Abstract
Objectives
The aims of this study were to describe the use of occupational health services and other health care of Finnish employees and to examine associations between health problems and risks, and primary care visits to occupational health nurses and physicians and other health care.
Methods
A nationally representative sample of 3,126 employees aged 30–64 participated in the Health 2000 study, which consisted of a health interview, questionnaires, a clinical health examination, and the Composite International Diagnostic Interview. The use of health services was measured by self-reported visits.
Results
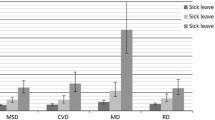
During the previous 12 months, 74 % of the employees visited occupational health services or municipal health centers, 52 % visited only occupational health services. From a third to a half of employees with lifestyle risks, depressive disorders or other health problems visited occupational health professionals. Obesity, burnout, insomnia, depressive mood, chronic impairing illnesses, and poor work ability were associated with visits to occupational health nurses. Among women, musculoskeletal diseases, chronic impairing illnesses, and poor work ability were associated with visits to occupational health physicians. Lower educational level, smoking, musculoskeletal diseases, chronic impairing illnesses, and poor work ability were associated with visits to health center physicians.
Conclusions
This study showed the importance of occupational health services in the primary health care of Finnish employees. However, a considerable proportion of employees with lifestyle risks, depressive mood, and other health problems did not use health services. Occupational health professionals are in an advantageous position to detect health risks in primary care visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal and depressive disorders and hazardous alcohol use are today’s major health problems causing disability. Earlier studies provide evidence that a considerable proportion of employees do not consult health services, despite their health problems (Bijl and Ravelli 2000; Honkonen et al. 2007; Hämäläinen et al. 2008; IJzelenberg and Burdorf 2004; Laukkala et al. 2001; Molano et al. 2001). Thus, it is a challenge to health services to contact employees with risks to work ability. Occupational health services (OHS) have a good opportunity to contact these persons.
In two Dutch studies, from one third to 44 % of the working population with low back pain sought care (Molano et al. 2001; IJzelenberg and Burdorf 2004). The study of scaffolders with low back pain showed that 20 % of them sought care from OH physicians (Molano et al. 2001). In Finnish studies, the proportion of subjects suffering from major depressive disorder (MDD) who used health services for mental problems varied from 28 to 36 % (Laukkala et al. 2001; Hämäläinen et al. 2008). In the Netherlands, of those who reported having psychiatric disorders, 33.9 % sought professional care (Bijl and Ravelli 2000). Such problems as burnout and insomnia have also been shown to predict permanent disability and increase the number of physician visits (Manocchia et al. 2001; Sivertsen et al. 2006; Ahola et al. 2007, 2009).
Seeking treatment for alcohol problems is not frequent. The proportion of those who contacted health care providers has varied from 12 to 17.5 % (Bijl and Ravelli 2000; Honkonen et al. 2007). Lifestyle risk factors such as smoking, obesity, and physical inactivity has been shown to be associated with higher use of health care services (Wetzler and Cruess 1985; Pronk et al. 1999; McDowell et al. 2006).
In Finland, employees can seek help for their health problems in municipal health centers (HC), in private clinics, or they can consult OHS, if their employers offer them primary care through OHS, which is voluntary in addition to mandatory OHS in which main tasks are workplace visits and health check-ups. Employers are partly reimbursed by the Social Insurance Institution for the costs of organizing OHS and primary care. By law, visits to OHS are free of charge to employees. Public health care collects moderate fees and private clinics have higher charges for treatment. Treatments by different health care providers are usually similar. The health problems treated in OHS are not circumscribed but work-related health problems are emphasized. Hospital outpatient clinics require a referral except in case of emergencies, and all primary health care providers have a right to refer their patients to hospital when needed. About half of the visits to private physicians are made to such specialist clinicians as ophthalmologists, gynecologists, and surgeons (Social Insurance Institution 2011).
In 2000, the proportion of employees who were also offered primary care through OHS was over 80 %; in 2009, it was over 90 % (Piirainen et al. 2000, Kauppinen et al. 2010). In 2003, 55 % of employed people had consulted OH physicians, and 45 % HC physicians during the previous year (Virtanen et al. 2006). In another study among employed people who had access to employer-arranged primary care, the proportion of all physician visits to OH physicians was 56 % among men and 45 % among women (Kimanen et al. 2010). Employees can also contact OH nurses or nurses in municipal health centers for primary care. OH nurses may either treat some health problems independently, or they can consult OH physicians. Among employees with access to employer-arranged primary care, the proportion of men who had visited OH nurses during the preceding 6 months was 44 % and of women 39 % (Kimanen et al. 2011).
