Becklake M, Blanc P, Henneberger P, Kreiss K, Mapp C, Milton D, Schwartz D, Toren K, Viegi G (2003) American Thoracic Society Statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med 167(5):787–797
Banks DE (2003) Use of the specific challenge in the diagnosis of occupational asthma: a ‘gold standard’ test or a test not used in current practice of occupational asthma? Curr Opin Allergy Clin Immunol 3(2):101–107. doi:10.1097/01.all.0000064773.57552.6e
Baur X (2008) Airborne allergens and irritants in the workplace. In: Kay AB, Kaplan AP, Bousquet J, Holt PG (eds) Allergy and allergic diseases. Blackwell Publishing, Oxford, pp 1017–1122
Baur X, Bakehe P, Vellguth H (2012a) Bronchial asthma and COPD due to irritants in the workplace—an evidence-based approach. JOMT 7(1):19. doi:10.1186/1745-6673-7-19
Baur X, Sigsgaard T, Aasen TB, Burge PS, Heederik D, Henneberger P, Maestrelli P, Rooyackers J, Schlunssen V, Vandenplas O, Wilken D (2012b) Guidelines for the management of work-related asthma. Eur Respir J 39(3):529–545
Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (2006) Asthma in the workplace and related conditions, vol 3, 3rd edn. Taylor & Francis, New York
Blanc PD, Toren K (1999) How much adult asthma can be attributed to occupational factors? Am J Med 107(6):580–587
Boyd R, Cowie H, Hurley F, Ayres J (2006) The true cost of occupational asthma in Great Britain. Health & Safety Executive (HSE), Suffolk
Burge PS, Moore VC, Robertson AS (2012) Sensitization and irritant-induced occupational asthma with latency are clinically indistinguishable. Occup Med (Lond) 62(2):129–133. doi:10.1093/occmed/kqr211
Deutsche Forschungsgemeinschaft (DFG) (ed) (2011) MAK- und BAT-Werte-Liste 2011: Maximale Arbeitsplatzkonzentrationen und Biologische Arbeitsstofftoleranzwerte, Mitteilung 47. Wiley-VCH, Weinheim
Deutsche Gesetzliche Unfallversicherung (DGUV) (2009) Dokumentation des Berufskrankheiten-Geschehens in Deutschland. BK-DOK 2008. http://www.dguv.de/inhalt/zahlen/documents/bk-dok-2008.pdf
Europäische Gemeinschaft (2001) Liste der gefährlichen Stoffe. Anhang 1 zu Richtline der Rates vom 27. Juni 1967 zur Angleichung der Rechts-und Verwaltungsvorschriften für die Einstufung, Verpackung und Kennzeichnung gefährlicher Stoffe (67/548/EWG). http://www.reach-clp-helpdesk.de/de/Downloads/CLP-Kompendium/RL_67_548_EWG_Anhang_I.pdf?__blob=publicationFile&v=2
European Parliament (2008) The Council of EU: Regulation (EC) No 1272/2008 of the European Parliament and on the Council of 16 December 2008 on classification, labelling and packing of substances and mixtures, amending and repealing Directives 67/548/EEC and 1999/45/EC, and amending Regulations (EC) No 1907/2006. Off J EU 1–1355. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2008:353:0001:0001:en:PDF
Harbour R, Miller J (2001) A new system for grading recommendations in evidence based guidelines. BMJ 323(7308):334–336
Health and Safety Executive (HSE) (2001) Asthmagen? Critical assessments of the evidence for agents implicated in occupational asthma. http://www.hse.gov.uk/asthma/asthmagen.pdf
Heederik D, Henneberger PK, Redlich CA, ERS task force on the management of work-related asthma (2012) Management of work-related asthma: primary prevention of occupational asthma: exposure reduction, skin exposure, and respiratory protection. Eur Respir Rev 21(124):112–124
LaMontagne AD, Radi S, Elder DS, Abramson MJ, Sim M (2006) Primary prevention of latex related sensitisation and occupational asthma: a systematic review. Occup Environ Med 63(5):359–364
Leroyer C, Perfetti L, Trudeau C, L’Archeveque J, Chan-Yeung M, Malo JL (1998) Comparison of serial monitoring of peak expiratory flow and FEV1 in the diagnosis of occupational asthma. Am J Respir Crit Care Med 158(3):827–832
