Abstract
Purpose
We conducted this study to determine if the preterm risks due to PM10 exposure vary with the exposure periods during pregnancy. This study was also conducted to estimate the different effects of PM10 exposure on preterm birth by exposure periods using the extended Cox model with PM10 exposure as a time-dependent covariate.
Methods
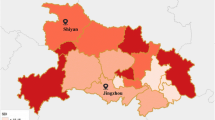
We studied birth data obtained from the Korea National Statistical office for 374,167 subjects who were delivered between 1998 and 2000 in Seoul, South Korea. We used PM10 data that was measured hourly to give 24-h averages at 27 monitoring stations in Seoul. The extended Cox model with time-dependent exposure was used to determine if the risk of preterm delivery could be associated with PM10 exposures for each trimester during pregnancy.
Results
Effect of PM10 exposure prior to the 37 weeks of gestational period was stronger on the risk of premature birth than that posterior to the 37 weeks of gestational weeks. This trend was consistent for each trimester; however, the hazard ratios for preterm delivery associated with PM10 exposure in the first and third trimester were slightly higher than those of the second trimester.
Conclusions
The risk of preterm birth associated with exposure to PM10 differed with the exposure period of the neonates. Therefore, when studying the impact of air pollution exposure during pregnancy, the exposure period during pregnancy should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational age, infant birth weight and growth of the fetus may have an effect on perinatal health. In addition, perinatal death, infant mortality, and illnesses in adults can all be caused by preterm birth, which is defined as delivery prior to 37 weeks of pregnancy (Joseph and Kramer 1996). Many studies have shown that environmental factors, including cigarette smoking (Horta et al. 1997; Cnattingius et al. 2006; Raatikainen et al. 2007), environmental tobacco smoke (ETS) (Windham et al. 2000; Kharrazi et al. 2004), organic solvents (Wang et al. 2000; Ha et al. 2002), and alcohol consumption can contribute to preterm delivery (Albertsen et al. 2004). The relationship between birth outcomes and air pollution exposure has also been examined in many epidemiological studies that have been conducted to evaluate factors including total suspended particulates (TSP) (Wang et al. 1997; Bobak and Leon 1999; Bobak 2000; Ha et al. 2001), sulfur dioxide (SO2) (Wang et al. 1997; Bobak and Leon 1999; Bobak 2000; Ha et al. 2001; Maisonet et al. 2001), carbon monoxide (CO) (Ha et al. 2001; Maisonet et al. 2001; Ritz and Yu 1999; Medeiros and Gouveia 2005; Salam et al. 2005), ozone (O3) (Salam et al. 2005; Hansen et al. 2006), nitrogen dioxide (NO2) (Ha et al. 2001; Medeiros and Gouveia 2005), and particulate matter <10 μm (PM10) (Bobak and Leon 1999; Medeiros and Gouveia 2005; Hansen et al. 2006; Dejmek et al. 1999; Ritz et al. 2000; Ha et al. 2003; Rogers and Dunlop 2006; Leem et al. 2006). In a previous study that we conducted in Seoul, South Korea, exposure to air pollution during pregnancy was found to be significantly associated with the occurrence of preterm birth (Ha et al. 2004).
The association of premature delivery with air pollution exposure during pregnancy has been investigated using various statistical approaches that can be classified as community- or individual-based. In studies that use a community-based approach, a time-series analysis based on a Poisson regression model is commonly used to find the increment of preterm delivery due to air pollution exposure (Anderson et al. 2001; Roberts 2004; Roberts 2005; Peng et al. 2005; Sagiv et al. 2005). However, because the population-based approach assumes that the population contains homogeneous characteristics for the entire study period, it is difficult to use individual-based confounders that vary with time. Therefore, the individual-based approach has become more popular. This approach has generally involved the use of a logistic regression model in which the distribution of predictors is compared in women that experienced preterm birth and those who carried their child to term (Bobak 2000; Hansen et al. 2006; Ritz et al. 2000; Ha et al. 2004; Xu et al. 1995; Maroziene and Grazuleviciene 2002; Yang et al. 2002; Yang et al. 2003; Tsai et al. 2003; Woodruff et al. 2003; Liu et al. 2003; Wilhelm and Ritz 2005). For studies in which a quantitative outcome, such as gestational age or fetal growth associated with air pollution exposure is required, a linear regression analysis approach has commonly been performed (Xu et al. 1995; Hansen et al. 2007).
