Abstract
Purpose
Mental health problems are associated with sickness absence (SA). The present study aimed at establishing which symptoms—distress, depression, anxiety, or somatization—at which symptom levels were associated with SA frequency and duration. Moreover, a number of possible confounders or effect modifiers were taken into account.
Methods
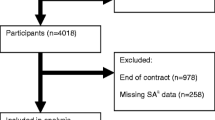
A survey was completed by 3,678 employees of a large Dutch telecom company. Symptoms were measured using the Four-Dimensional Symptom Questionnaire (4DSQ). SA data were registered by the company’s occupational health service during the 12 months’ period following the survey. Poisson regression was used to analyze the number of SA spells (SA frequency). Negative binomial regression was used to analyze the total number of SA days (SA duration).
Results
In the bivariate analyses distress, depression, anxiety, and somatization impacted on SA frequency and duration. In the multivariate analyses, anxiety and depression turned out not to be directly associated with SA, suggesting that the effect of anxiety and depression was due to the association between anxiety/depression and distress/somatization. Regarding the SA frequency, the rate ratio for ‘subclinical’ distress was 1.13 (95% CI 1.03–1.25), for ‘clinical’ distress 1.26 (1.08–1.47), for ‘subclinical’ somatization 1.34 (1.23–1.46), and for ‘clinical’ somatization 1.69 (1.46–1.95). Regarding the SA duration, the count ratio for ‘subclinical’ distress was 1.15 (95% CI 0.91–1.44), for ‘clinical’ distress 1.50 (1.04–2.16), for ‘subclinical’ somatization 1.34 (1.10–1.64), and for ‘clinical’ somatization 1.45 (1.04–2.03).
Conclusions
Somatization and distress are key to understand why depression and anxiety are related to SA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Previous studies have repeatedly substantiated the association between mental health problems and sickness absence (SA) (Hensing and Wahlström 2004; Duijts et al. 2007). These studies vary in a number of ways. The design of the studies was cross-sectional (Hilton et al. 2008; Kessler and Frank 1997; Dewa and Lin 2000; Kouzis and Eaton 1994; Suija et al. 2009; Kruijshaar et al. 2003) or longitudinal, using follow-up periods ranging from 3 months to 3 years (Broadhead et al. 1990; Jenkins 1985; Laitinen-Krispijn and Bijl 2000; Bültmann et al. 2005, 2006; Virtanen et al. 2007; Kivimäki et al. 2001, 2007; Bourbonnais and Mondor 2001; Andrea et al. 2003; Väänänen et al. 2003; Lexis et al. 2009; Duijts et al. 2006; Eriksen et al. 2003; Janssen et al. 2003; Ahola et al. 2008; Borritz et al. 2006; Krantz and Ostergren 2002). Some studies looked at interview-based psychiatric disorders (Kessler and Frank 1997; Dewa and Lin 2000; Kouzis and Eaton 1994; Suija et al. 2009; Kruijshaar et al. 2003; Broadhead et al. 1990; Jenkins 1985; Laitinen-Krispijn and Bijl 2000), others at questionnaire-based psychological symptoms (Hilton et al. 2008; Bültmann et al. 2005, 2006; Virtanen et al. 2007; Kivimäki et al. 2001; Bourbonnais and Mondor 2001; Andrea et al. 2003; Väänänen et al. 2003; Lexis et al. 2009; Duijts et al. 2006; Eriksen et al. 2003; Janssen et al. 2003; Ahola et al. 2008; Borritz et al. 2006; Kivimäki et al. 2007; Krantz and Ostergren 2002). The symptom predictors studied were distress (Hilton et al. 2008; Bültmann et al. 2005; Virtanen et al. 2007; Kivimäki et al. 2001; Bourbonnais and Mondor 2001; Andrea et al. 2003; Väänänen et al. 2003), depression (Bültmann et al. 2006; Lexis et al. 2009; Duijts et al. 2006; Eriksen et al. 2003), fatigue (Bültmann et al. 2005; Andrea et al. 2003; Duijts et al. 2006; Eriksen et al. 2003; Janssen et al. 2003), burnout (Bourbonnais and Mondor 2001; Duijts et al. 2006; Ahola et al. 2008; Borritz et al. 2006) and psychosomatic symptoms (Väänänen et al. 2003; Eriksen et al. 2003; Kivimäki et al. 2007; Krantz and Ostergren 2002). Some studies reported on SA as a dichotomous (yes/no) outcome (Kouzis and Eaton 1994; Laitinen-Krispijn and Bijl 2000; Bültmann et al. 2005; Eriksen et al. 2003; Ahola et al. 2008; Krantz and Ostergren 2002), others reported on the frequency of SA spells (Kivimäki et al. 2001, 2007; Väänänen et al. 2003; Duijts et al. 2006) or the total number of SA days (Kessler and Frank 1997; Dewa and Lin 2000; Suija et al. 2009; Kruijshaar et al. 2003; Broadhead et al. 1990; Andrea et al. 2003; Ahola et al. 2008). Few studies analyzed SA both in terms of frequency and duration as recommended by Hensing et al. (1998). SA was either established by self-report (Hilton et al. 2008; Kessler and Frank 1997; Dewa and Lin 2000; Kouzis and Eaton 1994; Suija et al. 2009; Kruijshaar et al. 2003; Broadhead et al. 1990; Jenkins 1985; Laitinen-Krispijn and Bijl 2000; Eriksen et al. 2003; Borritz et al. 2006) or by organizational absence records (Bültmann et al. 2005, 2006; Virtanen et al. 2007; Kivimäki et al. 2001, 2007; Bourbonnais and Mondor 2001; Andrea et al. 2003; Väänänen et al. 2003; Lexis et al. 2009; Duijts et al. 2006; Janssen et al. 2003; Ahola et al. 2008; Krantz and Ostergren 2002). Not all studies have taken into account possible confounding or effect modification by other factors.
