Abstract
Objectives
To investigate whether work-time influence moderated the effect of shift work on psychological well-being measured as vitality, mental health, somatic stress symptoms, and disturbed sleep.
Methods
We used questionnaire data from 2,148 health care workers who finished their education in 2004 and were followed during their first 2 years of employment in the eldercare and health care sectors. We analyzed the effect of shift work, work-time influence, and the combination of these two variables adjusted for differences in baseline psychological well-being, background factors, and psychosocial work environment.
Results
Surprisingly, in this cohort, shift workers had higher vitality and better mental health than day workers. The combination of shift work and moderate or low work-time influence was associated with lower vitality, worse mental health, and more somatic stress symptoms than would have been expected when adding the separate effects of working hours and work-time influence. Work-time influence did not have any effect among day workers.
Conclusion
Shift workers appear to be especially vulnerable to the negative effect of moderate or low work-time influence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shift work has been associated with suboptimal psychological health and well-being including such outcomes as fatigue (Jansen et al. 2003), sub-clinical depression (Bildt and Michelsen 2002), stress symptoms (Kandolin 1993), and sleepiness (Åkerstedt 2003). Still, the evidence of an effect of shift work on chronic mental health problems is mixed (Tucker and Knowles 2008). Nevertheless, shift work (defined as work outside conventional day time (Bøggild and Knutsson 1999)) is an unavoidable part of the job for some occupational groups. For example, many employees in the eldercare must work evening or night shifts as well as weekends to provide 24-h care (Geiger-Brown et al. 2004; Nabe-Nielsen et al. 2010). In situations where shift work is unavoidable, other solutions must be considered in order to reduce potential negative consequences.
One possible solution is to increase employee influence on the work schedule. Work-time influence could be exerted in many different ways ranging from complete self-scheduling (see for example Lowden and Åkerstedt (2000)) to a more loosely defined possibility of making changes (see for example Viitasalo et al. (2008)). Increased influence on own working hours could help employees to balance individual needs with work requirements (Baltes et al. 1999) and thereby improve the possibilities for mental recovery and stress reduction. Thus, our theoretical model implies that the negative effect of demanding working hours could be leveled out by influence on the working hours, as this influence could be used to schedule the working hours according to the employees’ preferences. This theory is supported empirically, as intervention studies of individual work-time influence have demonstrated positive effects (Joyce et al. 2010). More specifically, better work-life balance, higher job satisfaction, social support, and sense of community have been found among nurses and health care workers (Pryce et al. 2006), decreased tiredness has been found among midwifes (Kandolin and Huida 1996), and increased satisfaction with colleagues and reduced sleep problems have been found among retail workers (Lowden and Åkerstedt 2000).
In addition to the main effect of work-time influence, we also hypothesize that the effect of work-time influence differs between day workers and shift workers. As shift work may affect social life, health, and well-being (see for example Puttonen et al. (2010)), shift workers may be more in need of work-time influence compared with day workers. Nevertheless, none of the previous intervention studies analyzed whether shift workers profited more from increased work-time influence or were more vulnerable to lack of work-time influence than day workers. Yet, cross-sectional studies have found that work-time influence reduced the association between overtime work and mental distress (Kandolin et al. 2001) and also the association between long working hours and work–family interference (Hughes and Parkes 2007). Importantly, stronger study designs appear to corroborate the cross-sectional data. In a large prospective study of municipal employees, high work-time control reduced the association between long domestic and total working hours on the one hand and sickness absence on the other (Ala-Mursula et al. 2006). Another study of the same cohort found that control over daily working hours and days off moderated the association between work stressors and sickness absence (Ala-Mursula et al. 2005).
The aim of this study was, thus, to investigate whether work-time influence moderated the effect of shift work on psychological well-being measured as self-reported vitality, mental health, somatic stress, and disturbed sleep. Our measure of shift work only reflected which time(s) of the day, the participants were usually working. To minimize bias due to the healthy worker effect and residual confounding, the present study was conducted in a homogenous cohort of social and health care workers with one year of working experience in the eldercare or health care sector.
