Abstract
Objectives
To determine the prevalence of musculoskeletal pain in Norwegian nurses’ aides and how it varies with demographic factors, number of working hours per week, and service sector.
Methods
A random sample of nurses’ aides, represented by the Norwegian Union of Health and Social Workers, was mailed a questionnaire in 1999. The 6,485 vocationally active respondents who were not on leave because of illness or pregnancy comprised the sample of the present study.
Results
The prevalence (previous 14 days) of musculoskeletal pain was 88.8% [95% confidence interval (CI) 88.0–89.6%]. The prevalence of intense musculoskeletal pain was 51.1% (CI 49.9–52.3%). The prevalence of widespread pain was 26.6% (CI 25.5–27.7%). The prevalence of pain in the extremities increased with increasing age, whereas the prevalence of headache decreased with increasing age. Neck, shoulder, elbow, high back, and hip pains were more prevalent in women than in men. The prevalence of neck pain increased with increasing working hours per week. Low back pain was most prevalent in persons working in nursing homes. Pain in the extremities was most prevalent in persons working in nursing homes and in those who were working in somatic hospital departments for adults. Headache was most prevalent in persons working in institutions for mentally handicapped people. The prevalence of musculoskeletal pain was lowest in persons working in psychiatric and paediatric departments and the community-nursing service.
Conclusions
The prevalence of musculoskeletal pain in Norwegian nurses’ aides is very high. Not only the lower back but also several other regions of the body are frequently affected. The prevalence rates vary with age, gender, working hours per week, and the service sector in which the aides are working.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies indicate that nurses’ aides, the main providers of practical patient care in the health service, are frequently bothered by health problems and have a poorer health than many other occupational groups, including registered nurses (Leppänen and Olkinuora 1987; Estryn-Behar et al. 1990a, 1990b; Fuortes et al. 1994; Lagerström et al. 1995). However, there is sparse knowledge of the aides’ health situation, even when it comes to musculoskeletal health, which is essential in this occupation. There has indeed been extensive epidemiological research on low back pain in nursing personnel (for reviews, see Kaplan and Deyo 1988; Lagerström et al. 1998). However, few international studies of nursing personnel have focused on pain in other regions of the body (Lagerström et al. 1995; Engels et al. 1996; Ando et al. 2000), and only one of those reported data for nurses’ aides in particular (Lagerström et al. 1995). More knowledge of the health problems with which nurses’ aides are afflicted could result in a widening of the focus of causal research and preventive practice targeting this important occupational group.
Nurses’ aides are exposed to both mechanical and psychosocial stress at work. The type, intensity, and quantity of work stress may vary, though, according to service sector and number of working hours per week. Some studies have shown that the occurrence of back pain in hospital nurses is higher in surgical and medical wards than in paediatric, psychiatric, and gynaecological wards (Venning et al. 1987; Yassi et al. 1995). Higher risk of back pain has been found in full-time nurses than in part-time nurses (Yassi et al. 1995). Nevertheless, little is known of how the occurrence of musculoskeletal symptoms in nursing personnel is related to service sector and working hours. More knowledge of the epidemiological distribution of musculoskeletal symptoms could provide clues to the pathophysiological processes behind the symptoms, and indicate preferential groups of personnel for future interventions.
The objective of this study was to determine the prevalence of musculoskeletal pain in Norwegian nurses’ aides. We wanted to determine the prevalence of pain in several parts of the body and to explore how these complaints vary with demographic characteristics, number of working hours per week, and the service sector in which the aides are working.
Methods
Participants
Nursing personnel in Norway include two large occupational groups: the registered nurses (graduate nurses), with 3 years training after high school, and the certified nurses’ aides, with either a 1-year course after junior high school or a course that is part of a high school programme. In addition to those two large groups, a smaller group of unlicensed assistive nursing personnel has no formal training and often holds temporary jobs.