Depression and distress are the two most widely studied kinds of symptoms in the studies summarized above. However, none of the studies tried to distinguish between depression and distress. Distress is seldom clearly defined as a distinct entity but it is generally and loosely conceived of as a collection of signs and symptoms indicating otherwise unspecified mental health problems, including anxiety and depression, stress-related symptoms, emotional ill-being, and functional impairment (Ridner 2004; Emmanuel and St John 2010). As such, the concept of distress is broader than depression and encompasses depression to a large degree. Distress scales, such as the General Health Questionnaire (GHQ), have been used to screen for psychiatric disorders in large populations (Goldberg et al. 1997), illustrating the fact that distress includes depressive and anxiety disorders. While, traditionally, the concept of distress is theoretically linked to the social model of stress and coping, the concept of depression is associated with the medical model. However, some authors have pointed out that, over the past decades, the depression concept has been broadened to the extent that it overlaps with distress to a large extent (Middleton and Shaw 2000; Horwitz and Wakefield 2007). Therefore, depression and distress questionnaires often measure more or less overlapping constructs. Most studies described above involved only one kind of symptoms (e.g. depression). Only one study merged various symptoms in a single predictive model to partial out the unique impact of certain types of symptoms on the outcome of SA (Eriksen et al. 2003). In addition, none of the studies that we know of studied anxiety symptoms as determinant of SA and only a few studies paid attention to the differential effect of various severity levels of the symptoms studied (Bültmann et al. 2006; Lexis et al. 2009; Ahola et al. 2008), the severity threshold at which psychological symptoms start to impact on SA.
The present paper reports a large-scale prospective study into the relationships between psychological symptoms and subsequent SA frequency and duration among employees of a Dutch telecom company. Four dimensions of psychological symptoms, including distress, depression, anxiety, and somatization, were assessed using a validated questionnaire, whereas 12-month SA data were obtained from the company’s occupational health service registration. We addressed the following questions: (1) At which levels of severity are psychological symptoms associated with subsequent SA frequency and duration? (2) Which particular symptom dimensions are associated with which aspects of SA, frequency or duration? (3) Are these relationships modified by employee characteristics such as age, gender, education, function, and life style?
Methods
Design and participants
The present study utilized data from a study that was originally designed as an intervention study evaluating two different stress management programs (van Rhenen et al. 2007). An occupational health survey was administered to all employees (n = 7,522) of a large Dutch telecom company. Completion of the survey was strictly voluntary, and respondents consented to the use of their anonymized data. As the data were collected as part of a regular periodical occupational health survey and did not involve any health risks, ethical review was not necessary. All employees with a score ≥10 on the distress scale of the Four-Dimensional Symptom Questionnaire (4DSQ) and an equal number of randomly chosen employees with a distress score <10 were invited to take part in one of two preventive stress reduction programs (physical or cognitive), provided by the company’s health service. The invitation was accepted by 32% of the distressed employees and by 60% of the non-distressed employees but the interventions did not prove to exert an effect on SA (van Rhenen et al. 2007). Because of the low participation rates and the absence of an effect on SA, we assumed that it was safe to include the participants of the stress reduction programs into the present study. Exclusion of these participants was not an option since the willingness to participate in a stress reduction program may well be relevant for the association between psychological symptoms and SA, and exclusion of the participants might therefore bias the results. Exclusion of all the employees who were invited to the stress reduction programs was not an option because this would mean that all distressed employees would be excluded and that the association between distress and SA could no longer be studied. SA data were registered by the company’s occupational health service. Because the focus of the present study was on the association between current psychological symptoms and future SA, employees who were absent due to sickness at the time of the survey were excluded.
Measurements
Psychological symptoms
The independent (determinant) variables of interest consisted of the scales of the Four-Dimensional Symptom Questionnaire (4DSQ) that measures distress, depression, anxiety, and somatization (Terluin et al. 2006). These dimensions, which emerged from the factor analysis of the psychological symptomatology of primary care patients, are necessary and sufficient to describe the whole range of common psychological complaints (Terluin 1996). The 4DSQ contains 50 items that are scored on a 3-point scale (no symptoms: 0; sometimes: 1; regularly, often or very often: 2). The distress and somatization scales contain 16 items each (score range 0–32), the anxiety scale consists of 12 items (score range 0–24), and the depression scale comprises 6 items (score range 0–12). The distress scale measures the discomforting, emotional state experienced by an individual in response to a specific stressor or demand (Ridner 2004). High distress scores indicate that the individual is having a hard time trying to handle the stressor or demand and trying to maintain an acceptable level of psychosocial functioning (Terluin et al. 2004). Distress is characteristic of the symptoms of numerous people who are stressed or overworked, seen in primary care and occupational health care. The depression scale measures specific depressive symptoms such as depressive thoughts (including suicidal ideation) and loss of pleasure (anhedonia) and indicates the probability of suffering from a (moderate or severe) depressive disorder (Terluin et al. 2009). The anxiety scale measures specific pathological anxiety symptoms, such as free-floating anxiety, panic attacks, phobic anxiety, and avoidance behavior, and suggests the presence of one or more anxiety disorders, in particular panic disorder, agoraphobia, and social phobia (Terluin et al. 2009). The somatization scale measures ‘psychosomatic’ symptoms that represent bodily stress reactions when the symptoms are few and mild, but psychiatric illness when the complaints are multiple and severe (Clarke and Smith 2000). It should be noted that, unlike many depression and anxiety scales currently in use, the 4DSQ depression and anxiety scales focus specifically on the severe, ‘clinical’, disorder end of the depression, and anxiety spectra. So-called ‘mild’ or ‘subclinical’ symptoms of depression (e.g. feeling down, lack of energy) and anxiety (e.g. worry, feeling tense) are to be found in the 4DSQ distress scale, along with other stress-related symptoms. In line with the general nature of distress and the disorder nature of depression and anxiety, a special hierarchical relationship exists between distress on the one hand and depression and anxiety on the other hand (Terluin et al. 2006). High depression and anxiety scores are virtually always accompanied by high distress scores. However, the reverse is not true. Some people can have high distress scores without having any substantial depressive or anxiety symptoms. Distress represents the most general response to mental health and psychosocial problems of any kind. Including both distress and depression (or anxiety) in one regression model provides the opportunity to test whether the effect of depression (or anxiety) on SA is due to the association of depression (or anxiety) with distress, and, at the same time, whether the effect of distress on SA is due to the association between distress and depression (or anxiety). Reliability coefficients (Cronbach’s alpha) of the 4DSQ scales in this study were as follows: distress 0.90, depression 0.82, anxiety 0.79, and somatization 0.80. The validity of the 4DSQ has been established in a number of ways (Terluin et al. 2004, 2006, 2009).