Methods
Design and study population
Data used in the present study came from a prospective cohort study, “The Danish Health Care Worker Cohort—Class of 2004” (DHCWC-2004), of Danish social and health care helpers and assistants (SHC helpers and SHC assistants) who finished their education during 2004. SHC helpers have 14 months of training and are qualified for providing care of elderly people. SHC assistants are SHC helpers with an additional 20 months of training. The SHC assistants are qualified for working in the eldercare sector, hospitals, and psychiatry.
The cohort study consisted of a baseline questionnaire administered a few weeks before the students finished their education (2004) and a follow-up questionnaire survey after one (2005) and two (2006) years. The study population consisted of 6,347 students from 27 out of the 28 Danish schools educating SHC helpers and assistants. A total of 5,696 (90%) participants returned the baseline questionnaire. The 2005 questionnaire was returned by 3,708 (65%) of the baseline respondents, and the 2006 questionnaire was returned by 3,161 (56%) of the baseline respondents. A total of 2,774 participants returned all three questionnaires. To be included in the analyses, the participants should be employed in the eldercare or health care sector in 2005 and also respond to both questions on their work-time influence and their working hours (n = 2,148). On average, the participants had 11.4 months of working experience one year after finishing their education as SHC helper or assistant. However, 44.8% reported having previous experience from working in the eldercare or health care sector.
The present study analyzed the effect of working hours and work-time influence (exposures) in 2005 on psychological well-being (outcome) in 2006. We adjusted for background factors and pre-exposure psychological well-being measured in 2004 and other working environment variables measured in 2005.
Exposure measurements in 2005
Work-time influence was measured by the question “do you have influence on the planning of your own working hours” with the response options “yes” (reference), “partly”, and “no”. These exposure categories are referred to as “high” (equal to answering “yes”), “moderate” (equal to answering “partly”), and “low” (equal to answering “no”) work-time influence. We also asked the participants at which time of the day they usually worked. The responses were categorized into “day work” (reference, 53%) and “shift work”. Shift work consisted of evening work (17%), night work (4%), and combinations of day work, evening work, and night work (26%).
Indicators of psychological well-being in 2004 and 2006
We used four scales as outcome measures. “Vitality” (4 items) concerned whether the participants felt energetic, felt worn out, or were tired (Cronbach’s alpha 0.87). “Mental health” (5 items) concerned how often the participants felt nervous, blue or happy (Cronbach’s alpha 0.85). The vitality and mental health scales had six response options ranging from “all the time” to “never”. “Somatic stress” (4 items) concerned how often the participants suffered from stomach ache, a tight chest or chest pains, dizziness, and muscle tension (Cronbach’s alpha = 0.69). The somatic stress scale had five response options ranging from “always” to “never/almost never”. These scales came from the Copenhagen Psychosocial Questionnaire 1st version (Kristensen et al. 2005). “Disturbed sleep” (4 items) concerned how often the participants slept restlessly, had difficulties falling asleep, or experienced premature awakening or repeated awakenings (Cronbach’s alpha 0.88). The disturbed sleep scale was derived from the Karolinska Sleep Questionnaire, and the scale was also in use in the Copenhagen Psychosocial Questionnaire 2nd version (Pejtersen et al. 2010; Åkerstedt et al. 2002). The disturbed sleep scale had five response options ranging from “all the time” to “never”. For all the scales, the response on each item was coded from 0 to 100, and a scale score was calculated as the mean score of all the items in the scale as described by Pejtersen et al. (2010). A score of 100 represented the highest degree of the condition under study, i.e. the highest degree of vitality or the best mental health and the most somatic stress symptoms or disturbed sleep.
From the baseline measurements in 2004 to the second follow-up in 2006, we found a small improvement in mental health (mean difference = 0.94; p = 0.018) and less disturbed sleep (mean difference = −4.30; p = 0.000). However, we also found a decreased vitality (mean difference = −4.49; p = 0.000) and more somatic stress symptoms (mean difference = 3.96; p = 0.000).