In a previously conducted study, we compared the results obtained when logistic regression and Cox proportional hazards models were used to investigate the relationship between pollution and preterm birth in South Korea (Ha et al. 2004). In the present study, which was conducted to determine if the risk for a preterm birth due to air pollution exposure varied with gestational age, we used the extended Cox model, after accounting for the time-dependent covariate. We then compared the results from (1) the conventional individual-based logistic regression analysis, (2) the conventional regression analysis, (3) the Cox proportional hazards model, and (4) the extended Cox model with time-dependent exposure to determine the usefulness of the time-to-event analysis rather than conventional approaches in the study of preterm delivery due to exposure to air pollution, such as PM10, in pregnant Korean women.
Materials and methods
Population and data collection
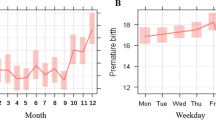
Birth data containing information such as the gender and weight of the infant, parental age, education and occupation, parity, birth order, gestational age, marital status, birth date, place of birth and history of delivery were obtained from the Korea National Statistical Office. Only subjects who were delivered between January 1, 1998 and December 31, 2000 in Seoul, South Korea were included in this study. The confounding factors to be controlled in this study were the gender of the infant, maternal age, paternal education, marital status, birth order, maternal occupation, maternal history of stillbirth, and month and day of the week at birth. Subjects who were born before 25 weeks or after 41 weeks of gestation were excluded, as were subjects who were delivered as multiple neonates. Finally 374,167 individuals were included in our analysis. The prevalence of preterm birth (before 37 weeks of gestation) in the subjects was 3.3% (N = 12,153).
Air pollution data
We obtained PM10 data, which was measured hourly to give 24-h averages at 27 monitoring stations in Seoul, from the National Institute of Environmental Research. We ruled out exposure data when there was a PM10 of ≥200 μg/m3 because these data may have been influenced by dust and sand storms in Mongolia or China. The air pollution exposure for each participant, based on the averaged exposure at 27 monitoring stations in Seoul, gestational age and delivery date, was then calculated for the first, second and third trimester. Each trimester was defined as 3 calendar months. Exposure during third trimester corresponded to the averaged exposure for a period from 186 days of gestation to birth. Infants with gestational duration less than 186 days have missing values for the third trimester exposure.
Statistical analysis
As a preliminary study, we investigated the relationship between preterm delivery and covariates, such as the gender of the infant, maternal age, paternal education, marital status, birth order, maternal occupation, maternal history of stillbirth and month and day of the week at birth using χ2 test or t test. We then evaluated the impact of PM10 exposure during each trimester to determine the risk of preterm birth and reduced pregnancy period using conventional statistical approaches, such as multiple logistic regression and multiple linear regression analyses, respectively, after adjusting for confounding factors and a continuous effect of a linear long-term trend. Odds ratios and regression coefficients were estimated for preterm delivery according to the increase of averaged interquartile range (IQR) of PM10 concentration levels in each trimester during pregnancy using the fitted logistic regression and regression models, respectively. As an alternative approach, we first performed Cox proportional hazards regression analysis, after adjusting for confounding factors and a continuous effect of long-term trend, on preterm delivery and estimated the hazard ratios for preterm birth according to the increase of averaged IQR of PM10 concentration levels in each trimester during pregnancy. We considered preterm delivery as an event and subject with a term birth as censoring in the Cox regression model. We censored the term births after 37 weeks of pregnancy at 38 gestational weeks in the Cox proportional hazards model (not at the date of birth). That is, the time variable of the Cox proportional hazards model was set to 38 for the term births after 37 weeks. Tied data were controlled by Breslow’s approximation. We next analyzed the data using an extended Cox model with time-dependent exposure, which permits