Sickness absence
The dependent (outcome) variable in this study was SA due to any reason during the 12-month period following the survey, as registered by the occupational health service. SA was recorded in calendar days, taking into account possible partial SA. A possible part-time employment factor was not taken into account. Thus, one week of SA of a full-time employee was counted as 7 days of SA, and one week SA of a part-time employee was also counted as 7 days of SA, but one week of 50% partial SA of a (full or part time) employee was counted as 3.5 days of SA. Partial SA often occurred at the end of SA spells of more than 4 weeks duration, as a result of partial return to work. We used two SA measures: the number of SA spells in 12 months (SA frequency) and the number of SA days in 12 months, given the SA frequency (SA duration).
Background variables
We measured a number of employee characteristics that were taken into account as possible confounders and effect modifiers. Gender, age, marital status, and salary were obtained from the company’s files, and therefore, we could use these variables to compare respondents with non-respondents. Education, function, number of years in current job, smoking, and alcohol consumption were asked by straightforward questions in the survey. Body mass index (BMI) was calculated from self-reported body weight and length. To avoid problems with possible non-linear relationships, all employee characteristics were categorized.
Analyses
First, we determined possible relevant cutoff points for the 4DSQ scales using bivariate analyses of the relationships between the separate 4DSQ scales and each SA outcome. A priori we decided not to use the conventional 4DSQ cutoff points because these ‘clinical’ cutoff points have been developed in primary care settings and may not be the most relevant cutoff points to explain SA in an occupational sample. To avoid any prior assumptions regarding (non-)linearity of the relationships between the 4DSQ scores and subsequent SA, the 4DSQ scales were divided into as many categories as was feasible, observing a minimum of 50 subjects per category. Since the number of SA spells was a count variable, we used Poisson regression to investigate the relationships between the 4DSQ scores and the SA frequency. Because, for a given employee, being absent due to sickness obviously reduced the number of days ‘at risk’ for getting a new SA spell, we allowed for differences in ‘exposure’ due to SA by using the natural logarithm of the proportion of non-SA days per 12 months as offset variable (Welch 2009). A small degree of overdispersion of the distribution of SA spells was taken into account by using the inverse of the deviance divided by the degrees of freedom value as scale weight (Welch 2009).
The number of SA days can also be considered a count variable. However, the ‘events’ of SA days are unlikely to be independent. Following a given SA day, the probability of another SA day is much higher than following a normal (non-SA) day. Because of the resulting large degree of overdispersion of the distribution of SA days, Poisson regression was not appropriate. Therefore, we used negative binomial regression analysis to study the relationships between the 4DSQ scores and the number of SA days (SA duration), rounded to whole days. We included the SA frequency as a covariate in these analyses to adjust for the number of SA spells. We limited the analysis of the SA duration to employees with one or more SA spells because modeling the SA duration obviously is inappropriate for employees without any SA. Note that the outcome variable of the latter analyses (i.e. the 12-month SA duration adjusted for the SA frequency) was independent of the outcome variable of the former analyses (i.e. the number of SA spells in 12 months). Cutoff points were determined based on visual inspection of the plots of the effect measures, rate ratios (RRs) for the Poisson regression analysis, and count ratios (CRs) for the negative binomial regression analysis, respectively. This resulted in fewer categories per 4DSQ scale.
Second, we determined the associations between the 4DSQ scores and each of the SA outcomes. Regression analysis was used in an explanatory way. That is, the purpose of the analyses was to establish the nature and strength of the association between psychological symptoms as determinants and subsequent SA as the outcome, accounting for possible confounders and effect modifiers. A confounder is a third variable that is correlated both with a determinant and with the outcome. Including the confounder as a covariate in the regression model produces an unbiased estimate of the regression coefficient of the determinant (McNamee 2005). The regression coefficient is said to be ‘adjusted’ for the confounder. Note that, in the regression equation, determinant(s) and confounder(s) are statistically equivalent. What is called a determinant and what is called a confounder is defined by the researcher. When two or more determinants are entered in a single regression model, the regression coefficients of the determinants are automatically adjusted for any mutual confounding among the determinants. When the relationship between a determinant and the outcome differs depending on a third variable, that variable is called an effect modifier. For instance, if the association between depression and SA is much stronger in women than in men, gender is called an effect modifier of the association between depression and SA.
Poisson regression was used for the SA frequency, in the way described above, and negative binomial regression for the SA duration adjusted for the SA frequency. In turn, each of the 4DSQ scales was entered in the analysis as determinant, while the other 4DSQ scales were entered as covariates one by one to test them for being a confounder and/or an effect modifier of the relationship between the determinant and SA. A change in the Beta coefficient of the determinant of 10% or more was taken as evidence of significant confounding. Next, interaction terms of the determinant and the 4DSQ scale were entered into the regression to test for effect modification. A statistically significant interaction term was taken as evidence of effect modification (p < 0.001 was adopted to account for multiple testing). Next, the four 4DSQ scales were entered simultaneously in multivariate regression models. This resulted in the first two models describing the relationships between the 4DSQ scales and subsequent SA, controlling for mutual confounding and effect modification of the 4DSQ scales.
