Abstract
Demonstration of glycogen can be done in different lesions and is considered diagnostically significant, mainly in some tumors. Glycogen staining is affected by the type of fixative, the temperature of fixation, and the staining technique.
Grocott’s methenamine (hexamine) silver technique quality was assessed after four different types of fixatives at two different temperatures [Bouin’s solution, 10% neutral buffered formalin (NBF), 80% alcohol, and Rossman’s solution at room temperature (RT) and 4 °C, for 24 h]. These variables were studied to optimize this technique for glycogen demonstration. Archived paraffin blocks were used in this study. They were prepared from one rabbit’s liver, and 32 paraffin sections were prepared and stained with Grocott’s methenamine (hexamine) silver technique. Eighty percent alcohol provided the highest staining quality scores at both RT and 4 °C in comparison with the other fixatives. We concluded that 80% alcohol at 4 °C seems to be the fixative of choice for glycogen with the Grocott’s methenamine (hexamine) silver technique at the level of this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glycogen is demonstrated in different lesions including glycogen storage disease (Tay et al. 2004), Ewing sarcoma (Mahoney and Alexander 1978), and juvenile rhabdomyosarcoma (de Wit 1986). Furthermore, glycogen can be demonstrated in some carcinomas including bladder cancer (Rigby and Franks 1970).
Gomori’s methenamine–silver nitrate was first described for glycogen and mucin demonstration (Gomori 1946), then was used by Grocott (1955) as a fungal stain in both smears and tissue. However, Grocott’s methenamine (hexamine) silver technique is a valuable technique for glycogen demonstration, which can provide staining results similar to those obtained by the periodic acid–Schiff (PAS) reaction, when used in combination with diastase or amylase control (Totty 2002).
It has been suggested that glycogen fixation involves one or both of two processes: first, the use of a fixative in which glycogen is not soluble and second, the use of a water soluble fixative that is an effective fixative of proteins, so that the glycogen is trapped (Totty 2002). Furthermore, some workers recommend picric acid-containing fixatives for glycogen fixation (Totty 2002). Consequently, in the present study we examined the effect of three types of fixatives (picric acid-containing, alcoholic, and aqueous fixatives) at 4 °C and room temperature (RT) to determine the optimal combination for demonstrating glycogen using Grocott’s methenamine (hexamine) silver method.
Methods
Study design
In this study, we examined the quality of the Grocott’s methenamine (hexamine) silver method in tissues fixed in different fixatives and temperatures of fixation.
In this study, we used archived liver paraffin blocks of known preparation methods. The blocks were obtained from another group in our department. These blocks were prepared from one rabbit by that group as follows:
Sampling
The liver was washed in normal saline, cut into eight sections of approximately 5 × 3 × 3 mm, and transferred to the required fixative.
Fixation
Each piece was fixed for 24 h in one of four fixatives: neutral buffered formalin (NBF), Bouin’s solution, 80% alcohol, or Rossman’s solution, at one of two temperatures: 4 °C in a refrigerator or RT.
Postfixation treatment
Tissues fixed in Rossman’s solution were treated with 95% alcohol for 2 h, while those fixed in Bouin’s solution were treated with 75% alcohol for 2 h (Hopwood 2002). Then each specimen was transported to a cassette, labeled according to the temperature of fixation and type of fixative.
Tissue processing
The specimens were transferred to the automated tissue processor. For dehydration, specimens fixed in 80% alcohol were transferred to one change of 80% alcohol followed by four changes of absolute alcohol for 1 h each. The specimens fixed in Bouin’s solution were dehydrated in one change of both 75% and 90% alcohol, followed by four changes of absolute alcohol for 1 h each. Specimens fixed in Rossman’s solution were dehydrated in one change of 95% alcohol followed by four changes of absolute alcohol for 1 h each. Specimens fixed in 10% NBF were dehydrated in one change of both 70% and 90% alcohol, followed by four changes of absolute alcohol for 1 h each. All specimens were cleared in two changes of xylene for 2 h each, impregnated in two changes of melted paraffin wax at 60 °C for 2 h each, embedded in paraffin wax using metal molds, and left to harden at room temperature and then in the refrigerator.
Cutting
Thirty-two albumenized and labeled slides were prepared and 3 µm sections were cut using a rotary microtome, four sections from each block (three tests and one control for each variable).
Staining
All sections were dewaxed with xylene for 6 min, hydrated in descending concentrations of alcohols from absolute through 90% and 70% to distilled water (DW) for 2 min each. Four sections from each block were stained by Grocott’s methenamine (hexamine) silver technique (three tests and one control).