Lombardo LJ, Balmes JR (2000) Occupational asthma: a review. Environ Health Perspect 108(Suppl 4):697–704
Malo JL, Chan-Yeung M (2007) Asthma in the workplace: a Canadian contribution and perspective. Can Respir J 14(7):407–413
Malo JL, Chan-Yeung M (2009) Agents causing occupational asthma. J Allergy Clin Immunol 123(3):545–550. doi:10.1016/j.jaci.2008.09.010
Malo JL, Ghezzo H, L’Archeveque J, Lagier F, Perrin B, Cartier A (1991) Is the clinical history a satisfactory means of diagnosing occupational asthma? Am Rev Respir Dis 143(3):528–532
Mapp CE, Boschetto P, Maestrelli P, Fabbri LM (2005) Occupational asthma. Am J Respir Crit Care Med 172(3):280–305
Moscato G, Godnic-Cvar J, Maestrelli P, Malo JL, Burge PS, Coifman R (1995) Statement on self-monitoring of peak expiratory flows in the investigation of occupational asthma. Subcommittee on Occupational Allergy of the European Academy of Allergology and Clinical Immunology. American Academy of Allergy and Clinical Immunology. European Respiratory Society. American College of Allergy, Asthma and Immunology. Eur Respir J 8(9):1605–1610
Newman Taylor AJ, Cullinan P, Burge PS, Nicholson P, Boyle C (2005) BOHRF guidelines for occupational asthma. Thorax 60(5):364–366
Nicholson PJ, Cullinan P, Burge PS, Boyle C (2010) Occupational asthma: prevention, identification & management: systematic review & recommendations. British Occupational Health Research Foundation, London. http://www.bohrf.org.uk/downloads/OccupationalAsthmaEvidenceReview-Mar2010.pdf
Ortega HG, Weissman DN, Carter DL, Banks D (2002) Use of specific inhalation challenge in the evaluation of workers at risk for occupational asthma: a survey of pulmonary, allergy, and occupational medicine residency training programs in the United States and Canada. Chest 121(4):1323–1328
Quint J, Beckett WS, Campleman SL, Sutton P, Prudhomme J, Flattery J, Harrison R, Cowan B, Kreutzer R (2008) Primary prevention of occupational asthma: identifying and controlling exposures to asthma-causing agents. Am J Ind Med 51(7):477–491. doi:10.1002/ajim.20583
Quirce S, Sastre J (2011) New causes of occupational asthma. Curr Opin Allergy Clin Immunol 11(2):80–85. doi:10.1097/ACI.0b013e328344586a
Sastre J, Vandenplas O, Park HS (2003) Pathogenesis of occupational asthma. Eur Respir J 22(2):364–373
Tan RA, Spector SL (2003) Provocation studies in the diagnosis of occupational asthma. Immunol Allergy Clin North Am 23(2):251–267
Tarlo SM (2007) Prevention of occupational asthma in Ontario. Can J Physiol Pharmacol 85(1):167–172
Tarlo SM, Malo JL (2009) An official ATS proceedings: asthma in the workplace: the Third Jack Pepys Workshop on Asthma in the Workplace: answered and unanswered questions. Proc Am Thorac Soc 6(4):339–349. doi:10.1513/pats.200810-119ST
Tarlo SM, Boulet LP, Cartier A, Cockcroft D, Cote J, Hargreave FE, Holness L, Liss G, Malo JL, Chan-Yeung M (1998) Canadian Thoracic Society guidelines for occupational asthma. Can Respir J 5(4):289–300
Tarlo SM, Balmes J, Balkissoon R, Beach J, Beckett W, Bernstein D (2008) Diagnosis and management of work-related asthma: American College of Chest Physicians Consensus Statement. Chest 134:1–41
Toren K, Blanc PD (2009) Asthma caused by occupational exposures is common—a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med 9:7
van Kampen V, Merget R, Baur X (2000) Occupational airway sensitizers: an overview on the respective literature. Am J Ind Med 38(2):164–218
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xaver Baur and Prudence Bakehe contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baur, X., Bakehe, P. Allergens causing occupational asthma: an evidence-based evaluation of the literature. Int Arch Occup Environ Health 87, 339–363 (2014). https://doi.org/10.1007/s00420-013-0866-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-013-0866-9