Third, we investigated whether employee characteristics (gender, age, marital status, education, function, number of years in current job, salary, smoking, alcohol consumption, and BMI) were confounders and/or effect modifiers of the relationships between the 4DSQ scores and the SA outcomes. To that end, the employee characteristics were tested one by one by entering them as covariates into the multivariate models obtained before. We used the same criteria for significant confounding and effect modification as described above. After having tested all characteristics in this way, significant confounders and interactions were added to the multivariate models with the 4DSQ scores. In order to obtain the simplest possible models, interaction terms that had become non-significant and covariates that did not cause a 10% change in Beta upon removal were discarded. This resulted in the final two models describing the multivariate relationships between the 4DSQ scores and the SA outcomes, adjusted for employee characteristics.
All analyses were performed with SPSS 15. Differences between respondents and non-respondents were tested using chi-square test for proportions, t test for normally distributed continuous variables, and Mann–Whitney U test for non-normally distributed variables.
Results
Sample description
The survey was completed and returned by 3,852 employees (response rate 51%), of which 160 were absent due to sickness at that time. Of the 3,670 non-respondents, 303 were also on sick leave. Due to missing SA data (14 respondents, 16 non-respondents), the respondents sample reduces to 3,678 and the non-respondents sample to 3,351. Non-response analysis revealed that the respondents were 3 years older, more often men and more often married, they earned a slightly higher salary, and had slightly less SA, compared with the non-respondents (Table 1). The respondents had a mean of 1.17 SA spells and a mean total of 14.5 SA days during the subsequent 12 months. The total number of respondents with one or more SA spell was 2,313 (62.9%). Table 2 displays the mean 4DSQ scores and the prevalence rates of low, moderate, and high 4DSQ scores according to conventional ‘clinical’ cutoff points, demonstrating the relatively healthy condition of the sample from a clinical point of view. Only 13.7% of the respondents scored moderate or high on any of the 4DSQ scales.
Determining cutoff points for the 4DSQ scales
We divided the distress scale into 15 categories, the depression scale into 5, the anxiety scale into 6, and the somatization scale into 14 categories. Marked floor effects accounted for the relatively small number of categories of the anxiety and depression scales.
The number of SA spells was associated with all four dimensions of the 4DSQ (Fig. 1, solid lines, left Y-axis). Moderate to severe somatization (scores ≥ 11) appeared to be the strongest determinant of the SA frequency, responsible for a 2–2.5 fold increase in the SA frequency compared to employees with a zero score on somatization (the reference category). Furthermore, Fig. 1 suggests that distress was a stronger determinant of the SA frequency than anxiety and depression. The number of SA days, adjusted for the SA frequency, was also associated with all four 4DSQ dimensions (Fig. 1, dashed lines, right Y-axis). Among the employees who had at least one day of SA, those with distress scores ≥21 had more than 3 times the number of SA days of employees with a distress score of zero (the reference category). However, there were only 65 employees with such high distress scores. After inspection of the plots in Fig. 1, somewhat arbitrarily, we trichotomized the scales along the following cutoff points: distress ≥5 and ≥11, depression ≥1 and ≥3, anxiety ≥1 and ≥4, and somatization ≥4 and ≥11. For the distress, depression, and somatization scales, the highest cutoff points relevant for SA were chosen to coincide with the lowest conventional ‘clinical’ cutoff points. However, for the anxiety scale, a lower cutoff point had to be chosen, underlining the fact that the conventional cutoff points of the anxiety scale need downward revision (Terluin et al. 2009). The percentages of employees in the various categories were as follows: distress 0–4: 68.8%, distress 5–10: 21.6%, distress 11–32: 9.7%, depression 0: 85.6%, depression 1–2: 11.0%, depression 3–12: 3.5%, anxiety 0: 72.3%, anxiety 1–3: 22.6%, anxiety 4–24: 5.1%, somatization 0–3: 61.7%, somatization 4–10: 31.6%, somatization 11–32: 6.7%. For convenience, we will denote the highest symptom levels as ‘clinical’ and the next highest as ‘subclinical’. Note that these ‘subclinical’ symptom levels (i.e. distress 5–10, depression 1–2, anxiety 1–3, and somatization 4–10), which are usually considered as relatively ‘normal’ and not indicative of clinically important mental problems (Terluin et al. 2004, 2006), appeared to be associated with an increased SA risk.
Plots of the outcomes of the bivariate Poisson regression analyses of the relationships between the 4DSQ scores and the SA frequency, as well as the outcomes of the bivariate negative binomial regression analyses of the relationships between the 4DSQ scores and the number of SA days adjusted for the SA frequency. The outcomes of the Poisson regressions are expressed in rate ratios (RR, solid lines, left Y-axis); the outcomes of the negative binomial regressions are expressed in count ratios (CR, black dashed lines, right Y-axis). Significant estimates are indicated by an asterisk when p < 0.05, or by a cross when p < 0.001. Proposed cutoff scores are indicated by vertical gray dashed lines
Sickness absence frequency
In the bivariate models, all 4DSQ scales were significantly associated with the SA frequency (Table 3). Since Poisson regression models the natural logarithm of the event rate, e (the base of the natural logarithm) raised to the power B (in short Exp(B)) represents an easily interpretable statistic. The Exp(B) of the intercept represents the event rate in individuals in whom the value of the determinant was zero. So, employees who scored in the lowest category of distress were predicted to have had a mean rate of 1.07 SA spells in the subsequent 12 months. The Exp(B) value of a determinant represents the rate ratio (RR) for that determinant. So, employees with ‘subclinical’ distress scores (scores 5–10) were predicted to have had a mean rate of SA spells of 1.33 times the SA rate of the reference group, i.e. 1.33 × 1.07 = 1.42 SA spells in 12 months. With respect to the association between distress and the SA frequency, the anxiety and somatization scales (but not the depression scale) turned out to be significant confounders. Likewise, with respect to the association between somatization and the SA frequency, the anxiety and distress scales turned out to be significant confounders. Concerning the association between anxiety and the SA frequency, the distress and somatization scales turned out to be significant confounders. Finally, regarding the association between depression and the SA frequency, all other three scales turned out to be significant confounders. There was no significant interaction between the 4DSQ scales (data not shown).
