Abstract
Insulin-like growth factor 1 (IGF-1) is a potent mitogenic protein which can enhance the osteogenic differentiation of periodontal ligament (PDL) fibroblasts. However, it remains unclear whether IGF-1 can stimulate the osteogenic differentiation and osteogenesis of human periodontal ligament stem cells (PDLSCs). In this study, STRO-1+ PDLSCs were isolated from human PDL tissues, treated with IGF-1, and their osteogenic capacity was investigated in vitro and in vivo. Dimethyl-thiazol-diphenyl tetrazolium bromide assay and flow cytometry results demonstrated that 10–200 ng/mL IGF-1 can stimulate the proliferation ability of PDLSCs and 100 ng/mL is the optimal concentration. Exogenous IGF-1 can modify the ultrastructure, enhance the alkaline phosphatase activity, the mineralization ability of PDLSCs, and increase the expression of osteogenic markers (runt-related transcription factor 2, osterix, and osteocalcin) at mRNA and protein levels. In vivo transplantation illustrated that IGF-1 treated implants generated more mineralized tissues, and presented stronger expression of RUNX2, OSX, and OCN than control group. Moreover, the expression of phosphor-ERK and phosphor-JNK in these stem cells was upregulated by IGF-1, indicating that MAPK signaling pathway was activated during the osteogenic differentiation of PDLSCs mediated by IGF-1. Together, the results showed that IGF-1 can promote the osteogenic differentiation and osteogenesis of STRO-1+ PDLSCs via ERK and JNK MAPK pathway, suggesting that IGF-1 is a potent agent for stem cell-based periodontal tissue regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontitis is a worldwide medical concern that causes irreversible destruction of periodontal support tissues, i.e., alveolar bone, periodontal ligament (PDL), and root cementum. World Health Organization (WHO) databanks indicate that severe periodontal disease is estimated to affect 5–20% of the population (Petersen et al. 2005). It is the main cause of tooth loss and associates with several systemic diseases including diabetes and hypertension. There is a wide range of treatment options that have been pursued in modern clinical practice, such as barrier membranes, autografts, demineralized freeze-dried bone allografts, bovine-derived xenografts, and combinations of membranes and fillers. However, only a few of these therapies have been regarded as true regenerative techniques with limited successes and unpredictable outcomes (Bosshardt and Sculean 2009).
Since the discovery of adult periodontal ligament stem cells (PDLSCs) in 2004, stem cell-based periodontal tissue regeneration has become one of the hot topics in the field of dentistry (Seo et al. 2004; Ding et al. 2010). Except for stem cells and biomimetic material niches, appropriate growth factors (GFs) are also necessary for the functional periodontal tissue regeneration (Chen et al. 2010a; Chen and Jin 2010). Usually, IGF-1 mediates its effects by binding to IGF-1 receptor on the cell surface, activating the inherent tyrosine kinase activity of the receptor, and enabling internalization of the receptor ligand complex to instigate signaling cascades, and to ultimately affect gene expression and protein synthesis (Romanelli et al. 2007; Laviola et al. 2007). A number of studies have proved that IGF-1 is a critical protein for the development and growth in many tissues. IGF-1 is a multifunctional peptide that regulates cell growth, differentiation, and expression of extracellular matrix proteins (Blom et al. 1992). Moreover, IGF-1 is believed to be a key mediator of wound healing and mesenchymal cell proliferation (Giannobile 1996). Raja et al. (2009) have reported that IGF-1 was able to enhance cell survival in PDL fibroblast by up-regulating antiapoptotic molecules and down-regulating pro-apoptotic molecules. Local and controlled release of IGF-1 from dextran-co-gelatin microspheres can improve periodontal regeneration (Chen et al. 2006). Moreover, a combination of IGF-1 and other GFs (PDGF-B or BMP-2) can enhance bone formation and periodontal reconstruction (Chen et al. 2010b). These studies suggest that IGF-1 may play an important role in the periodontal tissue regeneration. Although IGF-1 is able to enhance cell survival in PDL fibroblast by up-regulating antiapoptotic molecules and down-regulating pro-apoptotic molecules (Raja et al. 2009), little knowledge is available about the effects of exogenous IGF-1 on PDLSCs that are the main cell sources for functional periodontal tissue regeneration.
In this study, we hypothesized that exogenous IGF-1 may enhance the osteogenesis of PDLSCs. PDLSCs were isolated from human impacted molars, purified by STRO-1+ antibody and then treated with exogenous IGF-1. We found that IGF-1 can enhance the proliferation and osteogenic differentiation of PDLSCs in vitro and in vivo. We also demonstrated that IGF-1 can stimulate the osteogenic differentiation of PDLSCs via the MAPK signaling pathway, indicating that IGF-1 is a competent agent for stem cell-based periodontal tissue regeneration.
Materials and methods
Cell isolation and culture
Normal impacted non-caries third molars (n = 20) were collected from 15 individuals (aged 18–25 years) at the Department of Oral and Maxillofacial Surgery of Jiangsu Stomatological Hospital, following the approved guidelines set by the Ethical Committee of Stomatological School of Nanjing Medical University. PDL was gently separated from the root surface and then digested in a solution of 3 mg/mL collagenase type I (Sigma-Aldrich Chemie, Taufkirchen, Germany) and 4 mg/mL dispase (Roche, Mannheim, Germany) for 1 h at 37°C. PDL samples from different individuals were pooled and single-cell suspensions were obtained by passing the cells through a 70-μm strainer. Multi-colony-derived PDLSCs were isolated as previously described (Seo et al. 2004) and cultured in α-minimum essential medium (α-MEM; Gibco, Life Technologies, Grand Island, NY) supplemented with 10% fetal bovine serum (FBS; Gibco), 100 μmol/L ascorbic acid 2-phosphate (Sigma), 2 mmol/L glutamine (Gibco), 100 U/mL penicillin, and 100 μg/mL streptomycin (Gibco), and then incubated at 37°C in 5% CO2. These cells were purified by using rabbit anti-STRO-1 antibody (Santa Cruz, Delaware, CA) and sheep anti-rabbit IgG Dynabeads (Dynal Biotech, Oslo, Norway) according to the protocols of magnetic activated cell sorting (MACS). To determine their mesenchymal origin, PDLSCs were immunostained with antibodies against cytokeratin and vimentin (Bioworld Technology, Atlanta, GA, USA). Cells at 2–4 passages were used in subsequent experiments.
