Abstract
Morphological and histochemical analysis of the heart is fundamental for the understanding of cardiac physiology and pathology. The accurate detection of different myocardial cell populations, as well as the high-resolution imaging of protein expression and distribution, within the diverse intracellular compartments, is essential for basic research on disease mechanisms and for the translatability of the results to human pathophysiology. While enormous progress has been made on the imaging hardware and methods and on biotechnological tools [e.g., use of green fluorescent protein (GFP), viral-mediated gene transduction] to investigate heart cell structure and function, most of the protocols to prepare heart tissue samples for analysis have remained almost identical for decades. We here provide a detailed description of a novel protocol of heart processing, tailored to the simultaneous detection of tissue morphology, immunofluorescence markers and native emission of fluorescent proteins (i.e., GFP). We compared a variety of procedures of fixation, antigen unmasking and tissue permeabilization, to identify the best combination for preservation of myocardial morphology and native GFP fluorescence, while simultaneously allowing detection of antibody staining toward sarcomeric, membrane, cytosolic and nuclear markers. Furthermore, with minimal variations, we implemented such protocol for the study of human heart samples, including those already fixed and stored with conventional procedures, in tissue archives or bio-banks. In conclusion, a procedure is here presented for the laboratory investigation of the heart, in both rodents and humans, which accrues from the same tissue section information that would normally require the time-consuming and tissue-wasting observation of multiple serial sections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The green fluorescent protein (GFP) (Cody et al. 1993; Prasher et al. 1992) and its enhanced numerous variants represent a broad toolkit of fluorescent proteins (FPs) for the study of different biological and biochemical processes (Chalfie et al. 1994; Heim et al. 1994). FPs have been widely used for the generation of transgenic animals (Diekmann et al. 2015; Fasulo and Sullivan 2014; Hakamata et al. 2001; Matsunari et al. 2014; Miles et al. 2013; Okabe et al. 1997; Ormo et al. 1996) and represent useful markers for gene expression in experimental embryology, in the study of cellular structures or dynamics, as well as in regenerative medicine (Karussis et al. 2013; Kuai et al. 2015; Maldonado-Soto et al. 2014; Murry et al. 2004; Wang et al. 2014; Wu et al. 2015). For the optimal performance of such experiments, it is advisable to obtain, in the same tissue sample, information both on FP native fluorescence and on cell morphology and function by immuno- or histochemical analyses. However, retention of GFP within tagged cells, and even more so at the correct subcellular locations, requires intense tissue fixation (Chalfie and Kain 2005), which has to preserve FP conformation (Brejc et al. 1997; Li et al. 1997; Ormo et al. 1996), but inevitably causes autofluorescence and protein cross-linking (Del Castillo et al. 1989; Noonberg et al. 1992). This problem is particularly evident in striated muscles, due to the concurrent presence of several cell types of diverse morphology and size, and the inherent refractoriness of myocytes to antibody penetration, for the presence of densely packed myofibrils. At present, methods of tissue fixation allowing simultaneous detection of GFP and cell surface markers have been described for the lymphoid tissue (Kusser and Randall 2003). To the best of our knowledge, such methods have not been reported for the investigation of heart samples. In order to overcome this obstacle, immunofluorescence (IF) has been performed in unfixed sections, while adjacent ones were subsequently fixed with formaldehyde vapors, to detect native GFP fluorescence (Jockusch et al. 2003; Jockusch and Eberhard 2007). The main limitations of such approach are, however, represented by the time expenditure of the experimental procedure using serial sections, and the reduced preservation of tissue morphology and GFP fluorescence, all of which are not convenient for the detection and characterization of cells infiltrating or engrafting the myocardium (e.g., inflammatory or stem cells). The goal of our study was to develop a method of tissue fixation and permeabilization that simultaneously fulfills a series of requirements: (1) preservation of native GFP fluorescence; (2) preservation of tissue morphology and antigenicity and (3) detection of intracellular and extracellular epitopes. We validated such protocol in experimental models of cell therapy and viral gene delivery. In addition, we adapted our epitope-unmasking protocol to obtain IF staining in formalin-fixed, paraffin-embedded (FF-PE) human heart samples, demonstrating that our procedure can be exploited for the detailed analysis of postmortem human myocardial samples.
Materials and methods
General reagents
Zoletil (tiletamine cloridrate plus zolepam cloridrate) and Xilor (2 % xilazine) were used for animal anesthesia. Paraformaldehyde (PFA), ethanol, xilene, sucrose, bovine serum albumin (BSA) and Triton X-100 were obtained from Sigma-Aldrich (Milan, Italy). Primary antibodies used in this study are listed in Table 1. Secondary antibodies were provided by Jackson Lab (UK).
Equipment
In this study, we used: 0.5-ml syringes; 18G and 22G needles; 5/0 propylene suture; silicon tubes; peristaltic pump; Superfrost Plus coverslips; surgical instruments; coplin jar; microwave; cryostat (Leica CM1850, Leica Microsystems GmbH, Wetzlar, Germany); microtome (Jung AG, Heidelberg, Germania); fluorescence microscope (Leica DC130, Leica Microscopes, Germany) and confocal microscope (Leica TCS-SP5).
Animal models
The following animal models were studied: wild-type (WT) C57BL/6J male mice (Charles River, Milan, Italy); transgenic male mice expressing the enhanced GFP under the control of β-actin promoter (C57BL/6-Tg(CAG-EGFP)1Osb/J, Jackson Laboratories, Bar Harbor, Maine, USA); WT Sprague–Dawley rats (Harlan Lab., Milan, Italy), as well as GFP + transgenic rats (a gift from Dr. Okabe, University of Osaka, Japan) (Ito et al. 2001). All experimental procedures described in this manuscript have been approved by the institutional ethical committee (authorization number VIMM/C54) and communicated to the relevant Italian authority (Ministero della Salute, Ufficio VI), in compliance with Italian Animal Welfare Law (Laws n 116/1992, D.Lgs 26/2014 and subsequent modifications).