After entering the 4DSQ scales into a single multivariate model, accounting for mutual confounding among the 4DSQ scales, ‘subclinical’ depression and anxiety scores turned out to be no longer significant determinants of the SA frequency, while ‘clinical’ depression and anxiety scores had lost much of their power (p for ‘clinical’ depression scores: 0.059; p for ‘clinical’ anxiety scores: 0.046; Table 3, model 1). The Wald chi-square statistics indicated that somatization was the most powerful determinant among the 4DSQ dimensions.
Of the employee characteristics tested, the employee function turned out to be a significant confounder of the association between the anxiety score and the SA frequency. No significant interactions were discovered. In the final adjusted multivariate model of the associations between the 4DSQ scales and the SA frequency, ‘clinical’ levels of depressive and anxiety symptoms were no longer significant (Table 3, model 2). ‘Clinical’ and ‘subclinical’ levels of distress and somatization were associated with increased SA rates. Especially, ‘clinical’ levels of somatization (scores 11–32) were associated with a markedly increased SA rate (RR 1.69). However, ‘subclinical’ levels of distress (scores 5–10) and somatization (scores 4–10) were also responsible for 13 and 34% more SA spells (RRs 1.13 and 1.34). The confounder employee function was retained in the model because discarding it would have produced biased estimates of the associations between distress/somatization and SA frequency. The direct effect of employee function on SA frequency was not the present study’s focus.
Sickness absence duration
The bivariate models demonstrated that all 4DSQ scales were significantly associated with the SA duration (Table 4). Since negative binomial regression models the natural logarithm of the count, the predicted number of SA days for employees who had had only one SA spell and who scored in the lowest categories for distress can be calculated as 12.03 × 1.28 = 15.4 days. The Exp(B) value of a determinant represents the count ratio (CR) for that determinant. So, employees with one SA spell and a distress score in the ‘clinical’ range (scores 11–32) were predicted to have had 1.91 times as many SA days as employees with low distress scores (scores 0–4), i.e. 1.91 × 15.4 = 29.4 days. With respect to the association between distress and the SA duration, the depression and somatization scales (but not the anxiety scale) turned out to be significant confounders. Regarding the association between depression, anxiety and somatization and the SA duration, all other three scales turned out to be significant confounders. There was no significant interaction between the 4DSQ scales (data not shown).
When entering the 4DSQ scales, together with the SA frequency, into one multivariate negative binomial regression model, accounting for mutual confounding among the 4DSQ scales, the depression and anxiety scores, as well as ‘subclinical’ distress, turned out to be no longer significant determinants (Table 4, model 1).
Of the employee characteristics tested, educational level and salary turned out to be significant confounders of both distress and somatization. No significant interactions surfaced. After adding education and salary as covariates to model 1, salary (but not education) could be removed from the model without causing a 10% change in the Beta coefficients. The final adjusted model for the SA duration (Table 4, model 2) demonstrates that, adjusted for the SA frequency, ‘clinical’ levels of distress (scores 11–32) and somatization (scores 11–32) were associated with a marked increase in SA duration with 50 and 45%, respectively (CR 1.50 en 1.45) compared with low distress and somatization. ‘Subclinical’ somatization (scores 4–10) was also associated with a significant increase in the SA duration (CR 1.34). The model predicts that when an employee suffering both ‘clinical’ distress and ‘subclinical’ somatization reported sick, the expected SA duration was twice the SA duration of an employee with low distress and somatization, who reported sick (CR 1.50 × 1.34 = 2.01). Whether or not this person also had a ‘clinical’ level of depressive or anxiety symptoms (which might well have been the case), did not have any impact on the expected SA duration.
Discussion
In accordance with previous research, we ascertained that psychological symptoms predicted SA during the subsequent 12 months. These symptoms appeared to be more robustly associated with the frequency of SA spells than with the duration of SA given the SA frequency. Not only clearly elevated ‘clinical’ symptom levels, but also ‘subclinical’ levels, usually considered to be quite ‘normal’ and belonging to the everyday ‘stress of life’, appeared to be associated with SA, especially with the frequency of SA spells.
Before we discuss our findings in detail, it is important to acquire a deeper understanding of what was actually measured in our sample with respect to psychological symptoms and psychiatric disorders. The prevalence of ‘clinical’ symptom levels of depression and anxiety was 3.5% for depression and 1.1% for anxiety. The cutoff point of the 4DSQ anxiety scale may need to be downwardly revised, but even when ≥4 is adopted as the cutoff of ‘clinical’ anxiety symptoms, no more than 5.1% of the sample qualified for that label. These figures illustrate the low prevalence of clinical depression and anxiety in our sample. However, at the same time, these figures compare reasonably well with the prevalence of depressive and anxiety disorders reported in other studies using psychiatric interviews. The prevalence of major depressive disorder in working people is reported to be 2.3% by Kouzis and Eaton (1994) and 4.4% by Kessler and Frank (1997). Interestingly, in other studies, the prevalence of depressive symptoms is reported to be as high as 16.5–25.7% in occupational samples (Lexis et al. 2009; Niedhammer et al. 1998). There appears to be a big difference between depressive symptoms and depressive disorder, suggesting that depressive symptoms do not accurately provide information on depressive disorder. When we look at studies reporting the prevalence of distress in employee samples, figures vary between 12 and 25% (Kouzis and Eaton 1994; Hilton et al. 2008; Bültmann et al. 2005; Virtanen et al. 2007). Since the concept of distress includes depressive symptoms (among other symptoms), and given the similar prevalence figures for distress and depressive symptoms, the conclusion seems justified that depressive symptom scales not only measure symptoms of depressive disorder but often measure what is called distress too. Rarely, if ever, an attempt is made to disentangle distress from depression. Some researchers study ‘depression’ and other researchers study ‘distress’ and, very likely, they study more or less the same phenomenon using different labels. The 4DSQ employs a different approach insofar its depression scale focuses specifically on symptoms of depressive disorder. In addition, the 4DSQ comprises a separate distress scale. Note that the 4DSQ distress scale, like other distress scales, measures what is sometimes labeled ‘depression’. Note also that most ‘depression’ scales measure two components: a depressive disorder component and a depressive symptoms component, which is also present in measures of distress. We need these insights when interpreting our results.
