Abstract
The phenotypic modulation of contractile vascular smooth muscle cell (VSMC) is widely accepted as the pivotal process in the arterial remodeling induced by hypertension. This study aimed to investigate the potential role of transient receptor potential vanilloid type 1 (TRPV1) on regulating VSMC plasticity and intracranial arteriole remodeling in hypertension. Spontaneously hypertensive rats (SHR), Wistar–Kyoto (WKY) rats and TRPV1−/− mice on a C57BL/6J background were used. By microscopic observation of the histopathological sections of vessels from hypertensive SHR and age-matched normotensive WKY control rats, we found that hypertension induced arterial remodeling. Decreased α-smooth muscle actin (α-SMA) and SM22α while increased osteopontin (OPN) were observed in aorta and VSMCs derived from SHR compared with those in WKY, and VSMCs derived from SHR upregulated inflammatory factors. TRPV1 activation by capsaicin significantly increased expression of α-SMA and SM22α, reduced expression of OPN, retarded proliferative and migratory capacities and inhibited inflammatory status in VSMCs from SHR, which was counteracted by TRPV1 antagonist 5′-iodoresiniferatoxin (iRTX) combined with capsaicin. TRPV1 activation by capsaicin ameliorated intracranial arteriole remodeling in SHR and deoxycorticosterone acetate (DOCA)-salt hypertensive mice. However, the attenuation of arteriole remodeling by capsaicin was not observed in TRPV1−/− mice. Furthermore, TRPV1 activation significantly decreased the activity of PI3K and phosphorylation level of Akt in SHR-derived VSMCs. Taken together, we provide evidence that TRPV1 activation by capsaicin attenuates intracranial arteriole remodeling through inhibiting VSMC phenotypic modulation during hypertension, which may be at least partly attributed to the suppression PI3K/Akt signaling pathway. These findings highlight the prospect of TRPV1 in prevention and treatment of hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is an important global public-health burden with high frequency. The number of adults with hypertension is estimated to increase to a total of 1.56 billion in 2025, especially in economically developing regions (Kearney et al. 2005). Intracranial arteriole remodeling is the major adaptive mechanism to chronic increased blood pressure. However, maladaptive remodeling results in detrimental sequelae of luminal narrowing and hypoperfusion. Vascular smooth muscle cell (VSMC) is a key player in the process of vascular remodeling. VSMCs within mature vessels are highly plastic cells that can alter their phenotype in response to local environmental changes including atherosclerosis, angiogenesis and hypertension (Owens et al. 2004). As a result, the resident quiescent VSMCs undergo phenotypic modulation or switching which is characterized by decreased contractility but enhanced proliferative and migratory capabilities, as well as increased production of matrix and inflammatory cytokines. Although this plasticity is believed to have evolved as a mechanism of vascular repair, inappropriate or excessive phenotypic modulation acts as main contributor to vascular remodeling. Reportedly, about 60 % of neointimal volume is composed of VSMCs during early remodeled vessels (Farb et al. 2004). Therefore, the attenuation or inhibition of VSMC phenotypic modulation may represent an important therapeutic intervention in hypertension.
Capsaicin (8-methyl-N-vanillyl-trans-6-nonenamide) is the major pungent ingredient in hot pepper with well-known function of enhancing energy metabolism and decreasing body weight (Zhang et al. 2007). Capsaicin is a highly selective agonist for the transient receptor potential vanilloid type 1 (TRPV1) cation channel (Caterina et al. 1997), which is reported to exert important effects on cardiovascular system by increasing evidence (Gupta et al. 2007; Pacher et al. 2004). TRPV1 activation protects the heart from ischemia/reperfusion injury (Zhong and Wang 2007, 2008) and prevents ischemia/reperfusion-induced kidney injury (Rayamajhi et al. 2009). TRPV1 activation systemically can also reduce the blood pressure via promoting vasodilation (Franco-Cereceda and Rudehill 1989; Li and Wang 2003a; Scotland et al. 2004; Li and Wang 2003b; Kawasaki et al. 2011). Yang et al. (2010) demonstrated that TRPV1 activation in endothelial cells improves endothelium-dependent vasorelaxation and prevents hypertension. In addition, Ma’s study (Ma et al. 2011) indicated the essential role of TRPV1 in regulating VSMC function. They found that TRPV1 activation in VSMCs by capsaicin can reduce the cholesterol uptake and promote its efflux and ultimately inhibit the cellular lipid accumulation. In the present study, we investigated whether TRPV1 activation by capsaicin can regulate VSMC plasticity and ameliorate intracranial arteriole remodeling in hypertension, in an aim to clarify the potential therapeutic promise of capsaicin/TRPV1 for hypertension.
Materials and methods
Reagents
High-glucose Dulbecco’s modified Eagle’s medium (DMEM), fetal bovine serum (FBS), trypsin and phosphate buffer saline (PBS) were obtained from Hyclone (Logan, UT, USA). Capsaicin, 5′-iodoresiniferatoxin (iRTX) and LY294002 were purchased from Sigma-Aldrich (St. Louis, MO, USA). The deoxycorticosterone acetate (DOCA) pellets were purchased from Innovative Research of America (Sarasota, FL, USA). SDS-PAGE gel preparation kit and BCA protein assay kit were from Beyotime Institute of Biotechnology (Jiangsu, China). Cell Counting Kit-8 (CCK-8) was from Dojindo Laboratories (Mashiki-machi, Kumamoto, Japan). Antibodies targeting α-smooth muscle actin (α-SMA, ab32575), SM22α (ab14106) and osteopontin (OPN, ab8448) were from Abcam (Burlingame, CA, USA). Antibodies against phosphorylated-Akt (p-Akt, No. 12178) and total-Akt (No. 8596) were purchased from Cell Signaling Technology (Beverly, MA, USA). Antibody targeting GAPDH (TA-08) and secondary antibodies (ZB-5301, ZB-2305) were purchased from Zhongshan Golden Bridge Biotechnology (Beijing, China).