Heterotopic heart allo-transplantation
Male GFP + transgenic rats (3 months old, 200–250 g) were used as heart recipients, while heart donors were WT male rats (2 months old, 150–200 g). Heterotopic heart transplantation was performed according to the method described by Ono and Lindsey (Yokoyama et al. 1995), slightly modified at our center (Dedja et al. 2005). Donor rats were anesthetized by isoflurane (FORANE®, Abbott SpA, Campoverde di Aprilia) at 1–1.5 % with oxygen and treated with 5 mg/kg of intraperitoneal tramadol. After donor heparinization, hearts were removed, perfused with the cardioplegic preservation solution CELSIOR (CS) (Imtix, Sangstat, Lyon) for few minutes and then transplanted, under magnification, into the abdomen of the recipient. The donor’s aorta and the pulmonary artery were anastomized to the recipient’s abdominal aorta and abdominal vena cava, respectively. Transplanted animals were treated with 5 mg/kg tramadol, injected i.m. twice daily in the first two postoperative days. To prevent infections, the antibiotic terramycin LA (Pfizer) (60 mg/kg) was administered subcutaneously to the transplanted animals. Cyclosporine A (SANDIMMUNE®, Novartis Italia, Rome), 10 mg/kg/day was injected i.m., during post-op period. Transplanted rats were killed 15 days after surgery and hearts processed as described in “Results” section.
Heart perfusion with PFA
For heart perfusion, the rat and mouse thoracic cavity was opened and the aorta was cannulated in the abdomen with an 18-G needle (for rats) or 22-G needle (for mice), respectively. The right and left carotid arteries were occluded, and the inferior vena cava was cut to allow outflow of the fixative. Hearts were retrogradely perfused, using a peristaltic pump, with 50 ml (rats) or 20 ml (mice) of 1× PBS at a rate of 200 ml/h (rat) or 75–100 ml/h (mouse), followed by 150 ml or 30 ml of 4 % PFA, respectively. In the transplanted rats, at the time of killing, the abdominal cavity was opened, the right iliac artery was cannulated, and the abdominal aorta was cut. A peristaltic pump was connected to the iliac artery and the heterotopic heart perfused as previously described. At the end of perfusion, hearts were washed in 1× PBS and dehydrated in sucrose gradient (p:v in H2O) (i.e., 5 % sucrose for 15 min; 15 % sucrose for 30 min and 30 % sucrose overnight at 4 °C).
Human samples and processing
We analyzed postmortem heart samples archived in the historical collection of the institute of Pathological Anatomy of the University of Padova and acquired during routine postmortem clinical investigations. Samples were anonymous to the investigators and used in accordance with the directives of the national committee of Bioethics and Raccomandazione (2006) della Commissione dei Ministri degli Stati Membri sull’utilizzo di campioni biologici di origine umana per scopi di ricerca. The heart samples used in this study underwent prolonged formalin fixation (range from 3 to 6 weeks), followed by paraffin inclusion (PER-INTELSINT RVG/2 KALTEK srl). Microtome processed sections (3 µm thick) were placed on glass coverslips (Superfrost plus).
Microwave irradiation of heart slices
The cover glasses with the slides were placed in a glass case, lying on their long edge, and subsequently immersed in a jar filled with 200 ml of 1 mM EDTA, pH 8.00. A practical solution to maintain homogenous heat distribution (Shi et al. 1991) in the buffer volume was to always fill the jar with equal number of coverslips, by adding empty ones if necessary.
Adult mouse infection
AAV9-GFP-U6-CHMP2Bsh (1 × 1012) (Vector Biolabs) was delivered, by tail injection, to adult (3 months old) C57BL/6J wild-type mice. A control group of mice injected with the viral vehicle (1× PBS) was also set up. Animals were killed 6 weeks after viral infection.
Results
Comparison of different fixation protocols on preservation of tissue morphology and GFP fluorescence
To determine the best strategy to both maintain the integrity of myocardial morphology and preserve the native GFP fluorescence, we compared different fixation protocols in hearts from transgenic rats and mice, expressing enhanced GFP (EGFP) under control of the β-actin promoter. Comparison was made between hearts:
-
1.
snap frozen in liquid nitrogen;
-
2.
fixed by immersion in 4 % PFA (Sigma, Milan, Italy) (v:v in 1× PBS) for 2 h at room temperature;
-
3.
perfused with 4 % PFA.
Irrespective of the protocol used, the hearts were dehydrated in sucrose gradient, embedded in OCT matrix (Kaltek, Padova, Italy) and subsequently snap frozen in liquid nitrogen. After freezing, ten-micron-thick ventricular cryosections were prepared at the cryostat and used for both histological and immunofluorescence (IF) analysis and microscopy. As shown in Fig. 1a, b, snap-freezing the hearts without fixation (1) caused, as expected, gross alteration of myocardial structure and disappearance of EGFP fluorescence. On the contrary, PFA fixation allowed preservation of both morphology and EGFP fluorescence, the latter remaining better preserved in PFA-perfused (3), than in PFA-immersed (2) hearts.
Comparison of different fixation protocols and microwave treatments on heart sections from GFP-positive transgenic rats. a Hematoxylin–eosin staining on ventricular sections from hearts which underwent: no fixation (left panel), PFA-immersion (middle panel) or PFA-perfusion fixation (right panel). b Microscope imaging analysis of native EGFP fluorescence intensity (green signal) on ventricular sections which underwent: no fixation (left panel), PFA-immersion (middle panel) or PFA-perfusion fixation (right panel). The white lines in b evidence cardiomyocytes (CM). Images in a, b are details from the left ventricular wall
Identification of the optimal antigen retrieval protocol
It is well known that PFA perfusion either abolishes or drastically reduces immunoreactivity with the majority of the antibodies used routinely in cardiovascular studies. To preserve native EGFP fluorescence and unmask protein epitopes for specific antibody reactions, we tested different treatments:
-
1.
microwave irradiation;
-
2.
