Abstract
Objectives: Idiopathic orthostatic intolerance (IOI) is a common disorder that is characterized by chronic orthostatic symptoms and substantial increases in heart rate and plasma norepinephrine concentrations that are disproportionately high while standing. Several features of the syndrome, including the tachycardia, tremulousness, and exaggerated norepinephrine have been considered potentially due to hypoactive or hyperactive states of adrenergic receptors of the sympathetic nervous system. The aim of this study was therefore to ascertain whether genotypes at eight polymorphic loci within five relevant adrenergic receptor genes (α2A, α2B, α2C, β1 and β2) influence the risk for IOI. Methods: We studied 80 young men in military service (20 patients with IOI and 60 age-matched controls). All participants underwent a tilt table test including monitoring of blood pressure, heart rate and plasma catecholamines, in the supine position and during 30 min of standing. Genotyping at the eight loci (α2ALys251, α2BDel301-303, α2CDel322-325, β1Gly49, β1Arg389, β2Arg16, β2Glu27, β2Ile164) was performed in all participants. Chi-square tests of independence were used to test for associations between IOI and genotype. In addition, an association of the polymorphisms with haemodynamic variables (heart rate, supine and upright blood pressure) was ascertained using one-way variance analysis. Results: For the β1Gly49 polymorphism we found a decrease in the risk of IOI among persons who were homozygous (odds ratio, 0.88; 95% confidence interval, 0.81–0.97). In addition, we found an association between β1Gly49 and decreased heart rate in the upright position, regardless of IOI diagnosis. There were no associations with the other studied polymorphisms and IOI. Conclusions: Our current results suggest that the β1Gly49 polymorphism is protective for IOI. This is likely one of several common genetic loci that may represent modifiers of IOI phenotypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic orthostatic intolerance (IOI), also termed postural tachycardia syndrome, is characterized by an array of symptoms which occur upon assuming the upright position, with tachycardia and an exaggerated plasma norepinephrine response (Jacob and Biaggioni 1999). IOI is of great relevance for occupational medicine, because the secondary problems cause a wide range of personal, social and occupational difficulties. Firstly, severe IOI implies a substantial impairment of well-being and work performance (Grubb B et al. 2003; Winker et al. 2003). Secondly, it represents a major safety risk for particular professions (i.e. construction workers, roofers, and all employees who operate dangerous machines) (Winker and Rüdiger 2001). Unlike other syndromes with some similar characteristics, such as neurogenic orthostatic hypotension, the basis for IOI remains obscure (Jacob and Biaggioni 1999; Jordan et al. 1999). Several features of the syndrome, including the tachycardia, palpitations and tremulousness, have been considered potentially due to β-adrenergic receptor supersensitivity or other hypo/hyperactive states of autonomic receptors (Farquhar et al. 2000; Jacob and Biaggioni 1999; Jordan et al. 2002). The sympathetic nervous system is highly integrated, with nine different receptors for epinephrine and norepinephrine. Six adrenergic receptors (ARs) are known to have polymorphic variations in their coding regions that result in altered function or regulation (Green et al. 1993, 1994; Mason et al. 1999; Rathz et al. 2002; Small et al. 2001, 2000a, 2000b). Relevant to potential causes of IOI are the Ser/Gly49 and Gly/Arg389 forms of the β1AR; the Arg/Gly16, Gln/Glu27, and Thr/Ile164 forms of the β2AR; the Asn/Lys251 forms of the α2AAR; the “wild-type” and Del301-303 forms of the α2BAR; and the “wild-type” and Del322-325 forms of the α2CAR. Many of these polymorphisms are common in the population, and we have considered that one (or potentially a combination of several) may be associated with, are protective against, or modify IOI. To investigate this issue, two cohorts of young men with or without IOI were identified among military personnel, and genotypes at eight polymorphic loci within the five relevant adrenergic receptor genes were ascertained.