MTT assay
IGF-1 powder (Peprotech, Offenbach, Germany) was dissolved in sterile distilled water as the manual describes, aliquoted and stored at −70°C. The proliferation of PDLSCs was examined by MTT (Sigma) assay, a method based on the mitochondrial succinic dehydrogenase of proliferating cells in which MTT is reduced to an insoluble purple formazan reaction product, which can be determined quantitatively by a colorimetric assay. In brief, the cells were cultured in 96-well plates (Costar, Cambridge, MA) at an initial density of 3 × 103 cells/well in α-MEM containing 10% FBS until 60% confluence, and then serum-starved for 24 h. IGF-1 at 10, 20, 50, 100, and 200 ng/mL was added separately to α-MEM containing 10% FBS in the experiment groups. After 7 days of culture, the cells were treated with 5 mg/mL of MTT reagent and incubated at 37°C for 4 h. Cells were washed twice with 0.01 M PBS followed by the treatment with dimethyl sulfoxide (Sigma). The absorbance at 490 nm was read with an automatic enzyme-linked immunosorbent assay reader (ELx800, BioTek Instruments Inc., USA). MTT results are expressed as mean ± SD and experiments performed in triplicate.
Cell growth curve
To analyze the growth kinetics of IGF-1 treated PDLSCs, cells were seeded into 96-well plates (Costar) at a density of 3 × 103 cells/well. After serum starvation, cells were treated with 100 ng/mL IGF-1. Culture medium was changed every 2 days. For nine consecutive days, cells were harvested and counted everyday with Coulter counter (Beckman Coulter, Fullerton, CA). Trypan blue was added into the cell suspension to exclude the nonviable cells. Three independent growth kinetics experiments were performed for each group. The graph was plotted according to the average cell number, and population doubling time (PDT) was calculated according to Patterson formulation (Patterson 1979).
Flow cytometry
PDLSCs were plated into 6-cm culture dishes (Costar), cultured in α-MEM supplemented with 10% FBS until 60% confluence, and then serum-starved for 24 h. IGF-1 (100 ng/mL) was added into culture dishes of the experimental groups. After 3 days of incubation, cells were harvested and fixed with 75% ice-cold ethanol at 4°C for 30 min in the dark. DNA content was measured by FACScan flow cytometer (BD Biosciences, San Jose, CA). Cell cycle fractions (G0/G1, S, and G2/M phases) were determined by FCM. The experiment was repeated three times.
Cell ultrastructure
1 × 107 IGF-1 treated PDLSCs at day 7 were collected by centrifugation to deposit cell pellets for ultrastructural analysis. The pellets were fixed in 2.5% glutaraldehyde solution overnight at 4°C, and then examined by transmission electron microscopy (TEM) (JEM-2000EX, Japan).
Alkaline phosphatase activity and alizarin red staining
To evaluate osteogenic differentiation of these stem cells, both IGF-1 untreated and treated PDLSCs were seeded into 24-well plates (Costar) at a density of 1 × 104 cells/well, and then incubated in the osteogenic media containing α-MEM, 10% FBS, 100 U/mL penicillin, 100 μg/mL streptomycin, 2 mmol/L l-glutamine, 50 mg/L ascorbic acid, 10 mmol/L β-glycerophosphate, and 10 nmol/L dexamethasone (Sigma). ALP activity and calcium deposition were assessed at different time points. Another duplicate 24-well plate aliquoted with PDLSCs at the same cell density was applied to detect protein concentrations of different groups at different time points. ALP assay was performed as described previously (Lei et al. 2011) with an ALP kit (Sigma). Alizarin red staining was performed as described before (Yu et al. 2010); images were acquired using a scanner and then calcium contents were quantitatively analyzed by cetyl pyridinium chloride (CPC; Sigma) assay. All data were normalized to total protein content. Six parallel replicates were analyzed in each group.
Real-time reverse transcription-polymerase chain reaction (Real-time RT-PCR)
Both IGF-1 untreated and treated PDLSCs were cocultured with the osteogenic media. After 3, 7, and 14 days of culture, cells were harvested using 1 mL TRIzol reagent (Invitrogen, Carlsbad, CA). Total RNA was extracted according to the manufacturer’s protocol. The concentration and purity of the RNA samples were determined by the absorbance of RNA at 230, 260, and 280 nm, respectively. The first-strand cDNA was synthesized using a first-strand cDNA synthesis kit (Takara, Bio, Otsu, Japan). Real-time RT-PCR was performed using SYBR® Premix Ex Taq™ kit (Takara) in a quantitative PCR System (ABI 7300, CA). All primers were synthesized by the same manufacturer (Sangon Biotech, China). Sense and antisense primers used for the detection of RUNX2, OSX, OCN, and GAPDH were listed in Table 1. Real-time RT-PCR reaction conditions were: 95°C for 30 s, followed by 40 cycles of 95°C for 5 s and 60°C for 31 s. Gene expressions were normalized to the housekeeping gene GAPDH, which was used as an internal control. The relative expression was calculated according to the ratio of the copy numbers of the target genes (RUNX2, OSX, and OCN) to the GAPDH in each sample. The relative gene expression values were evaluated by the \( 2^{{ - \Updelta \Updelta C_{\text{t}} }} \) method (Livak and Schmittgen 2001; Bustin 2000). Data were expressed as mean ± standard deviation of three independent experiments.