The Norwegian Union of Health and Social Workers represents the great majority of certified nurses’ aides in Norway. In 1999, a random sample of nurses’ aides in this union was mailed a questionnaire. After one reminder, 7,478 of 12,000 (62.3%) consented to participate in the study and completed the questionnaire. The sample of the present study comprised the 6,485 nurses’ aides who were vocationally active and not on leave because of illness or pregnancy.
Measurements
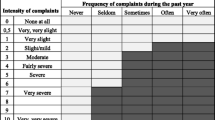
Musculoskeletal pain during the previous 14 days was recorded with a questionnaire that was a modification of the standardised Nordic questionnaire (Kuorinka et al. 1987). There were questions about the intensity of pain in the head, neck, shoulder, elbow, hand or wrist, upper or lower back, hip, knee, and ankle or foot. There was a checklist for each part of the body with the following optional answers: not bothered, a little bothered, rather intensely bothered, and very intensely bothered. The questions were supplemented by a “pain-region drawing”. Widespread pain was defined as pain both in the midline area (head, neck, upper or lower back), upper limbs (shoulder, elbow, wrist or hand), and lower limbs (hip, knee, ankle or foot).
The service sector in which the subjects were working was registered from the question “What is your main work place?”. There was a checklist with 12 optional answers.
Ethics
The research protocol was approved by the Committee for Medical Research Ethics, and the study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Informed written consent was given by the respondents prior to their inclusion in the study.
Statistical analyses
We used cross-tabulation and chi-square tests to examine the statistical relationship between demographic factors, working hours per week, and service sector, and the prevalence of headache or pain in the neck, shoulder, elbow, hand or wrist, higher back, lower-back, hip, knee, and foot or ankle.
Results
Prevalence of musculoskeletal pain
Table 1 presents the 14 day-prevalence rates of musculoskeletal pain in various locations.
The prevalence of musculoskeletal pain in one or several locations was 88.8% [95% confidence interval (CI) 88.0–89.6%]. The prevalence of intense (rather intense or very intense) musculoskeletal pain was 51.1% (CI 49.9–52.3%). The prevalence of widespread pain (i.e. pain in the midline area, upper extremities, and lower extremities) was 26.6% (CI 25.5–27.7%). Low back pain was the most prevalent type of pain. Head, neck, and shoulders were also very frequently affected.
Demographic characteristics and prevalence of musculoskeletal pain
The prevalence of pain in the extremities increased with increasing age, whereas the prevalence of headache decreased with increasing age (Table 2). The graph of the relationship between age and the occurrence of neck pain and high back pain tended to be hump-shaped, with lowest prevalence rates in the youngest and the oldest age groups. Neck, shoulder, elbow, high back, and hip pains were more prevalent in women than in men. Neck and low back pain, and pain in the hand or wrist were more prevalent in single persons than in married or cohabiting individuals.
Working hours per week and prevalence of musculoskeletal pain
The prevalence of neck pain increased with increasing number of working hours per week (Table 3). The prevalence of pain in other regions of the body was not significantly related to the number of working hours per week.
Service sector and prevalence of musculoskeletal pain
Headache was most prevalent in persons working in institutions for mentally handicapped people and less prevalent in those who were working in paediatric departments and somatic departments for adults (Table 4). Neck pain was most prevalent among aides working in old people’s homes. High back pain also tended to be more prevalent among those who were working in old people’s home, but this tendency was not statistically significant. Low back pain was most prevalent in subjects working in nursing homes and less prevalent in those who were working in psychiatric departments. Pain in the limbs was most prevalent among individuals working in nursing homes and somatic hospital departments and less common in persons working in paediatric departments and the community-nursing service.
Discussion
In this survey of Norwegian nurses’ aides, 9 out of 10 reported that they had been bothered by musculoskeletal pain during the previous 14 days. One-half had been intensely bothered. Not only the lower back but also several other regions of the body were frequently affected. The prevalence rates varied with the aides’ age, gender, marital status, and working hours per week, and with the service sector in which the aides were working.