More knowledge is needed regarding where employees with mental disorders, musculoskeletal diseases, and other chronic impairing illnesses or lifestyle risk factors threatening work ability seek primary care, as this would enable early interventions. The aims of this study were to describe the use of OHS and other health care services by working Finnish employees and to examine associations between health problems impairing work ability and health-related risk factors, and primary care visits to nurses and physicians focusing mainly on OH nurses and OH physicians.
Methods
Study design
This study is based on a Finnish multidisciplinary epidemiological study, the Health 2000 study, carried out in 2000–2001. The two-stage stratified cluster sample was representative of the Finnish population and comprised 8028 people aged 30 and over. Details and the methodology of the Health 2000 study are published elsewhere (Aromaa and Koskinen 2004; Heistaro 2008). Of the original sample, participation in some stage of data collection was 93 %, participation in the interview was 89 %, and in the health examination, 80 %. Of the total sample, 5,871 were of working age (30–64 years). Of this base population, 5,152 (88 %) people were interviewed, 4,911 (84 %) returned a questionnaire, and 4,886 (83 %) participated in a comprehensive health examination including a structured mental health interview, which was reliably performed on 4,706 subjects. This study focused on working employees aged 30–64 years. Of those, 3,126 were currently working part-time or full-time (during the last 12 months) and were included in this study.
Measures
Health care utilization was measured by numbers of self-reported visits, due to illnesses, to OH nurses, OH physicians, HC physicians, nurses in municipal health centers, private physicians, and physicians in hospital outpatient clinics during the past 12 months. The question in the interview regarding visits to physicians was: “How many times have you visited during the past 12 months for your illness (a) a health center physician, (b) hospital outpatient clinics, (c) an occupational health physician of your workplace, or (d) a private physician, (e) how many times has a doctor visited at home, (f) how many times have you visited a physician elsewhere?”. The question in the interview regarding visits to nurses was: “How many times have you visited during past 12 months for your illness (or maternity or delivery) (a) an occupational health nurse, (b) another nurse, or (c) how many times a nurse has visited you at home?”. The utilization was divided into two categories: yes/no. Health check-ups were excluded. The use of services specialized in mental health or alcohol problems was not studied. Participants were also asked which physician and nurse they primarily contacted when they needed medical help or advice in health-related matters.
Depressive and alcohol-use disorders were assessed by a Finnish translation of the German computerized version of the Composite International Diagnostic Interview (CIDI) (Wittchen et al. 1998; Heistaro 2008). Trained interviewers conducted interviews to determine 12-month prevalences of mental disorders according to DSM-IV criteria (American Psychiatric Association 1994). In this study, a depressive disorder means having a diagnosis for MDD or dysthymia within the preceding 12 months. Alcohol-use disorders included a 12-month prevalence of alcohol dependence and alcohol abuse.
Diagnoses of musculoskeletal diseases were based on the trained field physicians’ clinical examination, which was a standardized GP’s examination. The included diseases were arthritic conditions; chronic neck, low back, and shoulder syndromes; chronic diseases of upper extremities; and sequelae of injuries to the knee and ankle ligaments. The information on chronic impairing illnesses was based on replies to the interview question “Do you have a chronic or long-standing disability, disease, or injury which impairs your work ability or functional capacity?”. All diseases that participants reported as physician-diagnosed and lasting over 3 months were included.
Information on work ability was collected in the health interview and in questionnaires, including the items of the work ability index (WAI) developed at the Finnish Institute of Occupational Health (Tuomi et al. 1997, 1998). A score of 7–27 was classified as poor, 28–36 as moderate, 37–43 as good, and 44–49 as excellent work ability. We categorized the scores into two classes: poor and moderate as poor, and good and excellent as good work ability.
In the questionnaire, the original Beck Depression Inventory (BDI) consisting of 21 items was used to assess depressive symptoms (Beck et al. 1961, 1988). Their severity was assessed by the sum score so that scores 0–9 were considered to indicate no depression, 10–18 moderate depressive symptoms, and 19–63 severe depressive symptoms. Missing values (seven items at the most) were replaced by the mean of the existing values of the subject, and a sum score was calculated.