Triton X-100 permeabilization;
-
3.
a combination of (1) and (2).
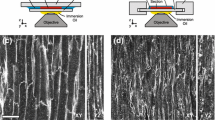
For microwave irradiation (see ‘Materials and methods’), different conditions of microwave power and irradiation times were tested to permeabilize heart cryosections while preserving the EGFP fluorescence. We found that microwave treatment for 10 min (i.e., a condition normally used when processing paraffin sections) dimmed significantly EGFP fluorescence, compared to the non-irradiated controls (Fig. 2a, b). This is likely due to temperature-dependent EGFP denaturation and disruption of the barrel-like conformation of the fluorescent protein (Yang et al. 1996). We identified the optimal antigen retrieval protocol to consist in three consecutive heat–cool cycles with 5-min heating at a power of 240 W (W), followed by slow cooling to 37 °C. The peak temperature of the coverslip bathing buffer ranged between 65 and 68 °C at the end of the heating cycle. These parameters allowed optimal preservation of native EGFP fluorescence and antigenicity, as demonstrated by subsequent immunostaining with an anti-GFP antibody, as well as tissue cyto-architecture (Fig. 2c–e). On the contrary, lower or higher number of microwave cycles decreased the antigen retrieval efficiency or preservation of tissue morphology, respectively.
Comparison of different microwave treatments on heart sections from GFP-positive transgenic rats. a–c Microscope imaging analysis of native EGFP fluorescence intensity (green signal) on ventricular sections from PFA-perfused hearts upon: no treatment (a), prolonged (240 Watt for 10 min) (b) and a short, but repetitive (240 W 5 min. for 3 times) (c, left panel) microwave treatments. The section in c was also co-stained with an anti-GFP antibody (right panel, red signal). Images in a–c are details from the left ventricular wall. d, e Hematoxylin–eosin staining on PFA-perfused ventricular sections upon: no treatment (d) and microwave–Triton treatment (e)
Heart section permeabilization
Microwave treatment was followed by IF staining, and we initially tested an antibody specific for the sarcomeric marker, α/β-Myosin Heavy Chain (α/β-MyHC) (Fig. 3a). Immunoreactivity was totally abolished by PFA perfusion (Fig. 3, NT) and only partially reconstituted by microwave treatment alone (Fig. 3, Mw). Based on our results, we thus used Triton X-100, a nonionic surfactant, previously used in both electron microscopy and light microscopy (Isobe et al. 1991; Schikorski 2010), to permeabilize the tissue and increase the immunostaining efficiency. Permeabilization alone was not sufficient to retrieve antigenicity (Fig. 3, Tr). The IF protocol was thus performed by incubating microwave-treated sections, with the primary (anti-α/β-MyHC, 12 h at 4 °C, then 2 h at 37 °C) and, subsequently, the secondary antibodies (2 h at 37 °C), both diluted in 1× PBS, supplemented with 1 % BSA and 1 % Triton X-100. We found that higher Triton concentrations (from 2 to 10 %) compromise preservation of tissue morphology and antigenicity, while lower (from 0.1 to 0.5 %) were not sufficient to achieve homogeneous immunostaining. In addition, too short Triton X-100 treatment (from 1 to 2 h at 37 °C) prior to heart slice incubation with primary antibodies did not allow obtaining good immunoreactivity. Combination of microwave and prolonged Triton treatment leads to full reconstitution of tissue immunoreactivity, without reducing the native EGFP fluorescence (Figs. 2c, 3, Mw/Tr), nor altering tissue morphology (Fig. 2d). In addition, such treatment blunts tissue autofluorescence and prevents aspecific interactions of secondary antibodies with tissue antigens (Suppl. Fig. 1–2).
Validation of the new protocol for the immunofluorescence analysis of heart sections from GFP-positive transgenic rats. a–g Immunofluorescence and microscope analysis on serial ventricular sections which underwent: no treatment (NT); microwave (Mw); Triton (Tr) or ‘microwave + Triton’ (Mw/Tr) treatments. Heart sections were stained with antibodies to: α/β-Myosin Heavy Chain (α/β-MHC) (a); desmin (b); smooth muscle actin (c, SMA); GATA-4 (d); connexin-43 (e, cx-43); CD31 (f, left panel) and laminin (g, left panel) (all red signals). The signal of native EGFP fluorescence (green signal), upon the combination of Mw/Tr treatments, is shown in the right panels. Images are all details from the left ventricle. The white arrow in d evidences a GATA-4-positive cardiomyocyte nucleus
Validation of the optimized method for immunostaining with examples of different antigens
To further validate our protocol, we tested antibodies for various proteins expressed by different myocardial cell types, at diverse subcellular location, including other cardiomyocyte sarcomeric proteins (i.e., desmin) (Fig. 3b); smooth muscle actin (SMA), expressed by muscular cells of the blood vessels (Fig. 3c); nuclear proteins, such as the transcription factors GATA-4 and Nkx2.5, expressed by most myocardial cells (Fig. 3d); connexin-43, forming the cardiac gap junctions (Fig. 3e) and the intermediate filament marker vimentin (not shown). Reduced number of Mw heating cycles and lower intensity permeabilization were sufficient for the detection of plasma membrane-associated proteins, such as CD31 and RECA-1 (for endothelial cells) (Fig. 3f), laminin (Fig. 3g) and dystrophin/dystroglicans (not shown). The same protocol was tested with a similar panel of antibodies in mouse heart samples (Suppl. Fig. 3).
In conclusion, we set up a protocol of tissue fixation and permeabilization that: (1) preserves tissue morphology; (2) demonstrates good sensitivity in the detection of both native EGFP and anti-GFP staining and (3) allows simultaneous imaging of native EGFP and IF staining on the same heart section.