Covariates measured in 2004 and 2005
The individual background factors measured at baseline were age, gender, and education (SHC helper or assistant). The work schedule characteristic was self-reported number of working hours per week. The psychosocial work factors included general influence (concerning one’s own work and what one does at work; 2 items; Cronbach’s alpha 0.74), emotional demands (emotionally disturbing situations at work; 1 item), demands for hiding emotions (required to hide feelings; 1 item), and social support from leaders and colleagues (sufficient support when I have too much to do or difficult problems, encouragement and recognition of how I perform at work; 3 items in each scale) (Cronbach’s alpha 0.87 and 0.83, respectively). The scales were derived from the Copenhagen Psychosocial Questionnaire 1st version (Kristensen et al. 2005). In accordance with the manuals, all psychosocial scales were re-coded from 0 to 100 points. A high score indicated a high degree of influence, demands, and support. These work factors were adjusted for, as previous research has indicated that the exposure to these factors differs between shifts (Bøggild et al. 2001; Nabe-Nielsen et al. 2009).
The distribution (frequency or mean and standard deviation) of the variables in the study is presented in Table 1.
Statistical analyses
For the statistical analyses presented in Table 2, we employed general linear models (GLM) that estimate the difference in the mean score of each outcome variable together with the 95% confidence intervals (95% CI). The GLM was chosen as all outcome variables were continuous and approximately normally distributed.
In model 1, we analyzed the effect of working hours, work-time influence, and working hours*work-time influence on the outcome adjusted for age, gender, education, and the baseline level of the outcome.
In model 2, we added the self-reported number of working hours per week, together with the self-reported emotional demands, demands for hiding emotions, general influence, and support from colleagues and leaders.
Significant interaction was defined as departure from additivity meaning that the combined effect of working hours and work-time influence differed significantly from the sum of the individual effects of the two variables (Rothman and Greenland 1998).
In all models, “day work” and “high work-time influence” were used as reference. We considered the effects statistically significant if the overall p value was <5% and the 95% confidence intervals of the estimates did not include zero.
Additionally, we used t tests to analyze whether those who were included in the study differed from those who were not eligible for inclusion either because they did not respond to one of the questionnaires, were not employed in the eldercare or health care sector, or did not report their working hours or level of work-time influence. We analyzed whether there were significant baseline differences with respect to vitality, mental health, somatic stress, and disturbed sleep. We also analyzed whether working hours and degree of work-time influence in 2005 were associated with inclusion in the study.
To estimate the potential selection of healthy workers into day work or shift work or into jobs with a high degree of work-time influence, we further tested whether psychological health at baseline predicted working hours and degree of work-time influence at follow-up using binary and nomial logistic regression.
We also used t test to conduct pairwise comparisons of the psychological well-being in 2004, 2005, and 2006 among fixed evening workers fixed night workers, and workers with combinations of day, evening, and/or night work too elucidate whether these groups differed with respect to psychological well-being.
Results
Vitality
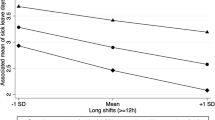
In the fully adjusted model (Table 2, model 2), the vitality level was significantly higher among shift workers than among day workers with high work-time influence (7.2; 95% CI: 3.7 to 10.7). We found no significant effect of work-time influence (p = 0.786) among day workers. However, the results showed that the combination of shift work and moderate or low work-time influence was associated with a lower vitality than would have been expected when adding the separate effects of working hours and work-time influence (−6.6; 95% CI: −10.7 to −2.3 and −5.4; 95% CI: −9.7 to −1.1). In the fully adjusted model, working hours and work-time influence explained <2% of the variance, while baseline vitality explained 14%.
Mental health
Among participants with high work-time influence, shift workers reported better mental health than day workers (5.0; 95% CI: 2.1 to 7.8) (Table 2, model 2). We found no significant effect of work-time influence among day workers (p = 0.197). However, the combination of shift work and moderate (but not low) work-time influence was associated with a significantly worse mental health than would have been expected when adding the separate effects of working hours and work-time influence (−5.3; 95% CI: −8.8 to −1.8). In the fully adjusted model, working hours and work-time influence explained <2% of the variance, while baseline mental health explained 10%.