Western blot analysis
Both IGF-1 untreated and treated PDLSCs were cultured in the osteogenic media for 3, 7, and 14 days. As for the evaluation of MAPK pathway, PDLSCs were seeded into 60 mm dishes. After 24 h incubation, cells were serum-starved for 48 h, and then treated with 100 ng/mL IGF-1 for 30, 60, and 90 min. Cells in different groups were collected, washed twice with cold PBS, and lysed in RIPA lysis buffer (Beyotime, China) containing 1 mM phenylmethylsulfonyl fluoride (PMSF; Beyotime) and phosphatase inhibitors (Roche). Cell debris was eliminated by centrifugation at 12,000 rpm for 15 min at 4°C. Protein concentrations were determined via Bradford protein assay. 40 μg protein per lane was loaded onto a 10% SDS-PAGE gel for electrophoresis, and then transferred onto 0.22 μm PVDF membranes (Millipore, Bedford, MA) at 300 mA for 1 h in a blotting apparatus (Bio-Rad, CA). Membranes were blocked with blocking solution (5% non-fat dried skimmed milk powder, 0.01 M PBS, and 0.1% Tween-20) at room temperature for 2 h, and subsequently incubated with primary antibodies (RUNX2, 1:1,000, Bioworld; OSX, 1:1,000, Abcam; OCN, 1:1,000, Abcam; ERK1/2, 1:1,000, Bioworld; phosphor-ERK1/2, 1:1,000, Bioworld; JNK1/2/3, 1:1,000, Bioworld; phosphor-JNK1/2/3, 1:1,000, Bioworld; P38, 1:1,000, Bioworld; phosphor-P38, 1:1,000, Bioworld; β-actin, 1:1,000, Abgent) overnight at 4°C. Finally, the membranes were rinsed with PBST (0.1% Tween-20 in 0.01 M PBS), incubated with appropriate horseradish peroxidase-conjugated secondary antibodies (1:10,000, Boster Biotech. Co. Ltd., Wuhan, China) at room temperature (22°C) for additional 1 h, visualized by SuperSignal West Pico Chemiluminescent Substrate (Thermo, Rockford, IL), and exposed to Kodak X-ray films. β-actin serves as the internal control in these experiments. This experiment was repeated in triplicate.
Cell pellet transplantation
1 × 106 PDLSCs at the third passage in IGF-1 untreated and treated groups were harvested by exposure to trypsin/EDTA for 1 min, centrifuged in a tube as cell pellets, and incubated with 10% FBS/α-MEM for another 3 h to make them well aggregated. 20 pellets were carefully seeded onto the absorbable gelatin sponges (AGS; Nanjing Pharmaceuticals Inc., China) immersed with 100 ng/mL IGF-1 and transplantation procedures were performed under ten renal capsules of immunocompromised mice using modified pipette tips. All retrieved tissues at day 21 post-transplantation were fixed in 4% polyoxymethylene, and processed for hematoxylin and eosin (H&E) staining.
Immunohistochemistry
Immunohistochemical analyses of recovered implants were performed using the streptavidin–biotin complex method according to the manufacturer’s recommended protocol. Briefly, tissue sections (5 μm) from representative paraffin blocks were deparaffinized in xylene and rehydrated through gradient ethanol solutions. For antigen epitopes retrieval, sections were processed by conventional microwave heating in 0.01 M citrate buffer (0.01 M sodium citrate and 0.01 M citric acid, pH 6.0) for 10 min. 100 μL 3% H2O2 was added on top of the section to suppress endogenous peroxidase activity for 10 min at room temperature (22°C). Then, sections were blocked by 5% normal goat serum for 1 h and incubated with primary antibodies (RUNX2, 1:200; OSX, 1:100; OCN, 1:100) overnight at 4°C. Incubation with PBS instead of primary antibodies served as negative controls. Finally, sections were rinsed and incubated with biotinylated secondary antibodies for 45 min at room temperature (22°C). Sections were washed three times with PBST, incubated with SABC (Boster) for 30 min, stained with 100 μL chromogen (DAB, Boster) solution. When brown color appeared, slides were counterstained with hematoxylin for 1 min and observed under the light microscope (Olympus). The percentage of positive areas or cells in each sample was calculated using Image-Pro Plus 5.0 software.
Statistics
Quantitative results were expressed as mean ± SD. Independent samples t test, Chi-square test, one-way analysis of variance (ANOVA), and Tukey’s multiple comparison test were performed with SPSS-Windows v.12.0 software. P values <0.05 were considered to be statistically significant.
Results
IGF-1 increased the proliferation and modified the ultrastructure of PDLSCs
PDLSCs were isolated and purified by STRO-1 antibody. These fusiform-shaped cells maintained the colony forming ability (Fig. 1a–c), and were positive for vimentin and negative for cytokeratin (Fig. 1d, e). Growth curve and flow cytometry were used to examine the cell proliferation rate. Generally, 20–200 ng/mL IGF-1 can promote the proliferation of PDLSCs, and 100 ng/mL IGF-1 is the optimal concentration (Fig. 2a; P < 0.01). Therefore, 100 ng/mL IGF-1 was utilized for subsequent experiments. As shown in cell growth curve (Fig. 2b), PDT in IGF-1 treated PDLSCs (39.71 ± 0.19 h) was significantly shorter (P < 0.01) than that in PDLSCs (45.74 ± 0.91 h). Flow cytometry assay revealed that the proliferation index (PI = S% + G2 M%) in IGF-1 group (38.33%) was significantly higher than that in PDLSCs group (25.58%, P < 0.01) (Fig. 2c, d). Moreover, some cell bodies and cytoplasmic processes of PDLSCs (Fig. 3a) become shorter after the treatment of 100 ng/mL IGF-1 (Fig. 3b). TEM analysis demonstrated that PDLSCs possessed the typical ultrastructural features of stem cells with a high nucleus/cytoplasm ratio and poorly developed cytoplasmic organelles (Fig. 3c, d). After 7-day treatment with IGF-1, these stem cells contained more organelles in the cytoplasm including the rough endoplasmic reticulum and mitochondria (Fig. 3e, f).
