Abstract
Background
Workers compensated for silicosis outside the mining industry are at an increased risk of developing lung cancer. In the meta-analyses no data from Germany are involved. Furthermore, exposure data are necessary if a threshold value is to be assessed in order to reduce the risk for silicosis and also for lung cancer.
Method
A cohort study among workers compensated for silicosis between 1988 and 2000 from the stone and quarry industry in Germany has been initiated. The cohort was followed up until the end of 2001. From all workers a detailed description of their jobs was assessed.
Results
Four hundred and forty workers were enrolled in the study. During the follow-up 144 workers died, compared with 74.35 expected cases based on the mortality rates of the general population from Germany, leading to a standard mortality ratio (SMR) of 1.94 (95% CI 1.63–2.28). Lung cancer was the cause of death in 16 cases (SMR 2.40; 95% CI 1.37–3.90). All workers had a peak exposure above 0.15 mg/m3, the current threshold value. The cumulative exposure was above 2 mg/m3·years and the average exposure was 0.10 mg/m3 or larger. No association between the exposure and the risk of developing lung cancer could be observed.
Conclusions
Workers from the stone and quarry industry compensated for silicosis are at an increased risk of developing lung cancer. In order to reduce that risk, the exposure has to be lowered, with a peak exposure below 0.15 mg/m3 and an average exposure below 0.10 mg/m3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The relationship between crystalline silica and silicosis, a non-malignant fibrosis of the lung, has been known for decades. For example, silicosis has been on the list of occupational diseases for which compensation is paid in Germany since 1929. The clinical toxicity of crystalline silica and the pathogenesis of silicosis have been summarized in detail [1]. In 1996 a working group of the International Agency for Research on Cancer (IARC) classified silica into group 1, carcinogenic to humans [2]. In the following years other agencies also made an assessment of that compound. The American Conference of Governmental Industrial Hygienists (ACGIH) classified quartz into group A2 (suspected human carcinogen) [3]. The German MAK-Kommission [4] came to the same decision as IARC. The lung cancer risk is present mainly among compensated silicotic workers, with the exception of coalminers [5, 6]. Among the silicotics the lung cancer risk is approximately 2–2.5 times higher than in the general population.
Cohort studies among exposed workers (with and without silicosis) also show an increased lung cancer risk, albeit at a lower level. The relative risk is in the range of 1.3 [2]. Some studies have investigated the lung cancer risk among non-silicotic miners [7, 8, 9]. No increased lung cancer risk after adjustment for smoking could be found. However, these studies were not large enough to exclude any risk. Some studies showed a dose–response relationship between silica dust and lung cancer risk [10, 11]. Workers with silicosis are exposed at higher levels. There is a clear dose–response relationship between the exposure to crystalline silica and the risk of developing silicosis; therefore, it is not surprising to observe an increasing risk of lung cancer with increasing exposure. It is still questionable whether silicosis is required for the development of lung cancer [12].
The discussion now is focused mainly on two questions: firstly, is it possible for workers to be identified that are at high risk of developing lung cancer and, secondly, can a “safe” level of exposure be assessed [12, 13, 14].
In order for both questions to be addressed (lung cancer risk and level of exposure) a cohort study of workers compensated for silicosis from the stone and quarry industry in Germany was performed.
Methods
Design of the study
All workers from the stone and quarry industry in Germany, compensated for silicosis between 1 January 1988 and 31 December 2000 were enrolled in this cohort-study. They worked mainly as stonemasons or stone sculptors in the crushing or cutting of stones, as well as processing sand and gravel. The workers were followed up from the time of compensation until the end of 2001. Silicosis is defined as an X-ray classified as ≥1/1 by ILO 1980. In order for workers to receive compensation, additionally, reduced lung function has to be present, which must exceed a reduction in working capacity of at least 20%. The death of a compensated worker is known to the industrial insurance institutes, for it causes a change in compensation funds. The cause of death has been ascertained by death certificates. The mortality rates have been compared with those from the general population of Germany.
Recording of exposure
The complete occupational history of all workers was ascertained. For workers who received compensation between 1988 and 1992 (the first phase of this study), for all periods with possible exposure to silica dust, the relevant information for assessing the level of exposure was considered by industrial hygienists. For each interval with a difference in the exposure caused by change in type of occupation, plant or technical equipment, the calendar period, level of exposure (in six categories) and other occupational exposures were recorded in a separate questionnaire. If there were no dust measurements available, the level of exposure was assessed by industrial hygienists who were well acquainted with the situation at the work places. The hygienists had no information about the vital status or the cause of death of the worker.