For Grocott’s methenamine (hexamine) silver technique, sections were treated with 5% aqueous chromic acid for 1 h, washed in tap water, rinsed in 1% sodium metabisulfite, washed for 5 min in tap water, rinsed in DW, and placed in a preheated (56 °C) incubating solution in the dark for up to 1 h (composed of 25 ml DW, 5 ml borax solution, and 25 ml methenamine silver solution). Sections were then rinsed in DW, treated with 3% sodium thiosulfate for 5 min, counterstained with Arzac’s stain for 15 s, blotted, dehydrated in alcohol, cleared in xylene, and mounted in distyrene, plasticizer, and xylene (DPX) (Stevens and Francis 1996).
Control sections
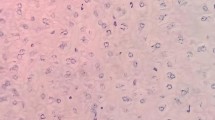
The negative control sections were brought to water, treated with saliva (a source of amylase) for 1 h at 56 °C in a water bath, then washed in running tap water and stained with the required technique (Fig. 1).
Scoring system
A subjective assessment of staining results was performed by two examiners, in which scores from zero to ten were given (Zakout et al. 2010). Scores were assigned as follows: from 0–4 (poor staining results), 5–6 (satisfactory staining results), 7–8 (good staining results), and 9–10 (excellent staining results). The average score of two examiners was calculated for each test section and the staining quality results were as follows:
Poor: 0 to < 5: glycogen is weakly stained, the granules appear small and indistinct, and identifying glycogen is hard.
Satisfactory: 5 to < 7: the glycogen is faintly stained; however, it is visible.
Good: 7 to < 9: glycogen is visible and distributed fairly evenly throughout the section.
Excellent: 9 to 10: glycogen is visible and the granules are large and well stained, and distributed fairly evenly all through the section.
Results and discussion
Eighty percent alcohol at 4 °C showed the highest staining quality (average score: 8.7) in comparison with other fixatives at the same temperature (Table 1, Figs. 2, 3, 4, 5). However, Bouin’s solution gave good results at this temperature (average score: 7.5), but with a lower average score compared with 80% alcohol. Furthermore, when fixation was conducted at RT, 80% alcohol was also found to be the best fixative for glycogen demonstration (average score: 8.3), where both Bouin’s solution and NBF fixatives gave satisfactory results, and Rossman’s solution provided poor results at the same temperature.
For the accurate preservation and demonstration of glycogen, it is fundamental to choose an appropriate fixative, temperature of fixation, and staining method. This study aimed to optimize Grocott’s methenamine (hexamine) silver for demonstration of glycogen by determining the best fixative and temperature of fixation for Grocott’s methenamine (hexamine) silver technique, using 80% alcohol, NBF, Bouin’s fluid, and Rossman’s fluid, at both RT and 4 °C.
In this study, 80% alcohol at 4 °C gave the highest average score of staining quality for glycogen demonstration using the hexamine silver method. By using this technique, glycogen appears black and is distributed in hepatocytes. These findings support the results obtained by Kugler and Wilkinson (1964). In their study, they reported that ice-cold 80% alcohol was a good preserver for glycogen present in the tissue when using different histochemical reactions. Bouin’s solution at 4 °C also provided good staining results, but its average score was less than that of 80% alcohol. The authors of that study used different types of fixatives. However, formalin was apparently used in their study without adding a buffer; this can lead to the presence of formalin pigment, which might affect the quality of evaluating glycogen in tissue. In our study, we used 10% NBF, which could prevent the formation of the formalin pigments and provides a more accurate and reliable evaluation for glycogen in the stained sections. Kugler and Wilkinson (1964) did not mention the temperature of fixation that was used in their study. In our study, we used two degrees of temperature (room temperature and 4 °C). This point is very critical as a low temperature during fixation could avoid the accumulation of glycogen at one side of the cells (polarization).
Kinsley et al. (2000) studied different fixatives to identify the best one for the preservation of glycogen in mouse liver. They evaluated four different types of fixatives: 100% ethyl alcohol, 1% periodic acid in 10% NBF, alcoholic formalin, and 10% NBF. They concluded that 1% periodic acid in 10% NBF for 48 h at 4 °C was the best fixative to preserve glycogen. The main drawback of their study was the omission of using any picric acid-containing fixatives, which are recommended for glycogen fixation (Totty 2002). In our study; Bouin’s fixative, which is one of the main picric acid-containing fixatives, was included. Another point of superiority of our current study is that Kinsley et al. (2000) did not evaluate Grocott’s methenamine (hexamine) silver method for glycogen demonstration. Instead, they only evaluated hematoxylin and eosin, periodic acid–Schiff reagent (PAS), and PAS after diastase digestion.
Trott (1961) evaluated several types of fixatives for fixing glycogen in rats’ liver. He used Rossman’s solution, alcohol formalin, Carnoy’s fluid, 10% neutral formalin, Bouin’s, acetic alcohol formalin, 10% formalin, and formol–saline for different durations. He concluded that good glycogen staining with the PAS method can be obtained after 3 months of fixation with acetic alcohol formalin. Furthermore, he reported that the aqueous-based fixatives tend to be unreliable for demonstrating the maximum amount of glycogen after 24–48 h of fixation. One point of superiority of our current study is that Trott (1961) did not evaluate Grocott’s methenamine (hexamine) silver method for glycogen demonstration. He only evaluated periodic acid–Schiff reagent (PAS) and Best’s carmine methods. Additionally, the temperature of fixation was not clarified in that study.