Animal treatment
Fifteen TRPV1−/− mice were obtained at eight–ten weeks of age from Jackson Laboratory (Bar Harbor, ME, USA). Fifteen eight-week-old male spontaneously hypertensive rats (SHR) and ten age-matched normotensive Wistar–Kyoto (WKY) control rats were obtained from Charles Rivers Laboratories (Beijing, China). DOCA-salt hypertensive mouse model was established with reference to a previous study (Perez-Rivera et al. 2005). Briefly, ten mice received unilateral nephrectomy under anesthesia using pentobarbital sodium. A DOCA pellet was implanted subcutaneously through a 1-cm incision between the shoulder blades. DOCA mice were given drinking water containing 1 % NaCl and 0.2 % KCl. Five sham mice also underwent unilateral nephrectomy, but no DOCA pellet implantation and were given tap water. After surgery, these mice were housed under standard conditions for 3 weeks. Animals were randomly assigned to receive the normal standard chow (control group), or normal chow plus with 0.01 % capsaicin for mice and 0.02 % capsaicin for rats (capsaicin group).
Ethics statement
This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals. Protocol approval was obtained from the Animal Research Committee of the Third Military Medical University. All surgery was performed under sodium pentobarbital anesthesia, and all efforts were made to minimize suffering.
Histopathology
After drug intervention, rats and mice were killed, and aortas, carotid arteries, mesenteric small arteries and brains were removed and perfusion fixed with 4 % paraformaldehyde. Perfusion-fixed samples were embedded in paraffin, cut transversely into 5-μm-thick sections and stained with hematoxylin and eosin (HE). Tissue slices were photographed and recorded using the Tissue Gnostics microscope (Zeiss, Oberkochen, Germany).
Cell culture
Rat VSMCs were isolated from thoracic aorta at 8–10 weeks of age using an explant method described previously (McMurray et al. 1991). The adventitia and intima were dissected from medial layer, and cells were grown from the medial layer explants in high-glucose DMEM with 10 % FBS, 100 U/mL penicillin and 100 μg/mL streptomycin (Hyclone, USA). When cell were grown to 70–80 % confluence, the explants were removed and the VSMCs were cultured in high-glucose DMEM containing 10 % FBS and antibiotics in the cell incubator containing 5 % CO2 and 95 % air at 37 °C. The cells were verified as VSMCs through immunofluorescent staining of smooth muscle (SM) specific marker, α-SMA. VSMCs at passages 3–10 were used in our experiments. In subsequent cell experiment in vitro, the concentration of TRPV1 agonist capsaicin and antagonist iRTX in cell culture media was both 1 μM, while PI3K inhibitor LY294002 was 25 μM.
Cell proliferation assay
A Cell Counting Kit-8 (CCK-8) was used to measure the proliferative capacity of VSMCs. VSMCs were seeded into a 96-well plate (5 × 103 cells/well) and cultured in DMEM containing 10 % FBS. After cell adherence and hunger, different drug treatments were added in the wells for 24 h in cell incubator. Then, 10 μL CCK-8 solution was added to the culture medium, and the cells were continued to incubate for 1 h. Light absorbance at 450 nm was measured using a Microplate Reader (Bio-Rad, Hercules, CA, USA).
Cell migration assay
Cell migration was examined using modified Boyden chambers as described in our previous studies (Zhang et al. 2010, 2011). DMEM containing 10 % FBS was added to the lower section of the Boyden chambers, and VSMCs suspended in FBS-free DMEM (5.0 × 104 cells/mL) were added to the upper section of the Boyden chambers. After incubation for 4 h at 37 °C, the upside of the filters was scraped and washed with PBS. Cells on the underside of the filters were fixed with 4 % paraformaldehyde and stained with DAPI (4,6-diamino-2-phenyl indole). Finally, cells were photographed and counted from five high-power (×400) fields per well. The average was used as the number of migrating cell.
Real-time PCR
Total RNA was extracted from cultured VSMCs using RNAiso Plus (Takara Bio, Otsu, Japan). Each sample was mixed with the genomic DNA (gDNA) Eraser to remove gDNA. The complementary DNA (cDNA) was obtained by reverse-transcription PCR using PrimeScript™ RT reagent Kit (Takara Bio, Otsu, Japan), following the manufacturer’s instructions. Real-time PCR was carried out with SYBR Premix Ex Taq™ II (Takara Bio, Otsu, Japan) on a CFX96 Real-Time System (Bio-Rad, Hercules, CA, USA) for IL-1β, IL-6, TNFα and MCP-1, with β-actin or GAPDH as control. And the primers for these genes are shown in Table 1. The target gene expression level was normalized to β-actin or GAPDH, and the result was presented as a fold change by using the formula 2−ΔΔCt.
Western blot analysis
Cells in 6-well plate were washed with ice-cold PBS, scraped by lysis buffer (with phenylmethanesulfonyl fluoride, PMSF) and centrifuged. The supernatant was then collected, namely protein solution. Protein concentration was determined by BCA protein assay kit. Protein samples as well as SDS-loading buffer were separated by SDS-PAGE and transferred to PVDF membranes (Bio-Rad, Hercules, CA, USA). After blocked in TBS containing 0.05 % Tween-20 and 5 % nonfat milk powder for 4 h at room temperature, the PVDF membranes were subjected to immunoblotting using antibodies to α-SMA (1:1000), SM22α (1:1000), OPN (1:1000), p-Akt (1:1000), total-Akt (1:1000), GAPDH (1:2000) and secondary antibodies (1:3000). Protein bands in PVDF membranes were detected using extended duration substrate kit (Thermo Scientific, Waltham, MA, USA) and quantified by Labworks 4.6 (UVP, Upland, CA, USA). The expression level of the various proteins was normalized to GAPDH.