Materials and methods
Study population
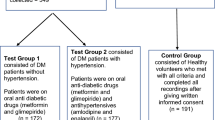
Controls (n=60) and patients with IOI (n=20) were recruited from the Austrian Army between January 2003 and December 2003. All 80 subjects were male Caucasians. The participants did not exhibit signs or symptoms of systemic illness and did not take medications, including nonprescription antihistamines or decongestants. All participants had had a traditional medical evaluation when entering the army several months prior to study. Those with a history of metabolic or neurologic diseases that might affect the autonomic nervous system were excluded. Supine blood pressures less than 90/50 or greater than 140/90, neurogenic orthostatic hypotension, mitral valve prolapse and deconditioning were considered exclusion criteria.
All participants underwent a standardised tilt table test. A digital plethysmograph (Task Force Monitor; CNSystems, Graz, Austria) was installed around the second phalanx of the middle finger of the right hand for the continuous noninvasive measurement of arterial blood pressure. The right arm was positioned at heart level. In addition to this beat-by-beat recording, blood pressure and heart rate were measured every 2 min at the left arm. The finger blood pressure signal was calibrated to the oscillometric blood pressure measurement as described (Gratze et al. 1998). Participants were supported by belts at the hips and by a footrest. Subjects equilibrated in the supine position for 30 min and then were subjected to a 75° upright tilt for 30 min. Plasma catecholamines were determined immediately at the conclusion of the supine and upright phases.
Patients were designated as having IOI if they met the following criteria:
-
1.
The occurrence of characteristic orthostatic symptoms for at least 6 months. These included at least three of the following: dizziness, headache, chest discomfort, tremulousness, palpitations, nausea or hyperhydrosis.
-
2.
Orthostatic tachycardia within 5 min after assuming an upright position (heart rate increase ≥30 beats per min without a decrease of ≥20 mmHg in systolic or ≥10 mmHg in diastolic blood pressure).
-
3.
Plasma norepinephrine concentrations >600 pg/ml while standing upright.
Each IOI subject was matched to three controls of similar age (thus a total of 60 controls). The protocol was approved by the ethics committee of the medical faculty of the University of Vienna and the University of Cincinnati College of Medicine, and all participants gave written informed consent before entering the study.
Plasma catecholamines determination
Plasma catecholamine levels were determined by high-performance liquid chromatography (HPLC) (Chromsystems; Munich, Germany) as previously described (Tschernko et al. 1996). Briefly, plasma was collected and frozen to −70°. Samples were mixed with dihydroxybenzylamine for recovery estimations and were afterward extracted with A1203. Eluted catecholamines were automatically injected and separated on a C18 silica column by HPLC. Catecholamines were measured by an electrochemical detector (Pharmacia, Sweden).
Genotyping
Genotyping was performed at the University of Cincinnati by S. Liggett. Genomic DNA was isolated from samples of peripheral blood, and the adrenergic receptor polymorphisms were determined exactly as previously described (Small et al. 2002a).
Statistical analysis
Data were analyzed with the Statistical Package for Social Sciences (SPSS, Chicago, IL, USA). The results are expressed as mean ± SD. Two-tailed t tests and Mann–Whitney tests were used for comparison between groups concerning the following variables: age, weight, height, heart rate, blood pressure and plasma norepinephrine concentration. Haemodynamic variables were compared in one-way analysis of variance with genotype as factor. All group differences were evaluated in post hoc analysis with the Scheffe test. Odds ratios as a measure of relative risk for IOI and 95% confidence intervals (95% CI) were calculated by standard methods. Chi-square tests were used to test for associations between IOI and genotype or allele. Differences were considered statistically significant at P<0.05.