Somatic stress
We found no significant effect of neither shift work (p = 0.134) nor work-time influence (p = 0.485) (Table 2, model 2) on somatic stress. The combination of shift work and moderate or low work-time influence was, however, associated with a significantly higher somatic stress level than would have been expected when adding the separate effects of working hours and work-time influence (5.2; 95% CI 1.3 to 9.0 and 3.9; 95% CI: 0.01 to 7.7). In the fully adjusted model, working hours and work-time influence explained <1% of the variance while baseline somatic stress explained 15%.
Disturbed sleep
We did not find any effect of working hours or work-time influence on disturbed sleep. Neither did the results show any interaction between working hours and work-time influence on this outcome. In the fully adjusted model, working hours and work-time influence explained <1% of the variance, while baseline disturbed sleep explained 20%.
Dropout analyses
Due to dropout from the study, dropout from the occupation, and missing values, only 37.7% of the baseline respondents were eligible for inclusion in the present study. At baseline, those who were included in the analyses differed from those who were not included: Dropouts had a significantly poorer self-reported mental health, lower degree of vitality, and experienced more somatic stress symptoms. The mean differences were between 1.37 and 2.77 points. Working hours (shift work or day work) and degree of work-time influence measured in 2005, however, were not associated with dropout.
Selection bias
We found no baseline differences in psychological well-being when comparing those who took up day work and those who took up shift work one year later (Table 1). However, the four indicators of psychological well-being at baseline (2004) were associated with work-time influence in 2005, i.e. meaning that the higher vitality/mental health score or the lower somatic stress/disturbed sleep score in 2004, the higher was work-time influence in 2005.
Comparison of employees with evening work, night work, or combined working hours
Pairwise comparison of the psychological well-being in 2004, 2005, and 2006 among fixed evening workers, fixed night workers, and workers with combinations of day, evening, and/or night work revealed that these groups did not differ with respect to psychological well-being.
Discussion
Our results showed that among SHC helpers and assistants with high work-time influence, shift workers had a higher level of vitality and better mental health 2 years after entering the labor market than day workers. Importantly, these groups did not differ with respect to psychological well-being before taking up day work or shift work. We found no overall significant effect of working hours or work-time influence on somatic stress symptoms and disturbed sleep. The combination of shift work and moderate or low work-time influence was, however, associated with worse psychological well-being than would have been expected when adding the separate effects of working hours and work-time influence. Thus, the results indicate that moderate or low influence on the working hours offsets the otherwise better psychological well-being among shift workers in this study. These results mean that shift work in this sample was associated with better psychological well-being but only in combination with high work-time influence, whereas day workers and shift workers did not differ from each other in the groups with moderate or low work-time influence.
Our results are supported by previous research showing that individual work-time flexibility moderates the effect of demanding working hours (Ala-Mursula et al. 2006; Hughes and Parkes 2007; Kandolin et al. 2001) and work stressors (Ala-Mursula et al. 2005), although none of these studies focus specifically on shift work. As evening and night work implies working unsocial hours (Wirtz et al. 2008) and increased sleepiness (Åkerstedt 2003), shift workers may be especially vulnerable to the exact scheduling of such shifts. Having influence on the scheduling of these shifts may increase the employees’ possibility of adjusting the working hours to family needs, need-for-recovery, private appointments, and other leisure-time activities taking place in the afternoon or evening.
Although the moderating effect of work-time influence may be considered small (4–6 points on scales from 0 to 100), the authors of the “User’s manual for the SF-36v2™ Health Survey” state that even a 3-point decrease in vitality or mental health is associated with an increased risk of inability to work, job loss, and mortality. A 3-point decrease in vitality is further associated with an increased risk of hospitalization, while a 3-point decrease in mental health is associated with an increased risk of using mental health services (Ware et al. 2007). Additionally, somatic stress symptoms (or “physical stress reactions”) are a risk factor of coronary heart disease among women, and the predictive ability of these symptoms is about the same level as biomedical risk factors (Hallman et al. 2001).