Moreover, Trott (1961) observed that the appearance of glycogen can be affected by the type of fixation. He found that tissues fixed in acetic alcohol formalin provide the most obvious polarization. However, he mentioned that less polarization is noticed following aqueous-based fixatives. Additionally, larger and coarser glycogen granules were observed following alcohol-based fixatives.
Also, we found that Grocott’s methenamine (hexamine) silver technique is a useful method for glycogen demonstration, particularly when tissue was fixed in 80% alcohol, in which it demonstrated glycogen as black clumps or granules in hepatocytes. This conclusion is supported by the finding of Murgatroyd (1971), who recommended this method as a good technique for glycogen demonstration. In conclusion, 80% alcohol seems to be the best fixative for glycogen demonstration by Grocott’s methenamine (hexamine) silver technique, which provides good staining results at both RT and 4 °C.
Data availability
All data generated or analysed during this study are included in this published article.
References
Gomori G (1946) A new histochemical test for glycogen and mucin. Am J Clin Pathol 10:177–179. https://doi.org/10.1093/ajcp/16.11_ts.177
Grocott RG (1955) A stain for fungi in tissue sections and smears using Gomori’s methenamine-silver nitrate technic. Am J Clin Pathol 25:975–979. https://doi.org/10.1093/ajcp/25.8_ts.0975
Hopwood D (2002) In: Theory and Practice Histological Techniques, Bancroft JD, Gamble M 5th (eds.), Churchill Livingstone, pp.76.
Kinsley D, Everds N, Arp L, Becker J, Geraci M (2000) Optimization of techniques for the preservation of glycogen in paraffin embedded mouse liver. J Histotechnol 23:51–55. https://doi.org/10.1179/his.2000.23.1.51
Kugler JH, Wilkinson WJC (1964) Quantitative studies with the solutions used for the fixation of glycogen. Acta Anat (basel) 56:184–195. https://doi.org/10.1159/000142501
Mahoney JP, Alexander RW (1978) Ewing’s sarcoma. a light- and electron-microscopic study of 21 cases. Am J Surg Pathol 2:283–298. https://doi.org/10.1097/00000478-197809000-00005
Murgatroyd LB (1971) Chemical and spectrometric evaluation of glycogen after routine histological fixatives. Stain Technol 46:111–119. https://doi.org/10.3109/10520297109067834
Rigby CC, Franks LM (1970) A human tissue culture cell line from a transitional cell tumour of the urinary bladder: growth, chromosone pattern and ultrastructure. Br J Cancer 24:746–754. https://doi.org/10.1038/bjc.1970.89
Stevens A, Francis RJ (1996). In: Theory and Practice of Histological Techniques, Bancroft JD, Stevens A, 4th ed., Churchill Livingstone, pp. 301.
Tay SK, Akman HO, Chung WK, Pike MG, Muntoni F, Hays AP, Shanske S, Valberg SJ, Mickelson JR, Tanji K, DiMauro S (2004) Fatal infantile neuromuscular presentation of glycogen storage disease type IV. Neuromuscul Disord 14:253–260. https://doi.org/10.1016/j.nmd.2003.12.006
Totty BA (2002). In: Theory and Practice Histological Techniques, Bancroft JD, Gamble M, 5th ed., Churchill Livingstone, pp. 170, 176.
Trott JR (1961) An evaluation of methods commonly used for the fixation and staining of glycogen. J Histochem Cytochem 9:703–710. https://doi.org/10.1177/9.6.703
de Wit LJ (1986) Fine Cytofilaments in a metastatic Juvenile Rhabdomyosarcoma (UP 6:341–346, 1984). Ultrastruct Pathol 10:107. https://doi.org/10.3109/01913128609015568
Zakout YM, Salih MM, Ahmed HG (2010) The effect of fixatives and temperature on the quality of glycogen demonstration. Biotech Histochem 85:93–98
Acknowledgements
We would like to thank Abeer Babiker Abdalraheem, Alobeid Mohammed Gubara, and all who assessed this study. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Atheelah Mohammed Idris and Hibatalla Elshazli Elgamri performed the technical work and histological techniques including cutting,and staining. Samah Abdelrahim Batran was responsible of the assessment of the results and the revising of the manuscript. Yosef Mohamed-Azzam Zakout was responsible of planning, designing, and directing the study, and writing and preparing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Idris, A.M., Elgamri, H.E., Batran, S.A. et al. Standardization of Grocott’s methenamine (hexamine) silver method for glycogen demonstration in liver tissue. Histochem Cell Biol 160, 159–163 (2023). https://doi.org/10.1007/s00418-023-02199-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-023-02199-0