Application of the method in cardiovascular stem cell biology research
The use of pluripotent and progenitor cells is a common method in stem cell therapy and cardiovascular regenerative medicine (Chen et al. 2015; Dixit and Katare 2015), with the goal of repopulating the damaged myocardium. Labelling of the transplanted cells with GFP allows to identify and characterize the fate of the cells engrafting the myocardium. However, engrafting cells are typically very rare and can potentially differentiate in any of the myocardial cell types, including endothelial, smooth muscle, fibroblasts and cardiomyocytes. For these reasons, it is important to unequivocally detect GFP-expressing cells in the heart sections with high sensitivity and detect, at the same time, markers of cell commitment (i.e., transcription factors) and differentiation (i.e., structural proteins). Here, we applied our sample processing protocol to image EGFP expressing cells in the experimental model of heterotopic heart transplant, previously used to determine the cardiogenic potential of circulating cells (Ausoni et al. 2005; Dedja et al. 2006). In this model, hearts from wild-type (WT) rats were transplanted into the abdomen of EGFP transgenic rat hosts, leading to the engraftment of EGFP circulating cells in the heterotopic transplanted heart (Fig. 4a). Sections obtained from the transplanted heart and processed using the protocol described above were stained with anti-GFP antibody, revealed with a red fluorescent-conjugated secondary antibody. Images of the sections were acquired, and fluorescent cells were independently counted in the red and green channels. The method did not alter myocardial cytoarchitecture (Suppl. Fig. 4a–b) and enhanced sensitivity in the detection of small non-cardiac GFP-positive cells engrafting the donor heart (Fig. 4a, b). In fact, cells scored positive in the red channel (anti-GFP IF) resulted all positive for EGFP when processed with our optimized protocol, while conventional fixation and IF protocols introduced false-negative results due to the variable reduction of EGFP fluorescence in a significant portion of donor-derived engrafting cells (see arrowheads in Fig. 4a, b). Such improved protocol was instrumental to the characterization of cell differentiation and lineage markers. We could easily detect cells immunoreactive for membrane proteins, such as the pan hematopoietic marker CD-45, the macrophage marker CD-163 and the widely used stem cell marker c-kit (CD-117) (Fig. 4c, d). Moreover, the combination of microwave and Triton X-100 treatment improved the staining with antibodies for nuclear and sarcomeric proteins. Figure 4e shows a cluster of typical EGFP-positive cells expressing the nuclear Ki-67, a marker of cycling cells, and Fig. 4f, g shows rare EGFP cells expressing the myocardial transcription factors GATA-4 and Nkx2.5, respectively. Consistent with our previous findings, rare EGFP-positive cells, expressing markers of mature cardiomyocytes (i.e., α-MyHC), were also detected (Fig. 4h). Identification and counting of such cells was much more easily performed using this improved method than the much more laborious one employed in our previous study.
Application of the new protocol to the characterization of small EGFP-positive infiltrating cells in rat heterotopic heart transplants (HHT). a, b Immunofluorescence (IF) analysis on ventricular sections from heterotopic heart transplants fixed by either PFA immersion (a) or PFA perfusion (b). Sections were stained with an antibody specific for GFP (right panels, red signals). The left panels show the signal of the native EGFP fluorescence (green signals). c IF analysis on untreated HHT sections which underwent to detection of native EGFP (left panel, green signal) and simultaneous co-staining with antibodies specific for CD-45 (middle panel, red signal) and CD-163 (right panel, blue signal). d Confocal IF analysis on untreated HHT sections which underwent to detection of native EGFP (left panel, green signal) and simultaneous staining with an antibody to the stem cell marker CD117 (middle panel, red signal). The right panel shows the merge of EGFP and CD117 signals. e–g Confocal IF analysis on ventricular sections from HHT. The combination of microwave treatment and Triton permeabilization allows the simultaneous detection of native EGFP (left panels, green signals) and the nuclear antigens: Ki-67 (e); GATA-4 (f) and Nkx2.5 (g) (middle panels, all red signals). The right panels in e–g represent the merges of the GFP signal and the antibody staining. White arrows indicate the circulating GFP+ cells engrafted into the myocardium and expressing proliferation markers (e) or cardiac transcription factors (f–g). h Confocal IF analysis on HHT sections treated with both microwave and Triton to detect simultaneously native EGFP (left panel, green signal) and α-MyHC (middle panel, red signal). The right panel shows the merge of the EGFP and α-MyHC signals. The white arrow indicates a mature GFP-positive cardiomyocyte
Application of the method in studies using viral-mediated gene delivery
Delivery of DNA or RNA in the heart cells by viral vectors (mainly AAV9) is largely used in cardiac gene therapy and molecular medicine (Bish et al. 2008a, b). The GFP gene is frequently included in the viral construct, either fused with the gene of interest or independently transcribed, to label and allow identification of the transduced cells in the tissue. Given that multiple factors may impact on the expression level of the virally encoded proteins (gene promoter, time from infection, targeted cell type), it is of paramount importance to use processing protocols preserving the highest degree of native GFP fluorescence. In addition, direct imaging of GFP, without the need of anti-GFP antibodies to amplify the fluorescence signal, allows easier co-staining with antibodies raised in the most widely used species (i.e., rabbit, mouse, goat).
We have previously addressed the role of the ESCRTIII protein CHMP2B, in the regulation of cardiomyocyte autophagy, by transducing shRNA targeted to CHMP2B with AAV9 vector (AAV9-GFP-U6-CHMP2Bsh) in adult WT mice (Zaglia et al. 2014). Assessment of the autophagy flux is based on the simultaneous detection of the expression level and subcellular localization of multiple proteins associated with autophagosomes and lysosomes. Such experiment required a time-consuming triple co-IF with antibodies raised in different species, like anti-LC3 (raised in rabbit), anti-p62 (raised in guinea pig) or anti-LAMP2a (in rat), all in combination with the anti-GFP to identify transduced cells. Our improved IF protocol allowed to detect transduced cells by direct imaging of GFP, thus reducing the complexity of the experiment (from a triple to a double co-IF) and allowing better correlation between the expression level of the transduced gene and the biological phenotype (Fig. 5; Suppl. Fig. 4c–d).