nonproportional hazards, managing for a time-dependent covariate of PM10 exposure during each trimester by adding a product term on time function (Kleinbaum and Klein 2005). The statistical model for the extended Cox model with time-dependent exposure in this study was as follows: \( h(t|X(t)) = h_{0} (t)\exp [ {\sum\nolimits_{i = 1}^{p} {\beta_{i} X_{i} + \delta_{1} X_{1} g_{1} (t)} } ] \) for gestational age, t. In this equation, h 0(t) is a baseline hazard function as all covariates are zero, X i (i = 2, …, p) is the ith time-independent covariate, and X 1 × g 1(t) is a product term where g 1(t) is a function of t for X 1, which is a time-dependent covariate of PM10 exposure during each trimester. We first tried the extended Cox model containing dummy variables for different time periods. As a result, since the outcomes for different time periods showed linearity, we considered g 1(t) as a linear indicator function in this study. That is, we considered g 1(t) to be 1 if t < 32; 3 if 32 ≤ t < 37; 5 if t = 37; and 7 if t > 37. So, the corresponding hazard ratios per IQR of X 1 were estimated by \( {\text{HR}} = { \exp }[ {{\text{IQR}}( {\hat{\beta }_{1} + \hat{\delta }_{1} } )} ] \) if t < 32; \( {\text{HR}} = { \exp }[ {{\text{IQR}}( {\hat{\beta }_{1} + 3\hat{\delta }_{1} } )} ] \) if 32 ≤ t < 37; \( {\text{HR}} = { \exp }[ {{\text{IQR}}( {\hat{\beta }_{1} + 5\hat{\delta }_{1} } )} ] \) if t = 37; \( {\text{HR}} = { \exp }[ {{\text{IQR}}( {\hat{\beta }_{1} + 7\hat{\delta }_{1} } )} ] \) if t > 37 where \( \hat{\beta }_{1} \) and \( \hat{\delta }_{1} \) are estimated coefficients for X 1 and X 1 g 1(t), respectively. All statistical analyses were conducted using SAS (version 8.2, SAS institute, Cary, NC).
Results
Table 1 shows the distribution of the demographic characteristics of the subjects included in this study. The neonates in the preterm group and those in the control group differed by either gender or birth order (P < 0.0001 by χ2 test). In addition, the prevalence of preterm birth of male newborns (3.5%) was higher than that of female newborns (3.0%), and the prevalence of preterm birth increased as birth order increased. Further, fathers who carried their baby to preterm tended to be less educated than those who carried their baby to term (P < 0.001 by χ2 test), and there were also significant differences in maternal age, marital status, maternal history of stillbirth, and month and day of the week at birth between the preterm and control group, respectively (P < 0.0001 by t test or χ2 test). Additionally, the preterm birth rate of single mothers (5.3%) was much higher than that of married mothers (3.2%). Furthermore, the occurrence of a previous stillbirth had a strong impact on the occurrence of preterm birth (7.4%). However, the preterm and control group did not differ when maternal occupation was considered (P > 0.1 by χ2 test). There were 1,471 neonates in the early preterm group (25–31 weeks of gestation), 10,682 in the preterm group having 32–36 weeks of gestation, 13,585 in the control group having 37 week of gestation, and 348,429 in the group having 38–41 weeks of gestation.
Table 2 shows the distribution of PM10 concentration levels according to trimester. The exposure levels of PM10 were almost the same among the three different periods during pregnancy, and the mean IQR of PM10 concentration levels of all three trimesters during pregnancy was 16.53 μg/m3.
We initially evaluated the risks for preterm delivery according to 16.53 μg/m3 (averaged IQR) increase of PM10 exposure level during pregnancy using a logistic regression model for preterm birth, after adjusting for confounding factors and a long-term trend effect (Table 3). The results showed that, when the impact of PM10 exposure on the risk for preterm delivery according to trimester was evaluated, the risks for preterm birth attributed to the PM10 exposures were significantly higher in the third trimester. To verify that the effect of PM10 exposures on the risk of preterm delivery according to trimester differed by gestational age, we performed a further analysis according to the gestational age of the neonates. To accomplish this, separate logistic regression analyses were conducted according to the gestational ages of the preterm babies, which was subdivided into two sets (25–31 and 32–36 weeks). The results of these analyses showed that the risks for preterm delivery that was attributed to PM10 exposures differed based on the gestational age of neonates, and that these risks were significantly higher for premature babies with relatively shorter gestational ages in the third trimester.