When the different dimensions of psychological symptoms (i.e. distress, depression, anxiety, and somatization) were merged into one multivariate model, only somatization and distress remained significantly associated with SA. The (‘clinical’) depression and anxiety scores, indicative of the possible existence of depressive and anxiety disorders (Terluin et al. 2009), lost their association with subsequent SA after distress and somatization had been taken into account. How does this fit in with the literature? After all, the effect of depression on SA has been established on several occasions. Given the correlation between depression and distress, it would be wrong to adjust the depression–SA association for distress in the case when distress is actually part of the causal chain between depression and SA. However, although it seems plausible that depression causes distress and distress causes sickness absence, it is highly unlikely that this is the whole story. Just the fact that depression is less prevalent than distress precludes the possibility that distress be entirely caused by depression. Rather, previous research suggests that distress causes depression (Terluin et al. 2006). Imagine one of our participants who, at the time of the survey, had a ‘clinical’ level of distress and a ‘subclinical’ level of somatization (according to the 4DSQ). This person had a significantly increased risk of having one or more SA spells in the subsequent year. This person might well have had a ‘clinical’ level of depressive symptoms too or, for that matter, might even have been suffering from a major depressive disorder. However, the presence of clinically significant depression would not have had any influence on the risk of SA. Since depression is virtually always accompanied by distress and to a variable degree accompanied by somatization, most persons with clinically significant depression will have an increased risk of SA, but the depression itself does not add to this risk. In other words, the effect of depression on SA is due to the fact that depression is associated with distress (and somatization) and that these latter symptom dimensions are associated with subsequent SA. When depression is measured with an instrument that actually includes distress to a large extent, it seems obvious that the distress component (and not the depressive disorder component) of the scale is responsible for its association with SA. Somatization and distress are key to understand why depression is related to SA. A similar reasoning applies to anxiety. In other words, it seems that depression and anxiety do not impact SA in the capacity of being a psychiatric disorder, but rather because of the distress and somatization that accompanies the disorder. Without the disorder, the same amount of distress and somatization has the same effect on SA. A depressive or anxiety disorder in itself does not have an extra effect on SA.
The nature of the association between distress and subsequent SA is not immediately apparent. There may be a direct causal relationship insofar ‘clinical’ distress itself may abate a person’s capability to work because of its effects on energy and motivation, the ability to concentrate, and irritability. Reduced energy and motivation make it difficult to sustain normal working hours especially in demanding jobs, concentration difficulties cause the employee to make more and more serious mistakes, and irritability may provoke conflicts with colleagues, superiors, and clients. However, ‘subclinical’ distress does not have such detrimental effects on the ability to work. The relationship between distress and SA may also be more indirect. Distress reflects a stress and coping process. So, work stress and stress in the person’s private life, as well as one’s coping abilities and social support, may all play a part. SA has been described as a special kind of coping behavior (Kristensen 1991; Hackett and Bycio 1996). The person takes a ‘timeout’ in order to restore his mental and physical equilibrium and to prevent more serious future illness. In the present study, we did not take into account measures of (work) stress, coping, and social support. Another explanation might be that distress compromises the immune system, giving rise to minor ailments and infections, which in turn lead to SA spells. We did not take into account the actual reasons for SA.
Somatization appeared to be consistently associated with the SA frequency in all groups and for both severity levels that we distinguished. An important reason why somatization, especially ‘clinical’ somatization, leads to SA most likely is that somatizing people just feel physically sick and not fit for work. In addition, somatization, especially ‘subclinical’ somatization, may be driven by stress, inadequate coping en insufficient social support, and, like distressed employees, somatizing individuals may feel the desire to take a ‘timeout’ to recuperate.
When SA is considered as purposeful employee behavior, the SA frequency can be regarded as the expression of the subjective need to interrupt the week after week work routine, whereas the SA duration, adjusted for the SA frequency, can be considered to represent the amount of time an employee, once on sick leave, needs in order to arrive at the moment when the perceived benefits of returning to work outweigh the perceived advantages of continued SA. Our results indicate that employees with somatization or ‘clinical’ levels of distress generally need significantly more time off work before they reach that moment.
In spite of differences in symptom measures and methodology, our results regarding the magnitude of the effects of psychological symptoms on SA compare reasonably well with the effect measures reported in the literature, as summarized in the introduction. Without trying to be comprehensive, a few examples will be presented here. Kivimäki et al. (2001) studied prospectively the 2-year SA in a cohort of hospital staff. Being a case on the General Health Questionnaire (GHQ-12, score > 3) was one of the predictors studied using Poisson regression analysis. The RRs for short SA spells (1–3 days) were 1.26 for doctors and 1.21 for nurses, whereas the RRs for long SA spells (>3 days) were 1.79 and 1.55, respectively. The GHQ is a well-known measure of distress, correlating 0.58 with the 4DSQ distress scale (Terluin et al. 2006). Lexis et al. (2009) studied the effect of depressive symptoms, measured by the depression scale of the Hospital Anxiety and Depression Scale (HADS), on subsequent 10-month SA in an epidemiological cohort, using Cox proportional hazard regression analysis. The hazard ratio (HR) was 1.20 (men) and 1.36 (women) for mild complaints (HADS score 8–10) and 1.57 (men) and 1.56 (women) for moderate to severe complaints (HADS score > 10). The HR is very much comparable with the RR. The HADS depression scale correlates 0.49 with the 4DSQ depression scale but 0.67 with the 4DSQ distress scale, illustrating the distress component in the HADS depression scale (Terluin et al. 2006). Eriksen et al. (2003) studied prospectively the occurrence of SA longer than 3 days in a cohort of nurses’ aides, during a period of 3 months. In a multivariate model, pain and fatigue were among the most powerful predictors with odds ratios (ORs) of 1.41 (for a little pain), 1.82 (for rather intense pain), 2.43 (for intense pain), and 1.73 (for always fatigued). The OR is to some extent comparable with the RR for relatively low rates. Pain and fatigue are well-known symptoms of somatization.