Application of the method in studies using viral-mediated gene delivery. a–c Confocal immunofluorescence analysis on heart sections from C57B6/6J WT mice that underwent AAV9-GFP-U6-CHMP2Bsh infection. Sections were treated with both microwave and Triton to detect native EGFP (a green signal) and simultaneously the staining with antibodies to LC3 (b pink signal) and LAMP2 (c red signal)
Adaptation of the epitope-unmasking protocol in formalin-fixed, paraffin-embedded human heart samples
Based on the efficiency of our improved IF protocol described above, we exploited it for the analysis of cellular and subcellular markers in human autoptic heart samples. These postmortem tissues underwent prolonged formalin fixation and paraffin embedding (FF-PE), the conventional procedure used in pathological anatomy worldwide for heart preservation and processing with standard morphological analyses. In this context, the problem is obviously not imaging FPs, but rather being able to efficiently perform IF in human samples from healthy and diseased hearts, which would represent a valuable resource for translational medicine. Unfortunately, the samples collected in such repositories have often undergone prolonged fixation, which offers optimal preservation of tissue morphology, without compromising the efficiency of standard histological analyses, used for the study of gross myocardial morphology, such as hematoxylin–eosin and trichrome staining. However, a strong fixation in formalin precludes the possibility to use methods of investigations useful to dissecting cellular, subcellular and molecular structures (e.g., confocal IF).
To this purpose, we adapted our protocol of tissue epitope unmasking and permeabilization, based on the combination of microwave and Triton X-100, for IF in human heart sections. FF-PE heart sections (3 µm thick) underwent, sequentially: (1) deparaffinization; (2) microwave treatment; (3) Triton X-100 tissue prepermeabilization and (4) IF staining. For microwave treatment (2), heart sections, immersed in 1 mM EDTA pH 8.00, were irradiated at a power of 750 W, and the bathing buffer was boiled for 45 s, before slow cooling to 45 °C. Such cycle was repeated for eight consecutive times. To improve homogeneity and intensity of IF staining (in Fig. 6b, c, compare panels Mw, Tr and Mw/Tr), heat-based epitope unmasking was associated with incubation of heart sections in 1× PBS, supplemented with 1 % BSA and 10 % Triton X-100, for 2 h at 37 °C (3). Permeabilization was prolonged overnight at 4 °C, in the presence of the primary antibody (4). Even if seemingly strong, such combination of microwave and Triton treatments did not damage myocardial morphology (Fig. 6a). A lower microwave power or number of heat–cool cycles as well as reduced Triton X-100 concentration decreased the antigen retrieval efficiency. On the contrary, a stronger unmasking/permeabilization protocol compromised preservation of protein antigenicity and myocardial cytoarchitecture. This protocol was validated by using antibodies to sarcomeric proteins (i.e., α-actinin), SMA (Fig. 6b, c), as well as cardiomyocyte membrane-associated proteins, such as dystrophin (see Fig. 6d; Suppl. Fig. 5 for controls). In addition, our procedure allowed revealing small and fragile heart components, e.g., adrenergic neuronal processes infiltrating the myocardial interstitium, without altering their fine morphological features (Fig. 6e).
Validation of the new immunofluorescence protocol on formalin-fixed and paraffin-embedded human heart sections. a Hematoxylin–eosin staining on serial transmural left ventricular sections undergone: no treatment (NT, left panel) or ‘microwave + Triton’ (Mw/Tr, right panel). b–e Confocal immunofluorescence analysis on serial transmural left ventricular sections undergone: no treatment (NT); microwave (Mw); Triton (Tr) or ‘microwave + Triton’ (Mw/Tr) treatments. Heart sections were stained with antibodies to: smooth muscle actin (b SMA), sarcomeric α-actinin (c), dystrophin (d), the sympathetic neuron marker tyrosine hydroxylase (e TOH) (all red signals, except dystrophin, green). Note that the combination of Mw/Tr significantly increases the efficiency of antibody staining
Conclusions
We here implemented a protocol of tissue unmasking and permeabilization allowing simultaneous IF and detection of GFP in mammalian hearts from different experimental models, as well as IF in FF-PE human hearts. In summary, the key steps of our optimized procedure are:
-
1.
for fixation of experimental hearts we recommend heart perfusion as it ensures uniform distribution of the fixative and allows shorter treatment duration, while preserving myocardial morphology and native FP fluorescence;
-
2.
during antigen unmasking with microwave irradiation, the critical points are the tight temperature control and the duration of heating cycles. Tissue temperature must be high enough to break the cross-bridges generated by the fixative, but no so high as to damage tissue integrity and FP fluorescence. For human heart samples, strong irradiation was used to increase homogeneity in tissue unmasking, given that samples had been fixed for prolonged time and did not express FPs;
-
3.
tissue permeabilization achieved using nonionic surfactants (e.g., Triton X-100) was found to improve antibody penetration and increase the signal of the specific versus background fluorescence.
Discussion
The study of myocardial histology and protein expression has classically been a fundamental step in the understanding of cardiac physiology and pathology. The many discoveries in cellular and molecular biology have brought about the necessity of more accurate and detailed analyses of myocardial cells in their tissue context. A great impulse in the investigation of cell biology derived from the discovery of GFP, which was soon used as a marker of cell lineage, as well as to label intracellular organelles and specific proteins, and all these approaches were rapidly applied to the investigation of heart biology. In parallel, the study of experimental medicine benefited from technological development of microscopy methods, which now allow detection of fluorescence in deep tissues at high spatial detail, and simultaneous discrimination of several light colors (i.e., fluorescence spectral windows).