Based on these information, a job exposure matrix was constructed. For all jobs and each calendar year a specific category among the six categories used was selected, mainly the mode of all the information available. The exposure of all workers who received compensation between 1993 and 2000 (the second phase of this study) was assessed by that matrix. For these workers all their jobs and the corresponding calendar years were recorded.
For the statistical analyses several indices of silica exposure are suggested. Typical surrogates of dose are duration of exposure, peak exposure intensity, or cumulative and time-weighted average exposure [15]. In this study all these indices have been calculated.
Smoking
Beside the workers’ exposure to crystalline silica, information about their smoking behaviour was recorded. These data were assessed routinely during the investigation for compensation.
Statistical analysis
The data are presented as medians and ranges (for continuous variables) or as numbers and percentages (for categorical variables). For comparison of the mortality rate between the cohort of compensated silicotic workers and the general population of Germany, standard mortality ratios (SMRs) have been calculated [16], together with 95% CIs, and were tested by Poisson distribution [17]. A significance level of α=5% was applied. The follow-up time was defined as the period between the date of compensation and the date of death or the end of the observation period (31 December 2001). In order to identify risk factors associated with total mortality, as well as with lung cancer mortality, an internal analysis using a Cox model was applied [18]. Usually, the influence of a continuous variable is assumed to be linear. However, newer methods allow a more flexible form of modelling to be used [19, 20]. Those methods have been used.
Results
Altogether, 440 male workers, alive at the time of compensation, were enrolled. The basic data are shown in Table 1. The median age of the workers at compensation was 62 years (range 36–88 years). The year of first exposure was mainly between 1945 and 1965. The duration of exposure was between 3 and 58 years, with a median of 33 years. Approximately 31% had never smoked, 27% were still smokers, 37% had stopped smoking and 5% were without any information about their smoking habits (Table 2).
Analysis of mortality
Among the 440 workers enrolled in the study, 144 had died up to the end of 2001. A total of 2,659 person-years could be obtained. The follow-up period was between 5 days and 14 years. Based on the mortality data from the general population of Germany, 74.35 cases had been expected, which led to an SMR of 1.94 (95% CI 1.63–2.28; P<0.001). A death certificate was available for all deceased workers. Lung cancer was the cause of death in 16 cases, compared with 6.67 expected cases, which resulted in a significant SMR of 2.40 (95% CI 1.37–3.90; P=0.002). Non-malignant respiratory disease (NMRD) was the leading cause of death (55 observed vs 5.43 expected cases; SMR 10.13; 95% CI 7.63–13.69). The majority of those cases died from silicosis (48 observed vs 0.23 expected). The analysis of all causes except NMRDs still shows a significantly increased SMR of 1.29 (89 observed vs 68.22 expected cases, 95% CI 1.04–1.59; P=0.011). In Table 3 the results of the mortality analysis for these causes and for other causes of death are listed.
In Fig. 1 the overall mortality rate of the cohort and of the general population, depending on the time since compensation, is shown. There is only a slight increase in the risk within the first 4 years. However, after that time it seems that the risk steadily increases. Within the first 4 years after compensation 53 out of the 144 died, compared with 38.41 expected, which gives an SMR of 1.38 (95% CI 1.03–1.80). In Table 4 the observed and the expected cases for different follow-up periods are given.
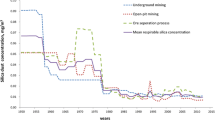
Exposure
For all workers compensated between 1988 and 1992 (n=175) a detailed description of the exposure was obtained, based on the files already opened for the proof of compensation. Up to 12 jobs with different exposure were recorded (median: 3 jobs). The level of exposure was classified into six categories, together with a category for no exposure (0; <0.03; 0.03–0.075; 0.075–0.15; 0.15–0.30; 0.30–0.75; ≥0.75 mg/m3). For approximately 25% of all jobs, measurements were available. All other exposure levels were estimated from these measurements and from the knowledge of the industrial hygienists, who were familiar with the particular work places. The maximum exposure was always above 0.15 mg/m3; in the majority of the workers in the highest category (>0.75 mg/m3). From the information about the exposure of those 175 workers, a job exposure matrix for the workers who were compensated between 1993 and 2000 (n=265) was developed (Fig. 2). For each job and each calendar year, distribution of exposure categories were available. In order for the job exposure matrix (JEM) to be constructed, the mode of these values was taken. For the calculation of the cumulative and average exposure for each of the six categories, a fixed value was ascertained. In the lower five categories (≤0.75 mg/m3) this value was the midpoint of the category. For the highest category a value of 1.5 mg/m3 was applied.