Effects of IGF-1 on proliferation of PDLSCs in vitro. a Proliferation activity of PDLSCs was enhanced by IGF-1 in a dose-dependent manner. IGF-1 at 20–200 ng/mL significantly stimulated the proliferation of PDLSCs as compared with the control group (P < 0.05) and IGF-1 at 100 ng/mL presented the highest activity of proliferation among all groups. b Growth curves of IGF-1 treated PDLSCs. Values are the mean ± SD, n = 6. c, d Flow cytometry analysis for IGF-1 untreated (c) and treated (d) PDLSCs. The proliferation index (PI = S% + G2M%) in IGF-1 group (38.33%) was significantly higher than that in PDLSCs group (25.58%, **P < 0.01)
Effects of IGF-1 on morphology of PDLSCs in vitro. a Untreated PDLSCs at day 7. b IGF-1 treated PDLSCs at day 7. c, e TEM analysis shown that untreated PDLSCs at day 7 had the typical ultrastructural features of stem cells, i.e., higher nuclear–plasma ratio (N/P ratio) and immature cytoplasmic organelles. d, f IGF-1 treated PDLSCs at day 7 contained more organelles in the cytoplasm including the rough endoplasmic reticulum (RER) and mitochondria (M). a, b Scale bars 100 μm; c–f Scale bars 2 μm
IGF-1 enhanced the osteogenic differentiation of PDLSCs
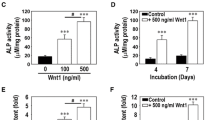
PDLSCs cultured with 100 ng/mL IGF-1 in osteogenic media show the higher ALP activities at day 3 (P < 0.01) and day 5 (P < 0.01), respectively, as compared with untreated cells (Fig. 4a). Alizarin red staining showed noticeable mineral nodules in the IGF-1 treated PDLSCs at day 21, as compared with control group (Fig. 4c). Furthermore, IGF-1 treated cells in osteogenic media at day 21 presented the strongest staining among all groups (Fig. 4c). CPC assay demonstrated that calcium concentrations in IGF-1 group at day 21 were significantly higher than control group (P < 0.01), while IGF-1 treated cells in osteogenic media demonstrated the highest calcium levels at days 14 and 21, respectively, among all groups (P < 0.01; Fig. 4b).
ALP assay and alizarin red staining of PDLSCs in different media. Four kinds of media: control medium, 100 mg/mL IGF-1 medium, mineralization inducing medium (MM), and 100 ng/mL IGF-1 plus mineralization inducing medium (IGF-1 + MM). a IGF-1 + MM group presented a higher level (P < 0.01) of ALP activity than MM group after 3-day and 5-day culture, respectively. b After 14-day culture, calcium contents in IGF-1 + MM group were significantly elevated (P < 0.01) as compared with those in MM group. After 21-day culture, calcium contents in IGF-1 + MM group were significantly higher (P < 0.01) than those in MM group. Moreover, calcium contents in IGF-1 group were also significantly uprised (P < 0.05) as compared with control group. Values are the mean ± SD, n = 6. c After 21-day culture, alizarin red staining demonstrated that IGF-1 group generated more calcification nodules than control group, while IGF-1 + MM group presented more mineralization than MM group (*P < 0.05, **P < 0.01)
Real-time RT-PCR results further revealed that RUNX2 mRNA was significantly uprised (Fig. 5a–c; P < 0.01) in IGF-1 treated PDLSCs both in basic medium and osteogenic medium (at days 3, 7, and 14, respectively), as compared with IGF-1 untreated groups. OSX mRNA was also significantly upregulated after 3-day simulation of IGF-1 both in basic medium and osteogenic medium (Fig. 5a; P < 0.01). OCN mRNA was significantly upregulated under the simulation of IGF-1 at days 7 and 14, respectively (Fig. 5b, c; P < 0.05).
Real-time reverse transcription-polymerase chain reaction and Western blot analyses of PDLSCs in different groups. a Gene expression of RUNX2, OSX, and OCN after 3-day culture. b Gene expression of RUNX2, OSX, and OCN after 7-day culture. c Gene expression of RUNX2, OSX, and OCN after 14-day culture. GAPDH was used as an internal control for each group. Gene expression was described as a fold change relative to the control group. Values are the means ± SD (**\( 2^{{ - \Updelta \Updelta C_{\text{t}} }} \) ≥ 2, P < 0.01; *1 < \( 2^{{ - \Updelta \Updelta C_{\text{t}} }} \) < 2, P < 0.01). d Protein expression of RUNX2, OSX, and OCN after 3-day culture. e Protein expression of RUNX2, OSX, and OCN after 7-day culture. f Protein expression of RUNX2, OSX, and OCN after 14-day culture. β-actin was used as a control for each group
Western blot results demonstrated that the protein levels of RUNX2 at days 3, 7, and 14 were elevated in IGF-1 treated groups both in basic medium and osteogenic medium (Fig. 5d–f), as compared with IGF-1 untreated groups. OSX levels were significantly increased in IGF-1 treated groups both in basic medium and osteogenic medium (at days 3, 7, and 14, respectively) as compared with IGF-1 untreated groups (Fig. 5d–f). The protein expression levels of OCN at days 7 and 14 were upregulated in IGF-1 treated groups (Fig. 5e, f) as compared with IGF-1 untreated groups.
Cell pellets were transplanted into renal capsules, and all implants at day 21 were successfully retrieved. Hematoxylin and eosin staining of serial sectioning show that all retrieved implants formed immature bone-like structures, in which IGF-1 treated group (Fig. 6d–f) presented bigger mineralization masses with less cell components than untreated group (Fig. 6a–c). Immunohistochemical findings demonstrated that the percentages of RUNX2/OSX-positive cells in treated implants (Fig. 7e, f, i, j) were significantly higher than those in untreated ones (Fig. 7a, b, i, j). The expression of OCN was much stronger in IGF-1 treated implants (Fig. 7g, k) than in untreated counterparts (Fig. 7c, k). These findings further confirmed the osteogenic effects of IGF-1 on PDLSCs.
Immunohistological staining of retrieved PDLSCs implants. a–c Untreated PDLSCs implants. A few cells were positive against RUNX2 (a) and OSX (b), and weak positive staining against OCN presented in untreated implants (c). d PBS as a negative control for untreated group. e–g Treated PDLSCs implants. Most cells in the bone-like structure were stained positively against RUNX2 (e) and OSX (f), whilst positive staining against OCN appeared in most area of the bone-like tissue (g), h PBS as a negative control for treated group. i The percentages of RUNX2-positive cells in treated and untreated groups. j The percentages of OSX-positive cells in treated and untreated groups. k Quantitative OCN immunopositive areas in treated and untreated groups. Values are the mean ± SD, n = 20. Scale bars 100 μm, **P < 0.01
IGF-1 can activate ERK and JNK pathways in PDLSCs
To elucidate why IGF-1 can promote the function of PDLSCs, we investigated whether MAPK pathway in PDLSCs is activated by IGF-1 treatment. As shown in Fig. 8, the levels of phosphor-ERK1/2 (Fig. 8a, d) and phosphor-JNK (Fig. 8b, e) in IGF-1 treated cells were upregulated. Quantitatively, the phosphor-ERK1/2 increased approximately eightfold at 30 min, sevenfold at 60 min and fivefold at 90 min in IGF-1 treated group as compared with control ones (Fig. 8d; P < 0.01). The phosphor-JNK increased approximately fourfold at 60 min and fivefold at 90 min in IGF-1 treated group as compared with untreated ones (Fig. 8e; P < 0.01). However, the levels of phosphor-P38 were not affected (Fig. 8c, f).