Results
Characteristics of the subjects
The characteristics of the patients with IOI and the controls are shown in Table 1. The mean age of the patients with IOI was 19.8 ± 2.4 years, and 20.4 ± 2.6 years for the controls. There were no differences in weight, size or age. Heart rate and blood pressure in the supine position were similar in both groups. Based on the predefined criteria, the IOI subjects had ~30 bpm higher heart rates, and upright norepinephrine levels approximately twofold greater, compared with the normal subjects. In addition, we noted that the IOI subjects had diastolic blood pressures in the supine position that were slightly higher than controls, as well as higher supine norepinephrine levels.
Potential relationships between adrenergic receptor polymorphisms and IOI
The distribution of genotypes of the adrenergic receptor polymorphisms is shown in Table 2. A polymorphism of the β1AR (Gly49) was significantly less common in IOI (allele frequency of β1Gly49 was 0.26 in controls and 0.10 in patients with IOI; P=0.04). The odds ratio based on the allele frequencies for the Gly49 allele was 0.319 (95% CI, 0.105–0.969). The odds ratio for IOI based on the Gly49 genotype distribution determined by two-by-three chi-square test was 0.88 (95% CI, 0.81–0.97, P=0.16). There were no homozygous Gly49 IOI subjects, so an analysis using the two homozygous and the heterozygous genotypes could not be considered. There was no association (Table 2) with the other functional β1AR polymorphism at position 389 and IOI. β2AR polymorphisms have also been shown to affect cardiac and vascular function (Brodde et al. 2001; Dishy et al. 2001; Hoit B et al. 2000), but in our study there was no difference in the frequencies of the two major β2AR polymorphisms between IOI and controls.
The α2AAR and α2CAR control presynaptic norepinephrine release; however, coding polymorphisms of these receptors’ genes are uncommon in Caucasians (Table 2; Small and Liggett 2001; Small et al. 2003). For the α2AAR, the Lys251 allele was not found in any of the 80 individuals. The α2CDel322-325 was uncommon in both groups, and there was no statistical difference between allele frequencies between IOI patients (0.025) and controls (0.075, P=0.26). The α2BDel301-303 polymorphism is common in Caucasians (Small et al. 2001), and has been associated with vascular responsiveness to catecholamines (Heinonen et al. 2002). However, we found no difference in allele frequency between our IOI and control subjects (0.28 in both groups).
Potential relationships between adrenergic receptor polymorphisms and phenotypic variables
The IOI cohort was defined by symptoms, blood pressure, and norepinephrine criteria. We considered that, while for some polymorphisms there were no associations with IOI as so defined, there may be associations with one physiologic aspect of the syndrome. To approach this possibility, potential relationships between blood pressure, heart rate, and norepinephrine levels, without regard to diagnosis of IOI, were explored.
In this model, we again found a relationship between heart rate and the position 49 polymorphism of the β1AR. Gly49 homozygotes (only found in controls) had upright heart rates of 69 ± 11 bpm, compared with 86 ± 17 bpm for Ser49 homozygotes, and an intermediate rate for heterozygotes of 82 ± 17 bpm (P=0.04 by ANOVA). In the group of IOI subjects, no relationship was found between heart rate and the β149 polymorphism. Also no association was found between the other β1AR polymorphic locus, at position 389, and baseline haemodynamic variables (Table 3). The two common β2AR polymorphisms studied showed no relationship between blood pressure and heart rate as well. Concerning the α2AR polymorphisms, the low frequency of the α2CDel322-325 allele limited analysis, but no trends were noted in heart rate or blood pressure parameters and presence of the allele. The common α2BAR polymorphism did not show any trend in association of heart rate or blood pressure parameters.
None of the receptor variants were associated with supine, upright, or the change in plasma norepinephrine. As noted earlier, the genes for the two receptors (α2AAR and α2CAR) that control presynaptic release of norepinephrine had either no or rare variability at the loci examined in these Caucasian cohorts.
