Abstract
Objectives
To study whether different information on a study may influence the reporting of symptoms suspected to be related to poor indoor climate at the workplace or at home.
Methods
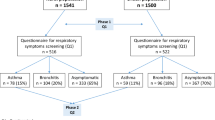
A questionnaire was mailed to a random sample (n=4,000) of the general population in Denmark. The participants were randomly allocated to two study groups, each group receiving a slightly different information letter. There were 2,710 subjects (67.8%) who completed the questionnaire, and 2,164 subjects, who were in employment, were included in the study. All subjects were informed that the purpose of the study was to assess the prevalence of non-specific symptoms related to the indoor climate at work and in dwellings. However, in the letter to one study group it was stated that knowledge was especially lacking about health effects related to the indoor climate at work (n=1,468). To the other study group the words at work were replaced with at home (n=696). The questionnaires were similar for each study group.
Results
The prevalence rates of symptoms were similar, but reporting of work-relatedness and home-relatedness differed considerably between the two study groups. If the information letter focused slightly more on the workplace than the home, the subjects were more likely to report that their symptoms were work-related (significant unadjusted odds ratios (ORs) between 1.8 and 5.5). We found that adjusting the results for several confounders mainly led to higher estimates of ORs. Likewise, the subjects reported more home-related symptoms if focus was on the environment at home (significant unadjusted ORs between 5.7 and 20.6).
Conclusions
The information about a study may play an important role in the reporting of symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years occupational and environmental health hazards have increasingly appeared as non-specific symptoms among those exposed or those feeling exposed to different emissions. Some of the conditions have even been defined as clinical entities or syndromes, such as Gulf War syndrome, Waste-disposal site syndrome, Multiple chemical sensitivity and Sick-building syndrome. Many of the symptoms are quite similar, in spite of the fact that the exposures are different. Furthermore, there is a substantial overlap of the symptoms with other conditions characterised by non-specific symptoms, for instance chronic fatigue syndrome and fibromyalgia [1, 11, 13].
Overlap of symptoms makes a case definition difficult and, consequently, the study of these conditions problematic. In addition, many psychological mechanisms can influence the reporting of symptoms [10]. Awareness of a potential environmental hazard has been shown to effect self-reported illness [5, 7]. Different information given about the consequences of an exposure to a chemical in an experimental study resulted in significant differences in reporting of health symptoms among the participants [2]. Likewise, in a questionnaire study on symptoms related to the indoor climate, participants who had been briefed on the study reported symptoms three times more frequently than those not informed [4].
Such bias complicates the interpretation of the studies and, accordingly, the risk evaluation and risk communication of occupational and environmental exposures. Earlier studies were conducted in communities where concern existed about health risks from environmental health hazards and in a work place setting. We investigated whether different information on the study influenced the reporting of symptoms in a random sample from the general population.
Material and methods
Subjects
We sent a self-completion postal questionnaire to a stratified random sample of 18 to 59-year-old persons (n=4,000) from the general population in Denmark. The general purpose of the study was to assess the prevalence of non-specific symptoms related to the indoor climate at work and in dwellings. This information was given to all subjects in a one-page information letter. For all subjects the letter was identical, except for one sentence. In the letter to study-group W (n=2,667) it was stated that knowledge was especially lacking about health effects related to the indoor climate at work. In the letter to study-group H (n=1,333) the two words "at work" were replaced with "at home". Study subjects were randomly allocated to the two study groups.
Questionnaire
All subjects answered identical questions about suffering from ten different non-specific symptoms during the previous 4 weeks. The symptoms were as follows: irritation of the eyes, irritation of the nose, stuffy/runny nose, irritation of the throat, hoarseness, dry skin on hands/arms, flushing face, tiredness, headache and lack of concentration. The subjects had to specify whether that particular symptom was more pronounced on days on or off work. Alternative response options to this were "equally present at work and at home" and "I don't know". The questionnaire also covered questions on smoking, allergies, and demographic, occupational, and personality characteristics, as well as general health (SF-12) [3] and other symptoms not usually related to the indoor climate [9]. In addition, we asked 17 questions on perceived indoor climate exposures at work and at home e.g. temperatures, odour, draught, noise, and dust.