Despite these progresses, most of the methods used for sample preparation and processing have remained almost identical for few decades, and as such, they suffer from important limitations when combined detection of FPs and antibody staining (e.g., IF) is required. One of the problems in the detection of FP-labelled cells is the high solubility of the fluorescent moiety that requires rather intense fixation of the sample, to preserve the FP conformation (Chalfie and Kain 2005; Ormo et al. 1996). The standard procedure using aldehyde fixation, however, increases tissue background and autofluorescence, generating false-positive results during cell characterization (Callis 2010; Kyosola et al. 1976). Paraformaldehyde also generates protein cross-linking that masks the antigenicity of many proteins, thus hampering the use of antibody staining for GFP-positive cell characterization. This is particularly critical for the study of myocardium (Kusser and Randall 2003), that is extremely refractory to antibody penetration, due to the presence of cells with densely packed myofibrils (Jockusch et al. 2003).
Some authors have developed methods of tissue fixation allowing simultaneous detection of GFP and fluorescent cell surface (Kusser and Randall 2003), while others have aimed at the optimization of procedures for correlative fluorescence and ultrastructural imaging using CLEM and other image acquisition technologies, mainly in cultured cells or nervous tissue (Paez-Segala et al. 2015; Peddie et al. 2014). To the best of our knowledge, however, similar protocols were not developed for the analysis of parenchymal organs, with complex cytoarchitecture and difficult antibody penetration, such as heart. At the time being, preservation of FP fluorescence in samples prepared for IF is a problem commonly experienced in research laboratories, which is often dealt with through procedural tricks and anecdotal solutions, as documented by the discussion thread in: www.researchgate.net/post/GFP_fluorescence_after_fixation10.
In addition, simultaneous imaging of several subcellular structures labelled with differently colored markers is theoretically possible in modern imaging systems that efficiently separate fluorescence emitted at various wavelengths (e.g., fluorescent-conjugated antibody). However, co-staining of more than two targets becomes difficult, due to cross-reactivity and reciprocal interference of the various antibodies used. Given that a broad range of spectral variants of FPs have been developed, and biotechnological strategies can be used to drive their expression in specific cell populations, the combination of FP imaging with IF would also reduce the number of antibodies necessary for multiple staining and improve accuracy by reducing artifacts. The procedure here described achieves all the aforementioned goals, with an affordable time and reagent expenditure.
Furthermore, the limits arising from the use of standard tissue preparation and processing protocols in studying specific intracellular structures in cardiac cells with IF are particularly evident when dealing with postmortem human heart samples. In fact, these samples are preserved in bio-banks or pathology archives, often after prolonged formalin fixation and paraffin embedding. In most cases, such tissue samples are analyzed with conventional histological methods used in clinical pathology, but this limits their potential in translational medicine. The development of optimized procedures to extract more detailed information on protein localization and interactions, as well as cellular signaling readouts, would open to the better understanding of cardiovascular disease mechanisms.
Abbreviations
- AAV9:
-
Adeno-associated virus serotype 9
- α/βMyHC:
-
α/β-Myosin Heavy Chain
- BSA:
-
Bovine serum albumin
- CHMP2B:
-
Charged multivesicular body protein 2B
- Cx43:
-
Connexin-43
- EGFP:
-
Enhanced green fluorescent protein
- FF-PE:
-
Formalin-fixed paraffin-embedded
- FP:
-
Fluorescent protein
- GFP:
-
Green fluorescent protein
- HHT:
-
Heterotopic heart transplant
- IF:
-
Immunofluorescence
- PBS:
-
Phosphate-buffered saline
- PFA:
-
Paraformaldehyde
- SMA:
-
Smooth muscle actin
- WT:
-
Wild type
References
Ausoni S, Zaglia T, Dedja A, Di Lisi R, Seveso M, Ancona E, Thiene G, Cozzi E, Schiaffino S (2005) Host-derived circulating cells do not significantly contribute to cardiac regeneration in heterotopic rat heart transplants. Cardiovasc Res 68(3):394–404
Bish LT, Morine K, Sleeper MM, Sanmiguel SJ, Wu D, Gao G, Wilson JM, Sweeney HL (2008a) Adeno-associated virus (AAV) serotype 9 provides global cardiac gene transfer superior to AAV1, AAV6, AAV7, and AAV8 in the mouse and rat. Hum Gene Ther 19(12):1359–1368
Bish LT, Sleeper MM, Brainard B, Cole S, Russell N, Withnall E, Arndt J, Reynolds C, Davison E, Sanmiguel J, Wu D, Gao G, Wilson JM, Sweeney HL (2008b) Percutaneous transendocardial delivery of self-complementary adeno-associated virus 6 achieves global cardiac gene transfer in canines. Mol Ther 16(12):1953–1959
Brejc K, Sixma TK, Kitts PA, Kain SR, Tsien RY, Ormo M, Remington SJ (1997) Structural basis for dual excitation and photoisomerization of the Aequorea victoria green fluorescent protein. Proc Natl Acad Sci USA 94(6):2306–2311
Callis G (2010) Glutaraldehyde-induced autofluorescence. Biotech Histochem 85(4):269