This study did not support the hypothesis of a general effect of work-time influence, as we did not find an overall effect on any of the outcomes. This result is in contrast to the findings of previous observational studies. These studies reported a negative association between degree of work-time influence and fatigue, stress, and psychological distress (Ala-Mursula et al. 2004; Costa et al. 2006). Furthermore, one intervention study showed an effect of introducing individual flexibility on tiredness (Kandolin and Huida 1996). Our inclusion of an interaction term and our extensive adjustment for confounding may explain some of the inconsistency in the findings compared with previous research. Another contribution to the inconsistency could be variations in the operationalization of work-time influence, for example, our use of a single, global item might not capture important differences in degree of work-time influence.
Our finding of a better psychological well-being among shift working SHC helpers and assistants is in opposition to previous studies. These studies reported more fatigue, sub-clinical depression, stress symptoms, and sleep problems among shift workers (Bildt and Michelsen 2002; Jansen et al. 2003; Kandolin 1993; Åkerstedt 2003). As fixed evening workers, fixed night workers, and workers with combinations of day, evening, and/or night work did not differ with respect to psychological well-being, our categorization of these employees into one group of shift workers did not hide important differences that might explain inconsistencies with previous findings.
The few studies on selection into shift work indicate selection mechanisms related to age, sleep pattern, and lifestyle habits (Knutsson and Åkerstedt 1992; Nabe-Nielsen et al. 2008; van Amelsvoort et al. 2004). Additionally, one study found that fatigue predicted changing from shift work to day work (Jansen et al. 2003), and a mismatch between work-time preferences and actual working hours was associated with self-reported intention to leave the workplace (Nabe-Nielsen et al. 2010). Thus, the results from these studies indicate that various selection mechanisms are at play. In the present study, we hypothesize that choosing shift work is a result of a liberate choice based on personal needs and preferences due to the current lack of qualified workers in the eldercare and health care sectors. This choice could also be considered as a way to exert a “once and for all” influence on the working hours (Bøggild 2009). The four indicators of psychological well-being at baseline (2004) were associated with work-time influence in 2005. Therefore, to reduce confounding, we adjusted for vitality, mental health, somatic stress symptoms, and sleep disturbances measured at baseline (2004). The fact that psychological well-being in 2004 was not associated with working hours in 2005 indicates that there was no strong selection of healthy workers into shift work. Still, we can not rule out a selection of unhealthy workers out of shift work or out of the study.
The present study was strengthened by the large sample (n = 2,148), and the cohort is unique as it includes almost all SCH helpers and assistants who finished their education in Denmark in 2004. Although about one-third of the participants had previous working experience from the eldercare or health care sector, the participants can be viewed as “non-exposed” when they entered the study. The homogeneity of the participants also reduced the risk of residual confounding, and additionally we adjusted for differences in the baseline level of each outcome, background factors, and psychosocial work environment. In post-hoc analyses, we also adjusted for “living with children” (yes or no) and “workplace” (homes for elderly requiring full-time care, home care, hospitals, or other). However, these covariates were not associated with psychological well-being, and they did not change the associations between shift work, work-time influence, and well-being.
Our use of self-reported exposure and outcome measures implies the risk of common method bias. Ala-Mursula et al. (2006) do, however, suggest that it is unlikely that the perception of work-time control could depend only on individual characteristics, and our study is further strengthened by our use of validated outcome measures (Kristensen et al. 2005; Setterlind and Larsson 1995; Åkerstedt et al. 2002). Yet, even though the outcomes are constructed as different scales, the correlations between vitality, mental health, somatic stress symptoms, and disturbed sleep were between 0.43 and 0.77. These high correlations are not surprising, though, as all scales estimate aspects of the participants’ psychological well-being.
Due to the homogeneity of the study sample, the contrast in the degree of work-time influence may be smaller than in other studies including several occupational groups (Ala-Mursula et al. 2006; Costa et al. 2006). However, the degree of potential individual flexibility among the participants in this study may be limited, because health care personnel are most often required to be present at a certain place at a certain time. Therefore, lack of contrast is not due to a sampling error, but rather a consequence of the working conditions in the eldercare and health care sectors.