The cumulative exposure was between 0.79 and 55.5 mg/m3·years with a median at 18.9 mg/m3·years. The average exposure has a median of 0.58 mg/m3 with a range between 0.10 and 1.5 mg/m3 (Table 5).
Factors associated with various causes of death
The causes of death were categorised into four classes:
- 1.:
-
Lung cancer (n=16).
- 2.:
-
NMRD (n=55).
- 3.:
-
All other cancer (n=73).
- 0.:
-
Alive at the end of observation (n=296).
There is a significant difference in the age at compensation between the four classes. The workers still alive had a similar age at compensation as the workers who died of lung cancer (61.5 vs 61.1 years). The workers who died from NMRD or other diseases were older (65.1 at compensation, for both classes). There was also a difference in the age at the end of observation. The workers with lung cancer died at 68.6 years. All other deaths were at an older age (NMRD 71.1 years; all other causes 70.3 years). The workers still alive were younger on average (mean 67.8 years).
Within the internal analysis the workers who died of lung cancer were compared with all other workers. In the Cox model, smoking was the only factor significantly associated with the outcome. No other factor, especially those describing the exposure, could be identified.
Discussion
Between 1988 and 2000 a total of 440 workers from the stone and quarry industry were compensated for silicosis. Up to 2001, one hundred and forty four of these workers had died. They have an about twofold increased mortality risk compared with the general population. This means their life expectancy after compensation is reduced by approximately 50%. The leading cause of death given on the death certificate was silicosis or other NMRDs. However, there was still an increase in all other causes of death besides NMRD. Workers compensated for silicosis have an increased risk of developing lung cancer. Sixteen cases have been observed, compared with 6.67 expected ones, giving an SMR of 2.40. The comparison with the remaining workers showed a difference only in smoking habits. All 16 cases with lung cancer had smoked, ten of them still smoked at the time of compensation, and the remaining six had stopped smoking.
It is difficult to separate out the effect of smoking. One attempt is to adjust the expected number of cases by the difference in the smoking habits between the cohort study and the general population [21]. It is assumed that the number of expected cases had to be increased by about 30%. The effect in this study is a decrease in the SMR to a value of approximately 1.85, still significant. No association between any of the exposure indices and the lung cancer risk could be observed. The cases died at a younger age than other deceased workers.
The data about the risk of developing silicosis at certain levels of exposure are somewhat controversial. Finkelstein [22] reports that the risk of silicosis (≥1/1) following a lifetime of exposure at 0.1 mg/m3 is likely to be at least 5%–10%. Greaves [23] asserted that at an average exposure of 0.05 mg/m3 over 45 years, the risk could be in the range of approximately 10%–20%.
In a pooled analysis of ten cohort studies, Steenland et al. [11] estimated that, at an exposure of 0.1 mg/m3 respirable crystalline silica over 45 years, the excess lung cancer risk could be in the range of 1.1%–1.7%. An average exposure of 0.02 mg/m3 over 45 years could result in an excess risk of between 0.5% and 0.8%.
However, there are some limitations with this analysis and the methods used [24]. An earlier publication of one of these studies came to another conclusion [25]. An average exposure below 0.1 mg/m3 did not increase the lung cancer risk.
All the calculations are based on the cumulative exposure, which seems to be the simplest way to quantify the risk. However, a recent publication by Buchanan et al. [26] indicates that the pure use of the cumulative exposure may lead to wrong conclusions. A short but high exposure seems to produce a greater risk of developing silicosis than a long but low exposure at a similar cumulative level. This means that taking of a certain value for the cumulative exposure and dividing it by 40 or 45 years, the maximum duration of exposure, leading to an average exposure, is too simple. Therefore, it seems that two steps have to be taken into account in order for the risk of silicosis to be reduced. In this study all workers had a peak exposure above 0.15 mg/m3 and an average exposure greater than or equal to 0.10 mg/m3. One step is for the peak exposure to be reduced, and the second step is for the average exposure to be limited. Based on this cohort study the peak exposure must be at a level of 0.15 mg/m3 or lower. The average exposure should not exceed 0.10 mg/m3. All workers within this cohort study had concentrations above both values. In order for the mortality risk to be reduced, all measures should be taken to avoid silicosis. These values are recommendations, since the study was not designed to assess a threshold value that would prevent silicosis.