We also used multiple linear regression analysis to confirm that PM10 exposure in the third trimester during pregnancy was a significant risk factor for preterm birth and obtained similar results to those obtained using the logistic regression method (Table 4). When we added an interactive effect between gestational age of the neonates and PM10 exposure to the multiple regression model, we were able to verify that the risk for reduced gestational age as a result of PM10 exposure was significant in each trimester during pregnancy, but was slightly higher in the third trimester than in the first or second trimester. In addition, the estimated regression coefficients of PM10 exposure on gestational age were reduced in a dose-dependant manner as the gestational age of the neonates decreased, and the risk for reduced gestational age associated with PM10 exposures tended to be higher for preterm babies that were born earlier, regardless of the period of PM10 exposure.
Because our data concerned the time-to-event data, we next performed Cox proportional hazards regression analysis after adjusting for confounding factors and a long-term trend effect, to estimate the hazard ratios for preterm birth according to 16.53 μg/m3 increase of PM10 exposure level during each trimester (Table 5). Almost same hazards for preterm delivery that was attributed to PM10 exposure were found in all trimesters, which were not statistically significant. It was hard to explain that there was not a risk for preterm birth associated with PM10 exposure; however, it was biologically well-explained that there were varied effects for birth weight reduction by PM10 exposure according to gestational age of the neonates. Therefore, we needed to use the methodology to estimate hazards varied with exposure period of the neonates in survival analysis. Moreover, the hazard ratios estimated by the Cox regression model were not valid statistically, since the assumption of proportional hazard function for PM10 exposure during each trimester was violated (P < 0.01 for interactions of PM10 exposure with time of exposure period). These results supported the finding that the hazard for preterm delivery associated with PM10 exposure during each trimester changed according to the time of gestational age of neonates. Therefore, we re-analyzed the data using an extended Cox model with time-dependent exposure after adjusting for confounding factors and a long-term trend effect and found that the estimated hazard ratio for preterm birth to PM10 exposure during each trimester varied with the gestational period of the neonates (Table 5). Among the periods of PM10 exposure, the hazard ratios for preterm delivery associated with PM10 exposure of the first and third trimester were slightly higher than those of the second trimester, and the trend of estimated hazard for preterm birth associated with PM10 exposure increased in a dose-dependant way as gestational duration decreased. Additionally, the estimated hazard ratios for preterm birth attributable to PM10 exposure were higher for preterm babies that were born within 25–31 weeks than for those that were born within 32–36 weeks, regardless of the PM10 exposure period.
Discussion
Exposure to adverse environmental agents is a well-known cause of preterm delivery, and many studies have shown that exposure to air pollution, such as PM10, leads to a greater risk of preterm delivery in each month or trimester during pregnancy. However, the period during pregnancy in which the effect of exposure is most significant has varied based on the location in which the study was conducted and the population used in the study. In a cohort study of 97,518 neonates in California, USA, Ritz et al. (2000) reported that the risk of preterm delivery after exposure to a 50 μg/m3 increase in PM10 levels rose 13% during the first month of pregnancy and 18% during the 6th week before delivery using logistic regression analysis. Hansen et al. (2006) conducted a retrospective cohort study of 28,200 newborns in Brisbane, Australia, and found that the OR for preterm delivery attributed to a 4.5 μg/m3 increase in PM10 exposure during the first trimester was 1.15 (95% CI = 1.06–1.25) using logistic regression analysis. In a study conducted on 52,113 neonates between 2001 and 2002 in Incheon, South Korea, Leem et al. (2006) found that the relative risk for preterm delivery was 1.27 times greater for women exposed to a high level of PM10 exposure (64.6–106.4 μg/m3) than for those exposed to a low PM10 (27.0–45.9 μg/m3) during the first trimester (95% CI = 1.04–1.56) using logistic regression analysis. In a previously conducted study of 382,100 newborn babies born in Seoul, South Korea, we detected a significant relationship between PM10 concentrations during pregnancy and preterm birth by logistic regression, generalized additive logistic regression and the proportional hazard model with the risk of preterm delivery after a 42.5 μg/m3 increase in PM10 exposure during the seventh month of pregnancy being 1.07 (95% CI = 1.01–1.14) when logistic regression model was used (Ha et al. 2004).