PI3K activity assay
The PI3K activity of VSMCs was measured using an enzyme-linked immunosorbent assay (ELISA) kit according to the manufacturer’s instructions and previous studies (Zhang et al. 2010).
Statistical analysis
Results are expressed as mean ± standard deviation (SD). Statistical difference between two groups was assessed by a paired t test, while differences among three or more groups were determined with a one-way analysis of variance with Newman–Keuls post hoc test using GraphPad Prism 6 software (La Jolla, CA, USA). A p value <0.05 was considered to be statistically significant.
Results
Hypertension-induced arterial remodeling and VSMC phenotypic modulation
To detect the arterial remodeling in hypertension, histopathological sections of vessels from hypertensive SHR and age-matched normotensive WKY control rats were used. As shown in Fig. 1a, vessels from SHR showed significant remodeling compared with those from WKY, mainly characterized by increased lumen diameter in aorta, thickened intima-media, disorganized VSMCs and elastic fibers in carotid artery, thickened vessel wall with hyaline change and stenotic or occluded lumen in mesenteric small artery and intracranial arterioles. These data indicate global arterial remodeling in hypertension, with distinct changes in different levels of arteries.
Hypertension-induced arterial remodeling and VSMC phenotypic modulation, a hematoxylin and eosin staining on cross sections from different levels of arteries are presented. Vessels from SHR showed significant remodeling compared with those from WKY, mainly characterized by increased lumen diameter in aorta, thickened intima-media, disorganized VSMCs and elastic fibers in carotid artery, thickened vessel wall with hyaline change and stenotic or occluded lumen in mesenteric small artery and intracranial arterioles. b As detected by Western blot, α-SMA and SM22α were markedly decreased, while OPN was markedly increased in SHR aorta (n = 5) compared with those in WKY (n = 5). * p < 0.05. Results are expressed as mean ± standard deviation (SD) of three independent experiments
To clarify whether VSMCs in vivo underwent phenotypic modulation during hypertension, we tested the expression of several proteins in aorta those widely accepted as specific markers of different VSMC phenotypes. Of those, α-SMA and SM22α express in contractile phenotype, and OPN expresses specifically in synthetic phenotype. As shown in Fig. 1b, α-SMA and SM22α were markedly decreased, while OPN was markedly increased in SHR aorta compared with those in WKY. These data indicate the transformation of VSMC from contractile to synthetic phenotype in hypertension, which may responsible for the arterial remodeling.
VSMCs derived from SHR showed activated inflammatory status
Phenotypic modulation was further detected in vitro in cultured VSMCs derived from SHR and WKY aorta. Consistent with the results from in vivo, SHR-derived VSMCs showed reduced expression of α-SMA and SM22α and increased expression of OPN compared with WKY-derived VSMCs (Fig. 2a). Hypertension has been accepted as a form of low-grade systemic inflammation, accompanied by secretion of various inflammatory mediators and activation of inflammatory signals. VSMCs can produce cytokines that attract and activate leukocytes, induce proliferation of VSMCs and promote expression of extracellular matrix components to aggravate inflammatory response and stimulate vascular lesions (Doran et al. 2008). Herein, we detected the inflammatory status of cultured SHR aortic VSMCs. As shown in Fig. 2b, compared with WKY-derived cells, the SHR-derived VSMCs showed increased mRNA expression of inflammatory factors including IL-1β, IL-6, TNFα and MCP-1. These data suggest that VSMCs derived from SHR show phenotypic modulation along with activated inflammatory status.
VSMCs derived from SHR showed activated inflammatory status, a primary VSMCs from SHR showed reduced protein expression of α-SMA and SM22α and increased expression of OPN compared with WKY-derived VSMCs detected by Western blot. b Compared with WKY-derived cells, the SHR-derived VSMCs showed increased mRNA expression of inflammatory factors including IL-1β, IL-6, TNFα and MCP-1. n = 1 rat (SHR/WKY) per primary VSMC culture (5 in total). * p < 0.05. Results are expressed as mean ± standard deviation (SD) of three independent experiments
TRPV1 activation inhibited phenotypic modulation of VSMCs derived from SHR
TRPV1, a nonselective cation channel of the TRP subfamily, can be activated by capsaicin and exert protective role against cardiovascular and cerebrovascular diseases. Recently, it has been reported that the effect of TRPV1 against hypertension was partly attributed to the improved action of VSMCs (Zhang et al. 2015). To investigate whether activation of TRPV1 inhibits VSMC phenotypic modulation during hypertension, we used capsaicin to activate TRPV1 and tested the further effects on the marker protein and inflammatory factor expression, proliferative and migratory capacities in SHR-derived VSMCs.
As shown in Fig. 3a, capsaicin significantly increased expression of α-SMA and SM22α and reduced expression of OPN, which was counteracted by TRPV1 antagonist iRTX combined with capsaicin in VSMCs from SHR. The same regulative tendency by capsaicin and iRTX was also detected in WKY-derived VSMCs, but the differences were not statistically significant. As shown in Fig. 3b and c, compared to WKY-derived VSMCs, SHR-derived VSMCs showed increased proliferative and migratory capacities, which were significantly retarded by TRPV1 agonist capsaicin. However, TRPV1 antagonist iRTX combined with capsaicin further facilitated the proliferation and migration in SHR-VSMCs. Besides, capsaicin also inhibited the proliferation and migration of WKY-VSMC. These data indicate that TRPV1 activation protected VSMCs from phenotypic switching in hypertension.