Statistical methods
We defined a relevant symptom as a symptom reported to be present several times a week or daily, a work-related symptom as a relevant symptom that was more pronounced on workdays, and a home-related symptom as a relevant symptom that was more pronounced at home. We compared the symptom prevalence rates of the two study groups, using the chi-square test to assess differences at the 5% level of significance. The work-related symptoms were compared with the three other response options altogether (home-related, equally present at work and home, and "I don't know") and, likewise, with the home-related symptoms. We used multiple logistic regression to examine the effect of the two different information letters on reporting a symptom as work-related, allowing for potential confounders. These analyses could not be conducted with regard to the home-related symptoms because of few cases. In the model we included gender, age, allergy, smoking, negative affectivity, social support at home, a general tendency to report symptoms, job demands, job decision latitude, social support at work, psychosocial climate at work, and perceived indoor climate exposures at work. For each of the ten symptoms the indoor climate exposures were divided, a priori, into factors with a plausible biological effect on the symptom and factors without such plausible effect. Complaints about noise, for instance, were considered not to have a plausible effect on eye irritation, but were accepted as a plausible cause of headache. Initially, we controlled for all the variables but excluded, alternately, the indoor climate exposures with and without a plausible biological effect on the symptom. In the final model all the variables were entered in the model in one step. Statistical analyses were conducted with SAS software [8].
Results
A total of 2,710 subjects (67.8%) completed the questionnaire. We excluded 546 subjects who were unemployed and students/apprentices, which left 2,164 subjects in the study group (1,468 subjects in group W and 696 in group H). The two groups were comparable with respect to rate of participation, age, gender, marital status, occupation, smoking habits, general health, personality traits, and perception of physical and psychosocial work environment. Of the participants, 51.5% were female, 32.2% smoked daily, 46% were 18 to 39 years old and 54% were 40 to 59 years old.
Table 1 shows the prevalence rates of symptoms in the two study groups. The prevalence rates of symptoms were similar, with the exception of the symptoms stuffy/runny nose and throat irritation, which were reported slightly more often in group W than in group H. When we adjusted for multiple testing by the Bonferroni-Holm method the two significant results became non-significant. However, reporting of work-relatedness and home-relatedness differed considerably for several symptoms (Table 2). In the univariate analyses group W reported, that a symptom was work related up to 3.5 times as often as group H did. Likewise, group H reported that a symptom was home related up to 18 times as often as group W did (prevalence-rate ratios not shown). Even though very few subjects answered that symptoms were more pronounced at home, most of the differences were statistically significant.
Adjusting for potential confounders, we found that the subjects were still more likely to report that their symptoms were work related if the information letter focused more on the workplace than on the home (Table 2). The significant odds ratios (ORs) were as follows: eye irritation (OR=3.94), dry skin (OR=2.08), tiredness (OR=7.50), and headache (OR=3.53). It had no effect on the estimates of the ORs to include the indoor climate exposures in the model.
High demands and low support at work were important predictors, too, of the reporting of a symptom as work related (data not shown).
Discussion
With a slight difference in the letter informing of the purpose of the study, we examined whether the context of the study affects the reporting of work-related and home-related symptoms. We showed that if focus was on the environment at the workplace the subjects tended to report that their symptoms were more pronounced at work. Similarly, they reported more home-related symptoms if focus was on the environment at home.
Allocation to the two study groups was random, so it is unlikely that different exposures to physical, chemical or microbiological factors at work, or that individual factors such as personal attitudes, knowledge and beliefs, should be the cause of the different reporting in the two groups.
The increase in reporting of work-related symptoms in group W could be due to different mechanisms of selection of responders in the two study groups, group W being more willing to respond if they were dissatisfied with their work environment. However, the rate of participation was the same in the two groups, and the two groups were comparable with respect to their perception of the physical as well as the psychosocial work environment. Thus, a differential selection of responders seems unlikely.