The present study had a number of limitations. The most important limitation was the fact that the study was performed in a single company with a male-dominated population. Although this was a large company with a highly heterogeneous population of employees, ranging from low educated blue-collar workers to highly educated technicians and managers, some of the findings may be attributed to the company’s SA ‘culture’. Our sample did not have as many women as men. From the fact that we did not find any effect modification by gender, it can be concluded that the associations between psychological symptoms and subsequent SA were not any different between women and men. Yet, it is difficult to tell how well our findings can be generalized to other companies and other countries and cultures. Another limitation derives from the relatively low response rate (51%). The relationships between psychological symptoms and SA may have been stronger or weaker in non-respondents. Furthermore, no data were available on psychiatric diagnoses and physical diseases, actual reasons for SA, and details about work stress and stress in the employees’ private lives. The fact that some employees participated in a stress reduction program, aimed at preventing SA, deserves some further consideration. Given the facts that the majority of employees had not been exposed to the programs and that the programs did not have an impact on SA, the chances of biased results seem minimal (Moons et al. 2009). However, should the programs have had any small but undetected effects on SA, this would have implied that the associations between distress/somatization and SA have been under-estimated. It is highly unlikely that the stress reduction programs could have produced spurious associations between distress/somatization and SA. The final limitation concerns the use of the 4DSQ. Our results rest heavily on the way the 4DSQ operationalizes distress, depression, anxiety, and somatization. Future studies using different instruments to assess distress, somatization, anxiety, and depression, including standardized diagnostic interviews for depressive and anxiety disorders, should clarify whether the effects of anxiety and depression are really only due to the accompanying distress and somatization. Strengths of our study include the large sample size, the simultaneous analysis of four dimensions of psychological symptoms, the independent registration of SA data, and the allowance for confounding and effect modification.
In conclusion, somatization and distress are important determinants of subsequent SA and key to understand why depression and anxiety are related to SA. Whether this is a genuine causal relationship and which mechanisms are responsible for the link between these mental health problems and SA, need further study.
References
Ahola K, Kivimäki M, Honkonen T et al (2008) Occupational burnout and medically certified sickness absence: a population-based study of Finnish employees. J Psychosom Res 64:185–193. doi:10.1016/j.jpsychores.2007.06.022
Andrea H, Beurskens AJHM, Metsemakers JFM et al (2003) Health problems and psychosocial work environment as predictors of long term sickness absence in employees who visited the occupational physician and/or general practitioner in relation to work: a prospective study. Occup Environ Med 60:295–300. doi:10.1136/oem.60.4.295
Borritz M, Rugulies R, Christensen KB et al (2006) Burnout as a predictor of self-reported sickness absence among human service workers: prospective findings from three year follow up of the PUMA study. Occup Environ Med 63:98–106. doi:10.1136/oem.2004.019364
Bourbonnais R, Mondor M (2001) Job strain and sickness absence among nurses in the province of Québec. Am J Ind Med 39:194–202. doi:10.1002/1097-0274(200102)39:2<194:AID-AJIM1006>3.0.CO;2-K
Broadhead WE, Blazer DG, George LK et al (1990) Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 264:2524–2528
Bültmann U, Huibers MJH, van Amelsvoort LGPM et al (2005) Psychological distress, fatigue and long-term sickness absence: prospective results from the Maastricht Cohort Study. J Occup Environ Med 47:941–947. doi:10.1097/01.jom.0000172865.07397.9a
Bültmann U, Rugulies R, Lund T et al (2006) Depressive symptoms and the risk of long-term sickness absence: a prospective study among 4747 employees in Denmark. Soc Psychiatry Psychiatr Epidemiol 41:875–880. doi:10.1007/s00127-006-0110-y
Clarke DM, Smith GC (2000) Somatisation: what is it? Aust Fam Physician 29:109–113
Dewa CS, Lin E (2000) Chronic physical illness, psychiatric disorder and disability in the workplace. Soc Sci Med 51:41–50
Duijts SFA, Kant IJ, Landeweerd JA et al (2006) Prediction of sickness absence: development of a screening instrument. Occup Environ Med 63:564–569. doi:10.1136/oem.2005.024521
Duijts SFA, Kant IJ, Swaen GMH et al (2007) A meta-analysis of observational studies identifies predictors of sickness absence. J Clin Epidemiol 60:1105–1115. doi:10.1016/j.jclinepi.2007.04.008
Emmanuel E, St John W (2010) Maternal distress: a concept analysis. J Adv Nurs 66:2104–2115. doi:10.1111/j.1365-2648.2010.05371.x
Eriksen W, Bruusgaard D, Knardahl S (2003) Work factors as predictors of sickness absence: a three month prospective study of nurses’ aides. Occup Environ Med 60:271–278. doi:10.1136/oem.60.4.271
Goldberg DP, Gater R, Sartorius N et al (1997) The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 27:191–197
Hackett RD, Bycio P (1996) An evaluation of employee absenteeism as a coping mechanism among hospital nurses. J Occup Organ Psychol 69:327–338
Hensing G, Wahlström R (2004) Sickness absence and psychiatric disorders. Scand J Public Health 32(Suppl 63):152–180. doi:10.1080/14034950410021871
Hensing G, Alexanderson K, Allebeck P et al (1998) How to measure sickness absence? Literature review and suggestion of five basic measures. Scand J Soc Med 26:133–144. doi:10.1080/14034949850153662