Burnout was measured using the Maslach Burnout Inventory—General Survey (MBI-GS) in the questionnaire (Maslach and Jackson 1981; Maslach et al. 1996). To assess the level of burnout, we used a weighted sum score of the three dimensions of burnout: exhaustion, cynicism, and lack of professional efficacy (Kalimo and Toppinen 1997; Kalimo et al. 2006). Burnout and the dimensional scores were categorized into two groups: no burnout (scores 0–1.49) and burnout (over 1.50). Burnout meant having monthly or more frequent symptoms.
Sleep problems were elicited by the question “Have you suffered from insomnia?” in the questionnaire; response options were yes or no.
The participants reported the weekly amount of alcohol consumed by frequency and amount of beer, wine, and spirits in the questionnaire. This information was transformed into grams of pure alcohol. In this study, the limit for hazardous drinking was 280 g of alcohol weekly for men and 140 g for women, which is based on the Finnish guideline in which the limits for health risks and recommendation to brief intervention are set to 40 g daily for men and 20 g for women (Salaspuro et al. 2005). We considered it hazardous health behavior for alcohol consumption, if the individual’s drinking habits exceeded the limits.
Other health behavior and risks were measured by regular smoking, body mass index (BMI, kg/m2), and reported physical activity. Smoking and physical activity were inquired in questionnaires, and BMI was based on measured weight and height in the clinical examination. Smoking was considered to be regular if the respondent reported smoking daily. Participants with a body mass index of 30 kg/m2 or over were classified as obese. Health-promoting physical activity was considered sufficient if the respondent reported exercising at least four times a week, for at least half an hour at a time.
Statistical analysis
Weighting adjustment and sampling parameters were used in all of the analyses to take into account the survey design complexities, including clustering in a stratified sample (Aromaa and Koskinen 2004; Heistaro 2008). We used procedures of SAS-callable SUDAAN software version 10.0 for the statistical analyses.
Associations of cross-tabulations were tested using a modified Chi-square. The relationship with visits to OH nurses, OH physicians, and HC physicians, nurses in municipal health centers, private physicians, and physicians in hospital outpatient clinics and explanatory variables were tested by logistic regression models adjusted for age. Calculations were made separately for women and men in order to identify possible differences.
Results
Table 1 shows the distribution of characteristics among the study population. Men had significantly more lifestyle health risks than women. Women reported chronic illnesses impairing work ability, depressive symptoms, and depressive disorders more often than men but men considered their work ability to be good more often than women.
The proportions of those who used health services were counted from the study population, which comprised also those whose information was missing. The number of those who used friend, relative, or other physicians was not studied. During the previous 12 months, 79 % (weighted %) of the study population had consulted a nurse or a physician in OHS, a nurse or a physician in municipal health centers, a private physician, or a physician in hospital outpatient clinics. Of the participants, 76 % had consulted OHS, health centers, or hospital outpatient clinics, 74 % had consulted OHS or municipal health centers, and 52 % had consulted only either OH nurses or OH physicians. The main contacts for primary care for employees were OH nurses, OH physicians, and HC physicians. An employee could have visited one or more of the health professionals. Men contacted only OH nurses as often as women, and women consulted other health care services more often. Over 40 % of the participants preferred to consult primarily OH professionals for their health problems. (Table 2).
Table 3 shows the proportion of male employees who visited nurses and physicians. Among men, those with a lower level of education and who were smokers visited HC physicians most often. Those who had been diagnosed with a depressive disorder contacted OH nurses the most. Among the men who had other risk factors or illnesses, consulting OH physicians was the most common. Among men, smokers consulted OH nurses and OH physicians less and HC physicians more than non-smokers. The proportion of those who had lifestyle risks did not visit more often private or hospital physicians than those without lifestyle risks. The proportion of those who visited nurses in municipal health centers was relatively low.
Among women (Table 4), the proportion of those who visited OH physicians was highest in relation to all other factors except for younger age, lower level of education, and physical inactivity, which related to the highest proportion of employees who consulted HC physicians.
About half of the women with hazardous alcohol consumption or alcohol-use disorders had visited OH physicians during the previous year.
Employees with insomnia or burnout consulted OH nurses, and such women consulted OH physicians significantly more often than those without these health problems. Depressive symptoms were related with a higher proportion of men (40 %) consulting OH nurses. Among women, those with depressive mood consulted OH nurses significantly more often (about 40 %) than those without (31–33 %). Almost half of the depressive women, and over 40 % of depressive men, had visited OH physicians.