Chalfie M, Kain SR (2005) Green fluorescent protein: properties, applications and protocols, 2nd edn. Wiley, Haboken, pp 407–421
Chalfie M, Tu Y, Euskirchen G, Ward WW, Prasher DC (1994) Green fluorescent protein as a marker for gene expression. Science 263(5148):802–805
Chen CH, Sereti KI, Wu BM, Ardehali R (2015) Translational aspects of cardiac cell therapy. J Cell Mol Med 19(8):1757–1772
Cody CW, Prasher DC, Westler WM, Prendergast FG, Ward WW (1993) Chemical structure of the hexapeptide chromophore of the Aequorea green-fluorescent protein. Biochemistry 32(5):1212–1218
Dedja A, Dall’Olmo L, Cadrobbi R, Baldan N, Fante F, Calabrese F, Rigotti P, Ferraresso M, Delriviere L, Cozzi E, Ancona E (2005) Heterotopic cardiac xenotransplantation in rodents: report of a refined technique in a hamster-to-rat model. Microsurgery 25(3):227–234
Dedja A, Zaglia T, Dall’Olmo L, Chioato T, Thiene G, Fabris L, Ancona E, Schiaffino S, Ausoni S, Cozzi E (2006) Hybrid cardiomyocytes derived by cell fusion in heterotopic cardiac xenografts. FASEB J 20(14):2534–2536
Del Castillo P, Ar Llorente, Stockert JC (1989) Influence of fixation, exciting light and section thickness on the primary fluorescence of samples for microfluorometric analysis. Basic Appl Histochem 33(3):251–257
Diekmann H, Kalbhen P, Fischer D (2015) Characterization of optic nerve regeneration using transgenic zebrafish. Front Cell Neurosci 9:118
Dixit P, Katare R (2015) Challenges in identifying the best source of stem cells for cardiac regeneration therapy. Stem Cell Res Ther 6:26
Fasulo B, Sullivan W (2014) Live confocal analysis of mutant- and drug-treated Drosophila embryos. Methods Mol Biol 1075:243–255
Hakamata Y, Tahara K, Uchida H, Sakuma Y, Nakamura M, Kume A, Murakami T, Takahashi M, Takahashi R, Hirabayashi M, Ueda M, Miyoshi I, Kasai N, Kobayashi E (2001) Green fluorescent protein-transgenic rat: a tool for organ transplantation research. Biochem Biophys Res Commun 286(4):779–785
Heim R, Prasher DC, Tsien RY (1994) Wavelength mutations and posttranslational autoxidation of green fluorescent protein. Proc Natl Acad Sci USA 91(26):12501–12504
Isobe Y, Hou GR, Lemanski LF (1991) Deep-etching immunogold replica electron microscopy of cytoskeletal elements in cultured hamster heart cells. Anat Rec 229:415–426
Ito T, Suzuki A, Imai E, Okabe M, Hori M (2001) Bone marrow is a reservoir of repopulating mesangial cells during glomerular remodeling. J Am Soc Nephrol 12(12):2625–2635
Jockusch H, Eberhard D (2007) Green fluorescent protein as a tracer in chimeric tissues: the power of vapor fixation. Methods Mol Biol 411:145–154
Jockusch H, Voigt S, Eberhard D (2003) Localization of GFP in frozen sections from unfixed mouse tissues: immobilization of a highly soluble marker protein by formaldehyde vapor. J Histochem Cytochem 51(3):401–404
Karussis D, Petrou P, Kassis I (2013) Clinical experience with stem cells and other cell therapies in neurological diseases. J Neurol Sci 324(1–2):1–9
Kuai XL, Ni RZ, Zhou GX, Mao ZB, Zhang JF, Yi N, Liu ZX, Shao N, Ni WK, Wang ZW (2015) Transplantation of mouse embryonic stem cell-derived oligodendrocytes in the murine model of globoid cell leukodystrophy. Stem Cell Res Ther 6(1):30
Kusser KL, Randall TD (2003) Simultaneous detection of EGFP and cell surface markers by fluorescence microscopy in lymphoid tissues. J Histochem Cytochem 51(1):5–14
Kyosola K, Partanen S, Korkala O, Merikallio E, Penttila O, Siltanen P (1976) Fluorescence histochemical and electron-microscopical observations on the innervation of the atrial myocardium of the adult human heart. Virchows Arch A Pathol Anat Histol 371(2):101–119
Li X, Zhang G, Ngo N, Zhao X, Kain SR, Huang CC (1997) Deletions of the Aequorea victoria green fluorescent protein define the minimal. J Biol Chem 272(45):28545–28549
Maldonado-Soto AR, Oakley DH, Wichterle H, Stein J, Doetsch FK, Henderson CE (2014) Stem cells in the nervous system. Am J Phys Med Rehabil 93(11 Suppl 3):S132–S144
Matsunari H, Kobayashi T, Watanabe M, Umeyama K, Nakano K, Kanai T, Matsuda T, Nagaya M, Hara M, Nakauchi H, Nagashima H (2014) Transgenic pigs with pancreas-specific expression of green fluorescent protein. J Reprod Dev 60(3):230–237
Miles EL, Gorman CO’, Zhao J, Samuel M, Walters E, Yi YJ, Sutovsky M, Prather RS, Wells KD, Sutovsky P (2013) Transgenic pig carrying green fluorescent proteasomes. Proc Natl Acad Sci USA 110(16):6334–6339
Murry CE, Soonpaa MH, Reinecke H, Nakajima H, Nakajima HO, Rubart M, Pasumarthi KB, Virag JI, Bartelmez SH, Poppa V, Bradford G, Dowell JD, Williams DA, Field LJ (2004) Haematopoietic stem cells do not transdifferentiate into cardiac myocytes in myocardial infarcts. Nature 428(6983):664–668
Noonberg SB, Weiss TL, Garovoy MR, Hunt CA (1992) Characterization and minimization of cellular autofluorescence in the study of oligonucleotide uptake using confocal microscopy. Antisense Res Dev 2(4):303–313
Okabe M, Ikawa M, Kominami K, Nakanishi T, Nishimune Y (1997) ‘Green mice’ as a source of ubiquitous green cells. FEBS Lett 407(3):313–319
Ormo M, Ab Cubitt, Kallio K, Gross LA, Tsien RY, Remington SJ (1996) Crystal structure of the Aequorea victoria green fluorescent protein. Science 273(5280):1392–1395