TRPV1 activation inhibited phenotypic modulation of VSMCs derived from SHR, a as detected by Western blot, capsaicin (cap, 1 μM) significantly increased expression of α-SMA and SM22α and reduced expression of OPN, which was counteracted by TRPV1 antagonist iRTX (1 μM) combined with capsaicin in VSMCs from SHR. The same regulative tendency by capsaicin and iRTX was also detected in WKY-derived VSMCs, but the differences were not statistically significant. b, c Compared to WKY-derived VSMCs, SHR-derived VSMCs showed increased proliferative and migratory capacities, which were significantly retarded by TRPV1 agonist capsaicin (1 μM). However, TRPV1 antagonist iRTX (1 μM) combined with capsaicin further facilitated the proliferation and migration in SHR-VSMCs. Besides, capsaicin also inhibited the proliferation and migration of WKY-VSMC. d The upregulated inflammatory factors including IL-1β, IL-6, TNFα and MCP-1 in SHR-derived VSMCs were significantly inhibited by TRPV1 agonist capsaicin (1 μM), while TRPV1 antagonist iRTX (1 μM) combined with capsaicin further increased the mRNA expression of these inflammatory factors. Moreover, TRPV1 antagonist iRTX could increase the inflammatory factor expression even in WKY-VSMCs. n = 1 rat (SHR/WKY) per primary VSMC culture (5 in total). * p < 0.05 versus WKY-VSMC control (con); #p < 0.05 versus SHR-VSMC control. Results are expressed as mean ± standard deviation (SD) of three independent experiments
Next, we further tested the effect of TRPV1 on inflammatory factor expression in VSMCs. As shown in Fig. 3d, the upregulated inflammatory factors including IL-1β, IL-6, TNFα and MCP-1 in SHR-derived VSMCs were significantly inhibited by TRPV1 agonist capsaicin, while TRPV1 antagonist iRTX combined with capsaicin further increased the mRNA expression of these inflammatory factors. Moreover, TRPV1 antagonist iRTX could increase the inflammatory factor expression even in WKY-VSMCs. Collectively, these data suggest that TRPV1 activation can inhibit the proinflammatory phenotype of VSMCs induced by hypertension.
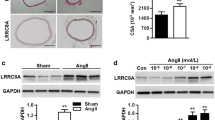
TRPV1 activation ameliorated intracranial arteriole remodeling in hypertension
Furthermore, we investigated the effect of TRPV1 activation by capsaicin on intracranial arteriole remodeling in hypertension in vivo. Previous study found that dietary capsaicin could significantly decrease the intima-media thickness of intracranial arterioles in stroke-prone SHR, indicating the role of capsaicin in improving cerebrovascular remodeling in hypertension (Xu et al. 2011). Consistently, the present study showed that capsaicin diet ameliorated the hypertrophic and inward remodeling of intracranial arterioles in SHR (Fig. 4a). DOCA-salt hypertensive mouse model is another important and commonly used in hypertension research (Zhao et al. 2015). Compared with untreated TRPV1−/− mice, DOCA-salt-treated TRPV1−/− mice showed thickened vessel wall with hyaline change and stenotic or occluded lumen in cerebral arterioles, suggesting inward remodeling induced by hypertension. However, the attenuation of arteriole remodeling by capsaicin was not observed in TRPV1−/− mice, as that occurred in SHR with intact TRPV1 (Fig. 4b). These data indicate that capsaicin ameliorated intracranial arteriole remodeling in hypertension through activating TRPV1 and highlight the potential promise of TRPV1 for preventing or delaying the vascular damage in hypertension.
TRPV1 activation ameliorated intracranial arteriole remodeling in hypertension, a capsaicin (cap) diet ameliorated the hypertrophic and inward remodeling of intracranial arterioles in SHR. b Compared with untreated TRPV1−/− mice (n = 5), DOCA-salt-treated TRPV1−/− mice (n = 5) showed thickened vessel wall with hyaline change and stenotic or occluded lumen in cerebral arterioles, suggesting inward remodeling induced by hypertension. However, the attenuation of arteriole remodeling by capsaicin was not observed in TRPV1−/− mice (n = 5), as that occurred in SHR with intact TRPV1
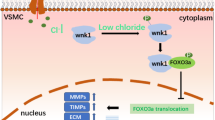
TRPV1 inhibited VSMC phenotypic modulation through suppressing PI3K/Akt pathway
Phosphatidylinositol 3 kinase/protein kinase B (PI3K/Akt) signaling pathway plays a major role in VSMC phenotypic modulation. Reportedly, enhanced PI3K/Akt signaling induced the VSMC phenotypic modulation, characterized by upregulation of a series of cytokines and decrease in SM markers (Furgeson et al. 2010). Our previous study has found that VSMCs derived from SHR showed significantly activated PI3K/Akt signaling; PI3K inhibitor LY294002 impeded phenotypic modulation of cultured VSMCs derived from SHR, as evidenced by rescuing the α-SMA and SM22α expression and counteracting the proliferative and migratory capacities (Zhang et al. 2010). In the present study, it was found that the mRNA expression of inflammatory factors including IL-1β, IL-6 and TNFα in SHR-derived VSMCs was reduced by PI3K inhibitor LY294002, as shown in Fig. 5a. These data suggest that inhibition of PI3K signaling could inhibit the inflammatory reaction of SHR-derived VSMCs. To further investigate the potential mechanisms of TRPV1 in regulating VSMC phenotype, we analyzed the activation status of PI3K/Akt signaling. As shown in Fig. 5b, the activity of PI3K and phosphorylation level of Akt in SHR-derived VSMCs were higher than those in WKY-derived VSMCs. Capsaicin treatment significantly decreased the activity of PI3K and phosphorylation level of Akt in SHR-derived VSMCs, which was reversed by TRPV1 antagonist iRTX. It is suggested that TRPV1 activation inhibits phenotypic modulation of VSMCs through, at least partly, suppressing PI3K/Akt signaling pathway.