The different focus in the information letter could affect reporting in two ways. Firstly, the letter on the work environment could make subjects answer that their symptoms were more pronounced at work solely because the letter cued them. Secondly, the letter could result in subjects considering the questions more thoroughly. However, the quality of the data was high in both groups, only few questions were skipped and only few inconsistent responses were found. This indicates that the responders in both groups had considered the questions equally carefully. Accordingly, a likely explanation for the increased prevalence of work-related or home-related symptoms in the two study groups is that the information letter cued the subjects to think of their symptoms as being worst on working days or on days off, respectively.
The findings are in accordance with our own experiences from interviewing occupants of buildings with "indoor climate problems". Often, the questionnaire statements on work-relatedness seem vague when more detailed time relations are explored by interview. Instead, a common argument for perceiving the symptoms as work-related is the awareness that many other occupants have "similar" indoor climate symptoms and that there are no other reasons for having the symptoms. Worries about potential adverse health effects from unknown or specific exposures may enhance this development.
The findings are also in accordance with previous studies that found an increase in symptom reporting if the subjects were aware of a potential hazard in the environment and, especially, if they were worried about it [2, 4, 5].
Several researchers have proposed that psychological and social factors play a central role in the reporting of symptoms and that the sick-building syndrome could be due to, or modified by, stress-related factors at work, personality factors, or a group behaviour as a "contagious" condition [6, 10, 12]. In our study the subjects filled in the questionnaire at home, out of context with the workplace, so no group behaviour ought to be present. High demands and low support at work were important predictors of the reporting of work-relatedness in our study (data not shown), but the most interesting result was the strong effect of the small difference in the information letter. This is important for one to have in mind when occupational or environmental factors are suspected causes of epidemic outbreaks of otherwise unexplained symptoms. In these cases it is essential for one to realise that the interpretation of symptom reporting requires an assessment of the psychosocial factors as well as a risk assessment of the physical or chemical potential hazard.
With respect to epidemiological research it is essential for the investigator to know that the information given about the study may influence the results and introduce bias. This may be especially important in studies on exposure–response relationships, where information on exposures as well as outcomes rely exclusively on the participants' subjective evaluations.
References
Aaron LA, Buchwald D (2001) A review of the evidence for overlap among unexplained clinical conditions. Ann Intern Med 134:868–881
Dalton P, Wysocki CJ, Brody MJ, Lawley HJ (1997) The influence of cognitive bias on the perceived odor, irritation and health symptoms from chemical exposure. Int Arch Occup Environ Health 69:407–417
Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M (1998) Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 51:1171–1178
Mikatavage MA, Rose VE, Funkhouser E, Oestenstad RK, Dillon K, Reynolds KD (1995) Beyond air quality—factors that affect prevalence estimates of sick building syndrome. Am Ind Hyg Assoc J 56:1141–1146
Moffatt S, Mulloli TP, Bhopal R, Foy C, Phillimore P (2000) An exploration of awareness bias in two environmental epidemiology studies. Epidemiology 11:199–208
Ooi PL, Goh KT (1997) Sick building syndrome: an emerging stress-related disorder? Int J Epidemiol 26:1243–1249
Roht LH, Vernon SW, Weir FW, Pier SM, Sullivan P, Reed LJ (1985) Community exposure to hazardous waste disposal sites: assessing reporting bias. Am J Epidemiol 122:418–433
SAS Institute (version 6.12) (1996) Cary, North Carolina, USA
Setterlind S, Larsson G (1995) The stress profile: a psychosocial approach to measuring stress. Stress Med 11:85–92
Spurgeon A (2002) Models of unexplained symptoms associated with occupational and environmental exposures. Environ Health Perspect 110 [Suppl 4]:601–605
Spurgeon A, Gompertz D, Harrington JM (1997) Non-specific symptoms in response to hazard exposure in the workplace. J Psychosom Res 43:43–49
Thorn A (2000) Emergence and preservation of a chronically sick building. J Epidemiol Community Health 54:552–556
Wessely S, Nimnuan C, Sharpe M (1999) Functional somatic syndromes: one or many? Lancet 354:936–939
Acknowledgements
The Danish Working Environment Council financially supported the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brauer, C., Mikkelsen, S. The context of a study influences the reporting of symptoms. Int Arch Occup Environ Health 76, 621–624 (2003). https://doi.org/10.1007/s00420-003-0463-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-003-0463-4