We used the extended Cox model with time-dependent PM10 exposure to confirm that the estimated hazard ratio for preterm birth to PM10 exposure during each trimester varied with the gestational period of the neonates in this study. The results obtained using the extended Cox model with time-dependent exposure were similar to those obtained when the multiple regression model was used when the interaction of PM10 exposure with gestational period was considered. The hazards for preterm birth associated with PM10 exposure were higher with shorter gestational periods of neonates, and fetuses were affected more by PM10 exposure with shorter gestational periods. This trend was consistent in each trimester; however, the hazard ratios for preterm delivery by PM10 exposure in the first and third trimester were slightly higher than those in the second trimester. Therefore, the risks for preterm delivery or reduced gestational age attributable to PM10 exposure during pregnancy according to the exposure period during pregnancy need to be further investigated. We note that the PM10 effects on the births after 37 weeks of gestation, which were as considered as censored data in the Cox model, can be statistically interpreted as the effects of exposure duration. But the PM10 effects on the births after 37 weeks of gestation are not meaningful as an epidemiological estimate of the preterm risk.
Survival analysis involves a statistical data analysis for which the outcome variable of concern is time until an event takes place. Preterm birth is characteristic of a time that corresponds to the gestational age until preterm birth occurs, therefore, it is reasonable to study preterm delivery using survival analysis. In O’Neill et al. (2003), they confirmed that survival analysis has an advantage over logistic regression analysis by accounting for time dependent exposure and outcome. They performed a sensitivity analysis to prove that the HR is better estimate than the OR in their study of urinary tract infection and preterm delivery (O’Neill et al. 2003). In this study, we used the extended Cox model after accounting for the time-dependent covariate to show that the effect of PM10 exposure differs with gestational period, and we found that this time-to-event analysis is more effective than conventional approaches in the study of preterm delivery. Platt et al. (2004) verified the effectiveness of the use of the extended Cox model with time-varying covariates for the study of fetal and infant death. In this study, we found that the effect of PM10 exposure on preterm delivery changes according to gestational period. Therefore, the environmental exposures that lead to an increased risk of preterm delivery in each trimester during pregnancy should be studied by different gestational periods.
It should be noted that our study had several limitations, including a lack of individual risk factors for preterm delivery, a low concentration of air pollutants in residential areas. We did not evaluate an accurate distance between each participant’s home address and the closest monitoring station due to a lack of exact Geographic Information System (GIS) data. Also, we could not take Caesarian section into account in the model, since the Birth data obtained from the Korea National Statistical Office had no information about a way of delivery. However, this study also showed several interesting features and strengths. For example, we found that PM10 exposure had a greater impact on fetuses with a shorter gestational age, which is reasonable considering the immaturity of the defense mechanisms to toxic insults of exogenous chemicals; however, this has rarely been shown in other studies on preterm birth. Our study also included a larger sample of Korean women than other studies.
In conclusion, the risk for preterm birth attributable to PM10 exposure differed by gestational periods. In studies evaluating the association of air pollution exposure during pregnancy to the risk for preterm delivery, exposure period during pregnancy should be considered.