TRPV1 inhibited VSMC phenotypic modulation through suppressing PI3K/Akt pathway, a the mRNA expression of inflammatory factors including IL-1β, IL-6 and TNFα in SHR-derived VSMCs were reduced by PI3K inhibitor LY294002 (25 μM). b As detected by PI3K Activity Assay and Western blot, the activity of PI3K and phosphorylation level of Akt in SHR-derived VSMCs were higher than those in WKY-derived VSMCs. Capsaicin (cap, 1 μM) treatment significantly decreased the activity of PI3K and phosphorylation level of Akt in SHR-derived VSMCs, which was reversed by TRPV1 antagonist iRTX (1 μM). n = 1 rat (SHR/WKY) per primary VSMC culture (5 in total). * p < 0.05 versus WKY; #p < 0.05 versus SHR. Results are expressed as mean ± standard deviation (SD) of three independent experiments
Discussion
Hypertension affects about one-third of adults worldwide and is responsible for about half the global risk for stroke and ischemic heart disease (Levy et al. 2009). Hypertension-induced arterial remodeling and the consequent atherosclerosis and arteriolosclerosis are the major contributor to the cardiac-cerebral vascular diseases. In the present study, hypertension induced global arterial remodeling, although the modes of remodeling were different in different levels of arteries. Large artery mainly displayed outward remodeling, with increased lumen diameter in aorta. In contrast, middle and small arteries showed significant inward remodeling. Carotid artery showed thickened intima-media, decreased lumen diameter and disorganized VSMCs and elastic fibers, while mesenteric small artery and intracranial arterioles displayed thickened vessel wall with hyaline change and stenotic or occluded lumen.
Although complicated processes and various cells in vessel wall are involved in the arterial remodeling in hypertension, phenotypic modulation of contractile VSMCs is widely accepted as the pivotal process. VSMCs within mature blood vessels play dominant role in regulating vascular contraction and dilation. Unlike either skeletal or cardiac muscle cells that are terminally differentiated, VSMCs retain remarkable plasticity and can undergo phenotypic modulation from contractile to synthetic phenotype in response to local environmental changes such as arterial injury and hypertension (Owens et al. 2004). Accumulating evidence suggests that inappropriate or excessive VSMC phenotypic modulation promotes vascular remodeling including media hypertrophy, neointimal hyperplasia and extracellular matrix deposition (Lee et al. 2015; Kudryavtseva et al. 2014). Therefore, the attenuation or inhibition of VSMC phenotypic modulation may display the protective function against intracranial arteriole remodeling in hypertension.
In the present study, both SHR aorta VSMCs and cultured VSMCs derived from SHR underwent phenotypic modulation, evidenced by decreased expression of SM contractile proteins (α-SMA and SM22α) and increased expression of SM synthetic protein (OPN). SHR-derived VSMCs also showed increased proliferative and migratory capacities in vitro. In addition, activated inflammatory status was observed in SHR-VSMCs, evidenced by increased mRNA expression of inflammatory factors including IL-1β, IL-6, TNFα and MCP-1. These results indicate that VSMCs showed proinflammatory phenotypic modulation during hypertension, paralleled with changed SM protein expression and increased viability, which synergistically promote the arterial remodeling in hypertension.
The capsaicin receptor TRPV1 is a ligand-gated and non-selective calcium influx channel which was isolated and cloned from sensory neurons (Caterina et al. 1997). TRPV1 is widely distributed in peripheral nervous system such as dorsal root ganglion neurons and colon to mediate various types of pain (Zhu et al. 2011; Chen et al. 2015; Fang et al. 2015). TRPV1 is also widely expressed in the central nervous system to control learning and memory, which may be the novel research target for mitigation of Alzheimer’s disease and Parkinson’s disease (Palazzo et al. 2008; Zschenderlein et al. 2011; Jayant et al. 2016; Nam et al. 2015). Besides, growing evidence indicates the protective role of TRPV1 in cardiac-cerebral vascular system. Previous study found that chronic dietary capsaicin ameliorated cerebrovascular hypertrophy and intima-media thickening of intracranial arterioles in stroke-prone SHR, which was associated with enhanced eNOS level and endothelium-dependent relaxation (Xu et al. 2011). We have reported that TRPV1 activation by capsaicin impeded VSMC-derived foam cell formation and further inhibited vascular atherosclerosis (Li et al. 2014). Although arterial remodeling is commonly initiated by intimal injury in the early stage, VSMCs are primarily involved in the vascular structure changes and are the main contributor to forming vascular hypertrophy trough proliferating and migrating (Zhang et al. 2011). Therefore, we tested the effect of TRPV1 on intracranial arterioles and cultured VSMCs in hypertensive animals in the present study. It was shown that TRPV1 activation by capsaicin inhibited the VSMC phenotypic modulation by increasing expression of α-SMA and SM22α, reducing expression of OPN and retarding the proliferative and migratory capacities in SHR-derived VSMCs. Furthermore, we found that capsaicin diet retarded the hypertrophic and inward remodeling in intracranial arterioles in SHR but not in hypertensive mice with impaired TRPV1, indicating the pivotal role of TRPV1 in attenuating arterial remodeling in hypertension.