Effects of IGF-1 on the MAPK pathway of PDLSCs. a Protein expression of phosphor-ERK 1/2 and ERK 1/2 by Western blotting. b Protein expression of phosphor-JNK and JNK. c Protein expression of phosphor-p38 and p38. d The ratio of pERK/ERK intensity in a. e The ratio of pJNK/JNK intensity in b. f The ratio of p-P38/P38 intensity in c. Values are the mean ± SD, n = 3. **P < 0.01
Discussion
During tooth root morphogenesis, various growth factors mediate the interactions between Hertwig’s epithelial root sheath (HERS) and adjacent mesenchymal tissues, such as fibroblast growth factors (FGFs), transforming growth factors (TGFs), bone morphogenetic proteins (BMPs), and insulin-like growth factors (IGFs) (Torres et al. 2006, 2008; Caton and Tucker 2009). Several studies have demonstrated that IGF-1 can stimulate the proliferation of PDL cells, promote the wound healing of PDL, maintain periodontal homeostasis, and even elongate the molar roots (Fujiwara et al. 2005; Palioto et al. 2004; Gestrelius et al. 1997; Kheralla et al. 2010; Lossdorfer et al. 2009; Caton et al. 2005; Han et al. 2007; Giannobile 1996; Granero-Molto et al. 2011). Thus, it is reasonable that IGF-1 may have some influence on the differentiation of PDLSCs.
In the present study, IGF-1 can significantly promote the proliferation of PDLSCs in a dose-dependent manner, decrease the nuclear–plasma ratio and modify the ultrastructures of PDLSCs in vitro. At the concentration of 100 ng/mL, the proliferation rate of PDLSCs was at the peak of the curve with the shortest PDT and highest proliferation index. Besides, IGF-1 can exert some influence on the upregulation of ALP activity, calcium deposition, and expression of osteoblast markers (RUNX2, OSX, and OCN) in PDLSCs, indicating that IGF-1 can enhance the osteogenic differentiation of these periodontal stem cells. IGF-1 treated PDLSCs exhibited higher gene/protein expression levels of RUNX2/OSX at day 3 and OCN at days 7–14, suggesting that IGF-1 can trigger the early-stage osteogenic differentiation and maintain the late-stage osteogenic differentiation of PDLSCs in vitro. The transcription factors RUNX2 and OSX are necessary for the osteogenic differentiation (Baek et al. 2009; Kaback et al. 2008; Komori 2006). Runx2 is one of the mouse homologues of the Drosophila runt protein family, a small group of highly conserved differentiation factors that are characterized by a DNA-binding runt domain. Genetic and molecular studies have shown that RUNX2 plays a key role in the osteogenesis and serves as an early transcriptional regulator of osteogenic differentiation (Takeda et al. 2001; Karsenty and Wagner 2002). Runx2-deficient mice exhibit a complete lack of bone formation due to the maturation arrest of osteoblasts (Yamaguchi et al. 2000; Yamashiro et al. 2002; Kobayashi et al. 2006). RUNX2 direct the differentiation of mesenchymal stem cells into an osteoblastic lineage, and inhibits them to differentiate into the adipocytic and chondrocytic lineages. After differentiating into preosteoblasts, OSX and RUNX2 can drive them into immature osteoblasts and produce bone matrix. Then, RUNX2 prevents the osteoblast maturation and the transition into osteocytes (Komori 2006). Moreover, RUNX2 was found to regulate the expression of other mineralization-related genes (Gaikwad et al. 2001; Yu et al. 2006, 2007, 2010; Tziafas and Kodonas 2010). As a downstream gene of RUNX2, OSX is a second transcription factor that is essential for osteogenic differentiation and specifically expressed in all developing bones (Baek et al. 2009; Kaback et al. 2008; Komori 2006; Nakashima et al. 2002).
OSX is involved in osteogenic differentiation at the early and later stages of osteogenesis (Chen et al. 2009; Celil and Campbell 2005; Ulsamer et al. 2008). Genetic studies have shown that the cortical bone and bone trabeculate formation is abolished in Osx knock-out mice (Nakashima et al. 2002). It may function during bone regeneration and control the osteogenic differentiation involved in the regenerative osteogenesis (Tu et al. 2007). Moreover, OSX plays an important role in the mechanical stress-induced osteogenic differentiation of PDLCs and alveolar bone remodeling during the orthodontic therapy (Zhao et al. 2008). OCN is generally thought as a later-stage marker of mineralized bones (Bai et al. 2010), which is usually uprised during the differentiation of PDLSCs into osteoblast lineages (He et al. 2010; Takeda et al. 2005). The increased levels of RUNX2, OSX, and OCN in IGF-1 treated PDLSCs at different time points suggest that IGF-1 plays an important role not only in the early stage of osteogenesis but also in the later stage of bone formation. Moreover, the upregulated expression of phosphor-ERK1/2 and phosphor-JNK by IGF-1 indicates that the MAPK pathway is activated during the osteogenic differentiation of IGF-1 treated PDLSCs.