Discussion
Genetic variability within the coding regions of ARs in the human population was first demonstrated in 1992 with the β2AR (Heinonen et al. 2002). Subsequently, nonsynonymous coding polymorphisms of the α1A, α2A, α2B, α2C, β1 and β3ARs have been identified (Small et al. 2003). (To date, the α1B and α1D coding regions have not been closely examined for variation.) Using heterologous expression systems in cells (Green et al. 1993, 1994; Mason et al. 1999; Rathz et al. 2002; Small et al. 2001, 2000a, 2000b) or mice (Mialet Perez et al. 2003; Turki et al. 1996), the relevance of these variants has been ascertained within the constraints imposed by such models. The α1A polymorphism was found to have no functional effect in recombinantly expressed CHO cells (Shibata et al. 1996). However, each of the other nonsynonymous polymorphisms of the α2A, α2B, α2C, β1, β2 and β3ARs have been reported to have a signaling phenotype (reviewed in Small and Liggett [2001]; Small et al. [2003]). These include alterations in expression, ligand binding affinities, functional coupling to G proteins, and regulation.
In case control as well as a limited number of family studies, the nonsynonymous coding polymorphisms of the α2B, α2C, β1 and β2ARs have been associated with a number of cardiovascular phenotypes (Small et al. 2003). These include associations for risk such as hypertension (Bray et al. 2000) and heart failure (Small et al. 2002b). In addition, certain of these polymorphisms have been associated with disease modification or disease subsets, such as survival (Liggett et al. 1998) and exercise tolerance in heart failure (Wagoner et al. 2000, 2002), and the response to β-blockers (Johnson et al. 2003). Other studies have revealed effects of certain adrenergic receptor polymorphisms on cardiac or vascular function in response to agonists or sympathetic nervous system activation in normal individuals (Brodde et al. 2001; Dishy et al. 2001). Results from these in vitro and human studies prompted us to examine the potential for associations of the functional coding polymorphisms of ARs and IOI. The features of IOI, either in terms of clinical symptoms and signs, or the physiologic findings that define the syndrome, are highly suggestive of altered cardiac, vascular, or norepinephrine kinetic responses in response to orthostatic challenge. Indeed, in recent studies of the rare entity familial orthostatic intolerance, a mutation of the coding region of the norepinephrine transporter gene (which is not polymorphic) has been identified as causative (Shannon et al. 2000).
We found that the bradycardia-promoting β1Gly49 polymorphism was underrepresented in the IOI group. See Fig. 1 for the basis of our hypothesis that the β1Gly49 variant may decrease the risk for IOI. In transfected cells, Gly49 β1AR undergoes enhanced agonist-promoted down-regulation (Rathz et al. 2002) and thus in the heart would represent a genotype less prone to tachycardia. This is consistent with the current findings. The Gly49 receptor has an atypical glycosylation pattern, which appears to be related to an enhanced steady-state degradation of internalized receptors. The Gly49 receptor has previously been reported to be associated with an improved outcome in heart failure (January et al. 1998) and resting heart rate (Ranade et al. 2002). The Gly49 allele frequencies were found to differ significantly between controls and patients (see Table 2). The observed allele frequency for controls was found to be in good accordance with a recently reported allele frequency for Caucasians (Small et al. 2002a). In summary, we have shown a significant association between Gly49 genotype and heart rate, as well as a significantly different allele frequency between IOI subjects and controls. Comparison of genotype distributions between controls and patients did not differ significantly. Nevertheless a trend supporting our hypothesis, that the β1Gly49 might be protective for IOI, was observed (none of the patients was homozygous for glycine, compared with 11.7% of the controls). To confirm these findings, further studies should include a larger number of patients.