VSMC proinflammatory phenotypic modulation is also a critical process during hypertension. However, rare literature reported the anti-inflammatory effects of TRPV1 on VSMCs. Previous studies showed that TRPV1 activation by capsaicin reduced inflammatory responses by decreasing the expression of TNFα, IL-6 and MCP-1, prevented macrophage infiltration in adipose tissue, inhibited differentiation, activation and pro-inflammatory cytokine production of dendritic cells (Kang et al. 2010; Toth et al. 2009). Additionally, TRPV1 gene deletion resulted in excessive inflammation and aggravated abnormal tissue remodeling after myocardial ischemia (Huang et al. 2009) and accelerated TGFβ-induced renal fibrosis in DOCA-salt hypertension (Wang and Wang 2011). In the present study, it was found that TRPV1 activation by capsaicin significantly inhibited the upregulated inflammatory factors including IL-1β, IL-6, TNFα and MCP-1 in SHR-derived VSMCs. Hence, these data suggest that TRPV1 activation by capsaicin inhibits VSMC phenotypic modulation as well as the paralleled inflammatory status, through which TRPV1 exerts inhibitory effect on intracranial arteriole remodeling induced by hypertension.
Regarding the molecular mechanism that involved in TRPV1-inhibited VSMC phenotypic modulation, we particularly focused on the role of PI3K/Akt pathway. PI3K/Akt has been demonstrated to be essential for VSMC proliferation and migration (Fernandez-Hernando et al. 2009). In addition, the proinflammatory effects of PI3K/Akt are associated with the enhanced nuclear localization and activation of NF-κB (Furgeson et al. 2010). In the present study, it was found that the mRNA expression of inflammatory factors including IL-1β, IL-6 and TNFα in SHR-derived VSMCs was reduced by PI3K inhibitor LY294002, suggesting the important inhibitory effect of PI3K on VSMC inflammation. The activity of PI3K and phosphorylation level of Akt in SHR-derived VSMCs were higher than those in WKY-derived VSMCs, indicating increased PI3K/Akt signaling pathway, which was counteracted by TRPV1 activation by capsaicin. These data suggest that TRPV1 activation inhibits phenotypic modulation of VSMCs through, at least partly, suppressing PI3K/Akt signaling pathway.
Taken together, we provide evidence that TRPV1 activation by capsaicin attenuates intracranial arteriole remodeling through inhibiting VSMC phenotypic modulation during hypertension, which may be at least partly attributed to the suppression PI3K/Akt signaling pathway. These findings highlight the prospect of TRPV1 in prevention and treatment of hypertension.
References
Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D (1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389(6653):816–824. doi:10.1038/39807
Chen K, Zhang Z-F, Liao M-F, Yao W-L, Wang J, Wang X-R (2015) Blocking PAR2 attenuates oxaliplatin-induced neuropathic pain via TRPV1 and releases of substance P and CGRP in superficial dorsal horn of spinal cord. J Neurol Sci 352(1):62–67. doi:10.1016/j.jns.2015.03.029
Doran AC, Meller N, McNamara CA (2008) Role of smooth muscle cells in the initiation and early progression of atherosclerosis. Arterioscler Thromb Vasc Biol 28(5):812–819. doi:10.1161/ATVBAHA.107.159327
Fang D, Kong LY, Cai J, Li S, Liu XD, Han JS, Xing GG (2015) Interleukin-6-mediated functional upregulation of TRPV1 receptors in dorsal root ganglion neurons through the activation of JAK/PI3K signaling pathway: roles in the development of bone cancer pain in a rat model. Pain 156(6):1124–1144. doi:10.1097/j.pain.0000000000000158
Farb A, Kolodgie FD, Hwang JY, Burke AP, Tefera K, Weber DK, Wight TN, Virmani R (2004) Extracellular matrix changes in stented human coronary arteries. Circulation 110(8):940–947. doi:10.1161/01.CIR.0000139337.56084.30
Fernandez-Hernando C, Jozsef L, Jenkins D, Di Lorenzo A, Sessa WC (2009) Absence of Akt1 reduces vascular smooth muscle cell migration and survival and induces features of plaque vulnerability and cardiac dysfunction during atherosclerosis. Arterioscler Thromb Vasc Biol 29(12):2033–2040. doi:10.1161/ATVBAHA.109.196394
Franco-Cereceda A, Rudehill A (1989) Capsaicin-induced vasodilatation of human coronary arteries in vitro is mediated by calcitonin gene-related peptide rather than substance P or neurokinin A. Acta Physiol Scand 136(4):575–580. doi:10.1111/j.1748-1716.1989.tb08704.x
Furgeson SB, Simpson PA, Park I, Vanputten V, Horita H, Kontos CD, Nemenoff RA, Weiser-Evans MC (2010) Inactivation of the tumour suppressor, PTEN, in smooth muscle promotes a pro-inflammatory phenotype and enhances neointima formation. Cardiovasc Res 86(2):274–282. doi:10.1093/cvr/cvp425