References
Silicosis and Silicate Disease Committee (1988) Diseases associated with exposure to silica and nonfibrous silicate minerals. Arch Pathol Lab Med 112:673–720
International Agency for Research on Cancer (1997) IARC monographs on the evaluation of carcinogenic risks to humans, silica, some silicates, coal dust and para-aramide fibrils, p 68
American Conference of Governmental Industrial Hygienists (ACGIH) (1999) Silica, Crystalline
Greim H (ed) (1999) Gesundheitsschädliche Arbeitsstoffe. Silicumdioxid
Smith AH, Lopipero PA, Barroga VR (1995) Meta-analysis of studies of lung cancer among silicotics. Epidemiology 6:617–624
Steenland K, Stayner L (1997) Silica, asbestos, man-made mineral fibers, and cancer, Cancer Causes Control 8:491–503
Mehnert WH, Staneczek W, Mohner M, Konetzke G, Muller W, Ahlendorf W, Beck B, Winkelmann R, Simonato L (1990) A mortality study of a cohort of slate quarry workers in the German Democratic Republic, IARC Sci Publ 97:55–64
Dong D, Xu G, Sun Y, Hu P (1995) Lung cancer among workers exposed to silica dust in Chinese refractory plants. Scand J Work Environ Health 21 [Suppl 2]:69–72
Ulm K, Waschulzig B, Ehnes H, Guldner K, Thomasson B, Schwebig A, Nuss H (1999) Silica dust and lung cancer in the German stone, quarrying, and ceramics industries: results of a case–control study. Thorax 54:347–351
Checkoway H, Hughes JM, Weill H, Seixas NS, Demers PA (1999) Crystalline silica exposure, radiological silicosis, and lung cancer mortality in diatomaceous earth industry workers. Thorax 54:56–59
Steenland K, Mannetje A, Boffetta P, et al (2001) Pooled exposure-response and risk assessment for lung cancer in 10 cohorts of silica-exposed workers: an IARC multi-centric study. Cancer Causes Controls 12:773–784
Checkoway H, Franzblau A (2000) Is silicosis required for silica-associated lung cancer? Am J Ind Med 37:252–259
Finkelstein MM (2000) Silica, silicosis, and lung cancer: a risk assessment. Am J Ind Med 38:8–18
Rice FL, Park R, Stayner L, Smith R, Gilbert S, Checkoway H (2001) Crystalline silica exposure and lung cancer mortality in diatomaceous earth industry workers: a quantitative risk assessment. Occup Environ Med 58:38–45
Checkoway H, Rice CH (1992) Time-weighted averages, peaks, and other indices of exposure in occupational epidemiology. Am J Ind Med 21:25–33
Breslow NE, Day NE (1987) Statistical methods in cancer research: volume II—the design and analysis of cohort studies. In: Heseltine E (ed) IARC Scientific Publications No. 82
Ulm K (1990) A simple method to calculate the confidence interval of a standardized morality ratio (SMR). Am J Epidemiol 131:373–375
Cox DR (1972) Regression models and life-tables. J R Stat Soc 34:187–220
Hastie TJ, Tibshirani RJ (1995) Generalized additive models for medical research. Stat Methods Med Res 4:187–196
Royston P, Altman DG (1994) Regression using fractional polynomials of continuous covariates: parsimonious parametric modeling. Appl Stat 43:429–467
Axelson O, Steenland K (1988) Indirect methods of assessing the effects of tobacco use in occupational studies. Am J Ind Med 13:105–118
Finkelstein MM (2000) Silica, silicosis, and lung cancer: a risk assessment. Am J Ind Med 38:8–18
Greaves IA (2000) Not-so-simple silicosis: a case for public health action. Am J Ind Med 37:245–251
Ulm K (2002) Risk assessment between silica dust and lung cancer. Cancer Causes Controls 13:779–780
Rice FL (2001) Crystalline silica exposure and lung cancer mortality in diatomaceous earth industry workers. Occup Environ Med 58:38–45
Buchanan D, Miller BG, Soutar CA (2003) Quantitative relations between exposure to respirable quartz and risk of silicosis. Occup Environ Med 60:159–164
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ulm, K., Gerein, P., Eigenthaler, J. et al. Silica, silicosis and lung-cancer: results from a cohort study in the stone and quarry industry. Int Arch Occup Environ Health 77, 313–318 (2004). https://doi.org/10.1007/s00420-004-0513-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-004-0513-6