Basis of the hypothesis that the α2CDel322-325 and the β1Arg389 variants may increase and the β1Gly49 variant may decrease the risk for idiopathic orthostatic intolerance. Under normal conditions, norepinephrine is released from vesicles in the neuron into the synaptic space, where it can interact with presynaptic and postsynaptic α- and β-adrenergic receptors. β1-Adrenergic receptors couple to the stimulatory G protein Gs, activating adenylyl cyclase and increasing intracellular cyclic AMP (cAMP). Eighty percent of the norepinephrine in the synaptic space is taken up by the norepinephrine transporter into the neuron, which releases it, and approximately 20% spills over into circulation. Norepinephrine is then converted to dihydroxyphenylglycol (DHPG) by monoamine oxidase. The α2-adrenergic receptor inhibits norepinephrine release at presynaptic nerve endings through negative feedback. The presence of the dysfunctionally running α2CDel322-325 receptor would therefore be expected to result in an in vivo increased norepinephrine release at the synapse. The hyperfunctional β1Arg389 receptor would be expected to increase chronotropy at the myocyte. Therefore, the presence of these two receptor polymorphisms were hypothesised to be risk factors for IOI. The β149Gly receptor variant, which should lead to decreased function via down-regulation was hypothesised to be a protecting factor for IOI.
Our current results now indicate that the underrepresentation of Gly49 (or increased frequency of Ser49) represents one of likely several genetic, and gene–environment interactions, associated with IOI. While it is attractive to consider that this polymorphism in combination with another adrenergic receptor polymorphism might contribute an additive effect, we found no evidence for interactions between any of the common adrenergic receptor polymorphisms and IOI risk. However, the low allele frequencies of β2Ile164, α2ALys251 and α2CDel322-325 have limited our ability to ascertain effects due to sample size. It should also be noted that promoter, 5′ UTR, or 3′ UTR polymorphisms of ARs may influence receptor expression (Drysdale et al. 2000), and these polymorphisms may not be in linkage disequilibrium with the coding polymorphismic sites examined in the current study (Drysdale et al. 2000). Thus, we cannot exclude some non-coding polymorphisms/haplotypes of ARs as contributing to IOI pathophysiology. Studies to address this will require identification and characterisation of these non-coding polymorphisms for each adrenergic receptor gene. We note that the odds ratio for protection against IOI is modest (0.88), and we are underpowered to address certain adrenergic receptor polymorphisms due to their low frequency. Further, as noted, non-coding polymorphisms were not considered. So, we cannot unequivocally exclude an adrenergic receptor polymorphism “load-score” (comprising multiple polymorphisms of multiple receptors) that associates with IOI. Such a study will require larger cohorts and genotyping of additional polymorphisms within all the genes. And finally, our study was restricted to males, but the syndrome is more common in females. Although a difference in allele frequencies has never been found by the Department of Molecular Genetics, University of Cincinnati (S. Liggett, personal communication), a sex–genotype–disease interaction cannot be excluded for IOI.
References
Bray MS, Krushkal J, Li L, Ferrell R, Kardia S, Sing CF, Turner ST, Boerwinkle E (2000) Positional genomic analysis identifies the beta(2)-adrenergic receptor gene as a susceptibility locus for human hypertension. Circulation 101:2877–2882
Brodde O E, Buscher R, Tellkamp R, Radke J, Dhein S, Insel P A (2001) Blunted cardiac responses to receptor activation in subjects with Thr164Ile beta(2)-adrenoceptors. Circulation 103:1048–1050