Gupta S, Lozano-Cuenca J, Villalon CM, de Vries R, Garrelds IM, Avezaat CJ, van Kats JP, Saxena PR, MaassenVanDenBrink A (2007) Pharmacological characterisation of capsaicin-induced relaxations in human and porcine isolated arteries. Naunyn Schmiedeberg’s Arch Pharmacol 375(1):29–38. doi:10.1007/s00210-007-0137-y
Huang W, Rubinstein J, Prieto AR, Thang LV, Wang DH (2009) Transient receptor potential vanilloid gene deletion exacerbates inflammation and atypical cardiac remodeling after myocardial infarction. Hypertension 53(2):243–250. doi:10.1161/HYPERTENSIONAHA.108.118349
Jayant S, Sharma BM, Sharma B (2016) Protective effect of transient receptor potential vanilloid subtype 1 (TRPV1) modulator, against behavioral, biochemical and structural damage in experimental models of Alzheimer’s disease. Brain Res 1642:397–408. doi:10.1016/j.brainres.2016.04.022
Kang JH, Goto T, Han IS, Kawada T, Kim YM, Yu R (2010) Dietary capsaicin reduces obesity-induced insulin resistance and hepatic steatosis in obese mice fed a high-fat diet. Obesity 18(4):780–787. doi:10.1038/oby.2009.301
Kawasaki H, Takatori S, Zamami Y, Koyama T, Goda M, Hirai K, Tangsucharit P, Jin X, Hobara N, Kitamura Y (2011) Paracrine control of mesenteric perivascular axo-axonal interaction. Acta Physiol (Oxf) 203(1):3–11. doi:10.1111/j.1748-1716.2010.02197.x
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J (2005) Global burden of hypertension: analysis of worldwide data. Lancet 365(9455):217–223. doi:10.1016/s0140-6736(05)17741-1
Kudryavtseva O, Herum KM, Dam VS, Straarup MS, Kamaev D, Briggs Boedtkjer DM, Matchkov VV, Aalkjær C (2014) Downregulation of L-type Ca2 + channel in rat mesenteric arteries leads to loss of smooth muscle contractile phenotype and inward hypertrophic remodeling. Am J Physiol Heart Circ Physiol 306(9):H1287–H1301
Lee TH, Sottile J, Chiang HY (2015) Collagen inhibitory peptide R1R2 mediates vascular remodeling by decreasing inflammation and smooth muscle cell activation. PLoS ONE 10(2):e0117356. doi:10.1371/journal.pone.0117356
Levy D, Ehret GB, Rice K, Verwoert GC, Launer LJ, Dehghan A, Glazer NL, Morrison AC, Johnson AD, Aspelund T, Aulchenko Y, Lumley T, Kottgen A, Vasan RS, Rivadeneira F, Eiriksdottir G, Guo X, Arking DE, Mitchell GF, Mattace-Raso FU, Smith AV, Taylor K, Scharpf RB, Hwang SJ, Sijbrands EJ, Bis J, Harris TB, Ganesh SK, O’Donnell CJ, Hofman A, Rotter JI, Coresh J, Benjamin EJ, Uitterlinden AG, Heiss G, Fox CS, Witteman JC, Boerwinkle E, Wang TJ, Gudnason V, Larson MG, Chakravarti A, Psaty BM, van Duijn CM (2009) Genome-wide association study of blood pressure and hypertension. Nat Genet 41(6):677–687. doi:10.1038/ng.384
Li J, Wang DH (2003a) Function and regulation of the vanilloid receptor in rats fed a high salt diet. J Hypertens 21(8):1525–1530. doi:10.1097/01.hjh.0000084709.87421.98
Li J, Wang DH (2003b) High-salt-induced increase in blood pressure: role of capsaicin-sensitive sensory nerves. J Hypertens 21(3):577–582. doi:10.1097/01.hjh.0000052465.40108.35
Li BH, Yin YW, Liu Y, Pi Y, Guo L, Cao XJ, Gao CY, Zhang LL, Li JC (2014) TRPV1 activation impedes foam cell formation by inducing autophagy in oxLDL-treated vascular smooth muscle cells. Cell Death Dis 5:e1182. doi:10.1038/cddis.2014.146
Ma L, Zhong J, Zhao Z, Luo Z, Ma S, Sun J, He H, Zhu T, Liu D, Zhu Z, Tepel M (2011) Activation of TRPV1 reduces vascular lipid accumulation and attenuates atherosclerosis. Cardiovasc Res 92(3):504–513. doi:10.1093/cvr/cvr245
McMurray HF, Parrott DP, Bowyer DE (1991) A standardised method of culturing aortic explants, suitable for the study of factors affecting the phenotypic modulation, migration and proliferation of aortic smooth muscle cells. Atherosclerosis 86(2–3):227–237. doi:10.1016/0021-9150(91)90219-S
Nam JH, Park ES, Won SY, Lee YA, Kim KI, Jeong JY, Baek JY, Cho EJ, Jin M, Chung YC, Lee BD, Kim SH, Kim EG, Byun K, Lee B, Woo DH, Lee CJ, Kim SR, Bok E, Kim YS, Ahn TB, Ko HW, Brahmachari S, Pletinkova O, Troconso JC, Dawson VL, Dawson TM, Jin BK (2015) TRPV1 on astrocytes rescues nigral dopamine neurons in Parkinson’s disease via CNTF. Brain 138(Pt 12):3610–3622. doi:10.1093/brain/awv297
Owens GK, Kumar MS, Wamhoff BR (2004) Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev 84(3):767–801
Pacher P, Batkai S, Kunos G (2004) Haemodynamic profile and responsiveness to anandamide of TRPV1 receptor knock-out mice. J Physiol 558(Pt 2):647–657. doi:10.1113/jphysiol.2004.064824
Palazzo E, Rossi F, Maione S (2008) Role of TRPV1 receptors in descending modulation of pain. Mol Cell Endocrinol 286(Suppl 1):S79–83. doi:10.1016/j.mce.2008.01.013