Paez-Segala MG, Sun MG, Shtengel G, Viswanathan S, Baird MA, Macklin JJ, Patel R, Allen JR, Howe ES, Piszczek G, Hess HF, Davidson MW, Wang Y, Looger LL (2015) Fixation-resistant photoactivatable fluorescent proteins for CLEM. Nat Methods 12(3):215–218 4 p following 218
Peddie CJ, Blight K, Wilson E, Melia C, Marrison J, Carzaniga R, Domart MC, O’Toole P, Larijani B, Collinson LM (2014) Correlative and integrated light and electron microscopy of in-resin GFP fluorescence, used to localise diacylglycerol in mammalian cells. Ultramicroscopy 143:3–14
Prasher DC, Eckenrode VK, Ward WW, Prendergast FG, Cormier MJ (1992) Primary structure of the Aequorea victoria green-fluorescent protein. Gene 111(2):229–233
Schikorski T (2010) Pre-embedding immunogold localization of antigens in mammalian brain slices. Methods Mol Biol 2010(657):133–144
Shi YC, Seib PA, Lu SP (1991) Leaching of amylose from wheat and corn starch. Adv Exp Med Biol 302:667–686
Wang Y, Zhou M, Wang X, Qin G, Weintraub NL, Tang Y (2014) Assessing in vitro stem-cell function and tracking engraftment of stem cells in ischaemic hearts by using novel iRFP gene labelling. J Cell Mol Med 18(9):1889–1894
Wu JM, Hsueh YC, Ch’ang HJ, Luo CY, Wu LW, Nakauchi H, Hsieh PC (2015) Circulating cells contribute to cardiomyocyte regeneration after injury. Circ Res 116(4):633–641
Yang TT, Kain SR, Kitts P, Kondepudi A, Yang MM, Youvan DC (1996) Dual color microscopic imagery of cells expressing the green fluorescent protein and a red-shifted variant. Gene 173:19–23
Yokoyama H, Ohmi M, Murata S, Nakame T, Tabayashi K, Mohri H (1995) Proposal of a working left heart model with a heterotopic transplantation technique in rats. J Heart Lung Transplant 14(4):706–712
Zaglia T, Milan G, Ruhs A, Franzoso M, Bertaggia E, Pianca N, Carpi A, Carullo P, Pesce P, Sacerdoti D, Sarais C, Catalucci D, Krüger M, Mongillo M, Sandri M (2014) Atrogin-1 deficiency promotes cardiomyopathy and premature death via impaired autophagy. J Clin Invest 124(6):2410–2424
Acknowledgments
We thank Dr. Stefano Schiaffino for critical reading of the manuscript and support to the experiments; Drs Emanuele Cozzi, Arben Dedja and Luigi Dall’Olmo for heterotopic heart transplantation. We thank Dr Camillo Barbisan for assistance on medical legal issues inherent in the use of human samples. We are also grateful to Alessandra Dubrovich and Emilio Bigon for technical assistance. This work was supported by University of Padova (Progetto Giovani Studiosi 2010, contract: GRIC101133) to Tania Zaglia, Telethon-Italy (GGP11224) to Marco Mongillo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicting of interest.
Additional information
Simonetta Ausoni and Marco Mongillo have contributed equally to this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure 1
Effects of the combined ‘Microwave+Triton’ treatment on tissue autofluorescence. (a–b) Hearts from GFP+ (a) and WT (b) rats were fixed by PFA perfusion. Ten µm heart sections underwent ‘microwave+Triton’ unmasking procedure and were imaged at the fluorescence microscopy using the same acquisition parameters. The images evidence that our protocol significantly blunts tissue autofluorescence without interfering with the GFP signal. (TIFF 3480 kb)
Figure 2
Secondary antibody staining in GFP positive mouse and rat heart sections. (a–c) Ventricular sections from GFP positive mice (a) and rats (b–c) underwent ‘microwave+Triton’ unmasking procedure, and were treated with 1X PBS, supplemented with 1% BSA and 1% Triton-X100 without a primary antibody, followed by incubation with anti-rabbit (a-b) and anti-mouse (c) secondary antibodies. (TIFF 14639 kb)
Figure 3
Validation of the new immunofluorescence protocol for the analysis of GFP positive mouse heart. (a–d) Immunofluorescence and microscope analysis on serial ventricular sections which underwent: no treatment (NT); microwave (Mw); Triton (Tr) or ‘microwave+Triton’ (Mw/Tr) treatments. Heart sections were stained with antibodies to: α/β-Myosin Heavy Chain (α/β-MHC) (a); desmin (b); GATA-4 (c); connexin-43 (d, cx-43). The signal of the native EGFP fluorescence upon the combination of Mw/Tr treatments is shown in the right panels (green signal). The white arrow in (c) evidences a GATA-4 positive cardiomyocyte nucleus. (TIFF 17504 kb)
Figure 4
Tissue morphology in heart sections from experimental models processed with the new immunofluorescence protocol. (a–d) Haematoxyln-eosin staining was performed in ventricular sections from heterotopic heart transplants (a–b) and hearts infected with AAV9-GFP-U6-CHMP2Bsh (c–d), before (a and c) and after (b and d) ‘microwave+Triton’ treatment. (TIFF 16867 kb)
Figure 5
Secondary antibody staining in human heart sections. (a–b) FF-PE heart sections underwent ‘microwave+Triton’ treatment and incubation with Cy3 conjugated anti-mouse (a), 488-conjugated anti-rabbit (b) and Cy3-conjugated anti-rabbit secondary antibodies, without previous incubation with specific primary antibodies. Sections were analyzed at the fluorescence microscopy. (TIFF 12676 kb)
Rights and permissions
About this article
Cite this article
Zaglia, T., Di Bona, A., Chioato, T. et al. Optimized protocol for immunostaining of experimental GFP-expressing and human hearts. Histochem Cell Biol 146, 407–419 (2016). https://doi.org/10.1007/s00418-016-1456-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-016-1456-1