References
Albertsen K, Andersen AM, Olsen J, Gronbaek M (2004) Alcohol consumption during pregnancy and the risk of preterm delivery. Am J Epidemiol 159(2):155–161. doi:10.1093/aje/kwh034
Anderson HR, Bremner SA, Atkinson RW, Harrison RM, Walters S (2001) Particulate matter and daily mortality and hospital admissions in the west midlands conurbation of the United Kingdom: associations with fine and coarse particles, black smoke and sulphate. Occup Environ Med 58(8):504–510. doi:10.1136/oem.58.8.504
Bobak M (2000) Outdoor air pollution, low birth weight, and prematurity. Environ Health Perspect 108(2):173–176. doi:10.2307/3454517
Bobak M, Leon DA (1999) Pregnancy outcomes and outdoor air pollution: an ecological study in districts of the Czech Republic 1986–8. Occup Environ Med 56:539–543
Cnattingius S, Akre O, Lambe M, Ockene J, Granath F (2006) Will an adverse pregnancy outcome influence the risk of continued smoking in the next pregnancy? Am J Obstet Gynecol 195(6):1680–1686. doi:10.1016/j.ajog.2006.06.071
Dejmek J, Selevan SG, Benes I, Slansky I, Sram RJ (1999) Fetal growth and maternal exposure to particulate matter during pregnancy. Environ Health Perspect 107:475–480. doi:10.2307/3434630
Ha E, Cho SI, Chen D, Chen C, Ryan L, Smith TJ, Xu X, Christiani DC (2002) Parental exposure to organic solvents and reduced birth weight. Arch Environ Health 57(3):207–214
Ha EH, Hong YC, Lee BE, Woo BH, Schwartz J, Christiani DC (2001) Is air pollution a risk factor for low birth weight in Seoul? Epidemiology 12:643–648. doi:10.1097/00001648-200111000-00011
Ha EH, Lee BE, Park HS, Kim YS, Kim H, Kim YJ, Hong YC, Park EA (2004) Prenatal exposure to PM10 and preterm birth between 1998 and 2000 in Seoul, Korea. J Prev Med Pub Health 37(4):300–305
Ha EH, Lee JT, Kim H, Hong YC, Lee BE, Park HS, Christiani DC (2003) Infant susceptibility of mortality to air pollution in Seoul, South Korea. Pediatrics 111(2):284–290. doi:10.1542/peds.111.2.284
Hansen C, Neller A, Williams G, Simpson R (2006) Maternal exposure to low levels of ambient air pollution and preterm birth in Brisbane, Australia. BJOG 113(8):935–941. doi:10.1111/j.1471-0528.2006.01010.x
Hansen C, Neller A, Williams G, Simpson R (2007) Low levels of ambient air pollution during pregnancy and fetal growth among term neonates in Brisbane, Australia. Environ Res 103(3):383–389. doi:10.1016/j.envres.2006.06.010
Horta BL, Victora CG, Menezes AM, Halpern R, Barros FC (1997) Low birthweight, preterm births and intrauterine growth retardation in relation to maternal smoking. Paediatr Perinat Epidemiol 11(2):140–151. doi:10.1046/j.1365-3016.1997.d01-17.x
Joseph KS, Kramer MS (1996) Review of the evidence on fetal and early childhood antecedents of adult chronic disease. Epidemiol Rev 18(2):158–174
Kharrazi M, DeLorenze GN, Kaufman FL, Eskenazi B, Bernert JT Jr, Graham S, Pearl M, Pirkle J (2004) Environmental tobacco smoke and pregnancy outcome. Epidemiology 15(6):660–670. doi:10.1097/01.ede.0000142137.39619.60
Kleinbaum DG, Klein M (2005) Survival analysis: a self-learning text, 2nd edn. Springer
Leem JH, Kaplan BM, Shim YK, Pohl HR, Gotway CA, Bullard SM, Rogers JF, Smith MM, Tylenda CA (2006) Exposures to air pollutants during pregnancy and preterm delivery. Environ Health Perspect 114(6):905–910
Liu S, Krewski D, Shi Y, Chen Y, Burnett RT (2003) Association between gaseous ambient air pollutants and adverse pregnancy outcomes in Vancouver, Canada. Environ Health Perspect 111(14):1773–1778
Maisonet M, Bush TJ, Correa A, Jaakkola JJ (2001) Relation between ambient air pollution and low birth weight in the Northeastern United States. Environ Health Perspect 109(Suppl 3):351–356. doi:10.2307/3434782
Maroziene L, Grazuleviciene R (2002) Maternal exposure to low-level air pollution and pregnancy outcomes: a population-based study. Environ Health 1(1):6. doi:10.1186/1476-069X-1-6
Medeiros A, Gouveia N (2005) Relationship between low birth weight and air pollution in the city of Sao Paulo, Brazil. Rev Saude Publica 39:965–972
O’Neill MS, Hertz-Picciotto I, Pastore LM, Weatherley BD (2003) Have studies of urinary tract infection and preterm delivery used the most appropriate methods? Paediatr Perinat Epidemiol 17(3):226–233. doi:10.1046/j.1365-3016.2003.00499.x