The study is weakened by the relatively wide time span between each measurement (about one year). The participants’ psychological well-being, working hours and work-time influence may be fluctuating leading to complex causal pathways with reverse effects that are difficult to disentangle. In the present sample, 14.9% had changed from shift work to day work or vice versa, while 47.9% changed level of work-time influence between 2005 and 2006. Change of job did not explain the change in work-time influence in this study. However, the extent to which the employees have influence on their own working hours may largely depend on their local leader. And as the leaders are frequently changing especially in the eldercare sector, this may explain some of the change in the self-reported degree of work-time influence. Variability in the exposures makes the results less reliable, especially if the exposures are expected to have a rather acute effect (e.g. within a few months). Additionally, the participants filled in the baseline questionnaire in a period where they were taking their final examinations. Thus, the participants might be more distressed than usual, which may have affected the baseline measures of psychological well-being. The advantage of adjusting for the 2004 measures of psychological well-being (as opposed to the 2005 measures) is that we avoided that psychological well-being was already affected by the degree of work-time influence. However, we cannot rule out that psychological well-being biased the perception and reporting of work-time influence. Furthermore, as psychological well-being at baseline was associated with work-time influence at first follow-up, psychological well-being might play a role when it comes to actually obtaining influence on own working hours.
Conclusion
In this cohort of employees working in the eldercare or health care sector, we found that moderate or low work-time influence had a negative effect on the psychological well-being among shift workers but not among day workers. Surprisingly, shift workers with high work-time influence reported better psychological well-being than day workers. This result may, however, not be valid for occupational groups with frequent involuntary shift work.
Our conclusion stresses the importance of involving shift workers in the planning of their work schedule, because shift workers appear to be especially vulnerable to the detrimental effect of low work-time influence.
References
Åkerstedt T (2003) Shift work and disturbed sleep/wakefulness. Occup Med (Lond) 53:89–94
Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G (2002) Sleep disturbances, work stress and work hours: a cross-sectional study. J Psychosom Res 53:741–748
Ala-Mursula L, Vahtera J, Pentti J, Kivimäki M (2004) Effect of employee worktime control on health: a prospective cohort study. Occup Environ Med 61:254–261
Ala-Mursula L, Vahtera J, Linna A, Pentti J, Kivimäki M (2005) Employee worktime control moderates the effects of job strain and effort-reward imbalance on sickness absence: the 10-town study. J Epidemiol Community Health 59:851–857
Ala-Mursula L, Vahtera J, Kouvonen A, Väänänen A, Linna A, Pentti J, Kivimäki M (2006) Long hours in paid and domestic work and subsequent sickness absence: does control over daily working hours matter? Occup Environ Med 63:608–616
Baltes BB, Briggs TE, Huff JW, Wright JA, Neuman GA (1999) Flexible and compressed workweek schedules: a meta-analysis of their effects on work-related criteria. J Appl Psychol 84:496–513
Bildt C, Michelsen H (2002) Gender differences in the effects from working conditions on mental health: a 4-year follow-up. Int Arch Occup Environ Health 75:252–258
Bøggild H (2009) Settling the question—the next review on shift work and heart disease in 2019. Scand J Work Environ Health 35:157–161
Bøggild H, Knutsson A (1999) Shift work, risk factors and cardiovascular disease [review]. Scand J Work Environ Health 25:85–99
Bøggild H, Burr H, Tüchsen F, Jeppesen HJ (2001) Work environment of Danish shift and day workers. Scand J Work Environ Health 27:97–105
Costa G, Sartori S, Åkerstedt T (2006) Influence of flexibility and variability of working hours on health and well-being. Chronobiol Int 23:1125–1137