Many studies have shown that IGF-1 is one of the key factors during osteogenic differentiation and presents a beneficial effect on bone development (He et al. 2006; Yao et al. 2008; Tiago et al. 2010; Kanbur et al. 2005). The transplantation results demonstrated that IGF-1 can promote the osteogenesis of PDLSCs, as indicated by more mineralized bone formation and much stronger expression of several bone-specific proteins (i.e., RUNX2, OSX, and OCN) in vivo, further confirming that IGF-1 can enhance the osteogenic capacity of periodontal stem cells. IGF-1 mediates its effects by binding to IGF-1R on the cell surface, activating the inherent tyrosine kinase activity of the receptor, and enabling internalization of the receptor ligand complex to instigate signaling cascades which ultimately affect the gene expression and protein synthesis. IGF-1 triggers at least two signaling pathways, i.e., MAPK pathway and PI3K/PDK-1/Akt pathway (Grey et al. 2003; Hatakeyama et al. 2008). The activation of MAPK pathway contributes to the osteoblast survival as well as cellular proliferation/differentiation. Some studies have shown that ERK in MAPK pathway can converge with PI3K/PDK-1/Akt pathway on the downstream effectors and IGF-1 can regulate the expression of ALP, RUNX2, OSX, and OCN via MAPK pathway (Hanai et al. 2006; Qiao et al. 2004; Celil and Campbell 2005; Granero-Molto et al. 2011). In this study, the levels of phosphor-ERK1/2 and phosphor-JNK in IGF-1 treated PDLSCs were significantly increased in a time-dependent manner, suggesting that IGF-1 can promote the osteogenic differentiation and osteogenesis of human PDLSCs via the MAPK pathway.
In summary, IGF-1 can promote the osteogenic differentiation of STRO-1+ PDLSCs via the MAPK pathway in vitro and enhance their osteogenic mineralization in vivo, suggesting that IGF-1 plays an important role during the osteogenic differentiation and may have clinical implications for periodontal tissue regeneration as well as alveolar bone reconstruction. More extensive studies are required to investigate other pathway mechanisms associated with IGF-1 mediated osteogenic differentiation of PDLSCs.
Abbreviations
- AGS:
-
Absorbable gelatin sponges
- ALP:
-
Alkaline phosphatase
- BMP2:
-
Bone morphogenetic protein 2
- BMPs:
-
Bone morphogenetic proteins
- CPC:
-
Cetyl pyridinium chloride
- DAB:
-
Dimethylaminoazobenzene
- EMD:
-
Enamel matrix derivative
- ERK:
-
Extracellular regulated protein kinases
- FBS:
-
Fetal bovine serum
- FCM:
-
Flow cytometry
- FGFs:
-
Fibroblast growth factors
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GFs:
-
Growth factors
- HERS:
-
Hertwig’s epithelial root sheath
- IGF-1:
-
Insulin-like growth factor 1
- JNK:
-
c-Jun N-terminal kinase
- MAPK:
-
Mitogen-activated protein kinase
- MACS:
-
Magnetic activated cell sorting
- α-MEM:
-
α-Minimum essential medium
- MTT:
-
3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide
- OCN:
-
Osteocalcin
- OSX:
-
Osterix
- PBS:
-
Phosphate buffered saline
- PDGF-B:
-
Platelet-derived growth factor-B
- PDL:
-
Periodontal ligament
- PDLSCs:
-
Periodontal ligament stem cells
- PDT:
-
Population doubling time
- PVDF:
-
Polyvinylidene difluoride
- RUNX2:
-
Runt-related transcription factor 2
- SABC:
-
Streptavidin–biotin complex
- STRO-1+ :
-
Stromal precursor cell marker
- TEM:
-
Transmission electron microscopy
- TGFs:
-
Transforming growth factors
References
Baek WY, Lee MA, Jung JW, Kim SY, Akiyama H, de Crombrugghe B, Kim JE (2009) Positive regulation of adult bone formation by osteoblast-specific transcription factor osterix. J Bone Miner Res 24(6):1055–1065. doi:10.1359/jbmr.081248
Bai Y, Matsuzaka K, Hashimoto S, Kokubu E, Wang X, Inoue T (2010) Formation of bone-like tissue by dental follicle cells co-cultured with dental papilla cells. Cell Tissue Res 342(2):221–231. doi:10.1007/s00441-010-1046-9
Blom S, Holmstrup P, Dabelsteen E (1992) The effect of insulin-like growth factor-I and human growth hormone on periodontal ligament fibroblast morphology, growth pattern, DNA synthesis, and receptor binding. J Periodontol 63(12):960–968
Bosshardt DD, Sculean A (2009) Does periodontal tissue regeneration really work? Periodontol 2000 51:208–219. doi:10.1111/j.1600-0757.2009.00317.x
Bustin SA (2000) Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol 25(2):169–193 (JME00927)
He H, Yu J, Cao J, E L, Wang D, Zhang H, Liu H (2010) Biocompatibility and osteogenic capacity of periodontal ligament stem cells on nHAC/PLA and HA/TCP scaffolds. J Biomater Sci Polym Ed. doi:10.1163/092050609X12587018007767
Caton J, Tucker AS (2009) Current knowledge of tooth development: patterning and mineralization of the murine dentition. J Anat 214(4):502–515. doi:10.1111/j.1469-7580.2008.01014.x
Caton J, Bringas P Jr, Zeichner-David M (2005) IGFs increase enamel formation by inducing expression of enamel mineralizing specific genes. Arch Oral Biol 50(2):123–129. doi:10.1016/j.archoralbio.2004.11.012
Celil AB, Campbell PG (2005) BMP-2 and insulin-like growth factor-I mediate Osterix (Osx) expression in human mesenchymal stem cells via the MAPK and protein kinase D signaling pathways. J Biol Chem 280(36):31353–31359. doi:10.1074/jbc.M503845200
Chen FM, Jin Y (2010) Periodontal tissue engineering and regeneration: current approaches and expanding opportunities. Tissue Eng Part B Rev 16(2):219–255. doi:10.1089/ten.TEB.2009.0562