Peng RD, Dominici F, Pastor-Barriuso R, Zeger SL, Samet JM (2005) Seasonal analyses of air pollution and mortality in 100 US cities. Am J Epidemiol 161(6):585–594. doi:10.1093/aje/kwi075
Platt RW, Joseph KS, Ananth CV, Grondines J, Abrahamowicz M, Kramer MS (2004) A proportional hazards model with time-dependent covariates and time-varying effects for analysis of fetal and infant death. Am J Epidemiol 160(3):199–206. doi:10.1093/aje/kwh201
Raatikainen K, Huurinainen P, Heinonen S (2007) Smoking in early gestation or through pregnancy: A decision crucial to pregnancy outcome. Prev Med 44(1):59–63. doi:10.1016/j.ypmed.2006.07.017
Ritz B, Yu F (1999) The effect of ambient carbon monoxide on low birth weight among children born in southern California between 1989 and 1993. Environ Health Perspect 107(1):17–25. doi:10.2307/3434285
Ritz B, Yu F, Chapa G, Fruin S (2000) Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology 11(5):502–511. doi:10.1097/00001648-200009000-00004
Roberts S (2004) Interactions between particulate air pollution and temperature in air pollution mortality time series studies. Environ Res 96(3):328–337. doi:10.1016/j.envres.2004.01.015
Roberts S (2005) An investigation of distributed lag models in the context of air pollution and mortality time series analysis. J Air Waste Manag Assoc 55(3):273–282
Rogers JF, Dunlop AL (2006) Air pollution and very low birth weight neonates: a target population? Pediatrics 118(1):156–164. doi:10.1542/peds.2005-2432
Sagiv SK, Mendola P, Loomis D, Herring AH, Neas LM, Savitz DA, Poole C (2005) A time-series analysis of air pollution and preterm birth in Pennsylvania, 1997–2001. Environ Health Perspect 113(5):602–606
Salam MT, Millstein J, Li YF, Lurmann FW, Margolis HG, Gilliland FD (2005) Birth outcomes and prenatal exposure to ozone, carbon monoxide, and particulate matter: results from the Children’s Health Study. Environ Health Perspect 113(11):1638–1644
Tsai SS, Yu HS, Liu CC, Yang CY (2003) Increased incidence of preterm delivery in mothers residing in an industrialized area in Taiwan. J Toxicol Environ Health A 66(11):987–994. doi:10.1080/15287390306396
Wang X, Chen D, Niu T, Wang Z, Wang L, Ryan L, Smith T, Christiani DC, Zuckerman B, Xu X (2000) Genetic susceptibility to benzene and shortened gestation: evidence of gene-environment interaction. Am J Epidemiol 152(8):693–700. doi:10.1093/aje/152.8.693
Wang X, Ding H, Ryan L, Xu X (1997) Association between air pollution and low birth weight: a community-based study. Environ Health Perspect 105:514–520. doi:10.2307/3433580
Wilhelm M, Ritz B (2005) Local variations in CO and particulate air pollution and adverse birth outcomes in Los Angeles County, California, USA. Environ Health Perspect 113(9):1212–1221
Windham GC, Hopkins B, Fenster L, Swan SH (2000) Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology 11(4):427–433. doi:10.1097/00001648-200007000-00011
Woodruff TJ, Parker JD, Kyle AD, Schoendorf KC (2003) Disparities in exposure to air pollution during pregnancy. Environ Health Perspect 111(7):942–946
Xu X, Ding H, Wang X (1995) Acute effects of total suspended particles and sulfur dioxides on preterm delivery: a community-based cohort study. Arch Environ Health 50(6):407–415
Yang CY, Chang CC, Tsai SS, Chuang HY, Ho CK, Wu TN, Sung FC (2003) Preterm delivery among people living around Portland cement plants. Environ Res 92(1):64–68. doi:10.1016/S0013-9351(02)00055-5
Yang CY, Chiu HF, Tsai SS, Chang CC, Chuang HY (2002) Increased risk of preterm delivery in areas with cancer mortality problems from petrochemical complexes. Environ Res 89(3):195–200. doi:10.1006/enrs.2002.4374
Acknowledgments
This study was supported by a Seoul Research & Business Development grant (#2005-1547-1), Republic of Korea.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Suh, Y.J., Kim, H., Seo, J.H. et al. Different effects of PM10 exposure on preterm birth by gestational period estimated from time-dependent survival analyses. Int Arch Occup Environ Health 82, 613–621 (2009). https://doi.org/10.1007/s00420-008-0380-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-008-0380-7