Perez-Rivera AA, Fink GD, Galligan JJ (2005) Vascular reactivity of mesenteric arteries and veins to endothelin-1 in a murine model of high blood pressure. Vascul Pharmacol 43(1):1–10. doi:10.1016/j.vph.2005.02.014
Rayamajhi S, Contractor T, Wang DH (2009) The potential of TRPV1 agonists for treating ischemia/reperfusion-induced renal injuries. Curr Opin Investig Drugs 10(9):963–970
Scotland RS, Chauhan S, Davis C, De Felipe C, Hunt S, Kabir J, Kotsonis P, Oh U, Ahluwalia A (2004) Vanilloid receptor TRPV1, sensory C-fibers, and vascular autoregulation: a novel mechanism involved in myogenic constriction. Circ Res 95(10):1027–1034. doi:10.1161/01.RES.0000148633.93110.24
Toth BI, Benko S, Szollosi AG, Kovacs L, Rajnavolgyi E, Biro T (2009) Transient receptor potential vanilloid-1 signaling inhibits differentiation and activation of human dendritic cells. FEBS Lett 583(10):1619–1624. doi:10.1016/j.febslet.2009.04.031
Wang Y, Wang DH (2011) Protective effect of TRPV1 against renal fibrosis via inhibition of TGF-beta/Smad signaling in DOCA-salt hypertension. Mol Med 17(11–12):1204–1212. doi:10.2119/molmed.2011.00063
Xu X, Wang P, Zhao Z, Cao T, He H, Luo Z, Zhong J, Gao F, Zhu Z, Li L, Yan Z, Chen J, Ni Y, Liu D, Zhu Z (2011) Activation of transient receptor potential vanilloid 1 by dietary capsaicin delays the onset of stroke in stroke-prone spontaneously hypertensive rats. Stroke 42(11):3245–3251. doi:10.1161/strokeaha.111.618306
Yang D, Luo Z, Ma S, Wong WT, Ma L, Zhong J, He H, Zhao Z, Cao T, Yan Z, Liu D, Arendshorst WJ, Huang Y, Tepel M, Zhu Z (2010) Activation of TRPV1 by dietary capsaicin improves endothelium-dependent vasorelaxation and prevents hypertension. Cell Metab 12(2):130–141. doi:10.1016/j.cmet.2010.05.015
Zhang LL, Liu DY, Ma LQ, Luo ZD, Cao TB, Zhong J, Yan ZC, Wang LJ, Zhao ZG, Zhu SJ, Schrader M, Thilo F, Zhu ZM, Tepel M (2007) Activation of transient receptor potential vanilloid type-1 channel prevents adipogenesis and obesity. Circ Res 100(7):1063–1070. doi:10.1161/01.RES.0000262653.84850.8b
Zhang L, Xie P, Wang J, Yang Q, Fang C, Zhou S, Li J (2010) Impaired peroxisome proliferator-activated receptor-gamma contributes to phenotypic modulation of vascular smooth muscle cells during hypertension. J Biol Chem 285(18):13666–13677. doi:10.1074/jbc.M109.087718
Zhang LL, Gao CY, Fang CQ, Wang YJ, Gao D, Yao GE, Xiang J, Wang JZ, Li JC (2011) PPARgamma attenuates intimal hyperplasia by inhibiting TLR4-mediated inflammation in vascular smooth muscle cells. Cardiovasc Res 92(3):484–493. doi:10.1093/cvr/cvr238
Zhang M-J, Yin Y-W, Li B-H, Liu Y, Liao S-Q, Gao C-Y, Li J-C, Zhang L-L (2015) The role of TRPV1 in improving VSMC function and attenuating hypertension. Prog Biophys Mol Biol 117(2–3):212–216. doi:10.1016/j.pbiomolbio.2015.03.004
Zhao Q, Zhang J, Wang H (2015) PGC-1α overexpression suppresses blood pressure elevation in DOCA-salt hypertensive mice. Biosci Rep 35(3):e00217. doi:10.1042/bsr20150076
Zhong B, Wang DH (2007) TRPV1 gene knockout impairs preconditioning protection against myocardial injury in isolated perfused hearts in mice. Am J Physiol Heart Circ Physiol 293(3):H1791–1798. doi:10.1152/ajpheart.00169.2007
Zhong B, Wang DH (2008) N-oleoyldopamine, a novel endogenous capsaicin-like lipid, protects the heart against ischemia-reperfusion injury via activation of TRPV1. Am J Physiol Heart Circ Physiol 295(2):H728–735. doi:10.1152/ajpheart.00022.2008
Zhu Y, Colak T, Shenoy M, Liu L, Pai R, Li C, Mehta K, Pasricha PJ (2011) Nerve growth factor modulates TRPV1 expression and function and mediates pain in chronic pancreatitis. Gastroenterology 141(1):370–377. doi:10.1053/j.gastro.2011.03.046
Zschenderlein C, Gebhardt C, und Halbach OVB, Kulisch C, Albrecht D (2011) Capsaicin-induced changes in LTP in the lateral amygdala are mediated by TRPV1. PLoS ONE 6(1):e16116. doi:10.1371/journal.pone.0016116
Acknowledgments
This work was supported by Natural Science Foundation Project of CQ CSTC (CSTC2012JJJQ10003 to Li-Li Zhang) and National Natural Science Foundation of China (NSFC 81471193 to Li-Li Zhang, 81271282 to Jing-Cheng Li and 81400967 to Yan Pi).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
M.-J. Zhang and Y. Liu have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Zhang, MJ., Liu, Y., Hu, ZC. et al. TRPV1 attenuates intracranial arteriole remodeling through inhibiting VSMC phenotypic modulation in hypertension. Histochem Cell Biol 147, 511–521 (2017). https://doi.org/10.1007/s00418-016-1512-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-016-1512-x