Chen FM, Zhao YM, Wu H, Deng ZH, Wang QT, Zhou W, Liu Q, Dong GY, Li K, Wu ZF, Jin Y (2006) Enhancement of periodontal tissue regeneration by locally controlled delivery of insulin-like growth factor-I from dextran-co-gelatin microspheres. J Control Release 114(2):209–222. doi:10.1016/j.jconrel.2006.05.014
Chen S, Gluhak-Heinrich J, Wang YH, Wu YM, Chuang HH, Chen L, Yuan GH, Dong J, Gay I, MacDougall M (2009) Runx2, osx, and dspp in tooth development. J Dent Res 88(10):904–909. doi:10.1177/0022034509342873
Chen FM, Zhang J, Zhang M, An Y, Chen F, Wu ZF (2010a) A review on endogenous regenerative technology in periodontal regenerative medicine. Biomaterials 31(31):7892–7927. doi:10.1016/j.biomaterials.2010.07.019
Chen FM, Zhang M, Wu ZF (2010b) Toward delivery of multiple growth factors in tissue engineering. Biomaterials 31(24):6279–6308
Ding G, Liu Y, Wang W, Wei F, Liu D, Fan Z, An Y, Zhang C, Wang S (2010) Allogeneic periodontal ligament stem cell therapy for periodontitis in swine. Stem Cells 28(10):1829–1838. doi:10.1002/stem.512
Fujiwara N, Tabata MJ, Endoh M, Ishizeki K, Nawa T (2005) Insulin-like growth factor-I stimulates cell proliferation in the outer layer of Hertwig’s epithelial root sheath and elongation of the tooth root in mouse molars in vitro. Cell Tissue Res 320(1):69–75. doi:10.1007/s00441-004-1065-5
Gaikwad JS, Hoffmann M, Cavender A, Bronckers AL, D’Souza RN (2001) Molecular insights into the lineage-specific determination of odontoblasts: the role of Cbfa1. Adv Dent Res 15:19–24
Gestrelius S, Andersson C, Lidstrom D, Hammarstrom L, Somerman M (1997) In vitro studies on periodontal ligament cells and enamel matrix derivative. J Clin Periodontol 24(9 Pt 2):685–692
Giannobile WV (1996) Periodontal tissue engineering by growth factors. Bone 19(1 Suppl):23S–37S
Granero-Molto F, Myers TJ, Weis JA, Longobardi L, Li T, Yan Y, Case N, Rubin J, Spagnoli A (2011) Mesenchymal stem cells expressing insulin-like growth factor-I (MSCIGF) promote fracture healing and restore new bone formation in Irs1 knockout mice: analyses of MSCIGF autocrine and paracrine regenerative effects. Stem Cells 29(10):1537–1548. doi:10.1002/stem.697
Grey A, Chen Q, Xu X, Callon K, Cornish J (2003) Parallel phosphatidylinositol-3 kinase and p42/44 mitogen-activated protein kinase signaling pathways subserve the mitogenic and antiapoptotic actions of insulin-like growth factor I in osteoblastic cells. Endocrinology 144(11):4886–4893. doi:10.1210/en.2003-0350
Han J, Meng HX, Tang JM, Li SL, Tang Y, Chen ZB (2007) The effect of different platelet-rich plasma concentrations on proliferation and differentiation of human periodontal ligament cells in vitro. Cell Prolif 40(2):241–252. doi:10.1111/j.1365-2184.2007.00430.x
Hanai Y, Tokuda H, Ishisaki A, Matsushima-Nishiwaki R, Nakamura N, Yoshida M, Takai S, Ohta T, Kozawa O (2006) Involvement of p44/p42 MAP kinase in insulin-like growth factor-I-induced alkaline phosphatase activity in osteoblast-like-MC3T3-E1 cells. Mol Cell Endocrinol 251(1–2):42–48. doi:10.1016/j.mce.2006.02.014
Hatakeyama N, Kojima T, Iba K, Murata M, Thi MM, Spray DC, Osanai M, Chiba H, Ishiai S, Yamashita T, Sawada N (2008) IGF-I regulates tight-junction protein claudin-1 during differentiation of osteoblast-like MC3T3-E1 cells via a MAP-kinase pathway. Cell Tissue Res 334(2):243–254. doi:10.1007/s00441-008-0690-9
He J, Rosen CJ, Adams DJ, Kream BE (2006) Postnatal growth and bone mass in mice with IGF-I haploinsufficiency. Bone 38(6):826–835. doi:10.1016/j.bone.2005.11.021
Kaback LA, Soung do Y, Naik A, Smith N, Schwarz EM, O’Keefe RJ, Drissi H (2008) Osterix/Sp7 regulates mesenchymal stem cell mediated endochondral ossification. J Cell Physiol 214(1):173–182. doi:10.1002/jcp.21176
Kanbur NO, Derman O, Kinik E (2005) The relationships between pubertal development, IGF-1 axis, and bone formation in healthy adolescents. J Bone Miner Metab 23(1):76–83
Karsenty G, Wagner EF (2002) Reaching a genetic and molecular understanding of skeletal development. Dev Cell 2(4):389–406 (S1534580702001570)
Kheralla Y, Gotz W, Kawarizadeh A, Rath-Deschner B, Jager A (2010) IGF-I, IGF-IR and IRS1 expression as an early reaction of PDL cells to experimental tooth movement in the rat. Arch Oral Biol 55(3):215–222. doi:10.1016/j.archoralbio.2010.01.002
Kobayashi I, Kiyoshima T, Wada H, Matsuo K, Nonaka K, Honda JY, Koyano K, Sakai H (2006) Type II/III Runx2/Cbfa1 is required for tooth germ development. Bone 38(6):836–844. doi:10.1016/j.bone.2005.10.026
Komori T (2006) Regulation of osteoblast differentiation by transcription factors. J Cell Biochem 99(5):1233–1239. doi:10.1002/jcb.20958
Laviola L, Natalicchio A, Giorgino F (2007) The IGF-I signaling pathway. Curr Pharm Des 13(7):663–669
Lei G, Yan M, Wang Z, Yu Y, Tang C, Yu J, Zhang G (2011) Dentinogenic capacity: immature root papilla stem cells versus mature root pulp stem cells. Biol Cell 103(4):185–196. doi:10.1042/BC20100134
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25(4):402–408. doi:10.1006/meth.2001.1262
Lossdorfer S, Abou Jamra B, Rath-Deschner B, Gotz W, Abou Jamra R, Braumann B, Jager A (2009) The role of periodontal ligament cells in delayed tooth eruption in patients with cleidocranial dysostosis. J Orofac Orthop 70(6):495–510. doi:10.1007/s00056-009-9934-x
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B (2002) The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 108(1):17–29 (S0092867401006225)
Palioto DB, Coletta RD, Graner E, Joly JC, de Lima AF (2004) The influence of enamel matrix derivative associated with insulin-like growth factor-I on periodontal ligament fibroblasts. J Periodontol 75(4):498–504. doi:10.1902/jop.2004.75.4.498