Dishy V, Sofowora GG, Xie HG, Kim RB, Byrne DW, Stein CM, Wood AJ (2001) The effect of common polymorphisms of the beta2-adrenergic receptor on agonist-mediated vascular desensitization. N Engl J Med 345:1030–1035
Drysdale CM, McGraw DW, Stack CB, Stephens JC, Judson RS, Nandabalan K, Arnold K, Ruano G, Liggett SB (2000) Complex promoter and coding region beta 2-adrenergic receptor haplotypes alter receptor expression and predict in vivo responsiveness. Proc Natl Acad Sci U S A 97:10483–10488
Farquhar W B, Taylor J A, Darling S E, Chase K P, Freeman R (2000) Abnormal baroreflex responses in patients with idiopathic orthostatic intolerance. Circulation 102:3086–3091
Gratze G, Fortin J, Holler A, Grasenick K, Pfurtscheller G, Wach P, Schonegger J, Kotanko P, Skrabal F (1998) A software package for non-invasive, real-time beat-to-beat monitoring of stroke volume, blood pressure, total peripheral resistance and for assessment of autonomic function. Comput Biol Med 28:121–142
Green SA, Cole G, Jacinto M, Innis M, Liggett SB (1993) A polymorphism of the human beta 2-adrenergic receptor within the fourth transmembrane domain alters ligand binding and functional properties of the receptor. J Biol Chem 268:23116–23121
Green SA, Turki J, Innis M, Liggett SB (1994) Amino-terminal polymorphisms of the human beta 2-adrenergic receptor impart distinct agonist-promoted regulatory properties. Biochemistry 33:9414–9419
Grubb BP, Kosinski DJ, Kanjwal Y (2003) Orthostatic hypotension: causes, classification, and treatment. Pacing Clin Electrophysiol 26:892–901
Heinonen P, Jartti L, Jarvisalo MJ, Pesonen U, Kaprio JA, Ronnemaa T, Raitakari OT, Scheinin M (2002) Deletion polymorphism in the alpha2B-adrenergic receptor gene is associated with flow-mediated dilatation of the brachial artery. Clin Sci Lond 103:517–524
Hoit BD, Suresh DP, Craft L, Walsh RA, Liggett SB (2000) Beta2-adrenergic receptor polymorphisms at amino acid 16 differentially influence agonist-stimulated blood pressure and peripheral blood flow in normal individuals. Am Heart J 139:537–542
Jacob G, Biaggioni I (1999) Idiopathic orthostatic intolerance and postural tachycardia syndromes. Am J Med Sci 317:88–101
January B, Seibold A, Allal C, Whaley BS, Knoll BJ, Moore RH, Dickey BF, Barber R, Clark RB (1998) Salmeterol-induced desensitization, internalization and phosphorylation of the human beta2-adrenoceptor. Br J Pharmacol 123:701–711
Johnson JA, Zineh I, Puckett BJ, McGorray SP, Yarandi HN, Pauly DF (2003) Beta 1-adrenergic receptor polymorphisms and antihypertensive response to metoprolol. Clin Pharmacol Ther 74:44–52
Jordan J, Shannon JR, Jacob G, Pohar B, Robertson D (1999) Interaction of genetic predisposition and environmental factors in the pathogenesis of idiopathic orthostatic intolerance. Am J Med Sci 318:298–303
Jordan J, Shannon JR, Diedrich A, Black BK, Robertson D (2002) Increased sympathetic activation in idiopathic orthostatic intolerance: role of systemic adrenoreceptor sensitivity. Hypertension 39:173–178
Liggett S B, Wagoner LE, Craft LL, Hornung RW, Hoit BD, McIntosh TC, Walsh RA (1998) The Ile164 beta2-adrenergic receptor polymorphism adversely affects the outcome of congestive heart failure. J Clin Invest 102:1534–1539
Mason DA, Moore JD, Green SA, Liggett SB (1999) A gain-of-function polymorphism in a G-protein coupling domain of the human beta1-adrenergic receptor. J Biol Chem 274:12670–12674
Mialet Perez J, Rathz DA, Petrashevskaya NN, Hahn HS, Wagoner LE, Schwartz A, Dorn GW, Liggett SB (2003) Beta 1-adrenergic receptor polymorphisms confer differential function and predisposition to heart failure. Nat Med 9:1300–1305