Among both genders, employees with musculoskeletal and chronic illnesses impairing work ability visited OH nurses, private physicians, and hospital physicians more than those without these illnesses. Approximately half of the employees with these illnesses consulted OH physicians.
The proportion of employees with poor work ability who visited OH nurses, OH physicians, private physicians, and hospital physicians was significantly higher than that of those with good work ability. Among men, this proportion was also significant regarding visits to HC physicians. Over 50 % of those with poor work ability had visited OH physicians.
Table 5 shows associations between factors and visits to nurses and physicians in age-adjusted logistic regression analysis among men and Table 6 among women. A lower level of education was associated with HC physician consultations. Among men, smoking was associated positively with visits to HC physicians and inversely with visits to OH nurses and OH physicians. The associations remained after adjusting for education (data not shown). Among women, smoking and lower education were inversely associated with visits to private physicians.
Obesity and insomnia were associated with visits to OH nurses, among men also burnout, and among women depressive mood. Obesity and depressive symptoms were also associated with visits to other nurses. Among men, musculoskeletal diseases, chronic illnesses, and poor WAI were associated with visits to OH nurses and HC physicians. After adjusting for education (data not shown), associations with visits to HC physicians were not significant. Among women, musculoskeletal disorders were associated with visits to OH physicians. Chronic illnesses and poor WAI were associated with visits to both OH nurses and OH physicians. Those factors were also associated with other nurses and hospital physicians. Illness-related factors were associated with visits to private and hospital physicians, but lifestyle factors were not.
Discussion
In this study, we found that a half of the study population consulted only OHS for primary care of those health care providers inquired after. However, only one third to a half of the employees with studied health problems or health risks had used health care services during the previous 12 months. Associations of insomnia, burnout, depressive disorders, and chronic impairing illnesses with visits to OH nurses and OH physicians suggest that the holistic approach is important in detecting and screening health problems and risk factors in primary care consultations.
The finding that 52 % of employees had consulted only OHS for primary care during the previous 12 months is in accordance with earlier studies showing that approximately half of employed people visited OH physicians (Virtanen et al. 2006; Kimanen et al. 2010). The proportion of the employees who visited OH nurses was lower in our study than in the earlier study, which was limited to employees who had access to employer-arranged primary care (Kimanen et al. 2011). In the present study, OHS arrangements were not elicited. Furthermore, the age range was different, and the participation rate was higher, which may also explain differences to earlier studies. Important reasons for the high use of OHS in Finland are that employees have rated access and quality of OHS as good (Halonen et al. 2006). In addition, the use of OHS is free of charge for employees.
In this study, we did not ask about the reasons for visiting health services. Thus, the results indicate the opportunity to detect possible harmful lifestyle risk factors and illnesses impairing work ability that need health intervention.
Of the lifestyle health risks, obesity was associated with visits to OH nurses. Obesity has also earlier been shown to associate with more frequent health care consultations (McDowell et al. 2006). In this study, this was shown only in visits to OH nurses. Smoking was associated with visits to HC physicians among men but did not associate in other groups and lower education did not explain it. However, smoking has been found to be more frequent among men with lower vocational education. Those men work more often in such industries as construction and small enterprises, which has lower coverage in arranging OHS and primary care through OHS which may partly explain visiting HC physicians in municipal health centers (Piirainen et al. 2000).
Physical inactivity did not associate with visits in crude associations; on the contrary, the proportion of physically active employees who visited OHS was higher than those of physically inactive employees. This may reflect general activity in taking care of one’s health. In earlier studies, smoking and physical inactivity associated with more frequent doctor visits (Wetzler and Cruess 1985).
For alcohol problems, seeking treatment from primary care (including OHS) has been found to be low (Honkonen et al. 2007). In this study, half of the women with hazardous alcohol consumption or alcohol disorders had consulted OH physicians, whereas among men, the proportion was one third. Alcohol disorders and hazardous alcohol consumption did not seem to have an effect on the consultation of OH professionals compared with those who did not drink excessively. Thus, hazardous alcohol consumption could be detected in primary care visits to OHS for other reasons. In this study, the limits for hazardous drinking were lower than in earlier Finnish studies, and thus, the prevalence of hazardous drinking was higher (Halme et al. 2008). We used the limits of the national guidelines as limits for health risks and recommendations for brief intervention, which is also feasible in OHS.