Methodological considerations
The results of the present study must be interpreted in the light of the limitations of the study. The overall response rate was moderate (62%), and as only the vocationally active respondents were included in the present study, the sample comprised 54% of those who were invited to fill in the questionnaire. However, the true response rate in vocationally active subjects was probably higher than 62%. The list of members of the Norwegian Association of Health and Social Workers also includes many retired persons, and contact over the telephone during the data collection gave the impression that non-working subjects were not motivated to participate in the study. The sample that was established was most likely representative for vocationally active nurses’ aides in Norway. Even so, some may have chosen not to participate in the study for reasons other than retirement or not currently working in the field. If subjects affected by musculoskeletal pain were more inclined to respond than healthy subjects, the measured prevalence rates may be somewhat higher than the true ones. If the motivation for participating in the study were also related to demographic factors and work characteristics, the statistical relationship between these factors and the prevalence of pain may have been influenced.
Pain is a subjective experience, and there exists no “gold standard” with which one may calibrate the instrument of measurement. However, test–retest reliability for reporting the presence of musculoskeletal pains during the previous 7 days and during the previous 12 months has been reported to be good (Kuorinka et al. 1987). The average of diary ratings of pain intensity over 2 weeks has been found to be strongly correlated to the retrospective ratings of the pain intensity (Jensen et al. 1996). Different techniques for measuring the severity of pain yield approximately similar results, whether it be visual analogue scales, numerical rating scales, or verbal rating scales (Raspe and Kohlman 1994).
As the study had a cross-sectional design, one cannot conclude causal associations. Several types of selection processes may have influenced the statistical relationship between the independent factors and the prevalence of pain. For example, unhealthy persons may have avoided specific high-exposure jobs or changed to lower-exposure jobs, and they may have preferred part-time jobs to full-time jobs. This may have weakened statistical associations between demanding working conditions and the occurrence of pain, and thereby levelled out differences between service sectors as well as differences between part-time and full-time jobs. The high frequency of disability pensioning in nurses’ aides because of musculoskeletal disorders (Bjerkedal and Wergeland 1995) may have resulted in a healthy-worker selection in the highest age groups, and true age-related increments in the prevalence of pain may have been veiled. The statistical relationship between marital status and the occurrence of pain may also have been influenced by selection, as unhealthy individuals may be less likely to find and retain a partner.
The prevalence of musculoskeletal pain
The prevalence of musculoskeletal pain was very high in this sample of vocationally active, Norwegian nurses’ aides. Not only the lower back but several other regions of the body were frequently affected. Lagerström et al. also found very high prevalence rates of pain in nurses’ aides (Lagerström et al. 1995). They reported that the prevalence of ongoing pain in the 268 nurses’ aides at a hospital in Sweden was as high as 60% in the shoulders, 59% in the neck, 35% in the knees, and 30% in the hands (Lagerström et al. 1995). These rates are, in fact, even higher than the ones found in the present study, but the sample of the Swedish study was restricted to nurses’ aides at one hospital.
Demographic and work-related characteristics and the prevalence of pain
Pain in the extremities became increasingly prevalent with increasing age, was more common in women than in men, and was more common in service sectors in which the physical demands are high, such as nursing homes. Hand or wrist pain was more prevalent in single persons than in married or cohabiting subjects. One explanation may be that pain in the extremities often originates from a long-term wear-and-tear process. Other studies have related upper limb disorders to physical work-demand factors (Fredriksson et al. 1999; Armstrong et al. 1993). The high prevalence in women may reflect the effect of mechanical load on physically weaker and more vulnerable limbs. In clinical practice, pain in the extremities is often interpreted as symptoms of tendinitis, bursitis, or osteoarthritis.