Geiger-Brown J, Muntaner C, Lipscomb JA, Trinkoff AM (2004) Demanding work schedules and mental health in nursing assistants working in nursing homes. Work Stress 18:292–304
Hallman T, Burell G, Setterlind S, Oden A, Lisspers J (2001) Psychosocial risk factors for coronary heart disease, their importance compared with other risk factors and gender differences in sensitivity. J Cardiovasc Risk 8:39–49
Hughes E, Parkes KR (2007) Work hours and well-being: the roles of work-time control and work-family interference. Work Stress 21:264–278
Jansen NW, van Amelsvoort LG, Kristensen TS, van den Brandt PA, Kant IJ (2003) Work schedules and fatigue: a prospective cohort study. Occup Environ Med 60(suppl 1): i47–i53
Joyce K, Pabayo R, Critchley JA, Bambra C (2010) Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev 2:CD008009
Kandolin I (1993) Burnout of female and male nurses in shiftwork. Ergonomics 36:141–147
Kandolin I, Huida O (1996) Individual flexibility: an essential prerequisite in arranging shift schedules for midwives. J Nurs Manag 4:213–217
Kandolin I, Härmä M, Toivanen M (2001) Flexible working hours and well-being in Finland. J Hum Ergol (Tokyo) 30:35–40
Knutsson A, Åkerstedt T (1992) The healthy-worker effect: self-selection among Swedish shift workers. Work Stress 6:163–167
Kristensen TS, Hannerz H, Hogh A, Borg V (2005) The Copenhagen psychosocial questionnaire–a tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 31:438–449
Lowden A, Åkerstedt T (2000) Introduction of self-selected work hours in retail work—effects on work satisfaction, health and social life. Arb Wiss 54:300–305
Nabe-Nielsen K, Garde AH, Tüchsen F, Hogh A, Diderichsen F (2008) Cardiovascular risk factors and primary selection into shift work. Scand J Work Environ Health 34:206–212
Nabe-Nielsen K, Tüchsen F, Christensen KB, Garde AH, Diderichsen F (2009) Differences between day and nonday workers in exposure to physical and psychosocial work factors in the Danish eldercare sector. Scand J Work Environ Health 35:48–55
Nabe-Nielsen K, Kecklund G, Ingre M, Skotte J, Diderichsen F, Garde AH (2010) The importance of individual preferences when evaluating the associations between working hours and indicators of health and well-being. Appl Ergon 41:779–786
Pejtersen JH, Kristensen TS, Borg V, Bjorner JB (2010) The second version of the Copenhagen psychosocial questionnaire. Scand J Pub Health 38:8–24
Pryce J, Albertsen K, Nielsen K (2006) Evaluation of an open-rota system in a Danish psychiatric hospital: a mechanism for improving job satisfaction and work-life balance. J Nurs Manag 14:282–288
Puttonen S, Härmä M, Hublin C (2010) Shift work and cardiovascular disease—pathways from circadian stress to morbidity. Scand J Work Environ Health 36:96–108
Rothman KJ, Greenland S (1998) Modern epidemiology. Lippincott-Raven Publishers, Philadelphia
Setterlind S, Larsson G (1995) The stress profile: a psychosocial approach to measuring stress. Stress Med 11:85–92
Tucker P, Knowles SR (2008) Review of studies that have used the Standard Shiftwork Index: evidence for the underlying model of shiftwork and health. Appl Ergon 39:550–564
van Amelsvoort LG, Schouten EG, Kok FJ (2004) Impact of one year of shift work on cardiovascular disease risk factors. J Occup Environ Med 46:699–706
Viitasalo K, Kuosma E, Laitinen J, Härmä M (2008) Effects of shift rotation and the flexibility of a shift system on daytime alertness and cardiovascular risk factors. Scand J Work Environ Health 34:198–205
Ware JE Jr, Kosinski M, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME (2007) User’s manual for the SF-36–v2TM health survey. QualityMetric Incoporated, Lincoln, RI
Wirtz A, Giebel O, Schomann C, Nachreiner F (2008) The interference of flexible working times with the utility of time: a predictor of social impairment? Chronobiol Int 25:249–261
Acknowledgments
This study was financed by the national budget through a special three-year grant to the SOSU research programme at the National Research Centre for the Working Environment.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nabe-Nielsen, K., Garde, A.H., Albertsen, K. et al. The moderating effect of work-time influence on the effect of shift work: a prospective cohort study. Int Arch Occup Environ Health 84, 551–559 (2011). https://doi.org/10.1007/s00420-010-0592-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-010-0592-5