Burnout and insomnia may relate to depressive disorders and disability (Ahola et al. 2005, 2009; Sivertsen et al. 2006). This study shows that employees suffering from burnout or insomnia visit OH professionals more frequently than those without which presents the opportunity for interventions. The prevalence of burnout among men was as high as among women, implying that screening it might reveal work-related mental ill-being also among men.
Several studies have found seeking treatment for depressive disorders to be insufficient (Bijl and Ravelli 2000; Laukkala et al. 2001; Honkonen et al. 2007, 2008). In this study, we found that over 40 % of employees with depressive symptoms or disorders visited OH professionals for some reason. This proportion is higher than that of people who seek treatment for their mental problems (Laukkala et al. 2001; Hämäläinen et al. 2008). In another Finnish study comprising individuals aged 15-75 years, about 65 % of those not using any health services for their major depressive episodes had contacted a doctor for some reason during the past 6 months (Hämäläinen et al. 2004). In a community survey in Canada, 21 % of subjects with a psychiatric diagnosis reported the use of mental health services, and 83 % of these same subjects used primary care physicians for general health problems (Parikh et al. 1997). In addition, we found that depressive employees visited OH nurses significantly more frequently than those with no depressive symptoms or disorders. Because disability and retirement due to depressive disorders in Finland is high, the coverage of health care contacts should be higher. However, employees with depressive symptoms do not necessarily feel the need for treatment, or it is possible that the threshold of help-seeking is still high. A health survey of a Finnish company revealed that during the six-month follow-up, 57 % of employees with depressive symptoms measured by the Depression Scale attended a consultation with an OH physician even after the invitation. Over 90 % of them had visited OHS for some reason (Taimela et al. 2007).
Of the men with physician-diagnosed musculoskeletal diseases, 46 % had visited OH physicians, and of women, 51 %. The lower numbers in seeking care from OH physicians in the Netherlands probably depends on the differences in health care systems (Molano et al. 2001). Chronic illnesses impairing work ability strongly were associated with visiting OH physicians, HC physicians, and private physicians in an earlier study, which only included employees who had access to OHS primary care (Kimanen et al. 2010). In the present study, all employees were included, and the association was found with visits to all other nurses and physicians except OH physicians among men, and OH nurses, nurses in health centers, OH physicians, and hospital physicians among women. Among men, none of the symptom, disorder, or disease factors associated with visiting OH physicians in crude associations. This may indicate that some other factors may play a more important role in contacting OH physicians. The employer’s requirement of a sickness certificate has been shown to be a significant factor (Kimanen et al. 2010).
Work ability measured by WAI was associated strongly with visits to OH professionals, nurses and physicians in health centers, and hospital physicians. In an earlier study, WAI predicted disability (Alavinia et al. 2009). Therefore, work ability should be considered in primary care visits.
In this study, we used data from the Finnish Health 2000 study, which has several strengths. It represents the entire Finnish 30- to 64-year-old population and the participation rate was high (80–88 %). Thus, the results can be generalized in these age groups. The questionnaires, the CIDI interviews, and the examination protocols were standardly applied, based on generally accepted recommendations and nationally established practices. The CIDI interview has been found to be a valid method in the assessment of mental disorders (Jordanova et al. 2004). Musculoskeletal diseases were assessed during the physicians’ clinical examinations. WAI has been used in several studies and has proved to be a valid measurement in predicting work disability (Ilmarinen et al. 1997).
The study did have some limitations, however. It was cross-sectional, thus causal relations cannot be assessed. We used self-reports of health care service use, which are vulnerable to recall bias, and may cause some under-reporting of visits (Siemiatycki 1979). In addition, all health care use was not analyzed as data of the visits to such physicians as friend, relative, or other physicians was not examined. The weakening effect on the results is likely to be insignificant as in earlier studies the number of these visits has been low (Piirainen et al. 2000; Kimanen et al. 2010). Several other factors were self-reported, causing possible inaccuracy. Chronic illnesses impairing work ability and insomnia were assessed by single questions. However, subjective conceptions in these conditions are often considerable. The results cannot be generalized to other countries as the health care systems are different. Although the study has been carried out in 2000–2001, the results can be considered still relevant as major changes in the Finnish health care system has not been occurred even though the role of OHS primary care has accentuated after 2001 (Kauppinen et al. 2010).