Like pain in the extremities, low back pain was more prevalent in service sectors in which the physical demands are high. Heavy lifting and frequent bending and twisting at work are well-documented risk factors of low back pain (Burdorf and Sorock 1997). However, unlike the prevalence of pain in the extremities, the prevalence of low back pain did not vary in a significant way with age and gender. In community studies, the prevalence of back pain seems to increase with age up to approximately 45–50 years, levelling off in older groups or decreasing slightly, whereas studies of occupational populations show no consistent association between age and back pain (for review, see Burdorf and Sorock 1997). Earlier studies also show no consistent association between gender and back pain (for review, see Burdorf and Sorock 1997). One explanation for the difference between limb pain and low back pain in epidemiological distribution may be that the pathophysiological processes behind these complaints are different. In the extremities, mechanical load tends to affect tendons, bursas, and joints. In the back other structures, such as inter-vertebral discs and muscles, are, perhaps, more likely to be affected. Osteoarthritis is also frequently seen in the lumbar spine, but is usually not associated with pain (Bogduk and Twomey 1991).
Headache became less prevalent with increasing age and was most common among persons working in institutions for mentally handicapped people. Nurses’ aides who work in such institutions are exposed to intense psychological stress (Abrahamsen 1994), and the high prevalence of headache among these aides could be a result of psychological factors. Several studies have related headache to psychological work stress (Rasmussen 1992; Antonov and Isacson 1997; Tobiasz-Adamczyk et al. 1985). It is unclear why headache was more common in the youngest age groups. In a study of the population of 11 Danish municipalities, the prevalence of tension-type headache decreased with increasing age, especially in women, whereas no correlation was found between age and the prevalence of migraine (Rasmussen et al. 1991). In a study of the Swedish population, however, Antonov et al. found no association in women between age and the prevalence of frequent headache (Antonov and Isacson 1997).
Neck pain and high back pain were more common in the 30–59-year-olds than in the youngest and the oldest age groups, and more common in women than in men. Neck pain was more common in individuals working many hours per week, and more common in single persons. One explanation may be that neck pain and high back pain, often interpreted as symptoms of “trapezius myalgia”, are evoked by high work demands or by role strain (Marks 1977) due to the double burden of combining paid work with family obligations. A hump-shaped graph of the relationship between age and the prevalence of neck pain and high back pain has also been reported by others (Natvig et al. 1995), as has the high prevalence of neck pain and high back pain in women (Natvig et al. 1995). Prospective studies indicate that high quantitative work demands may be a risk factor of neck pain (Fredriksson et al. 1999; Ariëns et al. 2001). It is unclear why neck pain and high back pain were more prevalent in persons who worked in old people’s homes than in those who worked in other sectors.
Conclusions
The study indicates that the prevalence of musculoskeletal pain in Norwegian nurses’ aides is very high. Not only the lower back but also several other regions of the body are frequently affected. The prevalence rates vary with the aides’ demographic characteristics, the number of hours they work per week, and with the service sector in which they are working.