Hilton MF, Scuffham PA, Sheridan J et al (2008) Mental ill-health and the differential effect of employee type on absenteeism and presenteeism. J Occup Environ Med 50:1228–1243. doi:10.1097/JOM.0b013e31818c30a8 [Published: November 2008]
Horwitz AV, Wakefield JC (2007) The loss of sadness. How psychiatry transformed normal sorrow into depressive disorder. Oxford University Press, New York
Janssen N, Kant IJ, Swaen GMH et al (2003) Fatigue as a predictor of sickness absence: results from the Maastricht cohort study on fatigue at work. Occup Environ Med 60(Suppl 1):i71–i76. doi:10.1136/oem.60.suppl_1.i71
Jenkins R (1985) Minor psychiatric morbidity in employed young men and women and its contribution to sickness absence. Br J Ind Med 42:147–154. doi:10.1136/oem.42.3.147
Kessler RC, Frank RG (1997) The impact of psychiatric disorders on work loss days. Psychol Med 27:861–873. doi:10.1017/S0033291797004807
Kivimäki M, Sutinen R, Elovainio M et al (2001) Sickness absence in hospital physicians: 2 year follow up study on determinants. Occup Environ Med 58:361–366. doi:10.1136/oem.58.6.361
Kivimäki M, Leino-Arjas P, Kaila-Kangas L et al (2007) Increased absence due to sickness among employees with fibromyalgia. Ann Rheum Dis 66:65–69. doi:10.1136/ard.2006.053819
Kouzis AC, Eaton WW (1994) Emotional disability days: prevalence and predictors. Am J Public Health 84:1304–1307
Krantz G, Ostergren PO (2002) Do common symptoms in women predict long spells of sickness absence? A prospective community-based study on Swedish women 40 to 50 years of age. Scand J Public Health 30:176–183. doi:10.1177/140349480203000303
Kristensen TS (1991) Sickness absence and work strain among Danish slaughterhouse workers: an analysis of absence from work regarded as coping behaviour. Soc Sci Med 32:15–27
Kruijshaar ME, Hoeymans N, Bijl RV et al (2003) Levels of disability in major depression: findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). J Affect Disord 77:53–64. doi:10.1016/S0165-0327(02)00099-X
Laitinen-Krispijn S, Bijl RV (2000) Mental disorders and employee sickness absence: the NEMESIS study. Soc Psychiatry Psychiatr Epidemiol 35:71–77
Lexis MAS, Jansen NWH, van Amelsvoort LGPM et al (2009) Depressive complaints as a predictor of sickness absence among the working population. J Occup Environ Med 51:887–895. doi:10.1097/JOM.0b013e3181aa012a
McNamee R (2005) Regression modelling and other methods to control confounding. Occup Environ Med 62:500–506. doi:10.1136/oem.2002.001115
Middleton H, Shaw I (2000) Distinguishing mental illness in primary care. We need to separate proper syndromes from generalised distress. BMJ 320:1420–1421. doi:10.1136/bmj.320.7247.1420
Moons KGM, Royston P, Vergouwe Y et al (2009) Prognosis and prognostic research: what, why, and how? BMJ 338:1317–1320. doi:10.1136/bmj.b375
Niedhammer I, Goldberg M, Leclerc A et al (1998) Psychosocial factors at work and subsequent depressive symptoms in the Gazel cohort. Scand J Work Environ Health 24:197–205
Ridner SH (2004) Psychological distress: concept analysis. J Adv Nurs 45:536–545. doi:10.1046/j.1365-2648.2003.02938.x
Suija K, Kalda R, Maaroos HI (2009) Patients with depressive disorder, their co-morbidity, visiting rate and disability in relation to self-evaluation of physical and mental health: a cross-sectional study in family practice. BMC Fam Pract 10:38. doi:10.1186/1471-2296-10-38
Terluin B (1996) De Vierdimensionale Klachtenlijst (4DKL). Een vragenlijst voor het meten van distress, depressie, angst en somatisatie [The four-dimensional symptom questionnaire (4DSQ). A questionnaire to measure distress, depression, anxiety, and somatization]. Huisarts Wet 39:538–547
Terluin B, van Rhenen W, Schaufeli WB et al (2004) The four-dimensional symptom questionnaire (4DSQ): measuring distress and other mental health problems in a working population. Work Stress 18:187–207. doi:10.1080/0267837042000297535
Terluin B, Van Marwijk HWJ, Adèr HJ et al (2006) The four-dimensional symptom questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry 6:34. doi:10.1186/1471-244X-6-34
Terluin B, Brouwers EPM, van Marwijk HWJ et al (2009) Detecting depressive and anxiety disorders in distressed patients in primary care; comparative diagnostic accuracy of the four-dimensional symptom questionnaire (4DSQ) and the hospital anxiety and depression scale (HADS). BMC Fam Pract 10:58. doi:10.1186/1471-2296-10-58
Väänänen A, Toppinen-Tanner S, Kalimo R et al (2003) Job characteristics, physical and psychological symptoms, and social support as antecedents of sickness absence among men and women in the private industrial sector. Soc Sci Med 57:807–824
van Rhenen W, Blonk RWB, Schaufeli WB et al (2007) Can sickness absence be reduced by stress reduction programs: on the effectiveness of two approaches. Int Arch Occup Environ Health 80:505–515. doi:10.1007/s00420-006-0157-9
Virtanen M, Vahtera J, Pentti J et al (2007) Job strain and psychologic distress: influence on sickness absence among Finnish employees. Am J Prev Med 33:182–187. doi:10.1016/j.amepre.2007.05.003
Welch K (2009) Generalized linear models using SPSS. Ann Arbor, MI: University of Michigan. http://www-personal.umich.edu/~kwelch/510/2009/handouts/spss_poisson_regression.doc. Accessed 5 April 2011
Conflict of interest
BT is the copyright owner of the 4DSQ and receives copyright fees from companies that use the 4DSQ on a commercial basis (the 4DSQ is freely available for non-commercial use in health care and research). BT received fees from various institutions for workshops on the application of the 4DSQ in primary care settings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terluin, B., van Rhenen, W., Anema, J.R. et al. Psychological symptoms and subsequent sickness absence. Int Arch Occup Environ Health 84, 825–837 (2011). https://doi.org/10.1007/s00420-011-0637-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-011-0637-4