In conclusion, OHS is the only contact with health care services inquired in this study for half of the employees in Finland, emphasizing its role in health interventions for improving employees’ work ability. However, a considerable proportion of employees had not contacted health care services during the previous 12 months, although they had harmful lifestyle health risks, symptoms, disorders, or diseases. Thus, other measures such as health check-ups and surveys are needed in OHS to find these employees. This study also shows that OH nurses and OH physicians are in an advantageous position to detect mental problems and other chronic conditions of employees. They should proactively search for health risks during primary care visits, in order to improve employees’ work ability.
References
Ahola K, Honkonen T, Isometsä E et al (2005) The relationship between job-related burnout and depressive disorders—results from the Finnish health 2000 study. J Affect Disord 88(1):55–62
Ahola K, Honkonen T, Virtanen M et al (2007) Interventions in relation to occupational burnout: the population-based health 2000 study. J Occup Environ Med 49(9):943–952
Ahola K, Gould R, Virtanen M, Honkonen T, Aromaa A, Lönnqvist J (2009) Occupational burnout as a predictor of disability pension: a population-based cohort study. Occup Environ Med 66(5):284–290
Alavinia SM, de Boer AG, van Duivenbooden JC, Frings-Dresen MH, Burdorf A (2009) Determinants of work ability and its predictive value for disability. Occup Med (Lond) 59(1):32–37
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington (DC)
Aromaa A, Koskinen S (eds) (2004) Health and functional capacity in Finland. Baseline results of the health 2000 examination survey. National Public Health Institute, Helsinki
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Beck AT, Steer RA, Garbin M (1988) Psychometric properties of the Beck depression inventory: twenty years of evaluation. Clin Psychol Rev 8:77–100
Bijl RV, Ravelli A (2000) Psychiatric morbidity, service use, and need for care in the general population: results of The Netherlands mental health survey and incidence study. Am J Public Health 90(4):602–607
Halme JT, Seppä K, Alho H et al (2008) Hazardous drinking: prevalence and associations in the Finnish general population. Alcohol Clin Exp Res 32(9):1615–1622
Halonen P, Vehviläinen A, Mäntyselkä P et al. (2006) Lääkäripalvelujen laatu väestön arvioimana (Patient satisfaction with the quality of physician services) (abstract in English) Suom Lääkäril 61:1739–1744
Hämäläinen J, Isometsä E, Laukkala T et al (2004) Use of health services for major depressive episode in Finland. J Affect Disord 79(1–3):105–112
Hämäläinen J, Isometsä E, Sihvo S, Pirkola S, Kiviruusu O (2008) Use of health services for major depressive and anxiety disorders in Finland. Depress Anxiety 25(1):27–37
Heistaro S (ed) (2008) Methodology report, health 2000 survey. Publications of National Public Health Institute, Helsinki
Honkonen T, Virtanen M, Ahola K et al (2007) Employment status, mental disorders and service use in the working age population. Scand J Work Environ Health 33(1):29–36
IJzelenberg W, Burdorf A (2004) Patterns of care for low back pain in a working population. Spine 29(12):1362–1368
Ilmarinen J, Tuomi K, Klockars M (1997) Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health 23(Suppl 1):49–57
Jordanova V, Wickramesinghe C, Gerada C, Prince M (2004) Validation of two survey diagnostic interviews among primary care attendees: a comparison of CIS-R and CIDI with SCAN ICD-10 diagnostic categories. Psychol Med 34(6):1013–1024
Kalimo R, Toppinen S (1997) Työuupumus Suomen työikäisellä väestöllä (Burnout in the Finnish working population). Finnish Institute of Occupational Health, Helsinki
Kalimo R, Hakanen J, Toppinen-Tanner S (2006) Maslachin yleinen työuupumuksen arviointimenetelmä MBI-GS. Finnish Institute of Occupational Health, Helsinki
Kauppinen T, Hanhela R, Kandolin I et al (eds) (2010) Työ ja terveys Suomessa 2009 (Work and Health in Finland 2009) (in Finnish). Finnish Institute of Occupational Health, Helsinki
Kimanen A, Manninen P, Räsänen K, Rautio M, Husman P, Husman K (2010) Factors associated with visits to occupational health physicians in Finland. Occup Med (Lond) 60(1):29–35