References
Abrahamsen B (1994) Ustabilitet blant hjelpepleiere—jobb eller familie? (Instability among nurses’ aides—job or family?). Institute for Social Research, Oslo. Rapport 94:9
Ando S, Ono Y, Shimaoka M, et al. (2000) Associations of self estimated workloads with musculoskeletal symptoms among hospital nurses. Occup Environ Med 57:211–216
Antonov K, Isacson D (1997) Headache in Sweden: the importance of working conditions. Headache 37:228–234
Ariëns GAM, Bongers PM, Hoogendoorn WE, et al. (2001) High quantitative job demands and low coworker support as risk factors for neck pain. Spine 26:1896–1903
Armstrong TJ, Buckle P, Fine LJ, et al. (1993) A conceptual model for work-related neck and upper-limb musculoskeletal disorders. Scand J Work Environ Health 19:73–84
Bjerkedal T, Wergeland E (1995) Disability pension because of musculoskeletal diseases among women in different occupations in Norway 1993 (in Norwegian). Tidsskr Nor Laegeforen 115:3522–3527
Bogduk N, Twomey LT (1991) Clinical anatomy of the lumbar spine, 2nd edn. Churchill Livingstone, London
Burdorf A, Sorock G (1997) Positive and negative evidence of risk factors for back disorders. Scand J Work Environ Health 23:243–256
Engels JA, van der Gulden JWJ, Senden TF, et al. (1996) Work related risk factors for musculoskeletal complaints in the nursing profession: results of a questionnaire survey. Occup Environ Med 53:636–641
Estryn-Behar M, Kaminski M, Peigne E, et al. (1990a) Strenuous working conditions and musculo-skeletal disorders among female hospital workers. Int Arch Occup Environ Health 62:47–57
Estryn-Behar M, Kaminski M, Peigne E, et al. (1990b) Stress at work and mental health status among female hospital workers. Br J Ind Med 47:20–28
Fredriksson K, Alfredsson L, Köster M, et al. (1999) Risk factors for neck and upper limb disorders: results from 24 years of follow up. Occup Environ Med 56:59–66
Fuortes LJ, Shi Y, Zhang M, et al. (1994) Epidemiology of back injury in university hospital nurses from review of workers’ compensation records and a case- control survey. J Occup Med 36:1022–1026
Jensen MP, Turner LR, Turner JA, et al. (1996) The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain 67:35–40
Kaplan RM, Deyo RA (1988) Back pain in health care workers. Occup Med 3:61–73
Kuorinka I, Jonsson B, Kilbom A, et al. (1987) Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 18:233–237
Lagerström M, Wenemark M, Hagberg M, et al. (1995) Occupational and individual factors related to musculoskeletal symptoms in five body regions among Swedish nursing personnel. Int Arch Occup Environ Health 68:27–35
Lagerström M, Hansson T, Hagberg M (1998) Work-related low-back problems in nursing. Scand J Work Environ Health 24:449–464
Leppänen RA, Olkinuora MA (1987) Psychological stress experienced by health care personnel. Scand J Work Environ Health 13:1–8
Marks SR (1977) Multiple roles and role strain: some notes on human energy, time and commitment. Am Sociol Rev 42:921–936
Natvig B, Nessiøy I, Bruusgaard D, et al. (1995) Musculoskeletal symptoms in a local community. Eur J Gen Pract 1:25–28
Rasmussen BK (1992) Migraine and tension-type headache in a general population: psychosocial factors. Int J Epidemiol 21:1138–1143
Rasmussen BK, Jensen R, Schroll M, et al. (1991) Epidemiology of headache in a general population—a prevalence study. J Clin Epidemiol 44:1147–1157
Raspe H, Kohlman T (1994) Disorders characterised by pain: a methodological review of population surveys. J Epidemiol Community Health 48:531–537
Tobiasz-Adamczyk B, Flak E, Jedrychowski WA (1985) Impact of psychosocial factors on the prevalence of headaches in the industrial setting. Neuroepidemiology 4:86–95
Venning PJ, Walter SD, Stitt LW (1987) Personal and job-related factors as determinants of incidence of back injuries among nursing personnel. J Occup Med 29:821–825
Yassi A, Khokhar J, Tate R, et al. (1995) The epidemiology of back injuries in nurses at a large Canadian tertiary care hospital: implications for prevention. Occup Med 45:215–220
Acknowledgements
This study was supported by the Norwegian Research Council, EXTRA funds from the Norwegian Foundation for Health and Rehabilitation fund, The Norwegian Ministry of Health and Social Affairs, Rhône-Poulenc Rorer Ltd., Peter Møller AS, and the Dr.Trygve Gythfeldt Research Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eriksen, W. The prevalence of musculoskeletal pain in Norwegian nurses’ aides. Int Arch Occup Environ Health 76, 625–630 (2003). https://doi.org/10.1007/s00420-003-0453-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-003-0453-6