Patterson MK Jr (1979) Measurement of growth and viability of cells in culture. Methods Enzymol 58:141–152
Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C (2005) The global burden of oral diseases and risks to oral health. Bull World Health Organ 83(9):661–669 (S0042-96862005000900011)
Qiao M, Shapiro P, Kumar R, Passaniti A (2004) Insulin-like growth factor-1 regulates endogenous RUNX2 activity in endothelial cells through a phosphatidylinositol 3-kinase/ERK-dependent and Akt-independent signaling pathway. J Biol Chem 279(41):42709–42718. doi:10.1074/jbc.M404480200
Raja S, Byakod G, Pudakalkatti P (2009) Growth factors in periodontal regeneration. Int J Dent Hyg 7(2):82–89
Romanelli RJ, LeBeau AP, Fulmer CG, Lazzarino DA, Hochberg A, Wood TL (2007) Insulin-like growth factor type-I receptor internalization and recycling mediate the sustained phosphorylation of Akt. J Biol Chem 282(31):22513–22524. doi:10.1074/jbc.M704309200
Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, Young M, Robey PG, Wang CY, Shi S (2004) Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet 364(9429):149–155. doi:10.1016/S0140-6736(04)16627-0
Takeda S, Bonnamy JP, Owen MJ, Ducy P, Karsenty G (2001) Continuous expression of Cbfa1 in nonhypertrophic chondrocytes uncovers its ability to induce hypertrophic chondrocyte differentiation and partially rescues Cbfa1-deficient mice. Genes Dev 15(4):467–481. doi:10.1101/gad.845101
Takeda K, Shiba H, Mizuno N, Hasegawa N, Mouri Y, Hirachi A, Yoshino H, Kawaguchi H, Kurihara H (2005) Brain-derived neurotrophic factor enhances periodontal tissue regeneration. Tissue Eng 11(9–10):1618–1629. doi:10.1089/ten.2005.11.1618
Tiago DM, Cancela ML, Laize V (2010) Proliferative and mineralogenic effects of insulin, IGF-1, and vanadate in fish osteoblast-like cells. J Bone Miner Metab. doi:10.1007/s00774-010-0243-7
Torres CB, Goes VS, Goes AM, Pacifico LG, Silva GA, Junior NL, Alves JB (2006) Fibroblast growth factor 9: cloning and immunolocalisation during tooth development in Didelphis albiventris. Arch Oral Biol 51(4):263–272. doi:10.1016/j.archoralbio.2005.08.003
Torres CB, Alves JB, Silva GA, Goes VS, Nakao LY, Goes AM (2008) Role of BMP-4 during tooth development in a model with complete dentition. Arch Oral Biol 53(1):2–8. doi:10.1016/j.archoralbio.2007.07.005
Tu Q, Valverde P, Li S, Zhang J, Yang P, Chen J (2007) Osterix overexpression in mesenchymal stem cells stimulates healing of critical-sized defects in murine calvarial bone. Tissue Eng 13(10):2431–2440. doi:10.1089/ten.2006.0406
Tziafas D, Kodonas K (2010) Differentiation potential of dental papilla, dental pulp, and apical papilla progenitor cells. J Endod 36(5):781–789. doi:10.1016/j.joen.2010.02.006
Ulsamer A, Ortuno MJ, Ruiz S, Susperregui AR, Osses N, Rosa JL, Ventura F (2008) BMP-2 induces Osterix expression through up-regulation of Dlx5 and its phosphorylation by p38. J Biol Chem 283(7):3816–3826. doi:10.1074/jbc.M704724200
Yamaguchi A, Komori T, Suda T (2000) Regulation of osteoblast differentiation mediated by bone morphogenetic proteins, hedgehogs, and Cbfa1. Endocr Rev 21(4):393–411
Yamashiro T, Aberg T, Levanon D, Groner Y, Thesleff I (2002) Expression of Runx1, -2 and -3 during tooth, palate and craniofacial bone development. Gene Expr Patterns 2(1–2):109–112 (S0925477302002988)
Yao S, Pan F, Prpic V, Wise GE (2008) Differentiation of stem cells in the dental follicle. J Dent Res 87(8):767–771 (87/8/767)
Yu J, Deng Z, Shi J, Zhai H, Nie X, Zhuang H, Li Y, Jin Y (2006) Differentiation of dental pulp stem cells into regular-shaped dentin-pulp complex induced by tooth germ cell conditioned medium. Tissue Eng 12(11):3097–3105. doi:10.1089/ten.2006.12.3097
Yu J, Wang Y, Deng Z, Tang L, Li Y, Shi J, Jin Y (2007) Odontogenic capability: bone marrow stromal stem cells versus dental pulp stem cells. Biol Cell 99(8):465–474. doi:10.1042/BC20070013
Yu J, He H, Tang C, Zhang G, Li Y, Wang R, Shi J, Jin Y (2010) Differentiation potential of STRO-1+ dental pulp stem cells changes during cell passaging. BMC Cell Biol 11:32. doi:10.1186/1471-2121-11-32
Zhao Y, Wang C, Li S, Song H, Wei F, Pan K, Zhu K, Yang P, Tu Q, Chen J (2008) Expression of Osterix in mechanical stress-induced osteogenic differentiation of periodontal ligament cells in vitro. Eur J Oral Sci 116(3):199–206. doi:10.1111/j.1600-0722.2008.00533.x
Acknowledgments
This work was supported by National Natural Science Foundation of China (No. 81070798), Medical Elitist Project of Jiangsu Province (No. RC2011140), Nature Science Foundation of Jiangsu Province (No. BK2009346), Funding Project to Science Facility in Institutions of Higher Learning Under the Jurisdiction of Beijing Municipality (No. PXM2011_014226_07_000066), A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions.
Conflict of interest
No competing financial interests exist.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Y. Yu and J. Mu contributed equally to this work and should be considered as co-first authors.
Rights and permissions
About this article
Cite this article
Yu, Y., Mu, J., Fan, Z. et al. Insulin-like growth factor 1 enhances the proliferation and osteogenic differentiation of human periodontal ligament stem cells via ERK and JNK MAPK pathways. Histochem Cell Biol 137, 513–525 (2012). https://doi.org/10.1007/s00418-011-0908-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-011-0908-x