Kimanen A, Rautio M, Manninen P, Räsänen K, Husman P, Husman K (2011) Primary care visits to occupational health physicians and nurses in Finland. Scand J Pub Health 39:525–532
Laukkala T, Isometsä E, Hämäläinen J, Heikkinen M, Lindeman S, Aro H (2001) Antidepressant treatment of depression in the Finnish general population. Am J Psychiatry 158(12):2077–2079
Manocchia M, Keller S, Ware JE (2001) Sleep problems, health-related quality of life, work functioning and health care utilization among the chronically ill. Qual Life Res 10(4):331–345
Maslach C, Jackson SE (1981) The measurement of experienced burn-out. J Occup Behav 2:99–113
Maslach C, Jackson SE, Leiter MP (1996) Maslach burnout inventory manual, 3rd edn. Consulting Psychologist Press, Palo Alto
McDowell MA, Hughes JP, Borrud LG (2006) Health characteristics of U.S. adults by body mass index category: results from NHANES 1999–2002. Public Health Rep 121(1):67–73
Molano SM, Burdorf A, Elders LA (2001) Factors associated with medical care-seeking due to low-back pain in scaffolders. Am J Ind Med 40(3):275–281
Parikh SV, Lin E, Lesage AD (1997) Mental health treatment in Ontario: selected comparisons between the primary care and specialty sectors. Can J Psychiatry 42(9):929–934
Piirainen H, Elo A, Hirvonen M et al (2000) Työ ja terveys-haastattelututkimus 2000, Taulukkoraportti (Work and Health Survey 2000) (in Finnish). Finnish Institute of Occupational Health, Helsinki
Pronk NP, Goodman MJ, O’Connor PJ, Martinson BC (1999) Relationship between modifiable health risks and short-term health care charges. JAMA 282(23):2235–2239
Salaspuro M, Alho H, Autti-Rämö I et al. (2005) Alkoholiongelmaisen hoito. Käypä hoito -suositus (Treatment of alcohol abuse. Current Care Guideline). Duodecim 121(7):788–803
Siemiatycki J (1979) A comparison of mail, telephone, and home interview strategies for household health surveys. Am J Public Health 69(3):238–245
Sivertsen B, Overland S, Neckelmann D et al (2006) The long-term effect of insomnia on work disability: the HUNT-2 historical cohort study. Am J Epidemiol 163(11):1018–1024
Statistical Yearbook of the Social Insurance Institution 2010 (2011) Official statistics of Finland. http://www.kela.fi/it/kelasto/kelasto.nsf/alias/Vk_10_pdf/$File/Vk_10.pdf?OpenElement. Accessed 08.03.2012
Taimela S, Mäkelä K, Justén S, Schugk J (2007) Masennusoireiden seulonta ja oireisten työntekijöiden hoitoonohjaus työterveyshuollossa (Screening for depressive symptoms in occupational health care and referral of symptomatic employees for treatment) (abstract in English). Suom Lääkäril 62:4203–4207
Tuomi K, Ilmarinen J, Seitsamo J et al (1997) Summary of the Finnish research project (1981–1992) to promote the health and work ability of aging workers. Scand J Work Environ Health 23(Suppl 1):66–71
Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A (1998) Work ability index, 2nd revised edition. Finnish Institute of Occupational Health, Helsinki
Virtanen P, Mattila K, Suominen S (2006) Väestövastuu ja työikäisten lääkärissäkäynnit eri kokoisissa kunnissa. (Visits to a physician by people of working age, according to whether or not they belong to the personal doctor system and the size of the municipality) (abstract in English). Suom Lääkäril 61:4485–4490
Wetzler HP, Cruess DF (1985) Self-reported physical health practices and health care utilization: findings from the national health interview survey. Am J Public Health 75(11):1329–1330
Wittchen HU, Lachner G, Wunderlich U, Pfister H (1998) Test-retest reliability of the computerized DSM-IV version of the Munich-composte international diagnostic interview (M-CIDI). Soc Psychiatry Psychiatr Epidemiol 33(11):568–578
Acknowledgments
We would like to thank the staff of the National Institute of Health and Welfare for data collection and processing.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ikonen, A., Räsänen, K., Manninen, P. et al. Use of health services by Finnish employees in regard to health-related factors: the population-based Health 2000 study. Int Arch Occup Environ Health 86, 451–462 (2013). https://doi.org/10.1007/s00420-012-0778-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-012-0778-0