Ranade K, Jorgenson E, Sheu WH, Pei D, Hsiung CA, Chiang FT, Chen YD, Pratt R, Olshen RA, Curb D, Cox DR, Botstein D, Risch N (2002) A polymorphism in the beta1 adrenergic receptor is associated with resting heart rate. Am J Hum Genet 70:935–942
Rathz DA, Brown KM, Kramer LA, Liggett SB (2002) Amino acid 49 polymorphisms of the human beta1-adrenergic receptor affect agonist-promoted trafficking. J Cardiovasc Pharmacol 39:155–160
Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D (2000) Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N Engl J Med 342:541–549
Shibata K, Hirasawa A, Moriyama N, Kawabe K, Ogawa S, Tsujimoto G (1996) Alpha 1a-adrenoceptor polymorphism: pharmacological characterization and association with benign prostatic hypertrophy. Br J Pharmacol 118:1403–1408
Small KM, Liggett SB (2001) Identification and functional characterization of alpha(2)-adrenoceptor polymorphisms. Trends Pharmacol Sci 22:471–477
Small KM, Forbes SL, Brown KM, Liggett SB (2000a) An asn to lys polymorphism in the third intracellular loop of the human alpha 2A-adrenergic receptor imparts enhanced agonist-promoted Gi coupling. J Biol Chem 275:38518–38523
Small KM, Forbes SL, Rahman FF, Bridges KM, Liggett SB (2000b) A four amino acid deletion polymorphism in the third intracellular loop of the human alpha 2C-adrenergic receptor confers impaired coupling to multiple effectors. J Biol Chem 275:23059–23064
Small KM, Brown KM, Forbes SL, Liggett SB (2001) Polymorphic deletion of three intracellular acidic residues of the alpha 2B-adrenergic receptor decreases G protein-coupled receptor kinase-mediated phosphorylation and desensitization. J Biol Chem 276:4917–4922
Small KM, Rathz DA, Liggett SB (2002a) Identification of adrenergic receptor polymorphisms. Methods Enzymol 343:459–475
Small KM, Wagoner LE, Levin AM, Kardia SL, Liggett SB (2002b) Synergistic polymorphisms of beta1- and alpha2C-adrenergic receptors and the risk of congestive heart failure. N Engl J Med 347:1135–1142
Small KM, McGraw DW, Liggett SB (2003) Pharmacology and physiology of human adrenergic receptor polymorphisms. Annu Rev Pharmacol Toxicol 43:381–411
Tschernko EM, Hofer S, Bieglmayer C, Wisser W, Haider W (1996) Early postoperative stress: video-assisted wedge resection/lobectomy vs conventional axillary thoracotomy. Chest 109:1636–1642
Turki J, Lorenz JN, Green SA, Donnelly ET, Jacinto M, Liggett SB (1996) Myocardial signaling defects and impaired cardiac function of a human beta 2-adrenergic receptor polymorphism expressed in transgenic mice. Proc Natl Acad Sci U S A 93:10483–10488
Wagoner LE, Craft LL, Singh B, Suresh DP, Zengel PW, McGuire N, Abraham WT, Chenier TC, Dorn GW II, Liggett SB (2000) Polymorphisms of the beta(2)-adrenergic receptor determine exercise capacity in patients with heart failure. Circ Res 86:834–840
Wagoner LE, Craft LL, Zengel P, McGuire N, Rathz DA, Dorn GW II, Liggett SB (2002) Polymorphisms of the beta1-adrenergic receptor predict exercise capacity in heart failure. Am Heart J 144:840–846
Winker R, Rüdiger H (2001) Orthostatische Intoleranz - Bedeutung in der Arbeitsmedizin. ASU 36:325–331
Winker R, Barth A, Dorner W, Mayr O, Pilger A, Ivancsits S, Ponocny I, Heider A, Wolf C, Rudiger HW (2003) Diagnostic management of orthostatic intolerance in the workplace. Int Arch Occup Environ Health 76:143–150
Acknowledgements
We are indebted to Dr Stephen B. Liggett (genotyping) and to Mr Guy Knibbeler (graphical assistance) for their contributions to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Winker, R., Barth, A., Valic, E. et al. Functional adrenergic receptor polymorphisms and idiopathic orthostatic intolerance. Int Arch Occup Environ Health 78, 171–177 (2005). https://doi.org/10.1007/s00420-005-0605-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-005-0605-y